Professional Documents
Culture Documents
122 PDF
Uploaded by
oopsadhit0 ratings0% found this document useful (0 votes)
14 views2 pagesThe Perioperative use of Ceftriaxone as infection prophylaxis in Neurosurgery: Cranioplasty JPSI 1 (5), Sept - Oct 2012, 27-28 Journal of Pharmaceutical and Scientific Innovation www.jpsionline.com case study.
Original Description:
Original Title
122_pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe Perioperative use of Ceftriaxone as infection prophylaxis in Neurosurgery: Cranioplasty JPSI 1 (5), Sept - Oct 2012, 27-28 Journal of Pharmaceutical and Scientific Innovation www.jpsionline.com case study.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views2 pages122 PDF
Uploaded by
oopsadhitThe Perioperative use of Ceftriaxone as infection prophylaxis in Neurosurgery: Cranioplasty JPSI 1 (5), Sept - Oct 2012, 27-28 Journal of Pharmaceutical and Scientific Innovation www.jpsionline.com case study.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
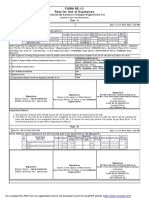
Amer Hayat Khan et al: The Perioperative use of Ceftriaxone in Neurosurgery: Cranioplasty
JPSI 1 (5), Sept Oct 2012, 27-28
Journal of Pharmaceutical and Scientific Innovation
www.jpsionline.com
Case Study
THE PERIOPERATIVE USE OF CEFTRIAXONE AS INFECTION PROPHYLAXIS IN NEUROSURGERY:
CRANIOPLASTY
Amer Hayat Khan*
1
, Andee Dzulkarnaen Zakaria
2
, Syed Azhar Syed Sulaiman
1
, Muhammad Ihtisham Umar
1
,
Nur-Elyana Yazmin Redhuan
1
1
School of Pharmaceutical Sciences Universiti Sains Malaysia, 11800 Penang, Malaysia
2
Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Health Campus, Kelantan, Malaysia
*Email: amerhayat@ymail.com
Received on: 21/07/12 Revised on: 10/08/12 Accepted on: 03/10/12
ABSTRACT
Prophylactic use of antibiotics applied peri or intraoperatively is commonly adopted in many hospitals to decrease the incidence of postoperative infections
following surgery, including neurosurgery. We report a case of a 20 years old young female who undergone cranioplasty. A year earlier, the subject underwent
removal of bone flap after a motor-vehicle-accident. It resulted into the development of a sinking skin flap, insisting a cranioplasty immediately after 6 months
that was delayed, however, for one year. The patient was given a course of antibiotic prophylaxis of IV Ceftriaxone 2gram stat pre-surgery and continued with
IV Ceftriaxone 1 gram for another 2 doses. No infection was developed in the subject several days after the surgical procedure, proving it to be successful. The
current case study encouraged the prophylactic use of antibiotics to prevent sepsis or infections associated with cranial surgeries.
Keywords: Cranioplasty; Ceftriaxone; Infection; Perioperative; Prophylaxis
INTRODUCTION
A surgery is one of the most stressful procedures a patient
could undergo. There are numerous types of surgeries. For
instance, a neurosurgery can either be a craniectomy
(removing a part of the skull), a craniotomy (visualizing and
gaining access to a structure within the cranium) or a
cranioplasty (repairing a cranial defect). According to
William and colleagues, there has always been a high risk of
infections associated with surgical procedures, doubting the
overall success of the otherwise carefully performed
surgeries.
1
Thus, the use of prophylactic antimicrobial drugs,
before and during surgical procedures, becomes imperative to
reduce infection possibility. The protective efficacy of
prophylaxis in clean and contaminated neurosurgical
procedures ranges between 63 and 76 percent.
2
The average
incidences of infections in clean neurosurgical procedure are
varying from 3 to 4 percent, and prevention of infectious
complications is far more practical than treating them.
2
Case Presentation
A 20 years old female was admitted to Hospital Universiti
Sains Malaysia (HUSM) for elective cranioplasty. A year
prior to admission, she sustained an epidural hematoma from
a motor-vehicle-accident and had undergone a craniectomy.
Bearing a severe conditions with a Glasgow Coma Scale
(GCS) score of 6, the patient had a follow up with the
neurologist for last 6 months. Cranioplasty was declared to be
mandatory for the patient by her doctor and was scheduled to
undergo the surgery.
On the day of admission, her vital signs were good, her GCS
score was 15/15 and she had no other medical illness.
Although apparently normal in household work, the patient
was not as much active as she was before the accident,
indicating a consistent underlying illness. She was not taking
any other medication prior to admission and was only allergic
to seafood. She was given a premedication; one dose of
7.5mg of Tablet Midazolam and an intravenous injection of
Ceftriaxone 2g stat for prophylaxis 1 hour prior to surgery.
During the procedure, it was found that the scalp over the
defect was indented. The previous bifrontal incision was then
reopened. Her bone which was preserved was then fixed to
the skull back with 4 sets of craniofix. Culture and sensitivity
swab was taken for analysis prior to surgery. Redivac was
inserted for drainage and the wound was then closed and
dressed.
The patient was then extubate and the GCS was monitored
hourly until the patient became fully conscious. The
intravenous drip continued until the patient could take the
medication orally. The wound was inspected on day 3 and the
stitches were removed on day 7. The Redivac was kept fully
functional for 24 to 48 hours post surgery before it was
removed. The surgery was successful and there was no
complication reported.
Medications of post-surgery:
1. IV Ceftriaxone 1g BD (for another 2 doses)
2. IV Tramadol 50 mg QID (For one week)
Medications for discharged:
1. C. Cloxacillin 500mg QID
2. T. Paracetamol 1g QID
3. Celecoxib 200mg BD
DISCUSSION
Postoperative infection following neurosurgery is a serious
complication which may be life threatening. It can occur in
superficial tissues such as skin surrounding the wound, bone-
flap or in the deeper tissues resulting in meningitis,
encephalitis and brain abscess.
3
It is known that Gram
positive Staphylococci are the most common causative
pathogens for postoperative infections in neurosurgery due to
the contamination from the skin. This comes to the need for
surgical prophylaxis to prevent the postoperative infection
especially in clean operative procedures.
3
Prophylactic use of antibiotics applied peri or intraoperatively
is commonly adopted in many hospitals to decrease the
incidence of postoperative infections following surgery,
including neurosurgery.
4
The patient was given 2 gram stat
dose of IV Ceftriaxone as prophylactic agent followed by
another 2 doses postoperatively. It has been suggested that an
ideal antibiotic regimen for prophylaxis not only should have
effectiveness with thelowest possible risk of adverse
Amer Hayat Khan et al: The Perioperative use of Ceftriaxone in Neurosurgery: Cranioplasty
JPSI 1 (5), Sept Oct 2012, 27-28
reactions, but also have convenience of administeration and
cost-effectiveness, recommending a single-dose
administration in many types of surgery.
5
Ceftriaxone is a 3rd generation cephalosporin with a long
half-life of approximately about 8 hours. As it reaches its
therapeutic concentration, it exhibits a very good penetration
into many tissues and able to cross the blood-brain barrier
even though the meninges are not inflamed. Its concentration
in the CSF is 10-1000 times higher than the MICs for the
majority of potential meningitis pathogenseven 24 h after the
administration of a single dose of approximately 50 mg/kg
body weight.
6
Therefore, perioperative administration of this
antibiotic shortly prior to neurosurgery has been suggested as
an effective agent for postoperative infection prophylaxis.
7
However, there are no published studies involving a
substantial number of patients in the literature.
Even though there is a very low incidence of infection in
clean neurosurgical procedures, which averages 3 to 4
percent, prevention of infectious complications is far more
practical than treating them once they have become
established.
4
In a randomized, controlled trial of antibiotic
prophylaxis in neurosurgery which involves 407 patients
done by Geraghty and Feely (1984) had shown that there is
significant benefit from antibiotic prophylaxis.
6
This is true in
this particular case, which there is no post-surgery
complication of infection and the surgery was considered a
success.
CONCLUSION
Antibiotic prophylaxis significantly reduces the risk of
surgical site infection or sepsis in clean cranial surgeries.
Further studies are recommended to determine the optimum
dose of antibiotic prophylaxis with assessment comparison of
the effectiveness of different antibiotics.
REFERENCES
1. Watters Iii, Baisden WC., Bono J., Heggeness CM., Resnick MH.,
Shaffer WO. et al., Antibiotic prophylaxis in spine surgery: an evidence-
based clinical guideline for the use of prophylactic antibiotics in spine
surgery, The Spine Journal. 2009; 9: 142-6.
2. The perioperative use of ceftriaxone as infection prophylaxis in
neurosurgery. Clinical Neurology and Neurosurgery. 1995; 97: 285 -
289.
3. Shehu BB., Mahmud MR. and Ismail NJ. Neurosurgical
infections.Nigerian Journal of Surgical Research. 2006; 8 (12): 1-18
4. Dipiro JT., Cheung REF., Bowden TA. et al. Single dose systemic
antibiotic prophylaxis of surgical wound infections. Am. J. Surg. 1986;1
(52): 552-559.
5. Cadoz M., Denis F., Peyramond D. et al. Experience with ceftriaxone in
bacterial meningitis: clinical, bacteriological and pharmacological
results in 62 patients. Current Chemotherapy and Immunotherapy. 1982;
3: 47-52.
6. Geraghty J, Feely M. Antibiotic prophylaxis in neurosurgery A
randomized controlled trial. J Neurosurg. 1984; 60: 724-726.
7. Adeolu AA. Malomo AO. Shokunbi TM. Intraoperative Irrigation with
Ceftriaxone In Neurosurgical Patients. The Internet Journal of
Neurosurgery. 2005; 2 (2). DOI: 10.5580/1c08
QUICK RESPONSE CODE
ISSN (Online) : 2277 4572
Website
http://www.jpsionline.com
How to cite this article:
Amer Hayat Khan, Andee Dzulkarnaen Zakaria, Syed Azhar Syed Sulaiman,
Muhammad Ihtisham Umar, Nur-Elyana Yazmin Redhuan. The
perioperative use of Ceftriaxone as infection prophylaxis in Neurosurgery:
Cranioplasty. J Pharm Sci Innov. 2012; 1(5):27-28.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Entity Level ControlsDocument45 pagesEntity Level ControlsNiraj AlltimeNo ratings yet
- Inside Animator PDFDocument484 pagesInside Animator PDFdonkey slapNo ratings yet
- Oracle Learning ManagementDocument168 pagesOracle Learning ManagementAbhishek Singh TomarNo ratings yet
- Sysmex Xs-800i1000i Instructions For Use User's ManualDocument210 pagesSysmex Xs-800i1000i Instructions For Use User's ManualSean Chen67% (6)
- PROF ED 10-ACTIVITY #1 (Chapter 1)Document4 pagesPROF ED 10-ACTIVITY #1 (Chapter 1)Nizelle Arevalo100% (1)
- Progressive Myoclonic Epilepsies - Practical Neurology 2015. MalekDocument8 pagesProgressive Myoclonic Epilepsies - Practical Neurology 2015. MalekchintanNo ratings yet
- Exp 8 - GPG - D12B - 74 PDFDocument4 pagesExp 8 - GPG - D12B - 74 PDFPRATIKSHA WADIBHASMENo ratings yet
- Iso 9001 CRMDocument6 pagesIso 9001 CRMleovenceNo ratings yet
- STAT455 Assignment 1 - Part ADocument2 pagesSTAT455 Assignment 1 - Part AAndyNo ratings yet
- Pom Final On Rice MillDocument21 pagesPom Final On Rice MillKashif AliNo ratings yet
- Google Dorks For PentestingDocument11 pagesGoogle Dorks For PentestingClara Elizabeth Ochoa VicenteNo ratings yet
- On The Behavior of Gravitational Force at Small ScalesDocument6 pagesOn The Behavior of Gravitational Force at Small ScalesMassimiliano VellaNo ratings yet
- Service and Maintenance Manual: Models 600A 600AJDocument342 pagesService and Maintenance Manual: Models 600A 600AJHari Hara SuthanNo ratings yet
- How Psychology Has Changed Over TimeDocument2 pagesHow Psychology Has Changed Over TimeMaedot HaddisNo ratings yet
- Controle de Abastecimento e ManutençãoDocument409 pagesControle de Abastecimento e ManutençãoHAROLDO LAGE VIEIRANo ratings yet
- Jfif 1.02Document9 pagesJfif 1.02Berry Hoekstra100% (1)
- Account Statement From 30 Jul 2018 To 30 Jan 2019Document8 pagesAccount Statement From 30 Jul 2018 To 30 Jan 2019Bojpuri OfficialNo ratings yet
- Memo Roll Out Workplace and Monitoring Apps Monitoring Apps 1Document6 pagesMemo Roll Out Workplace and Monitoring Apps Monitoring Apps 1MigaeaNo ratings yet
- System: Boehringer Mannheim/Hitachi AnalysisDocument20 pagesSystem: Boehringer Mannheim/Hitachi Analysismaran.suguNo ratings yet
- Radio Frequency Transmitter Type 1: System OperationDocument2 pagesRadio Frequency Transmitter Type 1: System OperationAnonymous qjoKrp0oNo ratings yet
- AATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsDocument3 pagesAATCC 100-2004 Assesment of Antibacterial Dinishes On Textile MaterialsAdrian CNo ratings yet
- PESO Online Explosives-Returns SystemDocument1 pagePESO Online Explosives-Returns Systemgirinandini0% (1)
- Liebert PSP: Quick-Start Guide - 500VA/650VA, 230VDocument2 pagesLiebert PSP: Quick-Start Guide - 500VA/650VA, 230VsinoNo ratings yet
- Log File Records Startup Sequence and Rendering CallsDocument334 pagesLog File Records Startup Sequence and Rendering CallsKossay BelkhammarNo ratings yet
- Ancient Greek Divination by Birthmarks and MolesDocument8 pagesAncient Greek Divination by Birthmarks and MolessheaniNo ratings yet
- Budgetary ControlsDocument2 pagesBudgetary Controlssiva_lordNo ratings yet
- ITU SURVEY ON RADIO SPECTRUM MANAGEMENT 17 01 07 Final PDFDocument280 pagesITU SURVEY ON RADIO SPECTRUM MANAGEMENT 17 01 07 Final PDFMohamed AliNo ratings yet
- Kami Export - BuildingtheTranscontinentalRailroadWEBQUESTUsesQRCodes-1Document3 pagesKami Export - BuildingtheTranscontinentalRailroadWEBQUESTUsesQRCodes-1Anna HattenNo ratings yet
- Merchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaDocument29 pagesMerchandising Calender: By: Harsha Siddham Sanghamitra Kalita Sayantani SahaSanghamitra KalitaNo ratings yet