Professional Documents
Culture Documents
SC 199492 A
Uploaded by
Ananda AwaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SC 199492 A
Uploaded by
Ananda AwaCopyright:
Available Formats
Paraplegia 32 (1994) 583-587 1994 International Medical Society of Paraplegia
Analyses of 94 consecutive spinal cord injury patients using ASIA
defnition and modifed Frankel score classifcation
M Capaul MD, 1 H Zollinger MD, 1 N Satz MD, 1 V Dietz MD, 1 D Lehmann MD, 2
B Schurch MDI
J Department of Orthopedics and Swiss Paraplegic Center, University Hospital Balgrist,
Zurich, Forchstrasse 340, 8008 Zurich, Switzerland; 2 Department of Neurology,
University Hospital, Zurich, Switzerland.
Serial neurological examinations were analysed on 94 consecutive spinal cord
injury (SCI) patients admitted for rehabilitation to the Swiss Paraplegic Center
at the Clinic Balgrist Zurich, Switzerland, between 1987 and 1992. Patients' data
were examined adopting ASIA and modified Frankel definitions in order to
compare the two classifications in terms of consistency and prognostic value.
The modified Frankel definition was subdivided into five categories (A, B, C, D
and E). On admission (discharge) 43 (37) patients were classified as Frankel A,
23 (11) patients in group B, 26 (42) patients in group C, 2 (2) patients as
Frankel D and 0 (2) patients in group E. A qualitative analysis of the results on
the base of a maximal score of 100 points (A = 0, B = 25, C = 50, D = 75 and
E = 100 points) suggested a mean score improvement from 21.5 (22.5) to 29.0
(26.3) or 7.5 (7.1), regarding all 94 patients during follow up (admission/
discharge). The median improvement was one modified Frankel grade (A/ to
B/C). No detailed assessments were yielded concerning motor and sensory
functions. Using ASIA definition, a continuous numerical score of motor and
sensory function was observed. Recovery during follow up was determined by
detailed motor and sensory function. For all 94 patients (quadriplegics and
tetraplegics), the average motor recovery according to the ASIA definition was
9.4 (9.6). The mean ASIA motor score improved from 52.2 (17.3) on
admission to 61.6 (17.9) on discharge. Light touch increased by 7.0 (1O.3)
from 72.7 (22.3) to 79.7 (22.7) and pinprick sensory function by 7.1 (13.6)
from 69.2 (21.8) to 76.3 (22.2). Change in status was progressively unidirec
tional using both definitions. Comparing the ASIA guidelines with modified
Frankel classification there was an unambiguous benefit using the new definition
of ASIA, as a gradual change of motor and/or sensory function was more clearly
documented for all cases by ASIA. Using modified Frankel score definition, the
patient's classification may be unchanged, regardless of whether the status
improved or remained stable. This was not the case using ASIA definition. It
was not the intention in this paper to assess and compare the treatment of
acutely spinal cord injured patients by (a) non operative and (b) operative
treatment.
Keywords: modified Frankel score definition; ASIA (American Spinal Injury
Association); spinal cord injury (SCI); ASIA Motor Index Score.
Introduction
During the last 30 years several meetings
have taken place worldwide in order to
Correspondence to Dr Marcel Capaul, Russenweg 18.
CH-8008 Zurich. Switzerland.
elaborate an effective classification of spinal
cord injury. 1 Despite different methods and
proposals no valid solution was agreed
upon.2.3 The modified Frankel score was
preferably used. Using the modified Frankel
score, complete and incomplete spinal cord
584 Capaul et al
injury were subdivided into five categories
(A, B, C, D and E), without yielding
detailed assessments of motor and sensory
function.
Recently the American Spinal Injury
Association (ASIA) worked out a new
classification of spinal cord injury based on
the ASIA Motor Score Index. Motor func
tion, light touch and pinprick sensory func
tion were scored and analysed by a different
points rationing scheme.4
According to the Standards for Neuro
logical Classification published by ASIA,
the term 'complete injury' is used when
there is an absence of sensory and motor
function in the lowest sacral segment; 'in
complete injury' means partial preservation
of sensory and/or motor function below the
neurological level including the lowest
sacral segment. Sacral sensation includes
sensation at the anal mucocutaneus junction
as well as deep anal sensation. The test for
motor function is the presence of voluntary
contraction of the external anal sphincter
upon digital examination.4
In the present paper, the two classifica
tions (ASIA/rankel) were compared and
the patients' data were separately analysed.
Methods and subjects
Serial examinations for motor and sensory
function were performed on 94 consecutive
spinal cord vertebral injury patients ad
mitted for treatment and rehabilitation to
the University Hospital Department of
Orthopedics and Swiss Paraplegic Center
Balgrist, Zurich between 1987 and 1992.
For this study the data on admission and
at discharge were used in order to compare
the definitions of the modified Frankel score
with ASIA classification in terms of consis
tency and prognostic ability. 5 The ASIA
Motor Index Score uses standard manual
muscle testing on a six grade scale (ab
sent = 0; trace = 1, visible or palpable
contraction; poor = 2, active movement
through range of motion with gravidity
eliminated; fair = 3, active movement
through range of motion against gravidity;
good = 4, active movement through range
of motion against resistance; normal = 5;
and NT = not testable). The key muscles/
Paraplegia 32 (1994) 583-587
functions included in the ASIA Motor Index
Score are: elbow flexors, wrist extensors,
elbow extensors, finger flexors, hand in
trinsics, hip flexors, knee extensors, ankle
dorsi fexors , long toe extensors and ankle
plantar fexors, whereas a total motor score
of 100 is possible. The sensory dermatome
chart recommended by ASIA was used.
Light touch and pinprick sensations were
tested for each sensory dermatome and
graded on a three point scale (absent = 0;
impaired = 1; and normal = 2). NT was
used for not testable. Quantitatively a max
imum light touch score of 112, pinprick
score of 112 is possible. Bladder, bowel and
sexual dysfunctions were separately ana
lysed.
For the modified Frankel score,6 a five
scale subdivision was used: A = complete
motor and sensory function disorder; B =
motor complete, sensory incomplete func
tion disorder; C = motor and sensory
incomplete function disorder; D = useful
motor function with or without auxiliary
means; E = no motor or sensory function
disorder.
In order to get a qualitative analysis, a 100
point scale was used (A = 0, B = 25,
C = 50, D = 75 and E = 100 points). By this
means, a patient with complete motor and
sensory function disorder (Frankel A) was
classified with no points, whereas a patient
with, for instance, a complete motor and
sensory function recovery (Frankel E) was
classified with the maximal score of 100
points. Patients were classified on both
scores (ASIA and Frankel) according to
their initial neurological level of injury on
admission and their final condition at dis
charge.
The ASIA Motor Index increase between
initial and final exams was used as an
indicator of motor recovery. The increase
between initial and final light touch and
pinprick scores was used to measure sensory
recovery.
Results
The mean age of all 94 patients on admis
sion was 37. 8 years. Of this population, 21
(22%) of the patients were women and 73
(78%) men. In accordance with the internal
Paraplegia 32 (1994) 583-587
guidelines for spinal cord injury, 28 patients
(30% ) were treated conservatively, while 43
patients (46%) were operated within 24 h
(early decompression) and 23 of the patients
(24 %) underwent surgical treatment later,
after more than 24 h (late decompression).
Without exception, all 94 patients were
hospitalized within 24 h after spinal cord
vertebral injury. All patients were directly
assigned to our clinic, either by ambulance
or aircraft.
Type of vertebral fracture
In 26 cases there was a dislocation of the
vertebral body (25.5%); in 24 cases (27.5%)
a dislocation-fracture; in 22 cases (23%) a
compression-fracture; in 14 cases (15%)
a burst-fracture and in eight cases (9%) a
communited-fracture.
Cause of injury
In 40 patients the cause of acute traumatic
vertebral lesion with consecutive SCI was a
traffic accident; in 23 patients sport acci
dents, in 20 patients work accidents, and in
6 patients attempted suicide were the causa
tive mechanisms. There were five cases of
vague reason.
Level of spinal cord injury
On admission 36 patients (38%) were tetra
plegic and 58 patients (62%) paraplegic. In
12 patients (12.7%) with a diagnosis of
tetraplegia the neurological level most often
affected was C6. In 10 patients (9.4%) with
the diagnosis of paraplegia the correspond
ing neurological injured level was Ll.
Thirty-two patients (94%) having para
plegia were affected between T11 and L2.
No primary spinal cord lesion was found at
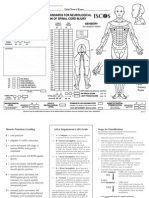
level Cl, C8, T1 and S3-5 (Fig la).
Level of vertebral column injury
In the patients with tetraplegia, the most
frequent affected spine level was C5
(14 patients). L1 was the location most
frequently injured in the 18 patients with
paraplegia. In general the thoracolumbar
junction was the most affected level
of vertebral column injury (25 patients)
(Fig Ib).
a
Spinal cord injury analysis 585
I:: \ \
. .
o 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29
b
20
15
J
,
. 10
/1
5
\ A H
o 1 3 5 7 9 11 13 15 17 19 21 23 25 27
Figure 1 (a) Level of spinal cord injury (30
segments). Cl-8 = 1-8; Tl-12 = 9-20; Ll-5 =
21-25; Sl-5 = 26-30. (b) Level of vertebral
lesion (29 segments). Cl-7 = 1-7; Tl-12 =
8-19; Ll-5 = 20-24; Sl-5 = 25-29. Obviously
there is a strong coincidence between the level
of spinal cord injury (SCI) and the level of
acute traumatic vertebral lesion. Main peaks
are at C6 and L1 in patients having the diag
nosis of tetraplegia and paraplegia respectively.
Neurological results
Frankel score. On admission, 43 patients
were classified as Frankel A, 23 patients as
Frankel B, 26 patients as Frankel C, two
patients as Frankel D and no patient as
Frankel E. At discharge, 37 patients were
still classified as Frankel A (six patients
changed to group B), 11 patients as Frankel
B (18 patients changed to group C), 42
patients as Frankel C (two patients changed
to group D), two patients as Frankel D and
two patients as Frankel E (two new pa
tients). Using the numerical scale of 100
points, there was a mean improvement from
21.5 (22.5) to 29.0 (26.3) or an increase
of 7.5 (7.1) considering all 94 patients.
The median improvement was one modified
Frankel grade (A/ to B/C).
ASIA Motor Index Score. The mean
ASIA motor score on admission of all 94
patients was 52.2 (17.3) and the last follow
up mean score on discharge was 61.6
(17.9) of a maximal score of 100 points.
There was a mean motor point improve
ment of 9.4 (9.6). For paraplegics, the
average motor recovery for all 58 patients,
was 4.9 (6.1), which was numerically less
586 Capaul et at
than the average motor recovery for all
36 quadriplegics 16.9 (11.2). Change in
neurological status of complete or incom
plete functional disorder was progressively
unidirectional, independent of whether con
servative or surgical treatment (early /ate
decompression) was performed. None of
the 66 (70%) operatively treated patients
demonstrated motor point deterioration
postoperatively. According to ASIA
definition 27 of all 58 paraplegics showed a
complete motor function disorder on admis
sion. Two of the 27 patients had changed to
incomplete status on discharge. Twenty
eight out of 36 tetraplegics showed a com
plete motor function disorder on admission.
Seven patients had changed to incomplete
status and 21 patients remained in a status of
complete motor function disorder on dis
charge.
On admission, the average score of pin
prick of all 94 patients was 69.2 (21.8) out
of a maximal 112 points. At discharge 76.3
(22.2) was the mean score, which was an
improvement of 7.1 (13.6). The light
touch score of 72.7 (22.3) improved to a
final score of 79.7 (22.7). There was a
mean increase of 7.0 (1O.3).
Rehabilitation and walking ability. The
quality of rehabilitation was divided into
five categories: 1 = only with wheelchair,
2 = with orthoses, 3 = with a walking stick;
4 = without help; 5 = no problems. At dis
charge 52 patients were able to move only in
a wheelchair; 12 patients used orthoses; 16
patients were using a walking stick; nine
patients could walk sufficiently without any
help; five patients showed absolutely no
walking disability (Fig 2).
Vegetative function disorder (bladder,
bowel and sexual) was found in 80 patients
on admission, and was still present in 67
patients on discharge.
Discussion
Immediately after spinal cord injury, a state
of spinal shock develops which result in
areflexia for varying time periods. A patient
at this time may have no motor or sensory
function below the level of the lesion, but
still regain neurological functions later. 7
The difference observed between the
Paraplegia 32 (1994) 583-587
Figure 2 Rehabilitation outcome. There are
five categories of rehabilitation: 1 = invalid
chair only; 2 = orthoses; 3 = walking stick;
4 = without help; 5 = normal.
Frankel analysis (66 patients with complete
motor function disorder and with complete
or incomplete sensory function disorder (43
Frankel A + 23 Frankel B)) and the ASIA
motor function score (55 patients with com
plete motor function disorder, 27 para
plegics and 28 tetraplegics) on admission, is
due to the more detailed definition of ASIA
to classify motor function disorder. Patients,
e.g. those with only a trace of muscle
contraction in the lowest sacral segment,
were determined, according to ASIA defini
tion, as incomplete motor function disorder;
meanwhile such patients were still classified
in group A or B with complete motor
function disorder, using the modified
Frankel score.
Our study suggests that an accurate classi
fication of recovery of patients with motor
and sensory function disorder is less possible
using the modified Frankel score. The mean
improvement of 7.5 points, from 21.5 to
29.0 points, showed a switch from interval
Frankel A-B to B-C on a 100 point scale,
leading to a hypothetical change of function
disorder of most of the patients (median)
from a motor and sensory complete
(Frankel A) to a motor complete and
sensory incomplete function disorder
(Frankel B). This did not of course corre
spond with the real outcome, as only six
patients left group A to join group B. The
principal change using Frankel score in this
Paraplegia 32 (1994) 583-587
study was the improvement of 18 patients
from group B to Frankel C (motor and
sensory incomplete disorder).
On the contrary, a step-like graduation
was not obvious using the ASIA definition,
as continuous numerical scores of motor and
sensory function were observed. Numeric
ally, nine of all 94 patients (two paraplegics
and seven tetraplegics) changed from com
plete to incomplete motor function dis
order, using ASIA definition. This is con
trary to the modified Frankel definition,
where 18 patients changed from complete to
incomplete motor function disorder (group
B to group C). However, the less detailed
standardisation of modified Frankel defini
tion using manual muscle testings revealed
less accurate and higher result of motor
recovery (complete to incomplete motor
function disorder) than using ASIA defini
tion.
The data referred to the ASIA classifica
tion revealed that, with increasing time after
injury, a persistence of complete injury
progressively diminishes the chance for
motor or/and sensory recovery. Patients in
this series were examined on admission and
on discharge and those having a diagnosis of
complete injury by ASIA definition had a
relatively small amount of motor or sensory
recovery during follow up in comparison to
patients having a diagnosis of incomplete
injury. The individual and gradual change of
motor and sensory function was more
clearly documented for all cases by ASIA,
allowing a more useful and valid system for
References
Spinal cord injury analysis 587
process analysis. Using modified Frankel
score definitions, the patient's classification
may be unchanged, regardless of whether
the status improved or remained stable.
Clear control of outcome was better
assessed by ASIA definition.
The higher increase of total score points
in tetraplegics compared with paraplegics,
having a diagnosis of incomplete injury on
admission, was obvious by counting addi
tively the upper and lower motor function as
a sum, recommended by the definition of
ASIA. A complete recovery in motor
and/or sensory function was only reached by
patients having a minimal neurological le
sion on admission after acute spinal cord
injury.
As documented,S the results of motor and
sensory function tests of spinal cord injury
could be rather inconsistent among exam
iners. As the using of ASIA guidelines
showed, precise evaluation of data is the key
for further elaboration of information and
allows better interpretation of data taken by
serial examinations.
Conclusion
Comparing the ASIA guidelines with the
modified Frankel score there is an unam
biguous benefit using the new classification
of ASIA, provided that the conventions
concerning the neurologic examination and
methods of classifying patients with spinal
cord injury are taken for granted.
1 Lucas 1T. Drucker TB (1979) Motor classification of spinal cord injuries with mobility, morbidity and
recovery indices. Am SlIrg 16: 45: 151-158.
2 Michaelis LS (1968) Discussion on classification of neurological lesions. Paraplegia 6: 46-63.
3 Michaelis LS (1969) International inquiry on neurological terminology and prognosis in paraplegia and
tetraplegia. Paraplegia 7: 1-5.
4 Ditunno 1F, Young W, Donovan WHo Creasey G (1994) The International Standards Booklet for
Neurological and Functional Classification of Spinal Cord Injury. Paraplegia 32: 70-80.
5 Young 1S, Burns PE, Bowen AM, McCutchen R (1982) Spinal cord injury statistics. Good Samaritan
Medical Center, Phoenix.
6 Meinecke FW (1990) Querschnittslahmung. Bestandesaufnahme und Zukunftsaussichten. Springer Verlag.
Berlin. Heidelberg.
7 Guttmann L (1963) Initial treatment of traumatic paraplegia and tetraplegia. In: Harris P. editor.
Symposium on Spinal Injuries. R Coli Surg Edinburgh: 80-92.
8 Donovan WH, Wilkerson MA. Rossi D et al (1990) A test of the ASIA guidlines for classification of spinal
cord injury. Neural Rehabil 4: 39-53.
You might also like
- Tryout UkdiDocument1 pageTryout UkdiAnanda AwaNo ratings yet
- Isncsci Exam Sheet r4Document2 pagesIsncsci Exam Sheet r4akhmadukiNo ratings yet
- Vital SignDocument6 pagesVital SignAlexanderbudi123No ratings yet
- Testicular CancerDocument50 pagesTesticular CancerMuhammad Ikhwan ZainNo ratings yet
- Normal ValuesDocument6 pagesNormal ValuesMc Crister SilangNo ratings yet
- HTTPDocument1 pageHTTPAnanda AwaNo ratings yet
- HTTPDocument1 pageHTTPAnanda AwaNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Objective Assessment of Spinal Cord InjuryDocument25 pagesObjective Assessment of Spinal Cord InjuryYangNo ratings yet
- Dwnload Full Paramedic Care Principles Practice Volume 5 5th Edition Bledsoe Test Bank PDFDocument36 pagesDwnload Full Paramedic Care Principles Practice Volume 5 5th Edition Bledsoe Test Bank PDFresegluerud59d100% (12)
- Rehabilitation Strategies After Spinal Cord InjuryDocument17 pagesRehabilitation Strategies After Spinal Cord Injuryhanna.oravecz1No ratings yet
- Spine TraumaDocument96 pagesSpine TraumaSherlockHolmesSezNo ratings yet
- ShockDocument25 pagesShockMohammad Ali Al-garniNo ratings yet
- Exception Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical SpineDocument29 pagesException Include Burst # of Spine, Some Lateral Wedge # and Extension Injuries of Cervical Spinebhavesh jain100% (2)
- Spinal Cord Syndrome Case PresentationDocument53 pagesSpinal Cord Syndrome Case PresentationPermata GBKP Runggun SurabayaNo ratings yet
- Musculoskeletal Problems Rev 11.21.07Document191 pagesMusculoskeletal Problems Rev 11.21.07jeshemaNo ratings yet
- Spinal Immobilisation or TraumaDocument20 pagesSpinal Immobilisation or Traumaeli romeroNo ratings yet
- Sci RehabDocument45 pagesSci RehabkaushikawebNo ratings yet
- Spinal Cord InjuryDocument52 pagesSpinal Cord Injurynur muizzah afifah hussinNo ratings yet
- Spinal Cord Injury....Document44 pagesSpinal Cord Injury....PrabhuswamyChowdiah75% (4)
- Chikuda 2021 Oi 210953 1639158704.75905Document13 pagesChikuda 2021 Oi 210953 1639158704.75905Neda PiratvisuthNo ratings yet
- 7721 (25) NeurotraumaDocument72 pages7721 (25) NeurotraumanewazNo ratings yet
- TRAUMA MCQs PDFDocument7 pagesTRAUMA MCQs PDFEslam Kandil75% (8)
- GPC Fractura VertebralDocument44 pagesGPC Fractura VertebralEdgar Vargas GranadosNo ratings yet
- Neurogenic ShockDocument10 pagesNeurogenic ShockHamza IshtiaqNo ratings yet
- UntitledDocument544 pagesUntitledyenaxoNo ratings yet
- Aaos Spine 2020.Document71 pagesAaos Spine 2020.ABUBAKER ZANBOUZINo ratings yet
- Care For Spinal ImobilizationDocument20 pagesCare For Spinal ImobilizationRhyal MudatsirNo ratings yet
- Boquecosa Nursing Review ReviewerDocument19 pagesBoquecosa Nursing Review ReviewerElay PedrosoNo ratings yet
- Fitness Choices and First Aid Study NotesDocument11 pagesFitness Choices and First Aid Study NotesAlan VanNo ratings yet
- Spinal Cord Injuries (SCI) : DR - Anas AlashramDocument80 pagesSpinal Cord Injuries (SCI) : DR - Anas AlashramMarah AbdulrahimNo ratings yet
- Nervous System Disorders Lecture Notes 6 - 7 - 20Document31 pagesNervous System Disorders Lecture Notes 6 - 7 - 20Cynthia FloresNo ratings yet
- Therapeutic Positions For PatientDocument18 pagesTherapeutic Positions For PatientJordanBangot100% (2)
- Motorcycle Helmets Associated With Lower Risk of Cervical Spine Injury: Debunking The MythDocument6 pagesMotorcycle Helmets Associated With Lower Risk of Cervical Spine Injury: Debunking The MythshishichanNo ratings yet
- SLICS Classification DetailedDocument7 pagesSLICS Classification DetailedOj AlimbuyuguenNo ratings yet
- CPG Pressure UlcerDocument104 pagesCPG Pressure Ulcerharfi100% (1)
- Prehospital Emergency Care 11th Edition 11th EditionDocument61 pagesPrehospital Emergency Care 11th Edition 11th Editionmarion.wade94398% (42)
- Brain-Spine Interface Allows Paralysed Man To Walk Using His ThoughtsDocument4 pagesBrain-Spine Interface Allows Paralysed Man To Walk Using His ThoughtsalumnogustaNo ratings yet