Professional Documents
Culture Documents
Acls
Uploaded by
Sel Neil0 ratings0% found this document useful (0 votes)
53 views10 pagesEpinephrine is the primary drug used in the pulseless arrest algorithm. It is used for its potent vasoconstrictive effects and also for its ability toincrease cardiac output. It should be used with caution in patients suffering from myocardial infarction.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentEpinephrine is the primary drug used in the pulseless arrest algorithm. It is used for its potent vasoconstrictive effects and also for its ability toincrease cardiac output. It should be used with caution in patients suffering from myocardial infarction.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
53 views10 pagesAcls
Uploaded by
Sel NeilEpinephrine is the primary drug used in the pulseless arrest algorithm. It is used for its potent vasoconstrictive effects and also for its ability toincrease cardiac output. It should be used with caution in patients suffering from myocardial infarction.
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 10
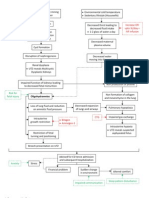
ACLS (ADVANCED CARDIAC LIFE SUPPORT)
ACLS Algorithms & Their Primary Drugs
Epinephrine is the primary drug used in the pulseless arrest algorithm. It is used for its potent vasoconstrictive effects and also for its
ability toincrease cardiac output. Epinephrine is considered a vasopressor.
Indications for ACLS
1. Vasoconstriction effects: epinephrine binds directly to alpha-1 adrenergic receptors of the blood vessels (arteries and veins)
causing direct vasoconstriction, thus, improving perfusion pressure to the brain and heart.
2. Cardiac Output: epinephrine also binds to beta-1-adrenergic receptors of the heart. This indirectly improves cardiac output by:
o Increasing heart rate
o Increasing heart muscle contractility
o Increasing conductivity through the AV node
Epinephrine is used in the pulseless arrest algorithm as a direct IV push and also in the bradycardia algorithm as an infusion. See the
respective algorithm pages for more information about their use in each.
Routes
During ACLS, epinephrine can be given 3 ways: intravenous; intraosseous, and endotracheal tube
Dosing
Intravenous Push/IO: 1mg epinephrine IV is given every 3-5 minutes.
IV infusion for bradycardia: 1mg epinephrine is mixed with 500ml of NS or D5W. The infusion should run at 2-10 micrograms/min
(titrated to effect).
IV infusion for post-cardiac arrest hypotension: The dosing is 0.1-0.5 mcg/kg/min (for example a 70kg adult: 7-35 mcg/min would
be given).
Endotracheal Tube: 2-2.5mg epinephrine is diluted in 10cc NS and given directly into the ET tube.
Epinephrine should be used with caution in patients suffering from myocardial infarction since epinephrine increases heart rate and
raises blood pressure. This increase in HR and BP can increase myocardial oxygen demand and worsen ischemia.
Vasopressin is a primary drug used in the pulseless arrest algorithm. In high concentrations, it raises blood pressure by inducing
moderate vasoconstriction, and it has been shown to be more effective than epinephrine in asystolic cardiac arrest (Wenzel V,
Krismer AC, Arntz HR, Sitter H, Stadlbauer KH, Lindner KH (January 2004). A comparison of vasopressin and epinephrine for out-of-
hospital cardiopulmonary resuscitation. N. Engl. J. Med. 350 (2): 10513. doi:10.1056/NEJMoa025431. PMID 14711909.)
One major indication for vasopressin over epinephrine is its lower risk for adverse side effects when compared with epinephrine.
With epinephrine, some studies have shown a risk of increased myocardial oxygen consumption and post arrest arrhythmias because
of an increase in heart rate and contractility (beta 1 effects). Vasopressin also is thought too cause cerebral vessel dilation and
theoretically increase cerebral perfusion.
Trivia: Another name for vasopressin is antidiuretic hormone (ADH).
Routes
Vasopressin may be given IV/IO or by endotracheal tube.
Dosing
40 units of vasopressin IV/IO push may be given to replace the first or second dose of epinephrine, and at this time, there is insufficient
evidence for recommendation of a specific dose per the endotracheal tube.
In the ACLS pulseless arrest algorithm, vasopressin may replace the first or second dose of epinephrine.
Amiodarone is considered a class III antiarrhythmic agent and is used for various types tachyarrhythmias. Because of its associated
toxicity and serious side-effects it should be used cautiously and care should be taken to ensure that cumulative doses are not
exceeded.
Indications for ACLS
Amiodarone is an antiarrhythmic that is used to treat both supraventricular arrhythmias and ventricular arrhythmias.
The mechanism of action of amiodarone remains unknown, but within the framework of ACLS, amiodarone is used primarily to treat
ventricular fibrillation and ventricular tachycardia that occurs during cardiac arrest and is unresponsive to shock delivery, CPR, and
vasopressors.
Amiodarone should not be used in individuals with polymorphic VT as it associated with a prolonged QT interval which is made worse
with antiarrhythmic drugs.
Amiodarone should only be used after defibrillation/cardioversion and first line drugs such as epinephrine and vasopressin have failed
to convert VT/VF.
Route
Amiodarone can be administered by intravenous or intraosseous route.
Dosing
The maximum cumulative dose in a 24 hour period should not exceed 2.2 grams.
Within the VT/VF pulseless arrest algorithm, the dosing is as follows:
300mg IV/IO push (if no conversion) 150 mg IV/IO push (after conversion) Infusion #1 360 mg IV over 6 hours (1mg/min)
Infusion #2 540 mg IV over 18 hours (0.5mg/min)
For tachyarrhythmias other than life threatening, expert consultation should be considered before use.
For Tachycardia other than pulseless VT/VF, Amiodarone dosing is as follows: (see above note)
150 mg over 10 minutes repeat as needed if VT recurs maintenance infusion of 1mg/min for 6 hours
Amiodarone should only be diluted with D5W and given with an in-line filter.
Infusions exceeding 2 hours must be administered in glass or polyolefin bottles containing D5W.
Lidocaine
Although lidocaine was removed from the 2010 Simplified Pulseless Arrest Diagram, it is still considered a suitable alternative if
amiodarone is ineffective in cardiac arrest from VT/VF.
Lidocaine was removed in the AHA Simplified Pulseless Arrest Diagram to help reduce emphasis on the use of medications and pl ace
more emphasis on high quality CPR and early defibrillation.
Indications for ACLS
In ACLS, Lidocaine is used intravenously for the treatment of ventricular arrhythmias. (VT/VF)
It is also useful for the treatment of stable monomorphic VT with preserved ventricular function and for stablepolymorphic VT with
preserved left ventricular function, normal QT interval, and correction of any electrolyte imbalances.
The overall benefits of lidocaine for the treatment arrhythmias in cardiac arrest has come under scrutiny. It has been shown to have no
short term or long term efficacy in cardiac arrest.
Routine prophylactic use is contraindicated for acute myocardial infarction.
Side Effects
Lidocaine should be used with caution due to negative cardiovascular effects which include hypotension, bradycardia, arrhythmias,
and/or cardiac arrest. Some of these side effects may be due to hypoxemia secondary to respiratory depression.
Lidocaine Toxicity
Symptoms of lidocaine toxicity progress in the following predictable pattern. It begins with numbness of the tongue, lightheadedness,
and visual disturbances and progresses to muscle twitching, unconsciousness, and seizures, then coma, respiratory arrest, and
cardiovascular depression.
There are several conditions that increase the potential for lidocaine toxicity:
1. Liver dysfunction increases the risk of toxicity due to lidocaine being metabolized by the liver.
2. Low protein increases the risk of toxicity because lidocaine is protein bound.
3. Acidosis can also increase the risk of toxicity since acidosis increase the potential of lidocaine to dissociate from plasma proteins.
Dosing
Cardiac Arrest from VT/VF:
Initial dose: 1 to 1.5 mg/kg IV/IO
For refractory VF may give additional 0.5 to 0.75 mg/kg IV push, repeat in 5 to 10 minutes; maximum 3 doses or total of 3mg/kg
Perfusing Arrhythmia:
For stable VT, wide-complex tachycardia of uncertain type and significant ectopy:
Doses Range from 0.5 to 0.75 mg/kg and up to 1 to 1.5mg/kg
Repeat 0.5 to 0.75 mg/kg every 5-10 minutes with maximum total dose of 3 mg/kg
Maintenance infusion:
1 to 4 mg/min (30-50 mcg/kg/min)
Atropine
When bradycardia is being treated in ACLS, if an underlying cause cannot be identified and corrected, medications are indicated.
There are three medications used in the bradycardia algorithm: atropine, epinephrine, and dopamine. Each drug and its use within the
bradycardia algorithm is explained below.
Atropine is the first drug used to treat bradycardia in the bradycardia algorithm. It is classified as an anticholinergic drug and increases
firing of the SA Node by blocking the action of the vagas nerve on the heart resulting in an increased heart rate.
Atropine should be used cautiously in the presence of myocardial ischemia and hypoxia since it increases oxygen demand of heart and
can worsen ischemia.
The dosing for Atropine is 0.5 mg IV every 3-5 minutes as needed, and the maximum total dosage that can be give is 3 mg.
Atropine should be avoided in hypothermic bradycardia and it will not be effective for Mobitz type II/Second Degree Block Type 2.
You may have read that Atropine is not effective for Mobitz II (2nd degree block type II) and Complete Heart Block (3rd degree block)
Epinephrine and Dopamine
Epinephrine and dopamine are second-line drugs for symptomatic bradycardia. They are both used as infusions in the bradycardia
algorithm if atropine is ineffective.
New 2010 ACLS guidelines state that if bradycardia is unresponsive to atropine, an equally effective alternative to transcutaneous
pacing is the use of an IV infusion of the beta-adrenergic agonists (dopamine or epinephrine).
Dosing:
Begin the epinephrine infusion at 2 to 10 mcg/min and titrate to patients response.
The goal of therapy is to improve the patients clinical status rather than target an exact heart rate.
Begin the dopamine infusion at 2 to 10 mcg/kg/min and titrate to the patients response.
Precautions
Prior to use of ACLS drugs in the treatment of symptomatic bradycardia, contributing factors of the bradycardia should be explored then
ruled out or corrected.
Adenosine
Adenosine should be used within the tachycardia algorithm when vagal maneuvers fail to terminate stable narrow-complex SVT.
Adenosine is the primary drug used in the treatment of stable narrow-complex SVT (supraventricular Tachycardia). It can now also be
used for regular monomorphic wide-complex tachycardia.
When given as a rapid IV bolus, adenosine slows cardiac conduction particularly effecting conduction through the AV node. The rapid
bolus of adenosine also interrupts reentry (SVT causing) pathways through the AV node and restores sinus rhythm in patients with
SVT.
When injected into the body, adenosine is rapidly absorbed by red blood cells and blood vessel endothelial cells and metabolized for
natural uses throughout the body. In light of this adenosine should be administered by RAPID intravenous bolus so that a significant
bolus of adenosine reaches the heart before it is metabolized.
A change from the 2010 guidelines now has adenosine given up to two times rather than three.
Dosing
The first dose of adenosine should be 6 mg administered rapidly over 1-3 seconds followed by a 20 ml NS bolus. If the patients rhythm
does not convert out of SVT within 1 to 2 minutes, a second 12 mg dose may be given in similar fashion. All efforts should be made to
administer adenosine as quickly as possible.
Precautions
Some side effects of adenosine administration incude flushing, chest pain/tightness, brief asystole or bradycardia.
Make sure that adenosine is not used for irregular, polymorphic wide-complex tachycardia and unstable VT. Use in these cases may
cause clinical deterioration.
ACLS RHYTHM INTERPRETATION
Pulseless Ventricular Tachycardia
The pulseless ventricular tachycardia rhythm is primarily identified by several criteria. First, the rate is usually greater than 180 beats
per minute and the rhythm generally has a very wide QRS complex.
Second, the patient will be pulseless and third, the rhythm originates in the ventricles. This is in contrast to other types of tachycardias
which have origination above the ventricular tissue (in the atria).
Not all ventricular tachycardias are pulseless and therefore, pulselessness must be established prior to beginning an algorithm. This is
accomplished simply by checking a carotid or femoral pulse.
Pulselessness with a tachyarrhythmia occurs because the ventricles are not effectively moving blood out of the heart and there is
therefore no cardiac output. Many tachyarrhythmias of a rate >150 will deteriorate into pulselessness if timely treatment is not given.
Ventricular Fibrillation
Ventricular fibrillation or VF occurs when there are uncoordinated contractions within the ventricles of the heart. The primary cause of
VF is hypoxia (lack of oxygen) to the heart muscle which causes hyperirritability in the cardiac muscle tissue.
As a result, multiple muscles cells within the ventricles simultaneously fire as pacemakers causing a quivering or fibrillation that is
ineffective for adequate cardiac output.
The two images above show what ventricular fibrillation will look like on a EKG rhythm strip.
VF can rapidly lead to heart muscle ischemia and there is a high likelihood that it will deteriorate into asystole.
Ventricular fibrillation is always pulseless and must be confirmed by EKG or defibrillator monitor. Defibrillation is the treatment of choice
and should occur as soon as possible.
Pulseless Electrical Activity (PEA) Rhythm
PEA rhythm occurs when any heart rhythm that is observed on the electrocardiogram (ECG) does not produce a pulse. PEA can come
in many different forms. Sinus Rhythm, tachycardia, and bradycardia can all be seen with PEA.
Performing a pulse check after a rhythm/monitor check will ensure that you identify PEA in every situation.
Pulseless electrical activity usually has an underlying treatable cause. The most common cause in emergency situations
is hypovolemia.
PEA is treated by assessing and correcting the underlying cause.
Pop-Quiz:
Question #1: If you saw the rhythm below after defibrillation, how would you determine if it is pulseless electrical activity?
click here for answer
You should check for a carotid or femoral pulse
Question #2: What is the most common cause of PEA?
click here for answer
Hypovolemia
Asystole or flatline
Asystole is not actually a true rhythm but rather is a state of no cardiac electrical activity. The main treatment of choice for asystole is
the use of epinephrine and CPR.
Asystole is treated using the right branch of the puslesless arrest arrest algorithm. Click below to view the pulseless arrest algorithm
diagram. When done click again to close the diagram.
Pulseless Arrest Algorithm Diagram.
During asystole, there is no blood flow to the brain and other vital organs. This results in very poor outcomes if resuscitation is
successful.
If asystole is visualized on the monitor, you should ensure that all leads are connected properly. If all leads are properly connected, you
should rapidly assess for any underlying causes for the asystole.
As with pulseless electrical activity (PEA), asystole can have possible underlying causes which can be remembered using the Hs and
Ts mnemonic.
First-Degree Heart Block
Also called first-degree AV block is a disease of the electrical conduction system of the heart in which the PR interval is lengthened
beyond 0.20 seconds.
This lengthening of the PR interval is caused by a delay in the electrical impulse from the atria to the ventricles through the AV node
Normally and in the case of ACLS, first-degree heart block is of no consequence unless it involves myocardial infarction or an
electrolyte imbalance.
Although first-degree heart block is not clinically significant for ACLS, recognition of the major AV blocks is important because treatment
decisions are based on the type of block present.
Second-Degree Heart Block (Type 1)
Also called Mobitz 1 or Wenckebach is a disease of the electrical conduction system of the heart in which the PR interval has
progressive prolongation until finally the atrial impulse is completely blocked and does not produce a QRS electrical impulse.
Once the p-wave is blocked and no QRS is generated, the cycle begins again with the prolongation of the PR interval.
One of the main identifying characteristics of second degree heart block type 1 is that the atrial rhythm will be regular.
In the above image, notice that the p-waves are regular, the PR-interval progressively gets longer until a QRS is dropped and only the
p-wave is present.
Although second degree heart block type-1 is not clinically significant for ACLS, recognition of the major AV blocks is important
because treatment decisions are based on the type of block present.
Second-Degree (AV) Heart Block (Type 2)
Also called Mobitz II or Hay is a disease of the electrical conduction system of the heart. Second-degree AV block (Type 2) is almost
always a disease of the distal conduction system located in the ventricular portion of the myocardium.
This rhythm can be recognized by the following characteristics:
1. non-conducted p-waves (electrical impulse conducts through the AV node but complete conduction through the ventricles is
blocked, thus no QRS)
2. P-waves are not preceded by PR prolongation as with second-degree AV block (Type 1)
3. fixed PR interval
4. The QRS complex will likely be wide click here to see why
Second-degree AV block (Type 2) is clinically significant for ACLS because this rhythm can rapidly progress to complete heart block
Second-degree AV block (Type 2) should be treated with immediate transcutaneous pacing or transvenous pacing because there is risk
that electrical impulses will not be able to reach the ventricles and produce ventricular contraction.
Atropine may be attempted if immediate TCP is not available or time is needed to initiate TCP. Atropine should not be relied upon and
in the case of myocardial ischemia it should be avoided.
Complete Heart Block
Third-degree AV block or complete heart block is the most clinically significant AV block associated with ACLS. Complete heart block
occurs when the electrical impulse generated in the SA node in the atrium is not conducted to the ventricles.
When the atrial impulse is blocked, an accessory pacemaker in the ventricles will typically activate a ventricular contraction. This
accessory pacemaker impulse is called an escape rhythm.
Because two independent electrical impulses occur (SA node impulse & accessory pacemaker impulse), there is no apparent
relationship between the P waves and QRS complexes on an ECG.
Characteristics that can be seen on an ECG include:
1. P waves with a regular P to P interval
2. QRS complexes with a regular R to R interval
3. The PR interval will appear variable because there is no relationship between the P waves and the QRS Complexes
In the image above note that the p-waves are independent of the QRS complexes. Also note the 4th QRS complex (impulse) looks
different from the others. This is because it is from a different accessory pacemaker in the ventricle than the other QRS complexes.
Common Causes
The most common cause of complete block is coronary ischemia and myocardial infarction. Reduced blood flow or complete loss of
blood flow to the myocardium damages the conduction system of the heart, and this results in an inability to conduct impulses from the
atrium to the ventricles.
Those with third-degree AV block typically experience bradycardia, hypotension, and in some cases hemodynamic instability.
The treatment for unstable third-degree AV block in ACLS is transcutaneous pacing.
Supraventricular Tachycardia (SVT)
SVT is a broad term for a number of tachyarrhythmias that originate above the ventricular electrical conduction system (purkinje fibers).
Classic Paroxysmal SVT has a narrow QRS complex & has a very regular rhythm. Inverted P waves are sometimes seen after the QRS
complex. These are called retrograde p waves
The heart fills during diastole, and diastole is normally 2/3 the cardiac cycle. A rapid heart rate will significantly reduce the time which
the ventricles have to fill. The reduced filling time results in a smaller amount of blood ejected from the heart during systole. The end
result is a drop in cardiac output & hypotension.
With the drop in cardiac output, a patient may experience the following symptoms. These symptoms occur more frequently with a heart
rate >150 beats per minute:
Shortness of air (S)
Palpitation feeling in chest (S)
Ongoing chest pain (U)
Dizziness (S)
Rapid breathing (S)
Loss of consciousness (U)
Numbness of body parts (S)
The pathway of choice for SVT in the tachycardia algorithm is based on whether the patient is stable or unstable. The symptoms listed
above that would indicate the patient is unstable are noted with the letter (U). Stable but serious symptoms are indicated with the letter
(S).
Unstable patients with SVT and a pulse are always treated with cardioversion
Atrial Flutter
This abnormal heart rhythm technically falls under the category of supra-ventricular tachycardias. Atrial flutter is typically not a stable
rhythm and will frequently degenerate into atrial fibrillation.
Atrial Flutter will usually present with atrial rates between 240-350 beats per minute. These rapid atrial rates are caused by electrical
activity that moves in a self-perpetuating loop within the atria.
The impact and symptoms of atrial flutter depend upon the ventricular rate of the patient (i.e. cardiac output). Usually, with atrial flutter,
not all of the atrial impulses will be conducted to the ventricles, and the more atrial impulses that are conducted, the greater the
negative effect.
Symptoms
Symptoms of atrial flutter are similar to those of atrial fibrillation and may include the following:
palpitations, chest pain or discomfort
shortness of air
lightheadedness or dizziness
nausea
nervousness and feelings of impending doom
symptoms of heart failure such as activity intolerance and swelling of the legs occur with prolonged fast flutter)
Complications
As with its symptoms, atrial flutter shares the same complications as atrial fibrillation. These complications are usually due to ineffective
atrial contractions and rapid ventricular rates. Ineffective atrial contractions can lead to thrombus formation in the atria and rapid
ventricular rates can cause decompensation and heart failure.
Prevent complications from atrial flutter with early cardioversion.
Treatment
For the purposes of ACLS, atrial flutter is treated the same as atrial fibrillation. When atrial flutter produces hemodynamic instability and
serious signs and symptoms, it is treated using ACLS protocol.
For the patient with unstable tachycardia due to this tachyarrhythmia (atrial flutter), immediate cardioversion is recommended. Drugs
are not used to manage unstable tachycardia.
Cardioversion
Atrial flutter is considerably more sensitive to electrical direct-current cardioversion than atrial fibrillation, and usually requires a lower
energy shock. 20-50J is commonly enough to revert to sinus rhythm.
Atrial Fibrillation
The most common cardiac arrhythmia, atrial fibrillation, occurs when the normal electrical impulses that are generated by the SA node
are overwhelmed by disorganized electrical impulses in the atria.
These disorganized impulses cause the muscles of the upper chambers of the heart to quiver (fibrillate) and this leads to the conduction
of irregular impulses to the ventricles.
For ACLS, atrial fibrillation becomes a problem when the fibrillation produces a rapid heart rate which reduces cardiac output and
causes symptoms or an unstable condition.
When atrial fibrillation occurs with a (RVR) rapid ventricular rate (rate > 100 beats/min), this is called a tachyarrhythmia. This
tachyarrhythmia may or may not produce symptoms. Significant symptoms that occur are due to a reduction in cardiac output.
The following is a list of the most common symptoms.
palpitations or chest discomfort
shortness of air and possibly respiratory distress
hypotension, light-headedness and possibly loss of consciousness
peripheral edema, jugular vein distention, and possibly pulmonary edema
For the purpose of ACLS, it is important to be able to recognize atrial fibrillation when the patient is symptomatic. On an ECG monitor,
there are two major characteristics that will help you identify atrial fibrillation.
1. No p-waves before the QRS on the ECG. This is because there are no coordinated atrial contractions.
2. The heart rate will be irregular. Irregular impulses that the ventricles are receiving cause the irregular heart rate.
When the heart rate is extremely rapid, it may be difficult to determine if the rate is irregular, and the absence of p-waves will be the
best indicator of atrial fibrillation.
ACLS Treatments:
For the purposes of ACLS atrial fibrillation is treated when the arrhythmia/tachyarrhythmia produces hemodynamic instability and
serious signs and symptoms.
For the patient with unstable tachycardia due to a tachyarrhythmia, immediate cardioversion is recommended. Drugs are not used to
manage unstable tachycardia.
Cardioversion of stable atrial fibrillation should be performed with caution if the arrhythmia is more than 48 hours old and no
anticoagulant therapy has been initiated due to the risk of emboli that can cause MI and stroke.
Other Tachycardia Rhythms
There are several other tachycardia rhythms that can be seen with both stable and unstable tachycardia. These rhythms
include monomorphic ventricular tachycardia and polymorphic ventricular tachycardiaboth of which are wide-complex
tachycardias.
Wide complex tachycardias are defined as a QRS of 0.12 second. Expert consultation should be considered with these rhythms.
These wide-complex tachycardias are the most common forms of tachycardia that will deteriorate to ventricular fibrillation.
Monomorphic Ventricular Tachycardia
With monomorphic VT all of the QRS waves will be symmetrical. Each ventricular impulse is being generated from the same place in
the ventricles thus all of the QRS waves look the same.
Treatment of monomorphic VT is dependent upon whether the patient is stable or unstable. Expert consultation is always advised, and
if unstable, the ACLS tachycardia algorithm should be followed.
Polymorphic Ventricular Tachycardia
With polymorphic ventricular tachycardia, the QRS waves will not be symmetrical. This is because each ventricular impulse can be
generated from a different location. On the rhythm strip, the QRS might be somewhat taller or wider.
One commonly seen type of polymorphic ventricular tachycardia is torsades de pointes. Torsades and other polymorphic VT are
advanced rhythms which require additional expertise and expert consultation is advised.
If polymorphic VT is stable the ACLS tachycardia algorithm should be used to treat the patient. Unstable polymorphic ventricular
tachycardia is treated with unsynchronized shocks (defibrillation). Defibrillation is used because synchronization is not possible.
These wide complex tachycardias tend to originate in the ventricles rather than like a normal rhythm which originates in the atria.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- DocuNotes Clinical Pocket Guide To Effective ChartingDocument203 pagesDocuNotes Clinical Pocket Guide To Effective ChartingShirlyn Ares Navarro96% (47)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- GrammatikkDocument115 pagesGrammatikkSel NeilNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Pearson DrugsDocument20 pagesPearson DrugsSel NeilNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- List of Drugs To Be Prepared ForDocument1 pageList of Drugs To Be Prepared ForSel NeilNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- DOH Nurse Deployment Project 2014 Application FormDocument1 pageDOH Nurse Deployment Project 2014 Application FormjamieboyRNNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Casepres ObDocument6 pagesCasepres ObSel NeilNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- IV PDFDocument63 pagesIV PDFelbagouryNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- PrejudiceDocument3 pagesPrejudiceSel NeilNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliDocument3 pagesThe Egyptian Heart Journal: Ahmed Elshazly, Hazem Khorshid, Hany Hanna, Ammar AliImran TarmiziNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Module 4. Ebj. Pingul, MCDocument4 pagesModule 4. Ebj. Pingul, MCCharline PingulNo ratings yet
- Pathways to Obesity, Hypertension, and Circulatory DisordersDocument1 pagePathways to Obesity, Hypertension, and Circulatory DisordersFitria NorkhalidaNo ratings yet
- Urokinase Dosage WheelDocument2 pagesUrokinase Dosage WheelNidhiNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- ElectrocardiogramDocument169 pagesElectrocardiogramjitendra magarNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- WS Emergency Echo SYMCARD 2022Document33 pagesWS Emergency Echo SYMCARD 2022IndRa KaBhuomNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- 2008.clin Chem - RantnerDocument7 pages2008.clin Chem - RantnertwkangNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Diagnosa PRBDocument12 pagesDiagnosa PRBSAEHANNo ratings yet
- Clinical Trials in Cardiology 2nd Ed PDFDocument272 pagesClinical Trials in Cardiology 2nd Ed PDFIrving H Torres LopezNo ratings yet
- CPG Management of Percutaneous Coronory Intervention (PCI) 2009Document92 pagesCPG Management of Percutaneous Coronory Intervention (PCI) 2009umiraihana1No ratings yet
- Preeklamsi 9Document22 pagesPreeklamsi 9Melda Amalia SikumbangNo ratings yet
- Burger Allen Exercises PDFDocument122 pagesBurger Allen Exercises PDFlucky 116No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Permanent Junctional Reciprocating Tachycardia in Children - A Multicenter Experience 2014Document26 pagesPermanent Junctional Reciprocating Tachycardia in Children - A Multicenter Experience 2014Võ Từ NhấtNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Pathophysiology (Cerebrovascular Accident Hemorrhagic Right Lobe)Document4 pagesPathophysiology (Cerebrovascular Accident Hemorrhagic Right Lobe)jhonkivenNo ratings yet
- MRI Case Study Cervical SpineDocument15 pagesMRI Case Study Cervical SpineTunas HarapanNo ratings yet
- CatheterizationDocument2 pagesCatheterizationElishah CaprichoNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- ECOCARDIODocument3 pagesECOCARDIOArun ComedsNo ratings yet
- Ecg TestDocument67 pagesEcg TestEm KayNo ratings yet
- The Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainDocument10 pagesThe Association Between Emergency Department Crowding and Adverse Cardiovascular Outcomes in Patients With Chest PainGrace Angelica Organo TolitoNo ratings yet
- Presented By: Bhawna Joshi Msc. Nursing 1 YearDocument52 pagesPresented By: Bhawna Joshi Msc. Nursing 1 YearBhawna JoshiNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Circulatory and Respiratory System, Working TogetherDocument32 pagesCirculatory and Respiratory System, Working TogetherRhona AngelaNo ratings yet
- Hemorrhagic StrokeDocument2 pagesHemorrhagic StrokeMuhammad Anwar AnsoriNo ratings yet
- (José Almeida) Atlas of Endovascular Venous SurgeDocument516 pages(José Almeida) Atlas of Endovascular Venous SurgeTa TaNo ratings yet
- Cerebrovascular Hypertension by John Dickinson and Julian PatonDocument272 pagesCerebrovascular Hypertension by John Dickinson and Julian PatonPaul DickinsonNo ratings yet
- AbijitDocument3 pagesAbijitvimalNo ratings yet
- Cardiovascular Management Using Yogic TechniquesDocument3 pagesCardiovascular Management Using Yogic TechniquesJacklynlim LkcNo ratings yet
- Stress Echocardiography: Dr. Surinder Singh HansraDocument35 pagesStress Echocardiography: Dr. Surinder Singh HansrasshansraNo ratings yet
- The Non Invasive Assessment of VascularDocument39 pagesThe Non Invasive Assessment of VascularLilia RadjefNo ratings yet
- Case Congenital AV BlockDocument27 pagesCase Congenital AV BlockPrima Hari NastitiNo ratings yet
- Amity College of Nursing: Nursing Care Plan ON Heart FailureDocument20 pagesAmity College of Nursing: Nursing Care Plan ON Heart Failurejyoti puniaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)