Professional Documents
Culture Documents
53 Sultan Ayaz (Scabies) JMPR 10 842
53 Sultan Ayaz (Scabies) JMPR 10 842
Uploaded by
M.Akram TatriOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
53 Sultan Ayaz (Scabies) JMPR 10 842
53 Sultan Ayaz (Scabies) JMPR 10 842
Uploaded by
M.Akram TatriCopyright:
Available Formats
Journal of Medicinal Plants Research Vol. 5(24), pp. 5706-5712, 30 October, 2011 Available online at http://www.academicjournals.
org/JMPR ISSN 1996-0875 2011 Academic Journals
Full Length Research Paper
ScaNeem: Herbo-mineral therapy for scabies
Sultan Ayaz, Abdul Hannan, Khan Usmanghani, Halima Nazar, E. Mohiuddin, M. Akram* and M. Ibrahim Khan
Faculty of Eastern Medicine, Hamdard University, Karachi, Pakistan.
Accepted 6 October, 2011
A study was conducted to determine the efficacy and safety of herbal coded medicine, ScaNeem, for the treatment of scabies. Open randomized descriptive study was employed in this study. The drug ScaNeem was prescribed to 60 patients while benzyl benzoate was prescribed to 60 patients who were registered at Shifa Ul Mulk Memorial Hospital. They all belong to villages around Hamdard University and urban population of Gadap Town area. The age range of patients was 10 to 50 years. The response of the treatment on symptomatology of scabies was analysed. ScaNeem was found to be an economical, safe and effective drug for scabies treatment and was statistically significant at p<0.03. Key words: Scabies, ScaNeem, benzoyl benzoate, clinical trial, efficacy. INTRODUCTION The skin is susceptible to many diseases and disorders. Skin disorders have a wide range of etiologies, including infection such as scabies (Chosidow, 2006). Scabies is a contagious dermatitis of human caused by the itch mite Sarcoptes scabiei var. hominis (hering), transmitted by close contact and characterized by papular eruption over tiny raised sinus burrows, produced by digging into the upper layer of the epidermis by the egg female mite, which is accompanied by intense purities (Johnston and sladden, 2005). The most common locations for scabies are on the sides of fingers, between the fingers, on the backs of the hands, on the wrists, heels, elbows, armpits, inner thighs and around the waist (belt line) (Walton et al., 2004). Scabies spreads rapidly under crowded conditions where there is frequent skin-to-skin contact between people, such as in hospitals, institutions, childcare facilities, and nursing homes (Hengge, 2006). Pimple-like irritations, burrows or rash of the skin, especially the webbing between the fingers; the skin folds on the wrist, elbow, or knee, the penis, the breast, or shoulder blades. Intense itching, especially at night and over most of the body. Sores on the body caused by scratching. Scabies burrows appear as tiny grey irregular tracks between the fingers and on the wrists (Arlian et al., 1984). They may also be found in armpits, buttocks, on the penis, insteps and backs of the heels. Microscopic examination of the contents of a burrow may reveal mites, eggs or mite feaces (scybala).
MATERIALS AND METHODS Study design It is a case control direct unicenter prospective randomized authentic allopathic control two arm parallel group clinical trial. Subjects Patients were of both genders (>10 years and <50 years) with clinical diagnosis of scabies. Sample sizes for this study included from ScaNeem a total of 60 and benzyl benzotae a total of 60 subjects were registered and treated. Setting Shifa-ul-Mulk Memorial Hospital for Eastern Medicine, Hamdard University, Gadap Town, Karachi that is surrounded by villages and the urban vicinity scenario. ScaNeem formulation Neem leaves (50 g) were dried under shade and left for 15 days at room temperature then it was powdered with grinder machine and this powder was sifted through sieve number (100) as micronized fine powder. Then the leaves were dissolved in olive oil and this was boiled at 100 C for one hour and left for three days to soak completely. Then the oil was filtered through filter paper. There after sulphur sublimate (50 g) borax powder 50 g and zinc oxide (50 g) were passed through sieve number (100) so as to give
*Corresponding author. E-mail: makram _0451@ hotmail.com.
Ayaz et al.
5707
micronized fine powder. The neem extracted oil (50 ml) was mixed with sulphur sublimate 50 g, broax powder 50 g and zinc oxide 50 g were mixed with vaslien 1000 g to form a homogenous ointment designated as ScaNeem ointment for the treatment of scabies. Inclusion criteria
7. Entire slide methodically was examined under low power (2.5-4x) and then at 25-50x magnification. Microscopic examination of the skin scrapings was then performed at Shifa ul-Mulk Memorial Hospital, the cover slip was secured to the slide at all edges with clear nail polish was subjected to screening. Statistical analysis
The cases of patients suffering from only scabies were selected, patients between 10 to 50 years of age, patients having no obvious pathological finding on routine examination, patients living in Karachi, Pakistan, and all socioeconomic classes including lower, middle and upper class .
Statistical analysis were performed using SPSS in cooperation with Mr. Syed Tashfeen Akhtar Takaful Pakistan Ltd. using excel software, the Chie Square Test was employed. The significant result with p-value less then 0.05 was defined as statistically significant.
Exclusion criteria Chronic and secondary infectious cases were excluded, Patients with concurrent physical illness, for example uncontrolled hypertension, diabetes mellitus, complications of chronic fever, bleeding disorders, patients having hyperpyrexia (103 F or more), patients with renal and hepatic impairment or any cardiac disorder, patient having history of adverse reactions to any of the study drugs or contraindicated for their use. All the patients gave verbal or written, informed consent for their participation and the protocol was approved by the appropriate independent ethics committee of Faculty of Eastern Medicine, Hamdard University, Karachi. Application Patients were advised to have their bath at night with dettol soap and apply the ScaNeem ointment all over the body parts infected with scabies at night below the neck and face. This procedure was repeated for 2 to 3 days. Procedure The patient skin was observed with a magnifying lens and look for lesions suggestive of scabies infestation. The shoulders, back, abdomen, hands, wrists, elbows, buttocks, axilla, knees, thighs and breasts are common sites for burrows. 1. The hand magnifying lens was used to identify recent burrows or papules. A bright light and magnifying lens assisted in visualizing the tiny dark speck (the mite) at the end of the burrow. 2. These high yield lesions were identified by applying mineral oil (best used over dry scaly areas) or by applying the burrow ink test to possible burrows. The burrow ink test was done by using a wide felt tip pen (blue or green are best) over burrows and then wiped off with an alcohol swab. The alcohol removed most surface ink, but the ink was not removed but taken up by the burrow, thus leaving a dark irregular line. 3. The mineral oil or preferably microscope immersion oil was applied to lesions or scalpel blade and glass slides. 4. Non-excoriated, non-inflamed areas were scrapped (burrows and papules) vigorously with a #15 scalpel blade or glass slide held at a 90 angle to the skin, while holding the skin tight, until the stratum corneum was removed. The blades or curettes between scrapings on different persons were changed. Blade was placed on and removed from the handle with a forceps. Used blades were placed in a sharps container. 5. The skin scrapings were transferred from at least 6 different sites to a single slide or to separate slides. These scrapings was then pushed onto the slide edge and then moved to the center of the slide. 6. The cover slip was placed over the slide.
RESULTS The intent-to-treat population consisted of 120 patients enrolled: 60 were treated with coded herbal formulation ScaNeem ointment, and 60 were treated with lotion benzyl benzoate. 13 (in test group) and 14 in the (control group) were lost to follow-up and therefore not evaluable. The data collected from 120 patients, 98 male patients (percentage of male is 81.66%) and 22 female patients (percentage of female is 18.33%), were enrolled in the study (Table 1). The demographic and baseline characteristics of the patients included in the groups evaluable for efficacy were found to be similar for the two treatment groups and were comparable to those of the intent-to-treat population as p>0.05. All of the patients recruited in this study were categorized in different class interval ranging from 10 years of age to 50 years of age. All patients had one or more pretreatment symptoms of scabies and local examination of skin which were almost same in both treatment groups as p >0.05 in tables as subsequently mentioned. The most frequent was the itching and Nocturnel pruritis (100%) in both treatment groups as shown in Table 2. The response in sign and symptoms and local examination are recorded as: Skin irritation In skin irritation before treatment, there was no difference between test and control group as shown in Table 2 and after treatment in the test and control group, it was shown that the test group (ScaNeem) has 91% improvement as compared to control (Benzyl benzoate) improvement with 46%. After applying the test of significance, there was significant difference between these two drugs; as such, Chi-Square test was applied and p-value was calculated as 0.006 as shown in Table 3. Skin folds For skin folds before treatment, there was little difference between the test and control group as shown in Table 2
5708
J. Med. Plants Res.
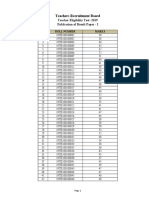
Table 1. Mean distribution by treatment group.
Treatment group Test group
Sex Male Female Total Male Female Total Male Female Total
Mean 25.50 23.61 24.05 16.13 15.98 16.00 22.09 19.56 20.02
Number (n) 46 14 60 52 8 60 98 22 120
Std. Deviation 14.627 12.421 12.864 2.900 6.847 6.444 12.513 10.529 10.907
Control group
Total
Table 2. Baseline scabies history.
Scabies history at baseline No Yes Total No Yes Total No Yes Total No Yes Total Rashes on abdomen and chest Rashes on arms Rashes on arms and abdomen Rashes on arms and chest Rashes on arms and legs Rashes on back and abdomen Rashes on chest Rashes on chest and back Rashes on legs Rashes on legs and abdomen Rashes on legs and back Rashes on legs and chest Total
Skin irritation
Treatment group Control (n = 40) Test (n = 80) 27 36 33 24 60 60 53 7 60 00 60 60 00 60 60 1 1 1 1 41 2 2 2 9 0 0 0 60 59 1 60 00 60 60 00 60 60 2 5 0 0 37 0 1 2 6 4 2 1 60
Total n = 120 63 57 120 112 8 120 00 120 120 00 120 120 3 6 1 1 78 2 3 4 15 4 2 1 120
P value
0.099
Skin fold
0.02
Itching
1.00
Nocturnel pruritis
1.00
Exam of skin
0.05
and after treatment in the test and control group, it was
observed that both the test (ScaNeem) and control
Ayaz et al.
5709
Table 3. Scabies history after treatment.
Treatment response Improved Not improved Total Improved Not improved Total Improved Not improved Total Improved Not improved Total Improved Not improved Total
Skin irritation
Treatment group Control (n = 40) Test (n = 80) 30 (91%) 11 (46%) 03 (9%) 13 (54%) 33 24 07 (100%) 00 (00%) 07 50 (83.33%) 10 (16.67%) 60 50 (83.33%) 10 (16.67%) 60 50 (83.33%) 10 (16.67%) 60 01 (100%) 00 (00%) 01 39 (65%) 21 (35%) 60 39 (65%) 21 (35%) 60 39 (65%) 21 (35%) 60
Total n = 120 41 16 57 08 00 08 89 31 120 89 31 120 89 31 120
P value
0.006
Skin fold
1.00
Itching
0.021
Nocturnel pruritis
0.021
Exam of skin
0.038
(Benzyl benzoate) groups have 100% improvement. After applying the test of significance, there was no significant difference between these two drugs; as such, Chi-Square test was applied and p-value was calculated as 1.00 as shown in Table 3. Itching For itching before treatment, there was no difference between the test and control group as shown in Tables 2 and 3, but after treatment in the test and control group, it was observed that the test group (ScaNeem) has 83.33% improvement as compared to the control (Benzyl benzoate) with 65% improvement. After applying the test of significance, there was significant difference between these two drugs; as such, Chi-Square test was applied and p-value was calculated as 0.021 as shown in Table 3. Nocturnel pruritis
the test of significance, there was significant difference between these two drugs; as such, Chi-Square test was applied and p-value was calculated as 0.021 as shown in Table 3. Examination of skin Examination of the skin showed variation of rashes in different parts of the body such as abdomen, chest, arms, legs and back. The examination of the patients skin at baseline showed that the test and control group exhibited no difference as shown in Table 2 and after treatment in the test and control group, it was observed that the test group (ScaNeem) has 83.33% improvement as compared to the control (Benzyl benzoate) with 65% improvement. After applying the test of significance, there was significant difference between these two drugs; as such, Chi-Square test was applied and p-value was calculated as 0.038 as shown in Table 3. Parasite response
For nocturnel pruritis before treatment, there was no difference between the test and control groups as shown in Table 2 and after treatment in the test and control groups, it was observed that the test group (ScaNeem) has 83.33% improvement as compared to the control (Benzyl benzoate) with 65% improvement. After applying
Clinically, relevant parasite Sarcoptes scabiei skin scraping before treatment with ScaNeem and Benzyl benzoate were found to be similar in both groups as p value 0.107 which is greater than 0.05 in this disease conditions as listed in Table 4.
5710
J. Med. Plants Res.
Table 4. Skin scrapping after treatment.
Parasite status Mite Mite and eggs Mite and mite feacal matter Mite, eggs and mite feacal matter Improved Total
Treatment group Test Control 8 7 9 18 2 7 0 1 41 27 60 60
Total 15 27 9 1 68 120
P value
0.035
Table 5. Side effects on patients self assessment.
Side-effects Burning sensation Skin irritation Skin irritation, burning sensation Skin ulcer No complaints
Treatment group Test Control 0 2 0 2 0 2 0 1 60 53
Total 2 2 2 1 113
P value
0.038
Effects of therapy on scabies Parasitic pathogens were eliminated dramatically in both treatment groups after therapy. The rates of complete elimination of Sarcoptes scabiei clearance were significant in test and control group. In the microscopic evaluable patients, the anti-parasitic success rate at the final visit was significant in test group, and patient in the control group achieving anti-parasitic success with the scabies. Subgroup analysis of anti-parasitic outcome by gender, age, demonstrated comparable results between treatment groups. Eradication rates of selected baseline pathogen (Sarcoptes scabiei) at the final visit are summarized for the parasitic evaluable patients in Table 4. Eradication rates generally were not similar between treatment groups for this pathogen. Similarly, the parasitic clearance response (failure rate) was observed as eradication in the test group and failure in the control group with scabies, but the test group (ScaNeem) success rate was better than that of the Benzyl benzoate that was found with scabies deduced by the p value as 0.035. Clinical success rates with scabies whether present or absent as infection were different in both treatment groups. The cure rates in both treatment groups were fairly reasonable. The clinical success rates in clinically evaluable patients of the two groups were also compared based on parasitic pathogen isolated at registration. Clinical success rates for the two most prevalent typical Sarcoptes scabiei pathogen. Overall clinical success was observed in test group as compared to control group,
however the efficacy of the test treated medication was superior to control group as p value 0.035. In conclusion on the basis of statistical analysis done by Chi Square test null hypothesis is strongly rejected in scabies as p<0.05 as shown in Table 4. Adverse effect profile Drug-related adverse events are summarized in Table 5. Adverse events categorized by the investigator as possibly or definitely drug related were reported nill in patients receiving herbal-o-mineral and in patient administered benzyl benzoate in scabies showed side effect such as burning sensation (02 patients), skin irritation (02 patients), skin irritation and burning sensation (02 patients) and skin ulcer (01 patients) shown in Table 5, were the most common drug-related events among control recipients and no side effects were recorded in test treated recipients. No patient in test or control groups discontinued use of the drug due to side effects. No life threatening side effect recorded in any group. Furthermore, comparison of data recorded by participants relating to these variables showed significant differences between test and control groups (P<0.05) despite of the fact that no side effects were at all recorded in test group. Benzyl benzoate treatment point out that 39 out of 60 showed good response and that long term use was devoid of any side effects. In view of the clinical trial assessment, the ScaNeem ointment
Ayaz et al.
5711
exhibited results which showed that all patients except 04 completely responded to treatment scabies; as such, Sarcoptes scabiei was eliminated. On the basis of statistical findings of all the variables the data offered support to the null hypothesis (when P<0.05), therefore the null hypothesis was rejected. DISCUSSION Health professionals treating scabies face considerable uncertainty as to the most effective and safe topical treatment for scabies. Scabicides which are currently available and in use are benzyl benzoate, crotamiton, malathion and permethrin. Treatment with benzyl benzoate requires repeat applications (Mounsey, 2008). Its use has not been adequately evaluated in randomized control trials, but non-controlled studies indicate cure rates of around 50%. However, resistance is frequent and in addition about a quarter of people treated with benzyl benzoate report a transient burning sensation, itching and dermatitis (Hanna et al., 1978; Burgess et al., 1986). As a corollary the scabies infection is quite prevalent in rural settings in the Gaddap communitys surroundings Hamdard University, Karachi and a study conducted conveniently show that scabies infection contributes as an epidemic spread and it was also cited that scabies diseases have direct relation with water in the vicinity. Therefore, the figures of scabies infection in Pakistan appear to be identical in nature and have been reported earlier in this discussion. A comparative study was conducted for herbal coded formulation ScaNeem ointment with allopathic lotion benzyl benzoate. The present study was undertaken to evaluate the therapeutic effectiveness of these medicinal preparations for scabies. Neem is the traditional examples to control scabies. In a test of 814 / 824 people with scabies, a mixture of neem and turmeric was used to cure 97% of the infected patients. Dr. S. X. Charles at the Medical and Cancer Research and Treatment Center in India sent us the results of a study of 814 people treated with neem and turmeric. Scabies is treated with a scrub bath, boiling the fomites (clothes and bed linens), and application of a paste made by grinding "Fresh Neem leaves and turmeric in the proportion of 4:1 by weight (Sunderktter, 2007). The measurement that is taught to mothers is a handful of neem leaves and a piece of turmeric that equals the length of the index finger. This paste is rubbed all over the body and left to dry. The procedure is repeated daily until the patient is cured. (Boiling clothes and scrub bath is carried out daily before application of the paste). "Paste rubbed on the face has not caused any skin reaction or other toxic symptoms. Of the 824 cases, 98% showed complete cure within 3 to 15 days of treatment. Those cases (95.8%) with localized lesions showed cure in 3 to 5 days. When lesions were all over the body and there
was secondary infection, treatment needed for a cure was 6 to 15 days. Failure of treatment was only 2%. The reasons for failure were irregular application of paste and not doing the preliminary treatment of scrub bath and boiling of fomites to prevent re-infection. The benzyl benzoate 25% is the recommended treatment for all cases. The solution is diluted as follows: Children less than 2 years of age, one part emulsion to three parts water. Children 2 to 10 years of age and adults with sensitive skin, dilute emulsion with equal parts of water. The emulsion should be applied to the whole body including the face and hair, (avoid the mucous membrane of the mouth and genitalia) and left on the body for 24 h before being rinsed off. Five percent sulphur cream 1 applied daily for 2 to 3 days can be used as an alternative for those children less than 2 months of age. Alternatively, 10% crotamiton cream 1 may be applied daily for 3 to 5 days. These agents are less effective and may not be able to cure the ailment. Dermatologists estimate that more than 300 million cases of scabies occur worldwide every year. The condition can strike anyone of any race or age, regardless of personal hygiene. The good news is that with better detection methods and treatments, scabies does not need to cause more than temporary distress. The mite causing the scabies is only 1/60 inch long, and almost impossible to see without magnification. Being a tiny, eight-legged creature with a round body, the mite burrows in the skin, usually on the hands, wrists, ankles, groin, and armpits. Within several weeks, the patient develops an allergic reaction causing severe itching; often intense enough to keep sufferers awake all night. One may have only six or seven scabies mites but be covered with hundreds of itchy spots. The itching areas are an allergic reaction, and no mite can be found in them. Scabies often resemble other rashes. The only way to find out whether one has scabies is to scrape off a piece of skin and examine it under a microscope. Sometimes doctors treat scabies because they suspect it, even though they cannot find the mite. Conclusion It is concluded that ScaNeem is more effective than the benzyl benzoate in the treatment of scabies. ScaNeem herbo-mineral ointment have proved effective against Sarcoptes scabiei. There was no untoward manifestation associated with the use of this medication and it was generally accepted by all treated patients. It has added benefit of safety.
REFERENCES Arlian LG, Runyan RA, Achar S, Estes SA (1984). Survival and infectivity of Sarcoptes scabiei var. canis and hominis. J. Am.
5712
J. Med. Plants Res.
Acad. Dermatol., 11: 210-215. Burgess I, Robinson R, Robinson J (1986). Aqueous malathion 0.5% as a scabicide: Clinical trial, B.M.J., 292: 1172. Chosidow O (2006). Scabies. N. Engl. J. Med., 354(16): 1718-1727. Hanna N, Clay J, Harris J (1978). Sarcoptes scabei infestation treated with malathion liquid. Br. J. Vener. Dis., 54: 354. Hengge UR (2006). Scabies: a ubiquitous neglected skin disease. Lancet Infect. Dis., 6(12): 769-779. Johnston G, Sladden M (2005). Scabies: diagnosis and treatment. B.M.J., 331: 619-622.
Mounsey KE (2008). Scabies: molecular perspectives and therapeutic implications in the face of emerging drug resistance. Future Microbiol., 3(1): 57-66. Sunderktter C (2007). Scabies. J. Dtsch. Dermatol. Ges., 5(5): 424430. Walton SF, Holt DC, Currie BJ, Kemp DJ (2004). Scabies: new future for a neglected disease. Adv. Parasitol., 57: 309-376.
You might also like
- 86-Arshad Original ArticleDocument34 pages86-Arshad Original ArticleM.Akram Tatri100% (1)
- 62 Medicinal Potentials of Alpinia GalangaDocument3 pages62 Medicinal Potentials of Alpinia GalangaM.Akram TatriNo ratings yet
- 60 Paper Published (Premenstrual Syndrome) JMPR 11 1198Document6 pages60 Paper Published (Premenstrual Syndrome) JMPR 11 1198M.Akram TatriNo ratings yet
- 54 Sinusitis (JMPR 11 184sajid Khan)Document9 pages54 Sinusitis (JMPR 11 184sajid Khan)M.Akram TatriNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Beneficiary & Emergency FormDocument2 pagesBeneficiary & Emergency FormreyjornNo ratings yet
- My Buddy: Delhi Public School, GandhinagarDocument54 pagesMy Buddy: Delhi Public School, GandhinagarHimani AggarwalNo ratings yet
- Jurnal Kepimpinan Pendidikan - : Kepuasan Kerja Dan Komitmen Guru Sekolah Menengah Cemerlang Di KelantanDocument14 pagesJurnal Kepimpinan Pendidikan - : Kepuasan Kerja Dan Komitmen Guru Sekolah Menengah Cemerlang Di KelantanNaliny MalaiNo ratings yet
- Spotlight I1 2023Document70 pagesSpotlight I1 2023Raul Alejandro Celis MaturanaNo ratings yet
- Minassian Full Reasons For JudgementDocument69 pagesMinassian Full Reasons For JudgementCityNewsTorontoNo ratings yet
- Atmospheric Pollution and Environmental ChangeDocument209 pagesAtmospheric Pollution and Environmental Changeviqrisyam rizkyNo ratings yet
- Dempsey V RTCDocument7 pagesDempsey V RTCDenise Jane DuenasNo ratings yet
- BA5015-Industrial Relations and Labor WelfareDocument19 pagesBA5015-Industrial Relations and Labor WelfareYamini AshleyNo ratings yet
- Gcse River Study CourseworkDocument7 pagesGcse River Study Courseworkf5dpebax100% (2)
- Cokaliong Shipping vs. UCPBDocument3 pagesCokaliong Shipping vs. UCPBglorybelle01No ratings yet
- PS182 - Terminal Report (1st Q)Document88 pagesPS182 - Terminal Report (1st Q)MarieBalangueNo ratings yet
- PERDEVDocument5 pagesPERDEVlennie cotiocoNo ratings yet
- Manual Stamford Avr SX421 PDFDocument4 pagesManual Stamford Avr SX421 PDFBrooke EdwardsNo ratings yet
- Shiying Sexy Lingerie Co., LTD.: New Items of The Last Two Weeks, Need More Items, Please Visit Our WebsiteDocument5 pagesShiying Sexy Lingerie Co., LTD.: New Items of The Last Two Weeks, Need More Items, Please Visit Our Websiterpnair0% (1)
- Wistia 2021 State of Video ReportDocument31 pagesWistia 2021 State of Video ReportThanh ĐặngNo ratings yet
- Earthquake-Induced Settlement: The Following Notation Is Used in This ChapterDocument27 pagesEarthquake-Induced Settlement: The Following Notation Is Used in This ChapternktanakaNo ratings yet
- Death and The CompassDocument12 pagesDeath and The CompassCrystal BerryNo ratings yet
- X-Seal PS800: Technical Data SheetDocument2 pagesX-Seal PS800: Technical Data SheetdamithNo ratings yet
- 6 - English-How I Taught My Grandmother To Read and Grammar-Notes&VLDocument11 pages6 - English-How I Taught My Grandmother To Read and Grammar-Notes&VLManav100% (3)
- Naval Review Vol XXXIII No 3 - August 1945 (British)Document93 pagesNaval Review Vol XXXIII No 3 - August 1945 (British)Philip Sturtivant100% (2)
- Lunar Code Final LayoutDocument208 pagesLunar Code Final LayoutPhillip LambertNo ratings yet
- Factors Affecting The Germination of Tall Morningglory (Ipomoea Purpurea) - Singh, Megh, Ramirez, Analiza H. M., Sharma, Shiv D., Jhala, Amit J.Document6 pagesFactors Affecting The Germination of Tall Morningglory (Ipomoea Purpurea) - Singh, Megh, Ramirez, Analiza H. M., Sharma, Shiv D., Jhala, Amit J.geraymanNo ratings yet
- ResultPaperI PDFDocument3,868 pagesResultPaperI PDFRavikumarNo ratings yet
- Keynote SpeechDocument9 pagesKeynote SpeechBLP CooperativeNo ratings yet
- TCS New Employee Orientation ProgramDocument8 pagesTCS New Employee Orientation ProgramNeha Chopra0% (2)
- Subsequent Measurement Accounting Property Plant and EquipmentDocument60 pagesSubsequent Measurement Accounting Property Plant and EquipmentNatalie SerranoNo ratings yet
- Earthquake Resistance BuildingDocument11 pagesEarthquake Resistance BuildingAnirudra Sharma100% (1)
- Pcog MnemonicsDocument4 pagesPcog MnemonicsFanBay100% (4)
- (H) - Sem6 - BCH 6.4 (D) - Industrial Relations and Labour Laws - W2 - CG - UNIT 5 - 0Document54 pages(H) - Sem6 - BCH 6.4 (D) - Industrial Relations and Labour Laws - W2 - CG - UNIT 5 - 0sanchiNo ratings yet
- Daikin M Motor - Pumps CatDocument9 pagesDaikin M Motor - Pumps CatOdiin Antonhy MarthNo ratings yet