Professional Documents
Culture Documents
UC Care Benefits Outline 2014 As of 09/27/13
Uploaded by
Chris NewfieldOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
UC Care Benefits Outline 2014 As of 09/27/13
Uploaded by
Chris NewfieldCopyright:
Available Formats
University of California UC Care
Blue Shield of California
THIS MATRIX IS INTENDED TO BE USED TO HELP YOU COMPARE COVERAGE BENEFITS AND IS A SUMMARY ONLY. THE PLAN CONTRACT SHOULD BE CONSULTED FOR A DETAILED DESCRIPTION OF COVERAGE BENEFITS AND LIMITATIONS.
Highlights: A description of the prescription drug coverage is provided separately
Effective: January 1, 2014
UC Select
Blue Shield 1 Preferred $250 per individual/ $750 per family $3,000 per individual/ $9,000 per family None
Non-Preferred 1 Providers $500 per individual/ $1,500 per family $5,000 per individual/ $15,000 per family None Non-Preferred 1 Providers 50% 50% 50% 50%
Calendar Year Medical Deductible
(Deductible amounts do not cross accumulate)
2
None
Calendar year copayment maximum
(UC Select and Blue Shield Preferred Copayment Maximum amounts cross accumulate. UC Select/Blue Shield Preferred and Non-Preferred Copayment Maximums do not cross accumulate)
$1,500 per individual/ $4,500 per family None UC Select
LIFETIME BENEFIT MAXIMUM
Covered Services
PROFESSIONAL SERVICES Professional (Physician) Benefits Physician office visits (Includes Internist, Family Practice, OB/GYN,
Pediatrician, General Practice)
Member Copayment
Blue Shield 1 Preferred 20% 20% 20% 20%
$20 per visit $20 per visit N/A
(services covered under Blue Shield Preferred)
Specialist office visits (Includes all other provider designations) CT scans, MRIs, MRAs, PET scans, and cardiac 3 diagnostic procedures utilizing nuclear medicine
(prior authorization is required)
Other outpatient X-ray, pathology and laboratory
(Diagnostic testing by providers other than outpatient laboratory, 3 pathology, and imaging departments of hospitals/facilities)
N/A
(services covered under Blue Shield Preferred)
Allergy Testing and Treatment Benefits Office visits (includes visits for allergy serum injections) Preventive Health Benefits Preventive Health Services (As required by applicable federal
law.)
$20 per visit No Charge
20% No Charge
(Not subject to the Calendar Year-Deductible)
50% 50%
OUTPATIENT SERVICES Hospital Benefits (Facility Services)
Outpatient surgery performed at an Ambulatory Surgery 3, 4 Center Outpatient surgery in a hospital Outpatient Services for treatment of illness or injury and necessary supplies (Except as described under "Rehabilitation
benefits" and "Speech therapy benefits")
N/A
(services covered under Blue Shield Preferred)
20% 20% 20% 20%
50% 50% 50% 50%
$100 per surgery $20 per visit $20 per visit
CT scans, MRIs, MRAs, PET scans, and cardiac diagnostic procedures utilizing nuclear medicine 3 performed in a hospital (prior authorization is required) Other outpatient X-ray, pathology and laboratory 3 performed in a hospital Bariatric Surgery (prior authorization required by the Plan; medically
necessary surgery for weight loss, for morbid obesity only)
6
$20 per visit $100 per surgery
20% 20%
50%
HOSPITALIZATION SERVICES Hospital Benefits (Facility Services) Inpatient Physician Services
No Charge $250 per admission $250 per admission
20% 20% 20%
50% 50% 50%
7 7 7
Inpatient Non-emergency Facility Services (semi-private
room and board, medically necessary services and supplies) Bariatric Surgery (prior authorization required by the Plan; medically 6 necessary surgery for weight loss, for morbid obesity only)
5
Skilled Nursing Facility Benefits
(Combined maximum of up to 100 prior authorized days per calendar year; semi-private accommodations)
Services by a free-standing Skilled Nursing Facility Skilled Nursing Unit of a Hospital
N/A
(services covered under Blue Shield Preferred)
20% 20%
50% 50%
N/A
(services covered under Blue Shield Preferred)
EMERGENCY HEALTH COVERAGE
Emergency room Services not resulting in admission (ER
facility copay does not apply if the member is directly admitted to the hospital for inpatient services)
$100 per visit
(Not subject to the Calendar Year-Deductible)
$100 per visit
(Not subject to the Calendar Year-Deductible)
$100 per visit
(Not subject to the Calendar Year-Deductible)
Emergency Room Services resulting in admission (When
the member is admitted directly from the ER)
$250 per admission 20% $20 per visit
$250 per admission 20% 20%
$250 per admission 20% 50%
Emergency room Physician Services Urgent Care Benefits Urgent care services (For urgent care services performed at a
center affiliated with a licensed hospital please refer to the Emergency Room services.)
AMBULANCE SERVICES
Emergency or authorized transport
N/A
(services covered under Blue Shield Preferred)
20%
20%
PRESCRIPTION DRUG COVERAGE Outpatient Prescription Drug Benefits A description of your outpatient prescription drug coverage is provided separately. If you do not have the separate drug summary that goes with this benefit summary, please contact your benefits administrator or call Customer Service. N/A
(services covered under Blue Shield Preferred)
PROSTHETICS/ORTHOTICS
Prosthetic equipment and devices (Separate office visit copay
may apply)
20% 20%
50% 50%
Orthotic equipment and devices (Separate office visit copay may
apply.)
N/A
(services covered under Blue Shield Preferred)
DURABLE MEDICAL EQUIPMENT
Durable Medical Equipment Breast Pump
N/A
(services covered under Blue Shield Preferred)
20%
50% Not Covered
N/A
(services covered under Blue Shield Preferred)
No Charge
(Not subject to the Calendar Year-Deductible)
MENTAL HEALTH SERVICES (PSYCHIATRIC)
Inpatient Hospital Services Outpatient Mental Health Services
9
Carved out to Optum
CHEMICAL DEPENDENCY SERVICES
Chemical Dependency and Substance Abuse Services
10
Carved out to Optum
10
HOME HEALTH SERVICES
visits per Calendar Year)
11
Home health care agency Services
(up to 100 prior authorized
N/A
(services covered under Blue Shield Preferred)
20% 20%
50% 50%
Home infusion/home intravenous injectable therapy and infusion nursing visits provided by a Home Infusion Agency
N/A
(services covered under Blue Shield Preferred)
10
OTHER Hospice Program Benefits Routine home care
10
N/A
(services covered under Blue Shield Preferred)
20% 20% 20% 20%
50% 50% 50% 50%
10
Inpatient Respite Care 24-hour Continuous Home Care General Inpatient care
11
N/A
(services covered under Blue Shield Preferred)
10
N/A
(services covered under Blue Shield Preferred)
10
N/A
(services covered under Blue Shield Preferred)
10
Chiropractic Benefits
Chiropractic services provided by a chiropractor
(Up to 24 visits per calendar year combined with acupuncture visits)
11
N/A
(services covered under Blue Shield Preferred)
20%
Not Covered
Acupuncture Benefits
Acupuncture services
(Up to 24 visits per calendar year combined with chiropractic services)
N/A
(services covered under Blue Shield Preferred)
20%
20%
Pregnancy and Maternity Care Benefits Prenatal and Postnatal Physician Office Visits
(For inpatient hospital services, see "Hospitalization Services.")
$20 initial visit only No Charge No Charge
20%
14
50%
14
Family Planning 12 Counseling and consulting
No Charge
(Not subject to the Calendar Year-Deductible)
50% 50% 50% 50% 50% 50% 50% 50%
Tubal ligation
13
No Charge
(Not subject to the Calendar Year-Deductible)
Elective abortion 20% 8 Vasectomy 20% Rehabilitation Benefits (Physical, Occupational and Respiratory Therapy) Outpatient visits (Office or outpatient facility location) $20 per visit Speech Therapy Benefits Outpatient visits ( Office or outpatient facility location) Diabetes Care Benefits Devices, equipment, and non-testing supplies (For testing
supplies, please see "Outpatient Prescription Drug Coverage Summary.") Diabetes self-management training (If billed by your provider, you will also be responsible for the office visit copayment)
13
20% 20% 20% 20% 20% 20%
$20 per visit 20% $20 per visit
Care Outside of Plan Service Area Within US: BlueCard Program
Outside of US: BlueCard Worldwide
All covered services provided through BlueCard Program, for out-ofstate emergency and non-emergency care, are provided at the preferred level of the local Blue Plan allowable amount when you use a Blue Cross/BlueShield provider. All covered services for emergency and non-emergency care will be eligible for reimbursement when received outside of the US. Please refer to the Blue Shield Preferred Tier for covered services and corresponding member liability.
2 3
4 5 6
Member is responsible for copayment in addition to any charges above allowable amounts. The copayment percentage indicated is a percentage of allowable amounts. Preferred providers accept Blue Shield's allowable amount as full payment for covered services. Non-preferred providers can charge more than these amounts. When members use non-preferred providers, they must pay the applicable copayment plus any amount that exceeds Blue Shield's allowable amount. Charges above the allowable amount do not count toward the calendar-year deductible or copayment maximum. Preferred Deductible does apply toward the Preferred calendar-year copayment maximum. Please refer to the Plan Contract for exact terms and conditions of coverage. Participating non Hospital based ("freestanding") outpatient X-ray, pathology and laboratory facilities centers may not be available in all areas. Regardless of their availability, you can obtain outpatient X-ray, pathology and laboratory services from a hospital or an ambulatory surgery center affiliated with a hospital, with payment according to your health plan's hospital services benefits. Participating ambulatory surgery facilities centers may not be available in all areas. Regardless of their availability, you can obtain outpatient surgery services from a hospital or an ambulatory surgery center affiliated with a hospital with payment according to your health plan's hospital services benefits. The maximum allowed charges for non-emergency surgery and services performed in a non-participating Ambulatory Surgery Center or outpatient unit of a nonpreferred hospital is $350 per day. Members are responsible for 50% of this $350 per day, plus all charges in excess of $350. Bariatric surgery is covered when pre-authorized by the Plan. However, for members residing in Imperial, Kern, Los Angeles, Orange, Riverside, San Bernardino, San Diego, Santa Barbara and Ventura Counties ("Designated Counties"), bariatric surgery services are covered only when performed at designated contracting bariatric surgery facilities and by designated contracting surgeons; coverage is not available for bariatric services from any other preferred provider and there is no coverage for bariatric services from non-preferred providers. In addition, if prior authorized by the Plan, a member in a Designated County who is required to travel more than 50 miles to a designated bariatric surgery facility will be eligible for limited reimbursement for specified travel expenses for the member and one companion. Refer to the
7 8 9 10 11 12 13 14
Plan Contract for further benefit details. The maximum allowed charges for non-emergency hospital services received from a non-preferred hospital is $600 per day. Members are responsible for 50% of this $600 per day, plus all charges in excess of $600 per day. If the procedure is performed in a facility setting (hospital or outpatient surgery center), an additional facility copayment may apply. Inpatient services for acute detoxification are covered under the medical benefit; see hospitalization services for benefit details. Services for medical acute detoxification are accessed through Blue Shield using Blue Shield's preferred providers or non-preferred providers. When these services are pre-authorized, the member pays the Preferred Provider copayment. For plans with a calendar-year medical deductible amount, services with a day or visit limit accrue to the calendar-year day or visit limit maximum regardless of whether the plan medical deductible has been met. Includes insertion of IUD, as well as injectable and implantable contraceptives for women. Copayment shown is for physician's services. If the procedure is performed in a facility setting (hospital or outpatient surgery center), an additional facility copayment may apply. For pregnancy and maternity at the Preferred and Non-Preferred level payment noted is for the global pregnancy bill. Plan designs may be modified to ensure compliance with federal requirements.
ASO RO 092713
You might also like
- Yang Forwards COO Nava On SpywareDocument7 pagesYang Forwards COO Nava On SpywareChris NewfieldNo ratings yet
- Gov. Brown UC Regents Proposal: Nov. 19, 2014Document1 pageGov. Brown UC Regents Proposal: Nov. 19, 2014John MyersNo ratings yet
- Health Retiree Insurance From Berkeley Emeriti Association December 2013Document1 pageHealth Retiree Insurance From Berkeley Emeriti Association December 2013Chris NewfieldNo ratings yet
- Specialty Drugs UCOP2 Union 26 August 2014Document1 pageSpecialty Drugs UCOP2 Union 26 August 2014Chris NewfieldNo ratings yet
- Illinois Chicago Letter Protests Cluster CancellationDocument6 pagesIllinois Chicago Letter Protests Cluster CancellationChris NewfieldNo ratings yet
- UC Berkeley Dean Letter Reinstating Palestine CourseDocument3 pagesUC Berkeley Dean Letter Reinstating Palestine CourseChris NewfieldNo ratings yet
- Jess Mckillop Media Coverage KillersDocument15 pagesJess Mckillop Media Coverage KillersChris NewfieldNo ratings yet
- UCOP Letter To UCSB Chair Bhavnani UC Care Petition Oct 2013 PDFDocument2 pagesUCOP Letter To UCSB Chair Bhavnani UC Care Petition Oct 2013 PDFChris NewfieldNo ratings yet
- MOOC Bill Amended (CA SB 520 April-May 2013)Document3 pagesMOOC Bill Amended (CA SB 520 April-May 2013)Chris NewfieldNo ratings yet
- UCLA MOOC Summit Jan 2013 Revised TranscriptDocument33 pagesUCLA MOOC Summit Jan 2013 Revised TranscriptChris NewfieldNo ratings yet
- UC Care Tier2 Providers Health InsuranceDocument8 pagesUC Care Tier2 Providers Health InsuranceChris NewfieldNo ratings yet
- White Paper Tech Transfer 2002Document97 pagesWhite Paper Tech Transfer 2002Chris NewfieldNo ratings yet
- Statement PowellDocument2 pagesStatement PowellChris NewfieldNo ratings yet
- February 15, 2008: Mark Yudof, "Are University Systems A Good Idea?"Document4 pagesFebruary 15, 2008: Mark Yudof, "Are University Systems A Good Idea?"Chris NewfieldNo ratings yet
- June 17, 2009: Mark Yudof On Furlough OptionsDocument6 pagesJune 17, 2009: Mark Yudof On Furlough OptionsChris NewfieldNo ratings yet
- Yudof at KPCC 3systems Summit Jan 13Document9 pagesYudof at KPCC 3systems Summit Jan 13Chris NewfieldNo ratings yet
- Jan 11, 2002: Mark Yudof, "Is The Public Research University Dead?"Document4 pagesJan 11, 2002: Mark Yudof, "Is The Public Research University Dead?"Chris NewfieldNo ratings yet
- May 13, 1992, Mark Yudof, "The Burgeoning Privatization of State Universities"Document5 pagesMay 13, 1992, Mark Yudof, "The Burgeoning Privatization of State Universities"Chris NewfieldNo ratings yet
- Yudof To UC Regents On 2012-13 BudgetDocument3 pagesYudof To UC Regents On 2012-13 BudgetChris NewfieldNo ratings yet
- March 12, 2004: Mark Yudof, " "What If The Yankees Were Run Like A Public University?"Document8 pagesMarch 12, 2004: Mark Yudof, " "What If The Yankees Were Run Like A Public University?"Chris NewfieldNo ratings yet
- Prof Watson To Yudof On Humanities in U BudgetsDocument7 pagesProf Watson To Yudof On Humanities in U BudgetsChris NewfieldNo ratings yet
- Mark Yudof To UC Community On Campus ClimateDocument2 pagesMark Yudof To UC Community On Campus ClimateChris NewfieldNo ratings yet
- June 17, 2009: Mark Yudof On Furlough OptionsDocument6 pagesJune 17, 2009: Mark Yudof On Furlough OptionsChris NewfieldNo ratings yet
- Yudof To Chronicle of HIgher Education On UCLA Prof's CritiqueDocument6 pagesYudof To Chronicle of HIgher Education On UCLA Prof's CritiqueChris NewfieldNo ratings yet
- ACLU Letter To UC Berkeley Police Review BoardDocument4 pagesACLU Letter To UC Berkeley Police Review BoardChris NewfieldNo ratings yet
- Drop Charges Nov 9 Berkeley Councilmember WorthingtonDocument5 pagesDrop Charges Nov 9 Berkeley Councilmember WorthingtonChris NewfieldNo ratings yet
- Academic Senate Budget Overview: Presented To The Regents May 17, 2007Document16 pagesAcademic Senate Budget Overview: Presented To The Regents May 17, 2007Chris NewfieldNo ratings yet
- June 30, 2009 Yudof To UCLA Faculty AssnDocument2 pagesJune 30, 2009 Yudof To UCLA Faculty AssnChris NewfieldNo ratings yet
- Butler and Simon Comment On Nov 9 To Police Review BoardDocument23 pagesButler and Simon Comment On Nov 9 To Police Review BoardChris NewfieldNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
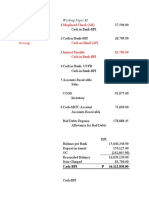
- Test Ii: Misplaced Check (AR)Document10 pagesTest Ii: Misplaced Check (AR)Hannaniah PabicoNo ratings yet
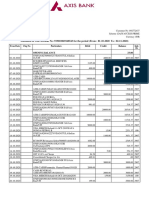
- Statement of Axis Account No:919010069168543 For The Period (From: 01-10-2020 To: 02-11-2020)Document2 pagesStatement of Axis Account No:919010069168543 For The Period (From: 01-10-2020 To: 02-11-2020)minniNo ratings yet
- Draft Guidelines For Issuance and Operation of Prepaid Payment Instruments in IndiaDocument12 pagesDraft Guidelines For Issuance and Operation of Prepaid Payment Instruments in IndiaSidharath GautamNo ratings yet
- HPCN QBDocument14 pagesHPCN QBArvNo ratings yet
- Lenovo Cashback Offer T&CsDocument3 pagesLenovo Cashback Offer T&CsChiragNo ratings yet
- Client Relationship Summary CRSDocument4 pagesClient Relationship Summary CRSTrish HitNo ratings yet
- Case Study RaghavDocument9 pagesCase Study RaghavrahultripathivnsNo ratings yet
- Peer Educators AllowanceDocument4 pagesPeer Educators AllowanceKealeboga Duece ThoboloNo ratings yet
- Company Profile 2020Document29 pagesCompany Profile 2020adityaNo ratings yet
- Audit Report 2020 2021Document18 pagesAudit Report 2020 2021SHIKHA SHARMANo ratings yet
- PNL PAB181Document8 pagesPNL PAB181NIRANJAN KUMARNo ratings yet
- Soal Latihan GMDSSDocument69 pagesSoal Latihan GMDSSRudi Anton SinagaNo ratings yet
- Module 3Document127 pagesModule 3nidhi goelNo ratings yet
- Mental Health Nursing R ShreevaniDocument3 pagesMental Health Nursing R ShreevaniBalwant SinghNo ratings yet
- 空白信用证版本Document5 pages空白信用证版本ansontzengNo ratings yet
- List of The Placement Consultants Consultant LocationDocument63 pagesList of The Placement Consultants Consultant LocationAnuth SiddharthNo ratings yet
- Hospital Management Information System ProjectDocument4 pagesHospital Management Information System ProjectAlfredo Jimenez CharlesNo ratings yet
- Talk+Up+Xfinity!+ +Job+AidDocument2 pagesTalk+Up+Xfinity!+ +Job+AidDaniel Rafael Dominuez AlfaroNo ratings yet
- Mcis - GSCDocument1 pageMcis - GSCPachaippan PachaiNo ratings yet
- Cyber Security Global Information InfrastructureDocument7 pagesCyber Security Global Information InfrastructureonesnoneNo ratings yet
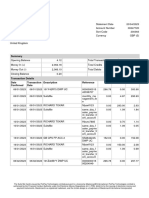
- Statement 2023 01 06 2023 04 20Document2 pagesStatement 2023 01 06 2023 04 20Avtar SNo ratings yet
- SDX 6000 SeriesDocument6 pagesSDX 6000 SeriesHakob DadekhyanNo ratings yet
- Basic Bank Documents and TransactionDocument25 pagesBasic Bank Documents and TransactionJoselyn Amon100% (1)
- Transportation and Public Service Law 2020.A PrelimDocument100 pagesTransportation and Public Service Law 2020.A PrelimRoland Ron Bantilan100% (1)
- Invoice August 2017-1743413Document1 pageInvoice August 2017-1743413Anthony ArmstrongNo ratings yet
- The Network Core: - Mesh of Interconnected RoutersDocument42 pagesThe Network Core: - Mesh of Interconnected RoutersĐào Quỳnh NhưNo ratings yet
- E MarketingDocument71 pagesE MarketingMUFADDAL SUTERWALANo ratings yet
- MGT 101 100% GuessDocument9 pagesMGT 101 100% GuessBint e HawaNo ratings yet
- Nigeria SAS 10 and New Prudential GuidelinesDocument21 pagesNigeria SAS 10 and New Prudential GuidelinesOuedraogo AzouNo ratings yet
- SAP International Financial Reporting Standards (IFRS)Document20 pagesSAP International Financial Reporting Standards (IFRS)yuryu100% (4)