Professional Documents
Culture Documents
Diagnosis Brucella Turkey
Uploaded by
Joshua Smith0 ratings0% found this document useful (0 votes)
14 views5 pagesdiagnosis patterns in turkey
Original Title
diagnosis brucella turkey
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentdiagnosis patterns in turkey
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views5 pagesDiagnosis Brucella Turkey
Uploaded by
Joshua Smithdiagnosis patterns in turkey
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 5
272
*Corresponding author: Mailing address: CBU Tip Fakulte-
si Dekanligi, Tibbi Mikrobiyoloji, Uncubozkoy, 45030
Manisa, Turkey. Tel: 902362331920/429, E-mail:
talat.ecemisgmail.com
272
Jpn. J. Infect. Dis., 64, 272-276, 2011
Original Article
Evaluation of Serological Tests for Diagnosis of Brucellosis
Ozan Pabuccuoglu, Talat Ecemis
*
, Sibel El
1
, Abdullah Coskun
2
,
Sinem Akcali, and Tamer Sanlidag
Celal Bayar University, Faculty of Medicine, Department of Medical Microbiology, Manisa;
1
Atat urk Education and Research Hospital, Department of Infectious Disease and
Clinical Microbiology, Izmir; and
2
State Hospital, Department of Infectious Disease and Clinical Microbiology, Manisa, Turkey
(Received January 24, 2011. Accepted April 8, 2011)
SUMMARY: The aim of the present study was to compare serological tests (Rose Bengal [RB]; stand-
ard agglutination test [SAT]; enzyme immunoassay [EIA] for detection of IgM, IgA, and IgG; and 2-
mercaptoethanol [2-ME] test) that are routinely used in patients prediagnosed with different clinical
types of brucellosis (acute, subacute, or chronic), and to evaluate the results of the IgG avidity test.
Ninety-two patients having titers 1/160 as measured by SAT were included in the study. The IgG avid-
ity test was performed in 78 patients who had positive EIA-IgG results. RB test results were positive in
88 (95.7z) patients. A statistically significant correlation was found between a positive EIA-IgM result
and the diagnosis of acute brucellosis. When compared to the results of the SAT, the 2-ME test showed
a lower titer in 55 (59.8z) patients, and the agreement between the 2-ME test and EIA-IgG was calculat-
ed as 84.8z. No statistical difference was found between the 40zavidity index used in the IgG avidity
test and avidity maturation time (6 months). From our study, we concluded that (i) the RB and SAT
tests are appropriate and reliable tests for the serological diagnosis of brucellosis; (ii) IgM can be used as
a marker of acute brucellosis; (iii) the 2-ME test, similar to EIA, can be used to determine IgM levels;
and (iv) the IgG avidity test should be standardized.
INTRODUCTION
Brucellosis is a systemic disease caused by bacteria of
the genus Brucella that affects humans and numerous
animal species. It has been a great concern for many
countries, especially those in the Middle East and
Mediterranean regions, in terms of public and animal
health. Human brucellosis infections can be unpredicta-
ble, with periods of chronicity, re-infection, and
relapse. A wide spectrum of clinical manifestations
makes clinical diagnosis difficult, and thus it is necessa-
ry to confirm brucellosis infection by thorough labora-
tory diagnosis (1,2).
Laboratory diagnosis of human brucellosis is based
on the isolation of Brucella spp. from blood cultures
and on the demonstration of the presence of specific an-
tibodies through the use of serological tests. Although
automated culture systems have reduced the growth
time of Brucella genus bacteria to 1 week, conventional
methods require nearly 4 times longer, and have a very
low success rate (only 1070z) (3). Laboratory diagno-
sis of brucellosis is frequently based on demonstration
of the presence of serum antibodies, and various labora-
tory tests are used for this purpose. The Rose Bengal
(RB) test is commonly used to screen for brucellosis in-
fections, but it has been suggested that the results of RB
should be verified by other tests (4). The standard ag-
glutination test (SAT), which was developed by Wright
and colleagues in 1897 in order to detect total antibod-
ies, is the most frequently used test to diagnose brucello-
sis. If the SAT test yields negative results due to the
presence of blocking antibodies, the Coombs' test may
be used instead.
Brucellosis can manifest as 3 different clinical types,
which are classfied according to the duration of sym-
ptoms: acute (initial 2 months), subacute (212
months), and chronic (12 months). The disease may
also be asymptomatic, subclinical, and focal, or present
with complications, relapses, and re-infections. The 2-
mercaptoethanol (2-ME) test can be used to predict the
course of the disease (5). Specific antibody classes (IgM,
IgG, and IgA) can be demonstrated by enzyme im-
munoassay (EIA) and immunochromatographic lateral
flow assay. Although all these tests may be implemented
to evaluate the different clinical forms and development
stages of the disease, in most cases they may not yield
definite results, and the stage of the disease may not be
determined serologically (1).
In some viral and parasitic diseases, it is possible to
determine whether the disease is acute or chronic, and at
which stage the disease is in, through implementation of
the IgG avidity test, which is based on maturing of an-
tibody affinity. The avidity test is not used routinely as
it has not yet been standardized for the diagnosis of
brucellosis; however, this test can be used to differenti-
ate between recent infections and previous infection. In
addition, some studies have revealed promising results
showing that the avidity test can be further developed
for the evaluation of brucellosis infections (6).
In this study, our aim was to compare serological tests
(RB, SAT, EIA, 2-ME) that are routinely used in
patients prediagnosed with different types of brucello-
273
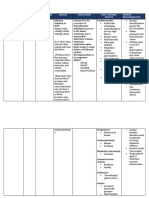
Table 1. Distribution of RB and EIA tests according to the type
of brucellosis
Acute
n 42 (z)
1)
Subacute
n 40 (z)
1)
Chronic
n 10 (z)
1)
Total
n 92 (z)
2)
RB 39 (92.9) 39 (97.5) 10 (100) 88 (95.7)
IgA 29 (69) 26 (65) 9 (90) 64 (69.6)
IgG 32 (76.2) 36 (90) 10 (100) 78 (84.8)
IgM 32 (76.2) 16 (40) 3 (30) 51 (55.4)
2-ME 33 (78.6) 19 (47.5) 3 (30) 55 (59.8)
1)
: Ratios in clinical types.
2)
: Ratios in total.
RB, Rose Bengal; EIA, enzyme immunoassay; 2-ME, 2-mercap-
toethanol.
Table 2. Distribution of SAT titers according to the type of
brucellosis
SAT
titers
Acute
n 42 (z)
1)
Subacute
n 40 (z)
1)
Chronic
n 10 (z)
1)
Total
n 92 (z)
2)
1/160 23 (56.1) 23 (57.5) 7 (70) 53 (57.6)
1/320 8 (19) 12 (30) 2 (20) 22 (23.9)
1/640 7 (16.7) 1 (2.5) 0 (0) 8 (8.7)
1/1,280 4 (9.5) 4 (10) 1 (10) 9 (9.8)
Footnotes
1)
and
2)
are in Table 1.
SAT, standard agglutination test.
273
sis, and to evaluate these results using the IgG avidity
test.
MATERIALS AND METHODS
The present study was conducted on patients pre-
diagnosed with brucellosis, and followed up by the
Izmir Atat urk Education and Research Hospital and
Manisa State Hospital Infectious Diseases Polyclinic
and Clinics in Turkey. A diagnosis form was created for
each patient whose disease course was known, and these
were classified as acute, subacute, or chronic. For all
patients, blood sera were analyzed by RB and SAT us-
ing the Brucella S99 strain according to the recommen-
dations of the manufacturer (Seromed, Istanbul, Tur-
key). Eligible patients were required to have a titer
1/160 in the SAT test to confirm the serological diag-
nosis of brucellosis, and sera from 92 patients meeting
this criterion were included in the study. Coombs' test
was performed on the sera from 2 patients who tested
negatively in the SAT test, in order to remove blocking
antibodies and/or eliminate the prozone phenomenon.
These sera were included in the study (7). All sera were
subjected to the 2-ME test using 0.05 M 2-ME (8). A
decreased titer in the 2-ME test compared to that of the
SAT was considered positive in terms of IgG antibody
presence. All these tests were evaluated by at least 2
microbiologists. The sera were then stored at 209C in
Eppendorf tubes for later testing in the EIA and IgG
avidity tests. After all the patient samples were collect-
ed, the presence of anti-Brucella IgM, IgG, and IgA an-
tibodies was determined using commercial EIA kits and
equipment (Radim, Rome, Italy). Results were consi-
dered either negative or positive on the basis of the cal-
culated cut-off values. When EIA test results conflicted
with SAT results, both the SAT and EIA tests were
repeated.
The avidity test was performed on the basis of the 8 M
urea denaturation method described by Hedmen and
Rousseau (9). The IgG avidity test was performed on
sera obtained from 78 patients who tested positive for
IgG antibodies; the test was performed using the proce-
dures, EIA anti-Brucella IgG kit, and equipment previ-
ously mentioned. Sera were diluted 1:100, and 1 pair
from each was added to the well. After initial incuba-
tion and washing, 100 ml of 8 M urea was added to one
of the serum pairs, and 100 ml of phosphate buffer solu-
tion was added to the other. Sera were then incubated
for 5 min. The remaining steps were performed accord-
ing to the manufacturer's recommendations, and ab-
sorption of all the wells was measured at 450 nm. Avidi-
ty index percentage was calculated according to the fol-
lowing formula:
IgG avidity index (AI)
absorbance of urea-treated microwells/
absorbance of untreated microwells 100
The AI cut-off value was set 40z, and the maturation
time (the time required for evolution of low-avidity an-
tibodies into high-avidity antibodies) was 6 months
(1,5).
Data were analyzed using SPSS 15.0 software (SPSS,
Chicago, Ill., USA). Pearson's chi-square test was used
to evaluate the avidity tests, and the McNemar test was
used to evaluate the degree of agreement between the
other serological tests. A P value 0.05 was considered
statistically significant.
RESULTS
Of the patients in the study, 45 (48.9z) were males,
while 47 (51.1z) were females. The average age of the
study participants was 39.2 years, with patients ranging
in age from 23 to 68 years. In the SAT, results revealed
titers ranging from 1/160 to 1/1,280. Ninety-two
patients were classified into 1 of 3 groups based on the
duration of their symptoms, and the number of acute,
subacute, and chronic patients was 42 (45.7z), 40
(43.5z), and 10 (10.9z), respectively. Distribution of
tests according to the type of brucellosis is described in
Tables 1 and 2.
The RB test was negative in 4 patients, and the agree-
ment between the SAT and RB tests was calculated as
95.7z. In 3 (3.2z) of the patients, all EIA tests were
negative. When EIA tests were evaluated according to
the clinical types, a statistically significant correlation
was found only between the presence of IgM antibodies
and acute-stage brucellosis (P 0.01). When EIA tests
were also evaluated in combinations of 2, there was no
statistically significant correlation between the com-
bined antibody tests and the clinical groups.
In 53 (57.6z) patients, SAT titer was 1/160, which
showed the highest ratio. The ratios of the other SAT
titers, 1/320, 1/640, and 1/1,280, were 23.9, 8.7, and
9.8z, respectively (Tables 2 and 3).
In 55 (59.8z) patients, the 2-ME test performed on
all sera revealed positivities, albeit with lower titers
compared to those obtained in SAT. In 46 (90.2z) of 51
IgM-positive patients, titers were decreased. Agreement
between the 2-ME and EIA-IgM tests were calculated to
274
Table 3. SAT results according to titers and distribution of positive RB and EIA tests according
to SAT titres
1/160
n 53 (z)
1)
1/320
n 22 (z)
1)
1/640
n 8 (z)
1)
1/1,280
n 9 (z)
1)
Total
n 92 (z)
2)
RB 49 (92.5) 22 (100) 8 (100) 9 (100) 88 (95.7)
IgM 24 (47.1) 12 (54.5) 6 (75) 9 (100) 51 (55.4)
IgA 30 (56.6) 17 (77.3) 8 (100) 9 (100) 64 (69.6)
IgG 44 (83) 20 (90.9) 6 (75) 8 (88.9) 78 (84.8)
1)
: Ratios in SAT titers.
2)
: Ratios in total.
Table 4. Comparison of 2-ME and IgM
IgM
Total (z)
2)
Positive (z)
1)
Negative (z)
1)
Decreased titer
in 2-ME test
Positive 46 (90.2) 9 (22) 55 (59.8)
Negative 5 (9.8) 32 (78) 37 (40.2)
Total (z)** 51 (55.4) 41 (44.6) 92 (100)
1)
: Ratios in IgM results.
2)
: Ratios in total.
Table 5. Distribution of different AIs according to disease
duration
6 months (z)
1)
6 months (z)
1)
Total (z)
2)
AI 40z
Low 27 (77.1) 8 (22.9) 35 (44.9)
High 30 (69.8) 13 (30.2) 43 (55.1)
AI 45z
Low 39 (78) 11 (22) 50 (64.1)
High 18 (64.3) 10 (35.7) 28 (35.9)
AI 50z
Low 46 (79.3) 12 (20.7) 58 (74.4)
High 11 (55) 9 (45) 20 (25.6)
AI 55z
Low 51 (77.3) 15 (22.7) 66 (84.6)
High 6 (50) 6 (50) 12 (15.4)
1)
: Ratios in disease durations.
2)
: Ratios in total.
AI, avidity index.
274
be 84.8z (Table 4). In the 2-ME test, 72 patients were
found to be positive, despite decreased titers.
In the IgG avidity test, 35 (44.9z) of 78 EIA-IgG-
positive patients had low AI values, while 43 (35.1z)
had high AI values. Forty (51.3z) of these 78 patients
were both EIA-IgG- and EIA-IgM-positive. When the
IgG avidity maturation time was set at 6 months, and
the AI cut-off value was 40z, there was no statistically
significant correlation between cut-off value and matu-
ration time ( P 0.465). When the AI cut-off value was
set at 45, 50, or 55z, P values were calculated to be
0.190, 0.035, and 0.050, respectively. Increasing matu-
ration time by 1 month also did not reveal any statisti-
cally significant correlation. The lowest P value associ-
ated with these 2 parameters was obtained when the
maturation time and AI cut-off value were evaluated at
6 months and 50z, respectively (Table 5).
DISCUSSION
In our study, RB test was found to be positive in 88 of
the 92 patients whose SAT tests showed titers 1/160.
We found 95.7z agreement between the RB and SAT
tests, revealing that RB is a valuable, easy-to-use, and
cost-effective screening test that can provide reliable
results in a relatively short time. Although studies on
this subject have yielded different results, those ob-
tained by comparing the RB test with the SAT test have
demonstrated results similar to ours (10). Some studies
have also reported 100z sensitivity for the RB test
(11,12). However, it has been shown that false negatives
could be due to a decrease in the agglutination ability of
antibodies at the low pH of the test medium (13). While
the RB test yields results within minutes, a minimum of
24 h is needed for the SAT test. This increases up to 48 h
when Coombs' test needs to be used to clarify negative
results. Unfortunately, evaluation of these tests involves
a level of subjectivity, and this may cause inexperienced
persons to report inaccurate results.
Evaluation of individual EIA tests in patient groups
classified according to symptoms showed that only one
immunoglobulin (i.e., IgG) can be used successfully,
with a 100z agreement with the SAT test, during the
chronic period. Although having a small number of
patients classified as chronic (10 patients) reduces the
strength of the study, similar results were found in a
study by Mantec on et al., where 100zIgG was detected
in 22 patients having a history of brucellosis (1).
Sirmatel et al. found the percentage of IgG-positive
patients to be 78.2z in a group composed of 92
chronic-stage patients (14). In regions where brucellosis
is endemic, persistent IgG positivities may reduce the di-
agnostic value of this test when it is used individually.
When evaluating the ratios of IgG-positive patinets dur-
ing the acute, subacute, and chronic periods of brucello-
sis (76.2, 90, and 100zrespectively), it appears that IgG
increases according to the duration of the disease. In the
panel of EIA tests, IgM was the only immunoglobulin
to show a statistically significant correlation with the
clinical types of brucellosis ( P 0.01), suggesting that
IgM can be used to diagnose acute brucellosis. The same
result has been obtained in many studies on EIA. Klerk
and Anderson reported that EIA-IgM is the ``most sen-
sitive test'' in the serological diagnosis of brucellosis
(15). Furthermore, Ariza et al. showed that a high level
of specific IgM was present at the beginning stages of
brucellosis, and that it decreased much more rapidly
than IgG or IgA (16). The rapid decrease shown by
Ariza et al. is also present in our results; number of
EIA-IgM-positive patients during the acute, subacute,
and chronic periods was found to be 32, 16, and 3, re-
spectively. Since positivity is not an issue in all patients
having brucellosis, it is not possible to exclude acute
275 275
brucellosis only on the basis of negative results. EIA-
IgG and IgA are not sufficient to make a diagnosis dur-
ing the acute and subacute periods. These should be
taken into consideration, along with the other tests, and
should definitely be tested in cases where negative EIA-
IgM results are found in acute period patients. EIA-IgM
can be detected as early as the first week after brucello-
sis infection, while IgG and IgA only appear after a cou-
ple of weeks (17). Therefore, these specific im-
munoglobulins cannot be reliably used during certain
disease phases. In fact, it is uncertain whether there is
value in such classifications for brucellosis, since it is a
disease that eventually evolves into a chronic state.
In 3 of the patients, all EIA tests were negative. Per-
formance in EIA tests varies in different studies.
Memish et al. found the sensitivities of SAT, EIA-IgG,
and EIA-IgM to be 95.6, 45.6, and 79z, respectively
(17), while Sisirak and Hukic reported sensitivities as
low as 64.8z for EIA-IgM and 56.1z for EIA-IgG
(11). In our country, Sirmatel et al. reported sensitivities
of SAT, EIA-IgM, and EIA-IgG to be 83.7, 61.9, and
49.5z, respectively (14). However, some studies have
reported very high sensitivities for EIA tests. For exam-
ple, Araj et al. reported sensitivities of 91 and 100zfor
EIA-IgG and EIA-IgM, respectively (18). Similarly, in a
study comparing blood cultures in various serological
tests, Ciftci et al. calculated the sensitivities of RB,
SAT, EIA-IgG, EIA-IgA, and EIA-IgM tests as 100,
94.3, 97.1, 94.1, and 71.4z, respectively (19). Our
results have shown that EIA tests should be evaluated
together, especially during the acute and subacute
stages, and an evaluation using only a single im-
munoglobulin may cause false-negative results.
Although no statistically significant correlation has
been found between EIA and SAT titers, nearly all
patients having an SAT titer of 1/1,280 had positive
results in EIA; in fact, only 1 patient was found to be
negative in the EIA-IgG test. The number of IgA-posi-
tive patients increased roughly in parallel to the SAT
titer values, with the P value close to the significance
threshold ( P 0.07). Since IgA titers increase with in-
creased antigenic stimulation, patients having 1/1,280
and 1/640 titers were found to have a greater number of
antibodies. Disagreement between IgM and IgG in the
first 2 titers could be due to the delay in switching from
IgM to IgG caused by antigenic stimulation. White
demonstrated that such a delay was possible (20). The
presence of IgM was revealed when comparing the
decrease in titers of the SAT test and the 2-ME test,
when the latter was performed in sera with total an-
tibody activity shown. This decrease was observed in 55
(59.8z) patients. When compared with results from the
EIA-IgM test, agreement was found to be 84.8z. This
suggests that the 2-ME test can be reliably used to deter-
mine the presence of IgM. Buchanan and Faber report-
ed that a negative 2-ME test is ``strong evidence'' of
chronic brucellosis (21). In a study evaluating 50 sera by
flow assay, Zeytinoglu et al. found a similar agreement
between the EIA-IgM and 2-ME tests, with a ratio of
88z (22).
According to the results of the present study, 6
months avidity maturation time and 50z AI were
found to be the best cut-off values for the avidity test.
Under these conditions, AI values from 4550zmay be
within the grey zone. Further studies investigating other
parameters that may affect the avidity test should be
performed with varied sets of parameters under con-
trolled conditions, in order to determine the most ap-
propriate criteria for application of this test. The other 2
parameters that can be changed in this test are the urea
concentration and treatment time. Based on previous
studies, we choose to use 8 M urea applied for 5 min.
These conditions may vary according to the specific
avidity test to be performed. However, in the diagnosis
of brucellosis, these conditions have not yet been stand-
ardized. In some studies, successful results have been
reported for the diagnosis of Brucella based on IgG
avidity test. In a study of 188 patients, Kutlu et al.
found a statistical correlation between AI and matura-
tion time when the cut-off values for these parameters
were 40z and 6 months, respectively. Furthermore,
when maturation time was set at 6 months, Gutierrez
et al. found the sensitivity and specificity of the IgG
avidity test to be 70.5 and 97.7z, respectively (6).
Montec on et al. found significantly high Brucella IgG
avidity in a group having a history of brucellosis, and
reported that the IgG avidity test could differentiate
between current and prior infections (1).
In conclusion, from a broad perspective, no perfect
test is available for the laboratory diagnosis of brucello-
sis. The RB test remains an important and appropriate
screening test. Furthermore, we believe that the SAT
test, which is cost-effective, easy-to-use, and has high
sensitivity and specificity, is the most appropriate test,
especially in regions endemic for brucellosis.
The ability to measure 3 specific antibodies by EIA
makes this an effective test that can be used to success-
fully diagnose brucellosis. This is especially important,
since it may be possible to use these laboratory tests to
confirm the clinical stage of the disease once the
presence of IgM is apparent during the acute stage.
Likewise, there may be similar value in the presence of
IgG during the chronic stage. To differentiate between
these 2 antibodies, the 2-ME test is a cheap and easy-to-
use alternative that yields sufficient results. Additional
studies aimed at further developing and standardizing
the IgG avidity test may significantly improve the clinic
diagnosis of brucellosis.
Acknowledgments We thank Prof. Dr. Metin Korkmaz for help-
ful suggestions and evaluations and Mehtap Kocan for performing
laboratory tests.
Conflict of interest None to declare.
REFERENCES
1. Mantec on, MA., Guti errez, MP., Zarzosa MP., et al. (2008): In-
fluence of brucellosis history on serological diagnosis and evolu-
tion of patients with acute brucellosis. J. Infect., 57, 397403.
2. Pappas, G., Akritidis, N., Bosilkovski, M., et al. (2005): Brucel-
losis. N. Engl. J. Med., 2, 23252336.
3. Roushan, M.R.H., Amiri, M.J.S., Laly, A., et al. (2010): Follow
up standard agglutination and 2-mercaptoethanol tests in 175
clinically cured cases of human brucellosis. Int. Infect. Dis., 14,
250253.
4. Gomez, M.C., Nieto, J.A., Rosa, C., et al. (2008): Evaluation of
seven tests for diagnosis of human brucellosis in an area where the
disease is endemic. Clin. Vaccine Immunol., 15, 10311033.
5. Aliskan, H. (2008): The value of culture and serological methods
in the diagnosis of human brucellosis. Mikrobiyol. Bul., 42,
276 276
185195 (text in Turkish with English summary).
6. Kutlu, S.S., Celikbas, A., Ergonul, O., et al. (2003): The value of
the immunoglobulin G avidity test for the serologic diagnosis of
brucellosis. Mikrobiyol. Bul., 37, 261267 (text in Turkish with
English summary).
7. Hall, W.H. and Manion, R.E. (1953): Comparison of the
Coombs test with other methods for Brucella agglutinins in hu-
man serum. J. Clin. Invest., 32, 96106.
8. Reddin, J.L., Anderson, R.K., Jenness, R., et al. (1965): Sig-
nificance of 7S and macroglobulin brucella agglutinins in human
brucellosis. N. Engl. J. Med., 272, 12631268.
9. Hedman, K. and Rousseau, S.A. (1989): Measurement of avidity
of specific IgG for verification of recent primary rubella. J. Med.
Virol., 27, 288292.
10. Mesa, J.D.R., Gonzales, J.S. and Reguera, J.M. (2005): Diag-
nostic yield and use for the rapid diagnosis of human brucellosis
in emergency departments in endemic areas. Clin. Microbiol. In-
fect., 11, 221225.
11. Sisirak, M. and Hukic, M. (2009): Evaluation and importance of
selected microbiological methods in the diagnosis of human
brucellosis. Bosn. J. Basic Med. Sci., 9, 198203.
12. Mert, A., Ozaras, R., Tabak, F., et al. (2003): The sensitivity and
specificity of brucella agglutination tests. Diagn. Microbiol. In-
fect. Dis., 46, 241243.
13. Serra, J. and Vi nas, M. (2004): Laboratory diagnosis of brucello-
sis in a rural endemic area in northeastern Spain. Int. Microbiol.,
7, 5358.
14. Sirmatel, F., Turker, M. and Bozkurt, A.I. (2002): Evaluation of
the methods used for the serologic diagnosis of brucellosis.
Mikrobiyol. Bul., 36, 161167 (text in Turkish with English sum-
mary).
15. Klerk, E.D. and Anderson, R. (1985): Comparative evaluation of
the enzyme-linked immunosorbent assay in the laboratory diag-
nosis of brucellosis. J. Clin. Microbiol. 21, 381386.
16. Ariza, J., Pellicer, T., Pallar es, R., et al. (1992): Specific an-
tibody profile in human brucellosis. Clin. Infect. Dis., 14,
131140.
17. Memish, Z.A., Almuneef, M., Mah, M.W., et al. (2002): Com-
parison of the Brucella Standard Agglutination Test with the
ELISA IgG and IgM in patients with Brucella bacteremia. Diagn.
Microbiol. Infect. Dis., 44, 129132.
18. Araj, G.F., Kattar, M.M., Fattouh, L.G., et al. (2005): Evalua-
tion of the PANBIO Brucella immunoglobulin G (IgG) and IgM
enzyme-linked immunosorbent assays for diagnosis of human
brucellosis. Clin. Diagn. Lab. Immunol., 12, 13341335.
19. Ciftci, C., Ozturk, F., Oztekin, A., et al. (2005): Comparison of
the serological tests used for the laboratory diagnosis of brucello-
sis. Mikrobiyol. Bul., 39, 291299 (text in Turkish with English
summary).
20. White, R.G. (1978): Immunoglobulin profiles of the chronic an-
tibody response: discussion in relation to brucellosis infections.
Postgrad. Med. J., 54, 595602.
21. Buchanan, T.M. and Faber, L.C. (1980): 2-Mercaptoethanol
brucella agglutination test: usefulness for predicting recovery
from brucellosis. J. Clin. Microbiol., 11, 691693.
22. Zeytinoglu, A., Turhan, A., Altuglu, I., et al. (2006): Compari-
son of brucella immunoglobulin M and G flow assays with serum
agglutination and 2-mercaptoethanol tests in the diagnosis of
brucellosis. Clin. Chem. Lab. Med., 44, 180184.
You might also like
- Diabetes HandbookDocument198 pagesDiabetes HandbookKeerthana SivarasaNo ratings yet
- Secrets of The SiddhasDocument1 pageSecrets of The SiddhasChiranth ChandNo ratings yet
- LMCC II Compilation Most RecentDocument118 pagesLMCC II Compilation Most RecentEmad Mergan100% (4)
- Handbook of NefrologyDocument244 pagesHandbook of NefrologyPopoviciu Florin MirceaNo ratings yet
- Oet Writing TipsDocument27 pagesOet Writing Tipsbjlk96% (47)
- Guidelines Microbiology Lab ProceduresDocument61 pagesGuidelines Microbiology Lab ProceduresSadao MatsumotoNo ratings yet
- Pedia Disorders Upgraded For Lnu CaDocument6 pagesPedia Disorders Upgraded For Lnu Cashirlenedel cariñoNo ratings yet
- Main 1Document4 pagesMain 1Raya KurniawanNo ratings yet
- Mercado, Marcela - 2020Document9 pagesMercado, Marcela - 2020Omar Cucho GamboaNo ratings yet
- 202 FullDocument4 pages202 FullDesi Suryani DewiNo ratings yet
- 12 Dengue Seroprevalence ComparisonDocument4 pages12 Dengue Seroprevalence ComparisonYipno Wanhar El MawardiNo ratings yet
- Utility of Serological Tests in The Era of Molecular Testing For Diagnosis of Human Brucellosis in Endemic Area With Limited ResourcesDocument4 pagesUtility of Serological Tests in The Era of Molecular Testing For Diagnosis of Human Brucellosis in Endemic Area With Limited ResourcesMiguel Pinedo TrujilloNo ratings yet
- Genexpert - On Body Fluid SpecimensDocument4 pagesGenexpert - On Body Fluid Specimensramo G.No ratings yet
- Jurnal Kulkel HemDocument5 pagesJurnal Kulkel HemAnonymous PrskyT0co6No ratings yet
- JCM 43 8 4194-4196 2005Document3 pagesJCM 43 8 4194-4196 2005Sumesh ShresthaNo ratings yet
- Na 2016Document5 pagesNa 2016abdullahkhilji.nitsNo ratings yet
- Weil-Felix Test in Diagnosis of ScrubDocument3 pagesWeil-Felix Test in Diagnosis of ScrubvyasakandarpNo ratings yet
- TJI-58070 (0) Tam Metin-Revizyon GerçekleştirilmişDocument10 pagesTJI-58070 (0) Tam Metin-Revizyon GerçekleştirilmişcerraheminNo ratings yet
- Msat - A Screening Test For Leptospirosis - Article 8Document3 pagesMsat - A Screening Test For Leptospirosis - Article 8Krishna KumarNo ratings yet
- Understanding Antigen Tests and Results ENG FinalDocument4 pagesUnderstanding Antigen Tests and Results ENG FinalAna CatarinaNo ratings yet
- 4 KNDocument25 pages4 KNMohammad Yusuf AlamudiNo ratings yet
- Mm7019a3 HDocument5 pagesMm7019a3 HShuvo H AhmedNo ratings yet
- Becker-2021-Exploring Beyond Clinical RoutineDocument12 pagesBecker-2021-Exploring Beyond Clinical RoutineNick FloresNo ratings yet
- Performance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsDocument6 pagesPerformance Verification of Anti-Sars-Cov-2-Specific Antibody Detection by Using Four Chemiluminescence Immunoassay SystemsadnanNo ratings yet
- Bmri2016 8905675Document9 pagesBmri2016 8905675helderjamsNo ratings yet
- Serum Iga, Igm, and Igg Responses in Covid-19: Cellular & Molecular ImmunologyDocument3 pagesSerum Iga, Igm, and Igg Responses in Covid-19: Cellular & Molecular ImmunologynpidasNo ratings yet
- Comparison of Real-Time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) and Igm-Igg Antibody Test For The Diagnosis of Sars-Cov-2 InfectionDocument18 pagesComparison of Real-Time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) and Igm-Igg Antibody Test For The Diagnosis of Sars-Cov-2 InfectionRizki AzpiNo ratings yet
- Img#Document5 pagesImg#AngelNo ratings yet
- 10 BlythDocument6 pages10 BlythAvis UnsoedNo ratings yet
- Critical AppraisalDocument20 pagesCritical AppraisalTuty NoviantyNo ratings yet
- Evaluation Serological Diagnostic Indices For Mucocutaneous Leishmaniasis: Immunofluorescence and Enzyme-Linked For Igm and Iga AntibodiesDocument6 pagesEvaluation Serological Diagnostic Indices For Mucocutaneous Leishmaniasis: Immunofluorescence and Enzyme-Linked For Igm and Iga AntibodiesnisaNo ratings yet
- Journal of Clinical Virology: SciencedirectDocument6 pagesJournal of Clinical Virology: SciencedirectVictor VargasNo ratings yet
- Laboratory Diagnosis For DengueDocument4 pagesLaboratory Diagnosis For DengueHamid RazaNo ratings yet
- Immunodiagnosis of Tuberculosis: An Update on Antibody Detection MethodsDocument5 pagesImmunodiagnosis of Tuberculosis: An Update on Antibody Detection MethodsPROFE EFRA LAGRANGENo ratings yet
- Dengue ICT NS1 PDFDocument7 pagesDengue ICT NS1 PDFAsti Rizki Arum PermanaNo ratings yet
- Significance and Value of The Widal Test in The Diagnosis of Typhoid Fever in An Endemic AreaDocument6 pagesSignificance and Value of The Widal Test in The Diagnosis of Typhoid Fever in An Endemic AreaDavide BorgesNo ratings yet
- Anti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsDocument6 pagesAnti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsdhairyasheelNo ratings yet
- Avb 2005074010051Document8 pagesAvb 2005074010051Saray CorredorNo ratings yet
- Pooling of Samples For Sars-Cov-2 Detection Using A Rapid Antigen TestDocument5 pagesPooling of Samples For Sars-Cov-2 Detection Using A Rapid Antigen TestErickson OngNo ratings yet
- Basic Problems of Serological Laboratory DiagnosisDocument37 pagesBasic Problems of Serological Laboratory DiagnosisSuzan MatarNo ratings yet
- (IJCST-V4I4P22) : Elena Trajkovska-Dokic, Snezana Stojkovska, Milena Petrovska, Nikola PanovskiDocument4 pages(IJCST-V4I4P22) : Elena Trajkovska-Dokic, Snezana Stojkovska, Milena Petrovska, Nikola PanovskiEighthSenseGroupNo ratings yet
- Detection of Typhoid CarriersDocument6 pagesDetection of Typhoid CarriersClarestaNo ratings yet
- Comparison of The HIV 1 Specific Immunoglobulin GDocument5 pagesComparison of The HIV 1 Specific Immunoglobulin GAlex MorwabeNo ratings yet
- Simon 2004Document12 pagesSimon 2004mr_curiousityNo ratings yet
- Clinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part IDocument5 pagesClinical Microbiology Newsletter: Genexpert Testing: Applications For Clinical Microbiology, Part ImagicianchemistNo ratings yet
- Serum Procalcitonin and C-Reactive Protein Levels As Markers of Bacterial Infection: A Systematic Review and Meta-AnalysisDocument12 pagesSerum Procalcitonin and C-Reactive Protein Levels As Markers of Bacterial Infection: A Systematic Review and Meta-AnalysissyahputriNo ratings yet
- Eurosurv 27 42 5Document13 pagesEurosurv 27 42 5Eben Leonel Albano MaiopueNo ratings yet
- Usefulness of Centor Score To Diagnosis of Group A Streptococcal Pharyngitis and Decision Making of Antibiotics UseDocument7 pagesUsefulness of Centor Score To Diagnosis of Group A Streptococcal Pharyngitis and Decision Making of Antibiotics UseAgus karsetiyonoNo ratings yet
- Rapid Diagnostic Tests Versus RT-PCR For Ebola Virus Infections: Systematic Review and Meta-AnalysisDocument24 pagesRapid Diagnostic Tests Versus RT-PCR For Ebola Virus Infections: Systematic Review and Meta-Analysissri wahyuniNo ratings yet
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroNo ratings yet
- Diagnostic Value of Serological Tests (IgA, IgG, IgM)Document4 pagesDiagnostic Value of Serological Tests (IgA, IgG, IgM)Gustomo PanantroNo ratings yet
- Anti-C1q Antibodies: Association With Nephritis and Disease Activity in Systemic Lupus ErythematosusDocument5 pagesAnti-C1q Antibodies: Association With Nephritis and Disease Activity in Systemic Lupus ErythematosusAlisNo ratings yet
- An Early Evaluation On The Usefulness of NS1 Antigen-Capture ELISA Versus IGM ELISA TEST For The Diagnosis of Acute Dengue InfectionDocument10 pagesAn Early Evaluation On The Usefulness of NS1 Antigen-Capture ELISA Versus IGM ELISA TEST For The Diagnosis of Acute Dengue Infectionkurniawan naryoNo ratings yet
- Volume Incidence Immunofluorescence Patterns Specific Autoantibodies 3183allasp1Document9 pagesVolume Incidence Immunofluorescence Patterns Specific Autoantibodies 3183allasp1osnolaromero4No ratings yet
- LeptospirosisDocument8 pagesLeptospirosisSanda Puspa RiniNo ratings yet
- Immunological Tests Essential and Supportive Tools in The Fight Against COVID-19Document62 pagesImmunological Tests Essential and Supportive Tools in The Fight Against COVID-19Gaspar PonceNo ratings yet
- Sepsis 2019Document12 pagesSepsis 2019EviNo ratings yet
- Prevalence of Mec A Gene Positive Coagulase Negative StaphyloDocument6 pagesPrevalence of Mec A Gene Positive Coagulase Negative Staphylosuresh151971No ratings yet
- 1-s2.0-S2212553112000908-mainDocument5 pages1-s2.0-S2212553112000908-mainbiopluslabo1No ratings yet
- Aqac126 303Document2 pagesAqac126 303Starix UkrNo ratings yet
- Fungi: Galactomannan and 1,3-β - Glucan Testing for the Diagnosis of Invasive AspergillosisDocument8 pagesFungi: Galactomannan and 1,3-β - Glucan Testing for the Diagnosis of Invasive AspergillosisntnquynhproNo ratings yet
- India CoulterDocument6 pagesIndia CoulterzainabNo ratings yet
- Sars-Cov-2 Seroconversion in Humans: A Detailed Protocol For A Serological Assay, Antigen Production, and Test SetupDocument15 pagesSars-Cov-2 Seroconversion in Humans: A Detailed Protocol For A Serological Assay, Antigen Production, and Test SetupAKNTAI002No ratings yet
- 7916 24362 1 PBDocument5 pages7916 24362 1 PBAchmad DainuriNo ratings yet
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalFrom EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalNo ratings yet
- Rapid On-site Evaluation (ROSE): A Practical GuideFrom EverandRapid On-site Evaluation (ROSE): A Practical GuideGuoping CaiNo ratings yet
- LancetID Piafrancoetal Human Brucellosis 2007Document12 pagesLancetID Piafrancoetal Human Brucellosis 2007Abby Pérez Sa.No ratings yet
- Brucellosis - Review On The Recent Trends in Pathogenicity and Laboratory DiagnosisDocument8 pagesBrucellosis - Review On The Recent Trends in Pathogenicity and Laboratory DiagnosisJoshua SmithNo ratings yet
- Pistopoiitiko ThanatouDocument2 pagesPistopoiitiko ThanatouJoshua SmithNo ratings yet
- 1Document8 pages1Joshua SmithNo ratings yet
- Clinical Approach To Isolated Splenomegaly: M M, P M, R KDocument5 pagesClinical Approach To Isolated Splenomegaly: M M, P M, R KlilisNo ratings yet
- Proses TGL 29Document12 pagesProses TGL 29TuraaNo ratings yet
- Posterior Retroperitoneoscopic AdrenalectomyDocument14 pagesPosterior Retroperitoneoscopic AdrenalectomyShreyNo ratings yet
- (Amanda J. Jenkins) Drug Testing in Alternate BiolDocument200 pages(Amanda J. Jenkins) Drug Testing in Alternate Bioljonathan sinartaNo ratings yet
- 1 SMDocument7 pages1 SMPiaggio PIAGGIONo ratings yet
- Minor Surgical Procedures in Maxillofacial SurgeryDocument65 pagesMinor Surgical Procedures in Maxillofacial SurgerydrzibranNo ratings yet
- OrganTrade ProefschriftFrederikeAmbagtsheer PDFDocument225 pagesOrganTrade ProefschriftFrederikeAmbagtsheer PDFJanani SankarNo ratings yet
- Hypohydrotic Ectodermal DysplasiaDocument1 pageHypohydrotic Ectodermal DysplasiamaddooNo ratings yet
- ASHHNA Competency Standards For Sexual and Reproductive Health and HIV NursesDocument30 pagesASHHNA Competency Standards For Sexual and Reproductive Health and HIV NursesRNdrei dela CruzNo ratings yet
- Diagnosis-Pedrosa, Joan ADocument27 pagesDiagnosis-Pedrosa, Joan AJoan Alde PedrosaNo ratings yet
- Delivery of Evidence-Based Treatment For Multiple Anxiety Disorders in Primary Care: A Randomized Controlled TrialDocument5 pagesDelivery of Evidence-Based Treatment For Multiple Anxiety Disorders in Primary Care: A Randomized Controlled TrialRaja DarmawanNo ratings yet
- Comprehensive Edited)Document82 pagesComprehensive Edited)mikrobyo_ng_wmsuNo ratings yet
- Jurnal AnestesiDocument5 pagesJurnal AnestesiridwanNo ratings yet
- 2016 ProgramDocument30 pages2016 ProgramctyvteNo ratings yet
- Cardiovascular Risk Factors of Hypertension, Smoking and Obesity: Emerging Concerns Among Pathan and Persian Young Adults?Document5 pagesCardiovascular Risk Factors of Hypertension, Smoking and Obesity: Emerging Concerns Among Pathan and Persian Young Adults?-No ratings yet
- Post-Partum HemorrhageDocument15 pagesPost-Partum Hemorrhageapi-257029163No ratings yet
- WNHS OG PregnancyFirstTrimesterDocument60 pagesWNHS OG PregnancyFirstTrimesterBharata YudhaNo ratings yet
- Mongolian SpotsDocument9 pagesMongolian SpotsiekafzNo ratings yet
- Journal Review2Document7 pagesJournal Review2api-589685298No ratings yet
- CASE PRES PreeclampsiaDocument51 pagesCASE PRES PreeclampsiaRaiza Love Caparas-PablicoNo ratings yet
- Drug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesDocument2 pagesDrug Name Brand Name Classification Dosage Indications Side/ Adverse Effects Nursing ResponsibilitiesRonald BurkeNo ratings yet
- Ayushman Bharat hospitals in BangaloreDocument163 pagesAyushman Bharat hospitals in BangaloreShreedhar KadkolNo ratings yet
- Trapdoor Effect Cause and CorrectionsDocument4 pagesTrapdoor Effect Cause and CorrectionsMarcelo BarberoNo ratings yet
- Opportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaDocument4 pagesOpportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaPinay YaunNo ratings yet