Professional Documents
Culture Documents
ClinicalpracticePart2 3
Uploaded by
Persis NairOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ClinicalpracticePart2 3
Uploaded by
Persis NairCopyright:
Available Formats
Chapter 3 - Indication and contraindications of implant treatment
General Manager of Department of Dentistry, Oral and Maxillofacial Surgery, Machida
Municipal Hospital
Takefumi Ogasawara
Associate Professor of Department of Oral and Maxillofacial Surgery,
Tokyo Medical University Hospital
Tomoaki Inou
I. Assessing the suitability of the case for implant treatment
The implant treatment has become widely applied globally, and has become acknowledged as the general
dental treatment procedures. The 21
st
century can be said to be the shift in the predominance by the
denture treatment to implant treatment and should be considered as the treatment option for the cases of
tooth loss. The recent advances in the medical care have enabled control of various systemic diseases and
help the patients in the everyday life and have lengthened their survival. Although various information
regarding the patient have to be gained via an intimate communication with the doctor in charge of the
patient, it is the role of the dental practitioner to analyze the gathered information, grasp the patient
condition in order to judge the suitability of the implant treatment. Regarding the localized bone quantity
and quality determined from the imaging analysis gave been discussed in the previous chapter therefore
will mention of the analysis of the systemic indications.
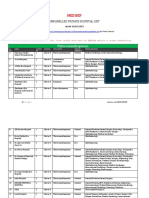
The knowledge and understanding of the values of basic systemic analyses that frequents the scene of
blood tests (Table 2-3-1) are essential. I will not go into depth, but these numerical values act as
important indicators, not only for the suitability of the implant treatment, but also the postoperative
infections, and predict any problems to arise with the wounding healing process. The Table 2-3-2 shows
the risk classifications for the invasive procedures that have been utilized in the outpatient hematology
clinic in the Department of dental surgery, Tokyo Medical University Hospital. In the risks classed in
terms of likeliness of infection and bleeding, Class I, indicate normal level, and Class II required caution,
but where there are no other abnormal signs, surgery can be performed. Whereas with the Class III
should be dealt with the possibility of delaying the surgical procedure. The ranges of the values should be
interpreted such that the reduction in the level of total protein or albumin should indicate decrease in the
rate of wound healing, or diabetes should be suspected where an abnormal level of HbA1c has been
presented.
II. Contraindications
The implant treatment has been said to be one that has no absolute contraindications, however there are
cases amongst the systemic disease where the perioperative and postoperative managements become
complicated. In order to limit the risks to the minimum, and to maximize the success of the treatment, it
is essential to communicate with the doctor specializing in internal medicines, and fully understand the
systemic conditions of the patient from the information gained in order to judge the suitability of implant
treatment.
A. Systemic contraindications and conditions where special attention is required
1. Systemic contraindications for general implant treatment
Severe blood diseases (hemophilia etc.)
Contents Normal level
Hematologic test
White blood count (WBC) 3,0008,000 /l
Neutrophil 4274%
Red blood count (RBC) 3,700,0005,400,000 /l
Hematocrit (Ht) 34.049.0%
Hemoglobin (Hb) 11.017.0 g/dl
Blood platelet count (PLT) 150,000350,000 /
Biochemical test
GOT 38 U/l
GPT 444 U/l
- GTP 1673 U/l
LDH 106211U/l
Total protein 6.68.2 g/dl
Albumin (ALB) 4.05.2 g/dl
Urea nitrogen 8.022.6 mg/dl
Creatinine 0.61.1 mg/dl
Blood sugar 60110 mg/dl
HbA1c 4.35.8
Coagulation test
PT-INR (PT: Prothrombin Time) 1.0 0.1
Activated partial thronboplastin time (APTT) 30.0 5.0 seconds
FDP < 4.0 g/ml
Table 2-3-1 Examination criteria
I II III
1. White blood count** > 2000 2000-1000 <1000
2. Neutrophil count* > 1000 999-500 < 500
3. Blood platelet count** > 150 149-50 < 50
4. Hb***
male > 12 12-10 < 10
female > 10 10-8 < 8
5. PT-INR < 1.2 1.2-1.5 < 1.5
6. APTT Normal Delay < 30 % Delay > 30 %
7. FDP Normal Slight outlier High outlier
8. Hepatorenal function Normal Slight outlier High outlier
(*/l, ** 10
3
/l, *** mg/dl)
Table 2-3-2 Risk classifications for invasive procedures
The patient is to be classed in the high category if even one factor fits with the criteria.
Myocardial infarction: within six months of an attack
Cerebral infarction and cerebral apoplexy: In cases where the condition of the disease is serious and
the patient are concurrently taking anticoagulants.
Severe immunodeficiency
Patients who are undergoing strong chemotherapy
Severe neuropsychiatric disease, mental disability, and narcotic drug addicts
Patients who are concurrently taking bisphosphonates
Youths under the age of 15
2. Systemic conditions that require special attention in implant treatment
Be aware of any postoperative infection, abnormality in blood coagulation, and of any delay in wound
healing.
a. In case of bleeding
(1) Idiopathic thrombocytopenic purpura
It is necessary to note the number of platelets, as the long-term steroidal uses have been associated with
osteoporosis.
(2) Aplastic anemia and leukemia
In addition to concern as to the postoperative infection and bleeding, the future treatment plan should be
re-considered.
(3) Hemophilia
Bleeding during the procedure can be controlled with the application of blood products in the case of mild
hemophilia, but corporation of the medical doctor is required. The outcome of these cases have not been
satisfactory, and they have often resulted in the falling out of the fixtures
(4) Patients taking anticoagulants (proprietary name Warfarin)
Decide on the suitability of implant treatment using the PT-INR
as the reference.
(5) Patients taking antiplatelet agents (proprietary name Bayaspirin, Bufferin for children, Panaldine,
Plavix, and Pletaal)
Monitor the blood platelet count and their functions. The reduction in the platelet counts can result in
bleeding and abnormal blood coagulation.
b. In case of infection
This is of particular importance to consider in the patients with leucopenia, and HIV but the incidence of
postoperative infection has been found to be the highest in diabetics. Whether the diabetic patient is
undergoing oral medical treatment or with insulin injection can determine the extent of the condition,
however, the control of the illness is the requirement for conducting implant treatment. HbA1c less than
7% indicates well controlled condition, and range between 7 and 9% been indicated to be the general
range.
c. Osteoporosis
Not all of osteoporosis are contraindicated for implant treatment. Bone density measurement may be
necessary in some cases but it has been reported that normal level of bone metabolism is still possible
with only a third of the regular amount. The concomitant use of bisphosphonates as the treatment drug
has led to an accelerated number of cases resulting in jaw bone necrosis in the recent years therefore the
implant treatment has become contraindicated in patients currently undergoing a course of
bisphophonates.
d. Angina pectoris
The implant treatment has been indicated for patients who have not had the attack within the last one to
two months, or even then if the condition is considered to be relatively light, the treatment is still possible.
In the case of frequent angina attacks, it might be best to avoid undergoing surgery. In any case, the
decision and treatment planning should be conducted with the medical doctor in a coordinated manner.
e. Myocardial infarction, cerebral infarction and stroke
The implant treatment can be performed for those who have not had heart attack in the last six months,
without presentation of any complications. As for the cases of cerebral infarction and stroke, the
suitability of the implant procedure should be judged on the disease state and the medications. In any
case, the decision and treatment planning should be conducted with the medical doctor in a coordinated
manner.
f. Hypertension
Hypertension is diagnosed when the systolic blood pressure (BP) becomes over 140 mmHg and the
diastolic BP becomes over 90 mmHg (140/90 mmHg). These patients should be referred to the medical
doctor nearby for the BP control, before initiating the implant surgery. During surgery, measures such as
the administration of minor tranquillizers from the day before, or relaxing the patient during surgery to
avoid the rise in the BP are necessary.
The patient should be monitored for their BP, pulse and use electrocardiograms, and the implant surgery
may best be discontinued if the BP rises over 200/120 mmHg.
The conventional sublingual administration of nifedipine (product name Adalat) has been
contraindicated as a general rule for the implant treatment due to the risk of inducing rapid fall in BP
and reflex tachycardia. If the use is inevitable, an antihypertensive that has been indicated for cases of
emergency via intravenous administration should be applied (E.g. continuous infusion of perdipine
(product name) at 0.5g/kg/min).
g. Uncooperative patients
This is evidently not a systemic condition, even then intraoperative and postoperative managements can
be made difficult.
*1 As a screening test procedure, the platelet count (Normal range: 15- 3510
4
/l), PT (prothrombin
time, normal range: 10- 13 sec) and PTT (partial thromboplastin time, normal range: 28 to 34 sec) have
been the standard values for analysis in the past, but the standard reference has been shifted to the use
of international normalized ratio (INR) that is calculated from the PT. The INR is the ratio of a patient's
prothrombin time to a normal (control) sample, raised to the power of the ISI value for the analytical
system used. A normal person has the INR of 1.0. Provided that the platelet count and APTT values are
within the normal range, hemostasis is possible in small invasive surgery by the application of suture,
electrocoagulation or with local coagulants (thrombin, gelatin, oxidized cellulose) even if the INR value is
1.5 to 2.5 (to be more precise, <3.5)
B. Local contraindications and conditions where special attention is required
1. Contraindications of local conditions for general implant treatment
Insufficient bone quantity, but where bone augmentation procedures with bone graft is not possible.
Intractable periodontitis and serve periodontal disease (cases where improvements in oral hygiene
does not recover the disease condition)
High exposure to radiation
Chronis osteomyelitis
2. Localized conditions that require special attention in implant treatment
Mouth-closing disorder (temporomandibular joint disorder, temporomandibular joint ankylosis,
post-tumour resection)
Bruxism
Smoking (heavy smoker)
Drying of oral cavity (dry mouth, Sjgren syndrome, and other xerostomias)
Poor oral hygiene
Uncooperative patients who have no understanding of the need for a regular follow-up.
References
1) Suda T, Ozawa H, and others eds. Bone Biology. Tokyo. Ishiyaku Pub, Inc. 2007. (in Japanese)
2) Igari J, Nakahara K eds. Standard Laboratory medicine. Tokyo. Igaku-Shoin Ltd. 2006. (in Japanese)
3) Yamazaki M, Takahashi T, and others. Ultimate Guide IMPRANTS. Tokyo. Ishiyaku Pub, Inc. 2006.(in
Japanese)
4) Watzek G: Implants in Qualitatively compromised bone. Quintessence Publishing Surry, UK, 2004.
5)Renouard F, Rangert B. Translation by Maeda Y, Yonehata Y.Risk factors in implant dentistry.
Tokyo. Quintessence Publishing Co., Ltd. 2000. (in Japanese)
6) Misch CE: Bone density; a key determinant for clinical success. Contemporary implant dentistry, 2
nd
ed, Mosby, St Louis, 1999.
7) Lekholm U, Zarb GA: Patient selection and preparation. In Branemark P-I, ZarbGA, Alberktsson
T(eds). Tissueintegrated prostheses: Osseointegration in clinical Dentistry. Quintessence, Chicago, 1985.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Personal Protective EquipmentDocument3 pagesPersonal Protective EquipmentPersis NairNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Diagnosis of Crack On ToothDocument5 pagesDiagnosis of Crack On ToothPersis NairNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Guidelines For Sedation AapdDocument17 pagesGuidelines For Sedation AapdPersis Nair100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- H1localane PDFDocument20 pagesH1localane PDFMohammed FeroNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Erythema DoseDocument4 pagesErythema DosePersis NairNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- About Implant PartsDocument16 pagesAbout Implant PartsPersis Nair100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Tic BookDocument19 pagesTic BookPersis NairNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Adult Health (Integration)Document26 pagesAdult Health (Integration)L1NEDS DNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Epididymal CystDocument6 pagesEpididymal CystShree Kumar MishraNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- HBP 2022Document203 pagesHBP 2022NoneNo ratings yet
- Zygomatic ImplantsDocument3 pagesZygomatic ImplantsDeb SNo ratings yet
- International Patient Safety GoalsDocument30 pagesInternational Patient Safety GoalsMuvenn Kannan50% (2)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Zeenat Amna Azhar CVDocument2 pagesZeenat Amna Azhar CVvapigih769No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- CHOLECYSTECTOMYDocument35 pagesCHOLECYSTECTOMYfaitheee100% (3)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Scalpel: Common Surgical InstrumentsDocument40 pagesScalpel: Common Surgical InstrumentsAli IgnacioNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- WHODocument142 pagesWHONers KeperawatanNo ratings yet
- Jamafacial Chen 2019 Oi 190014Document7 pagesJamafacial Chen 2019 Oi 190014Krzysztof FejdaszNo ratings yet
- Pyogenic Liver AbscessDocument5 pagesPyogenic Liver AbscessPatcharaporn Fern KlongklaewNo ratings yet
- Total Ankle ReplacementDocument21 pagesTotal Ankle ReplacementfaizahNo ratings yet
- Chola Ms Family Healthline Insurance PolicyDocument40 pagesChola Ms Family Healthline Insurance Policyhappy39No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- HTTP WWW - Apic.org AM Template - CFM Template CM Content DisplayDocument14 pagesHTTP WWW - Apic.org AM Template - CFM Template CM Content Displayvo_bartNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Issue 30 - The Nurse Advocate - Hamad Medical Corporation - December 2017Document20 pagesIssue 30 - The Nurse Advocate - Hamad Medical Corporation - December 2017Brent ForemanNo ratings yet
- 2 - Laparoscopic SplenectomyDocument8 pages2 - Laparoscopic SplenectomyAmor KourdouliNo ratings yet
- Plastic Surgery Marketing in The 21st Century: An A-Z GuideDocument44 pagesPlastic Surgery Marketing in The 21st Century: An A-Z Guidevagabond2010No ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- A Prospective Randomized Multicenter Trial Comparing Clinical Outcomes of Patients Treated Surgically With A Static or Dynamic Implant For Acute Ankle Syndesmosis RuptureDocument8 pagesA Prospective Randomized Multicenter Trial Comparing Clinical Outcomes of Patients Treated Surgically With A Static or Dynamic Implant For Acute Ankle Syndesmosis RuptureJake sanchezNo ratings yet
- AmputationDocument75 pagesAmputationFaith LoveNo ratings yet
- Shanavas MEDISEP Hospitals 2023 18.02.23Document47 pagesShanavas MEDISEP Hospitals 2023 18.02.23Abhi BalaNo ratings yet
- proGAV2.0 TA013871 SOP-AIC-5001399Document22 pagesproGAV2.0 TA013871 SOP-AIC-5001399LouisWangNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Scope Vet Assistant Duties PDFDocument70 pagesScope Vet Assistant Duties PDFSandri Alexandra NegreanuNo ratings yet
- Mobile C-Arm: Oec Flexiview 8800Document135 pagesMobile C-Arm: Oec Flexiview 8800mauro_2912100% (1)
- STOMA COMPLICATIONS: CAUSES AND TREATMENTDocument35 pagesSTOMA COMPLICATIONS: CAUSES AND TREATMENTAlex Ciorogar100% (1)
- Ramesh Chandra Agarwal Vs Regency Hospital LTD SC 2009 Expert Opinion Can Not Be Accepted Without ExaminationDocument18 pagesRamesh Chandra Agarwal Vs Regency Hospital LTD SC 2009 Expert Opinion Can Not Be Accepted Without ExaminationYatn BangadNo ratings yet
- Daes 2016Document2 pagesDaes 2016pancholin_9No ratings yet
- Uso de Guía Aintree para Intubación Con FibroscopioDocument1 pageUso de Guía Aintree para Intubación Con Fibroscopio1cucu0No ratings yet
- Experienced orthopaedic surgeon and directorDocument3 pagesExperienced orthopaedic surgeon and directorHospital BhiwaniNo ratings yet
- Step-by-Step Guide - Key Steps in A MIS TLIF Procedure PDFDocument11 pagesStep-by-Step Guide - Key Steps in A MIS TLIF Procedure PDFAlvaro Perez Henriquez100% (2)
- Section Editor: Steven A. Newman, MD: J Neuro-Ophthalmol, Vol. 28, No. 4, 2008Document10 pagesSection Editor: Steven A. Newman, MD: J Neuro-Ophthalmol, Vol. 28, No. 4, 2008Jessica Leika MatibagNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)