Professional Documents
Culture Documents
Nej MR A 1216008
Uploaded by
guillosarahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nej MR A 1216008
Uploaded by
guillosarahCopyright:
Available Formats
review article
The new engl and journal o f medicine
n engl j med 371;2 nejm.org july 10, 2014
150
Edward W. Campion, M.D., Editor
Mold Infections of the Central
Nervous System
Matthew McCarthy, M.D., Axel Rosengart, M.D., Ph.D., M.P.H.,
Audrey N. Schuetz, M.D., Dimitrios P. Kontoyiannis, M.D., Sc.D.,
and Thomas J. Walsh, M.D.
From the Transplantation-Oncology Infec-
tious Diseases Program, Departments of
Medicine, Pediatrics, and Microbiology and
Immunology (M.M., T.J.W.), and the De-
partments of Neurology, Neuroscience,
and Neurosurgery (A.R.) and Pathology
and Laboratory Medicine (A.N.S.), Weill
Cornell Medical Center of Cornell Univer-
sity, New York; and the Infectious Diseases
Department and Division of Internal Med-
icine, University of Texas M.D. Anderson
Cancer Center, Houston (D.P.K.). Address
reprint requests to Dr. Walsh at the
Transplantation-Oncology Infectious Dis-
eases Program, Weill Cornell Medical Cen-
ter of Cornell University, 1300 York Ave.,
Rm. A-421, New York, NY 10065, or at
thw2003@med.cornell.edu.
N Engl J Med 2014;371:150-60.
DOI: 10.1056/NEJMra1216008
Copyright 2014 Massachusetts Medical Society.
T
he recent outbreak of Exserohilum rostratum meningitis linked to
epidural injections of methylprednisolone acetate has brought renewed at-
tention to mold infections of the central nervous system (CNS).
1
Although
uncommon, these infections are often devastating and difficult to treat. This focused
review of the epidemiologic aspects, clinical characteristics, and treatment of mold
infections of the CNS covers a group of common pathogens: aspergillus, fusarium,
and scedosporium species, molds in the order Mucorales, and dematiaceous molds.
Infections caused by these pathogen groups have distinctive epidemiologic profiles,
clinical manifestations, microbiologic characteristics, and therapeutic implications,
all of which clinicians should understand.
Common Features
Molds are ubiquitous organisms found in soil, water, and decaying vegetation.
2
All
have septate, angular, branching hyphae in tissue, with the exception of those in the
order Mucorales, which have broad, ribbonlike, nonseptate or hyposeptate hyphae
(Fig. 1). The respiratory tract is usually the portal of entry, with subsequent hema-
togenous dissemination to the CNS. However, direct inoculation of CNS or para-
spinal tissue as a result of surgery, trauma, intravenous drug use, or contaminated
medical supplies may also occur in immunocompetent persons, including those
infected with Exophiala dermatitidis (formerly known as Wangiella dermatitidis) and
E. rostratum.
3
Organisms may also spread to the CNS from adjacent structures, in-
cluding the sinuses, mastoid, and orbit. Infection of the ethmoid sinuses may lead
to cavernous sinus thrombosis as a result of invasion of the emissary veins that
drain the sinuses. Hyphae can invade from the ethmoid sinuses through the lamina
papyracea and into the periorbital space, thus threatening the eye, extraocular
muscles, and posterior apical structures, including the optic nerve.
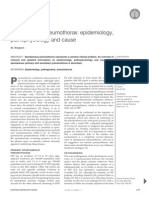
Angioinvasion is common in immunocompromised patients and accounts for
the hematogenous dissemination from the lungs that causes focal neurologic
deficits (Fig. 2). Histopathological examination of involved brain tissue reveals
hyphal angioinvasion with thrombosis in small and large vessels, hemorrhagic
infarction, and coagulative necrosis, as well as vasculitis and granuloma forma-
tion. Susceptibility to angioinvasion also confers a predisposition to the formation
of mycotic aneurysms. Without effective management, mold infections of the CNS
carry poor prognoses, particularly in immunocompromised patients; such patients
may present with isolated brain abscesses that simulate tumors of the CNS.
There are four cornerstones of the management of mold infections of the CNS:
early diagnosis, administration of antifungal chemotherapy, neurosurgical assessment
and intervention, and management of immunologic impairment. Figure 1 outlines
the comparative epidemiologic profiles, clinical characteristics, laboratory features,
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Mold Infections of the Central Nervous System
n engl j med 371;2 nejm.org july 10, 2014
151
and neuroimaging features of mold infections of
the CNS. Early diagnosis may allow for timely
therapeutic intervention and prevention of neuro-
logic sequelae. Computed tomography (CT) and
magnetic resonance imaging (MRI) are impor-
tant adjuncts in the detection of infection and in
monitoring the course of therapy. Patients who
are at risk or who have documented invasive
mold infection of the lungs or sinuses should be
evaluated with the use of neuroimaging if they
have any neurologic signs or symptoms. Patients
with intracranial lesions suggestive of fungal
abscesses or granulomas may be candidates for
stereotactic biopsy.
Two distinct patterns characterize mold infec-
tions of the CNS. In some patients, the disease
arises by direct extension from the paranasal si-
nuses, eye, or middle ear, causing a single abscess
or a few abscesses.
4,5
These lesions usually occur
in the frontal or temporal lobe. Other patients
have hematogenous infection, which may lead to
solitary or multiple small abscesses that are of-
ten seen at the junction of cerebral gray and
white matter and in the putamenstriatal arterial
distribution. Mycotic aneurysms may form and
rupture, which creates the potential for hemor-
rhagic strokes, subarachnoid hemorrhage, and
empyema formation.
Early Diagnosis
Detection of galactomannan antigen and 1,3--d-
glucan in cerebrospinal fluid (CSF) may be helpful
in establishing the diagnosis of CNS aspergillo-
sis or other mold infections, such as fusariosis.
6,7
However, because galactomannan antigen and
1,3--d-glucan can also be expressed by fusari-
um species, its presence in CSF does not consti-
tute a definitive diagnosis of CNS aspergillosis
8
;
1,3--d-glucan may also be expressed by scedo-
sporium species and Exserohilum ros tratum. A poly-
merase-chain-reaction assay that is specific for
aspergillus also may prove useful, but standard-
ized platforms are lacking.
9
Antifungal Therapy
Table 1 outlines therapeutic interventions for mold
infections of the CNS. The arsenal against these
infections includes three classes of antifungal
agents: polyenes (amphotericin B formulations),
triazoles (voriconazole, itraconazole, and posa-
con azole), and echinocandins (caspofungin, mi-
cafungin, and anidulafungin). Voriconazole is
the primary agent for the treatment of CNS as-
pergillosis.
12
Amphotericin B and its lipid formu-
lations are first-line agents for the treatment of
mucormycosis. The roles of other triazoles and
echinocandins in the treatment of mold infec-
tions of the CNS have not been well defined.
Antifungal agents vary widely in their distri-
bution in the CSF.
13
Voriconazole is a relatively
small (349-dalton), moderately lipophilic mole-
cule with a concentration in CSF that is approxi-
mately 50% of its concentration in plasma, in
both animals and humans. Other antimold tri-
azoles, such as posaconazole and itraconazole
(708 and 705 daltons, respectively), are highly lipo-
philic molecules with negligible concentrations in
CSF. Amphotericin B (923 daltons) and its lipid
formulations have relatively limited distribution
in the CSF, but they do have detectable concen-
trations that are at or above inhibitory concentra-
tions within brain parenchyma. Echinocandins
are larger cyclic hexapeptide molecules (1140 to
1292 daltons) with relatively low or undetectable
concentrations in CSF. The administration of
antifungal agents through a ventriculostomy or by
the intrathecal route is not recommended because
of local toxic effects and a lack of proven efficacy.
Neurosurgical Assessment and Intervention
The clinical characteristics of mold infections of
the CNS warrant assessment for possible biopsy
and neurosurgical intervention (Table 2). A de-
finitive diagnosis almost invariably requires a
biopsy, with prompt inspection of the specimen
by means of wet-mount preparation with calco-
fluor white stain, culture, and histologic analysis
(with Gomori methenamine silver stain and peri-
odic acidSchiff stain). In situ hybridization and
immunohistochemical analysis may be helpful if
cultures of biopsy specimens are negative. Be-
cause brain biopsies are highly invasive and may
lead to neurologic deficits, they are often not fea-
sible; therefore, diagnosis of a mold infection of
the CNS is more often made by inference based
on the recovery of the pathogen from a pulmo-
nary or sinus source in a patient who has a CNS
lesion that is radiologically consistent with a
mold infection.
If the patient has a hemispheric ischemic
stroke that is thought to be due to invasive fun-
gal infection, and if the patients clinical condi-
tion that is, coexisting conditions, coagula-
tion status, and overall health status permits,
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The new engl and journal o f medicine
n engl j med 371;2 nejm.org july 10, 2014
152
Mold
Mold Taxon and Common
Features Used for Identification
Dematiaceous Mold
Aspergillus fumigatus
Calcofluorpotassium hydroxide
fluorescent stain: Thin, septate
hyphae of A. fumigatus are
seen on this direct smear of a
brain-biopsy sample.
Mucor circinelloides
LPCB: The hyphae are broad,
ribbonlike, and hyposeptate. Two
large, round sporangia (arrows)
contain many spores. Rhizoids are
absent.
Scedosporium apiospermum
Front of inhibitory mold agar plate
showing dark, mouse-gray
colonies.
Scedosporium prolificans
LPCB: Hyphae are septate, and
the conidiogenous cell has a
swollen base (arrow) and elongat-
ed neck. Conidia with truncated
bases form in clusters at the apex
of the conidiogenous cell.
Fusarium species
Sabouraud dextrose agar
showing yellow-orange colonies.
Cladophialophora bantiana
LPCB: Long, wavy chains of
smooth, oval conidia (arrow)
extend from the conidiophore.
The brown pigment of the conidia
and hyphae is apparent.
Ochroconis gallopava
LPCB: The conidiophore (thin
arrow) extends from a septate
hypha. The two-celled, oval
conidium (wide arrow) extends
from the conidiophore by means
of a threadlike attachment.
Exserohilum rostratum
LPCB: Dark hyphae with brown
septate conidia. At both ends
of the conidia, the septa are
dark and conspicuous bands
(arrows).
Common Host
Factors
Neutropenia, solid-
organ or hematopoietic
stem-cell transplan-
tation
Diabetes mellitus,
neutropenia, solid-
organ or hematopoietic
stem-cell transplan-
tation, iron-overload
conditions
Drowning, trauma,
neutropenia, solid-
organ or hematopoietic
stem-cell trans-
plantation
Trauma, neutropenia,
solid-organ or hemato-
poietic stem-cell trans-
plantation
Neutropenia, hemato-
poietic stem-cell trans-
plantation
Immunocompetent
host, trauma
Neutropenia, solid-
organ or hematopoietic
stem-cell transplan-
tation
Immunocompetent
host, history
of injection of
methylprednisolone
Common Symptoms
and Signs
Focal deficits
Sino-orbital mucor-
mycosis; cranial-nerve
palsies, cavernous
sinus infection, focal
deficits
Focal deficits
Focal deficits
Focal deficits,
nodular cutaneous
lesions, bilateral
endophthalmitis
Focal deficits
Focal deficits
Focal deficits,
meningitis,
arachnoiditis
Diagnostic
Tests
Galactomannan
in serum,
bronchoalveolar-
lavage specimen, or
CSF; 1,3--D-
glucan in serum or
CSF; positive PCR
assay
Positive PCR
assay
1,3--D-glucan
in serum or CSF;
positive PCR assay
Positive blood
culture; 1,3--D-
glucan in serum
or CSF; positive
PCR assay
Positive blood
culture; galacto-
mannan in serum,
bronchoalveolar-
lavage specimen,
or CSF; 1,3--D-glucan
in serum; positive
PCR assay
None developed
None developed
1,3--D-glucan;
positive PCR assay
Neuroimaging
Cerebral infarcts,
parenchymal hemor-
rhage, mycotic
aneurysms, abscess
Cerebral infarcts,
parenchymal hemor-
rhage, mycotic
aneurysms, cavernous
sinus thrombosis
Cerebral infarcts
and abscesses
Cerebral infarcts
and abscesses
Cerebral infarcts,
parenchymal hemor-
rhage, mycotic
aneurysms
Solitary encapsulated
masses simulating a
brain tumor, abscess
with satellite lesions
Cerebral infarcts,
parenchymal hemor-
rhage, brain abscess
Cerebral infarcts,
mycotic aneurysm,
brain abscess,
epidural abscess,
arachnoiditis
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Mold Infections of the Central Nervous System
n engl j med 371;2 nejm.org july 10, 2014
153
early selective decompressive hemicraniectomy
and durotomy may prevent devastating secondary
brain herniation. Selective stereotactic decom-
pression of edematous intracerebral lesions may
prevent herniation while sparing functionally
critical areas. Bulk excision of either intracranial
abscesses or granulomas should be avoided, es-
pecially within critical functional regions.
Compressive and intramedullary spinal cord
syndromes caused by intradural, extradural, or
vertebral fungal infections necessitate prompt
neurosurgical decompression, drainage, and re-
section. Surgical drainage or excision, tailored
to the location and size of the lesion, is the first-
line treatment for intramedullary abscess or
granuloma formations. In contrast, localized
meningitis, arachnoiditis, radiculopathy, radiculo-
myelopathy, and anterior-spinal-artery infarction
are treated conservatively.
Management of Immunologic Impairments
Because innate host defenses play a critical role
in protection from and eradication of mold infec-
tions of the CNS, the reversal of immunosup-
pression is essential for a successful outcome.
The intrinsic immune responses within the brain,
involving microglia and the complement system,
appear to be inadequate as a host defense against
invasive Aspergillus fumigatus.
14
In transplant re-
cipients, for whom reversal of immunosuppres-
sion may not be feasible, immunosuppressive
therapy should be minimized in close coordina-
tion with the patients primary care team.
Strategies that can augment the innate host
response against mold infection of the CNS in-
clude the use of growth factors to accelerate re-
covery from neutropenia, provision of granulo-
cyte transfusions with sustained circulating
neutrophils until the patient recovers from neutro-
penia, and discontinuation or reduction in the dose
of glucocorticoids.
15,16
The correction of metabolic
acidosis and hyperglycemia is a cornerstone of
the treatment of CNS mucormycosis.
Specific Pathogens
The management of mold infections of the CNS
is individualized for each patient on the basis of
the host response, neuroanatomical involvement,
and the specific pathogen involved.
Aspergillus Species
The risk factors for CNS aspergillosis include
neutropenia, systemic glucocorticoid treatment,
mastoidectomy, spinal anesthesia, and paraspi-
nal glucocorticoid injections.
17
A. fumigatus was
isolated from the index patient in the 2012 out-
break of fungal meningitis.
18
Focal neurologic deficits and seizures caused
by stroke or mass effect are the most common
clinical manifestations of CNS aspergillosis.
19
Meningeal signs are uncommon, and their pres-
ence is indicative of a subarachnoid hemorrhage.
20
CNS aspergillosis should be high on the list of
disorders in the differential diagnosis for patients
with immunosuppression and focal brain lesions,
especially those with characteristic pulmonary
infiltrates in whom focal neurologic deficits or
focal seizures develop. Recovery of aspergillus
from pulmonary lesions with the use of bron-
choalveolar lavage or fine-needle aspiration should
be pursued when possible. An enzyme immuno-
assay for detection of galactomannan in serum or
bronchoalveolar lavage fluid should be performed
when feasible.
21
As described above, galactoman-
nan and 1,3--d-glucan may be found in the se-
rum or CSF of patients with CNS aspergillosis.
6,7
Voriconazole is the first-line treatment for
CNS aspergillosis.
12
Although there are no for-
mal guidelines regarding therapeutic drug mon-
itoring in CNS aspergillosis, we recommend
maintaining trough concentrations of 2 to 5 g
per milliliter in serum. Drug-related adverse
events may necessitate a reduction in dosage. Be-
cause voriconazole has approximately 50% pene-
tration through the bloodbrain barrier, measure-
ment of concentrations in CSF is not necessary.
For patients in whom voriconazole as primary
therapy might have unacceptable adverse effects,
liposomal amphotericin B is an alternative.
12
Monitoring of the therapeutic response of CNS
aspergillosis and other mold infections of the
CNS should include careful bedside evaluation
and serial CT or MRI scans. The frequency of
scanning should vary directly with the severity
of the infection, but a reasonable interval is a
Figure 1 (facing page). Comparative Features of Mold
Infections of the Central Nervous System.
The use of a polymerase-chain-reaction (PCR) assay of
cerebrospinal fluid (CSF) remains investigational and has
not been approved by the Food and Drug Administration.
The host factors listed here are the most common; how-
ever, other hosts may be susceptible. LPCB denotes lacto-
phenol cotton blue stain.
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The new engl and journal o f medicine
n engl j med 371;2 nejm.org july 10, 2014
154
minimum of every 1 to 2 weeks until the pa-
tients condition is stable.
Mucorales
Cerebral mucormycosis, which is perhaps the
most aggressive mold infection of the CNS, con-
stitutes a medical emergency. Early cases were
uniformly fatal. However, recent studies have
shown improved survival, possibly as the result of
earlier diagnosis and better control of under lying
diseases.
22
Diabetes mellitus and iron-overload
conditions are distinctive risk factors for the de-
velopment of mucormycosis.
23
In patients with
neutropenia or patients receiving glucocorticoid
therapy, mold infections of the CNS develop as
sino-orbital infections or through hematogenous
dissemination of pulmonary mucormycosis.
24
In
contrast, patients with diabetes mellitus usually
present with sino-orbital mucormycosis and sel-
dom present with pulmonary or disseminated
infection.
23,25
Among intravenous drug users, CNS
mucormycosis is a relatively common cause of
A B
D E
200 m
C
Figure 2. Characteristic Findings Associated with Mold Infections of the Central Nervous System.
Patient 1, a 7-year-old girl with newly diagnosed, high-risk, preB-cell acute lymphocytic leukemia, presented with
neutropenia and cough, paralysis of the left arm, and left homonymous hemianopsia. Computed tomography (CT)
of the chest (Panel A) revealed nodular densities in the lower lobe of the right lung. Magnetic resonance imaging
(MRI) of the head (Panel B) showed numerous cortical and subcortical infarcts with surrounding edema leading to
mass effects; stereotactically guided brain biopsy yielded a specimen for culture that was positive for Aspergillus fu-
migatus. Patient 2, a 24-year-old woman with acute myeloid leukemia, was admitted for fever and neutropenia fol-
lowed by rapid deterioration of mental status; CT of the chest (Panel C) showed nodular pneumonia. MRI of the
head (Panel D) revealed multiple bilateral infarcts, the largest of which shown in the left parietaloccipital region.
Examination of a brain-biopsy specimen (Panel E, Gomori methenamine silver stain) revealed numerous acutely
branching septate hyphae. No organisms were grown in culture, because the biopsy specimen was obtained while
the patient was receiving antifungal therapy. The histologically compatible organisms include aspergillus, fusarium,
scedosporium, and other hyaline molds. The use of immunohistochemical and molecular diagnostic procedures,
such as a PCR assay and in situ hybridization, may make it possible to further identify the causative organism.
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Mold Infections of the Central Nervous System
n engl j med 371;2 nejm.org july 10, 2014
155
intracerebral fungal abscesses.
25
Treatment with
the iron-chelating agent deferoxamine is a well-
recognized risk factor for disseminated mucor-
mycosis.
26
Perhaps more than any other infection, mucor-
mycosis of the ethmoid sinuses may involve all
structures along its invasive path, including the
orbit and eye, bone, and brain tissue.
25,27
Be-
cause venous drainage of the ethmoid sinuses
extends into the cavernous sinuses, ethmoidal
mucormycosis carries a high risk of cavernous
sinus thrombosis. Impairment of cranial nerves
III, IV, V
1
, V
2
, and VI may be the initial signs of
cavernous sinus thrombosis. Sinus opacifica-
tion, bony erosions, and obliteration of deep
fascia planes can be detected with the use of CT
and MRI. The organism may be identified by
swabbing, scraping, or biopsy of an involved
area to obtain samples for analysis, such as
black pus from the nasal turbinates, fluid
from a surgically drained sinus, or brain tissue.
Wet-mount preparations reveal ribbonlike,
broad, nonseptate or hyposeptate hyphae, which
are highlighted with the use of calcofluor white.
Because it can be difficult to detect hyphae in
frozen sections stained with hematoxylin and
eosin, some institutions have introduced calcoflu-
or-stained homog enates of intraoperative speci-
mens as a rapid means of determining whether
Mucorales organisms are present.
28
Successful management of rhinocerebral mu-
cormycosis depends not only on early diagnosis
but also on primary antifungal therapy with
amphotericin B, reversal of host impairments
particularly diabetes mellitus, neutropenia,
and glucocorticoid exposure and timely sur-
gical intervention, when indicated. Posacon-
azole, which has in vitro activity against some
isolates of Mucorales, particularly species of
mucor, may have a role in follow-up therapy.
29
Although iron chelation with deferasirox has been
shown to improve the outcome in a diabetic
murine model of disseminated mucormycosis, a
randomized trial of this agent did not show a
benefit.
30
Adjunctive treatments, such as hyper-
baric oxygen, granulocytemacrophage colony-
stimulating factor, and interferon-, require fur-
ther study.
31
Fusarium Species
CNS fusariosis develops predominantly in patients
with prolonged neutropenia. These organisms
are highly angioinvasive and cause hemorrhagic
infarction with strokelike events.
32
Portals of en-
try include the lungs, sinuses, vascular catheters,
and distinctively, periungual lesions (paronychia
in patients with neutropenia).
33
Fusarium species
are also most frequently associated with funge-
mia, multiple erythematous nodular cutaneous
lesions, and septic arthritis. A positive blood cul-
ture growing a hyaline (i.e., colorless or lightly
pigmented) mold in a patient with persistent neu-
tropenia is most likely to indicate the presence of
fusarium. A definitive mycologic diagnosis can be
rapidly established by biopsy and culture of these
cutaneous lesions. As compared with other mold
infections of the CNS, disseminated fusariosis is
more commonly associated with bilateral endo-
phthalmitis, which may lead to blindness. Hema-
togenously disseminated fusarium infections cause
chorioretinitis at a rate that is disproportionally
higher than that seen with other organisms causing
mold infections of the CNS.
34
Because dissemi-
nated fusariosis commonly causes fungemia and
cutaneous lesions, early diagnosis and therapy
may prevent progression to encephalitis and en-
dophthalmitis.
Fusarium species vary in their susceptibility
to antifungal agents.
35
Voriconazole is licensed for
second-line therapy; however, amphotericin B also
has been used successfully.
36
A rational approach
for treating patients with CNS fusariosis, pending
determination of susceptibility, is the adminis-
tration of voriconazole plus a lipid formulation
of amphotericin B.
Scedosporium Species
Scedosporium apiospermum is readily isolated from
soil, polluted water, and sewage. Mold infections
of the CNS caused by S. apiospermum are strongly
associated with drowning events in immuno-
competent hosts, when the organism invades
through the cribriform plate or disseminates
from pneumonic foci.
37,38
Among immunocom-
promised patients, the features of CNS scedospo-
riosis resemble those of aspergillosis, including
hematogenous dissemination from pulmonary
lesions or by extension from the sinuses. Al-
though scedosporium species form branching
septate hyphae that are similar to those of asper-
gillus, in rare cases, terminal annelloconidia are
seen in tissue. Nonetheless, culture is required for
a definitive diagnosis. Voriconazole is licensed as
second-line therapy for S. apiospermum infections
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The new engl and journal o f medicine
n engl j med 371;2 nejm.org july 10, 2014
156
T
a
b
l
e
1
.
T
h
e
r
a
p
e
u
t
i
c
O
p
t
i
o
n
s
f
o
r
M
o
l
d
I
n
f
e
c
t
i
o
n
s
o
f
t
h
e
C
e
n
t
r
a
l
N
e
r
v
o
u
s
S
y
s
t
e
m
(
C
N
S
)
.
*
M
o
l
d
F
i
r
s
t
-
L
i
n
e
T
h
e
r
a
p
y
S
e
c
o
n
d
-
L
i
n
e
T
h
e
r
a
p
y
A
d
j
u
n
c
t
i
v
e
T
h
e
r
a
p
y
a
n
d
C
o
m
m
e
n
t
s
A
d
u
l
t
s
C
h
i
l
d
r
e
n
A
d
u
l
t
s
C
h
i
l
d
r
e
n
A
s
p
e
r
g
i
l
l
u
s
s
p
e
c
i
e
s
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
C
a
s
p
o
f
u
n
g
i
n
:
l
o
a
d
i
n
g
d
o
s
e
,
7
0
m
g
/
d
a
y
I
V
;
m
a
i
n
t
e
-
n
a
n
c
e
d
o
s
e
,
5
0
m
g
/
d
a
y
I
V
P
o
s
a
c
o
n
a
z
o
l
e
:
2
0
0
m
g
4
t
i
m
e
s
a
d
a
y
i
n
i
t
i
a
l
l
y
,
t
h
e
n
4
0
0
m
g
P
O
t
w
i
c
e
a
d
a
y
I
t
r
a
c
o
n
a
z
o
l
e
:
d
o
s
a
g
e
d
e
-
p
e
n
d
s
o
n
f
o
r
m
u
l
a
t
i
o
n
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
C
a
s
p
o
f
u
n
g
i
n
:
l
o
a
d
i
n
g
d
o
s
e
,
7
0
m
g
/
m
2
/
d
a
y
I
V
;
m
a
i
n
-
t
e
n
a
n
c
e
d
o
s
e
,
5
0
m
g
/
m
2
/
d
a
y
I
V
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
a
n
d
d
i
s
c
o
n
t
i
n
u
a
-
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
C
o
m
b
i
n
a
t
i
o
n
t
h
e
r
a
p
y
w
i
t
h
v
o
r
i
-
c
o
n
a
z
o
l
e
p
l
u
s
e
c
h
i
n
o
c
a
n
d
i
n
m
a
y
b
e
m
o
r
e
e
f
f
e
c
t
i
v
e
t
h
a
n
v
o
r
i
c
o
n
a
z
o
l
e
a
l
o
n
e
i
n
p
u
l
m
o
-
n
a
r
y
a
s
p
e
r
g
i
l
l
o
s
i
s
,
b
u
t
i
t
s
e
f
-
f
e
c
t
i
v
e
n
e
s
s
h
a
s
n
o
t
b
e
e
n
d
e
t
e
r
-
m
i
n
e
d
f
o
r
C
N
S
a
s
p
e
r
g
i
l
l
o
s
i
s
M
u
c
o
r
a
l
e
s
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
d
i
s
c
o
n
t
i
n
u
a
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
,
a
n
d
c
o
n
t
r
o
l
o
f
d
i
a
b
e
t
e
s
m
e
l
l
i
t
u
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
;
u
s
e
o
f
h
y
p
e
r
b
a
r
i
c
o
x
y
g
e
n
r
e
-
m
a
i
n
s
c
o
n
t
r
o
v
e
r
s
i
a
l
C
o
m
b
i
n
a
t
i
o
n
t
h
e
r
a
p
y
w
i
t
h
l
i
p
o
s
o
-
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
a
n
d
e
c
h
i
-
n
o
c
a
n
d
i
n
m
a
y
b
e
s
y
n
e
r
g
i
s
t
i
c
,
b
u
t
i
t
s
r
o
l
e
i
n
C
N
S
d
i
s
e
a
s
e
i
s
n
o
t
w
e
l
l
d
e
f
i
n
e
d
S
c
e
d
o
s
p
o
r
i
u
m
a
p
i
o
s
p
e
r
m
u
m
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
P
o
s
a
c
o
n
a
z
o
l
e
:
2
0
0
m
g
o
r
a
l
l
y
4
t
i
m
e
s
a
d
a
y
i
n
i
t
i
a
l
l
y
,
t
h
e
n
4
0
0
m
g
o
r
a
l
l
y
t
w
i
c
e
a
d
a
y
I
t
r
a
c
o
n
a
z
o
l
e
:
d
o
s
a
g
e
d
e
-
p
e
n
d
s
o
n
f
o
r
m
u
l
a
t
i
o
n
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
a
n
d
d
i
s
c
o
n
t
i
n
u
a
-
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
S
c
e
d
o
s
p
o
r
i
u
m
p
r
o
l
i
f
i
c
a
n
s
S
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
S
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
d
i
s
c
o
n
t
i
n
u
a
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
T
h
i
s
o
r
g
a
n
i
s
m
i
s
r
e
s
i
s
t
a
n
t
t
o
a
l
l
l
i
c
e
n
s
e
d
a
n
t
i
f
u
n
g
a
l
a
g
e
n
t
s
.
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Mold Infections of the Central Nervous System
n engl j med 371;2 nejm.org july 10, 2014
157
F
u
s
a
r
i
u
m
s
p
e
c
i
e
s
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
P
o
s
a
c
o
n
a
z
o
l
e
:
2
0
0
m
g
o
r
a
l
l
y
4
t
i
m
e
s
a
d
a
y
i
n
i
t
i
a
l
l
y
,
t
h
e
n
4
0
0
m
g
o
r
a
l
l
y
t
w
i
c
e
a
d
a
y
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
a
n
d
d
i
s
c
o
n
t
i
n
u
a
-
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
D
e
m
a
t
i
a
c
e
o
u
s
m
o
l
d
s
C
l
a
d
o
p
h
i
a
l
o
p
h
o
r
a
b
a
n
t
i
a
n
a
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
3
5
m
g
/
k
g
/
d
a
y
I
V
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
3
5
m
g
/
k
g
/
d
a
y
I
V
N
o
s
i
n
g
l
e
a
n
t
i
f
u
n
g
a
l
a
g
e
n
t
o
r
c
o
m
b
i
n
a
t
i
o
n
o
f
a
g
e
n
t
s
h
a
s
p
r
o
v
e
d
t
o
b
e
e
f
f
e
c
t
i
v
e
;
s
u
r
g
i
-
c
a
l
r
e
s
e
c
t
i
o
n
i
s
c
r
i
t
i
c
a
l
f
o
r
a
s
u
c
c
e
s
s
f
u
l
o
u
t
c
o
m
e
O
c
h
r
o
c
o
n
i
s
g
a
l
l
o
p
a
v
a
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
V
o
r
i
c
o
n
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
L
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
7
.
5
m
g
/
k
g
/
d
a
y
I
V
A
m
p
h
o
t
e
r
i
c
i
n
B
l
i
p
i
d
c
o
m
-
p
l
e
x
:
5
m
g
/
k
g
/
d
a
y
I
V
R
e
v
e
r
s
a
l
o
f
n
e
u
t
r
o
p
e
n
i
a
,
s
u
r
g
i
c
a
l
r
e
s
e
c
t
i
o
n
,
a
n
d
d
i
s
c
o
n
t
i
n
u
a
-
t
i
o
n
o
f
g
l
u
c
o
c
o
r
t
i
c
o
i
d
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
I
n
t
e
r
p
r
e
t
i
v
e
b
r
e
a
k
p
o
i
n
t
s
f
o
r
i
n
v
i
t
r
o
a
n
t
i
f
u
n
g
a
l
s
u
s
c
e
p
t
i
b
i
l
i
t
y
t
e
s
t
s
h
a
v
e
n
o
t
b
e
e
n
e
s
t
a
b
-
l
i
s
h
e
d
f
o
r
t
h
i
s
o
r
g
a
n
i
s
m
E
x
s
e
r
o
h
i
l
u
m
r
o
s
t
r
a
t
u
m
I
n
i
t
i
a
l
t
h
e
r
a
p
y
v
o
r
i
c
o
n
-
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
6
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
4
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
F
o
r
s
e
v
e
r
e
o
r
r
e
f
r
a
c
t
o
r
y
i
n
-
f
e
c
t
i
o
n
,
a
d
d
l
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
m
g
/
k
g
/
d
a
y
I
V
I
n
i
t
i
a
l
t
h
e
r
a
p
y
v
o
r
i
c
o
n
-
a
z
o
l
e
:
l
o
a
d
i
n
g
d
o
s
e
,
9
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
;
m
a
i
n
t
e
n
a
n
c
e
d
o
s
e
,
8
m
g
/
k
g
I
V
e
v
e
r
y
1
2
h
r
F
o
r
s
e
v
e
r
e
o
r
r
e
f
r
a
c
t
o
r
y
i
n
-
f
e
c
t
i
o
n
,
a
d
d
l
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
:
5
m
g
/
k
g
/
d
a
y
I
V
D
e
c
o
m
p
r
e
s
s
i
o
n
o
f
s
p
i
n
a
l
e
p
i
d
u
r
a
l
a
b
s
c
e
s
s
s
h
o
u
l
d
b
e
u
s
e
d
a
s
a
d
-
j
u
n
c
t
i
v
e
t
h
e
r
a
p
y
*
T
h
e
m
o
s
t
e
f
f
e
c
t
i
v
e
d
u
r
a
t
i
o
n
o
f
t
r
e
a
t
m
e
n
t
f
o
r
m
o
l
d
i
n
f
e
c
t
i
o
n
s
o
f
t
h
e
C
N
S
i
s
u
n
k
n
o
w
n
.
H
o
w
e
v
e
r
,
a
r
e
a
s
o
n
a
b
l
e
a
p
p
r
o
a
c
h
i
s
t
o
p
r
o
v
i
d
e
t
r
e
a
t
m
e
n
t
u
n
t
i
l
a
l
l
l
e
s
i
o
n
s
h
a
v
e
r
e
s
o
l
v
e
d
o
r
s
t
a
b
i
-
l
i
z
e
d
.
I
f
i
m
m
u
n
o
s
u
p
p
r
e
s
s
i
o
n
p
e
r
s
i
s
t
s
,
a
n
t
i
f
u
n
g
a
l
t
h
e
r
a
p
y
s
h
o
u
l
d
b
e
c
o
n
t
i
n
u
e
d
t
h
r
o
u
g
h
o
u
t
t
h
e
p
e
r
i
o
d
o
f
i
m
m
u
n
o
s
u
p
p
r
e
s
s
i
o
n
.
P
r
e
m
a
t
u
r
e
d
i
s
c
o
n
t
i
n
u
a
t
i
o
n
o
f
a
n
t
i
f
u
n
g
a
l
t
h
e
r
a
p
y
m
a
y
l
e
a
d
t
o
r
e
c
r
u
d
e
s
c
e
n
t
i
n
f
e
c
t
i
o
n
.
I
V
d
e
n
o
t
e
s
i
n
t
r
a
v
e
n
o
u
s
l
y
.
T
r
e
a
t
m
e
n
t
w
i
t
h
g
r
a
n
u
l
o
c
y
t
e
c
o
l
o
n
y
-
s
t
i
m
u
l
a
t
i
n
g
f
a
c
t
o
r
,
g
r
a
n
u
l
o
c
y
t
e
m
a
c
r
o
p
h
a
g
e
c
o
l
o
n
y
-
s
t
i
m
u
l
a
t
i
n
g
f
a
c
t
o
r
,
o
r
g
r
a
n
u
l
o
c
y
t
e
t
r
a
n
s
f
u
s
i
o
n
s
c
a
n
b
e
u
s
e
d
t
o
p
r
o
m
o
t
e
r
e
c
o
v
e
r
y
f
r
o
m
n
e
u
t
r
o
p
e
n
i
a
.
B
e
c
a
u
s
e
t
r
o
u
g
h
l
e
v
e
l
s
m
a
y
v
a
r
y
,
t
h
e
r
a
p
e
u
t
i
c
d
r
u
g
l
e
v
e
l
s
s
h
o
u
l
d
b
e
m
o
n
i
t
o
r
e
d
,
w
i
t
h
d
o
s
a
g
e
a
d
j
u
s
t
m
e
n
t
a
s
w
a
r
r
a
n
t
e
d
.
T
h
e
p
e
d
i
a
t
r
i
c
d
o
s
a
g
e
o
f
p
o
s
a
c
o
n
a
z
o
l
e
h
a
s
n
o
t
b
e
e
n
w
e
l
l
d
e
f
i
n
e
d
.
T
h
e
l
i
m
i
t
e
d
e
x
p
e
r
i
e
n
c
e
w
i
t
h
p
o
s
a
c
o
n
a
z
o
l
e
f
o
r
t
h
e
t
r
e
a
t
m
e
n
t
o
f
m
o
l
d
i
n
f
e
c
t
i
o
n
s
o
f
t
h
e
C
N
S
c
o
m
e
s
f
r
o
m
t
h
e
u
s
e
o
f
t
h
e
p
o
s
a
c
o
n
a
z
o
l
e
s
u
s
p
e
n
s
i
o
n
;
t
h
e
n
e
w
e
r
f
o
r
m
u
l
a
t
i
o
n
s
o
f
p
o
s
a
c
o
n
a
z
o
l
e
(
i
n
t
r
a
v
e
n
o
u
s
a
g
e
n
t
s
a
n
d
e
x
t
e
n
d
e
d
-
r
e
l
e
a
s
e
t
a
b
l
e
t
s
)
a
p
p
e
a
r
t
o
h
a
v
e
i
m
p
r
o
v
e
d
p
h
a
r
m
a
c
o
k
i
n
e
t
i
c
p
r
o
p
e
r
t
i
e
s
,
b
u
t
t
h
e
r
e
a
r
e
n
o
d
a
t
a
a
v
a
i
l
a
b
l
e
o
n
t
h
e
i
r
u
s
e
f
o
r
t
r
e
a
t
i
n
g
t
h
e
s
e
i
n
f
e
c
t
i
o
n
s
.
T
h
e
i
n
v
i
t
r
o
a
n
t
i
f
u
n
g
a
l
s
u
s
c
e
p
t
i
b
i
l
i
t
y
o
f
v
o
r
i
c
o
n
a
z
o
l
e
v
a
r
i
e
s
o
v
e
r
a
w
i
d
e
r
a
n
g
e
f
o
r
t
h
e
s
e
o
r
g
a
n
i
s
m
s
.
1
0
,
1
1
I
n
i
t
i
a
l
t
h
e
r
a
p
y
w
i
t
h
b
o
t
h
v
o
r
i
c
o
n
a
z
o
l
e
a
n
d
l
i
p
o
s
o
m
a
l
a
m
p
h
o
t
e
r
i
c
i
n
B
,
p
e
n
d
i
n
g
t
h
e
a
v
a
i
l
a
b
i
l
i
t
y
o
f
d
a
t
a
o
n
m
i
n
i
m
u
m
i
n
h
i
b
i
t
o
r
y
c
o
n
c
e
n
t
r
a
t
i
o
n
s
,
m
a
y
b
e
w
a
r
r
a
n
t
e
d
.
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The new engl and journal o f medicine
n engl j med 371;2 nejm.org july 10, 2014
158
and, in the absence of alternatives, is used as
initial therapy, until the in vitro susceptibility
profile is available.
39
In contrast, S. prolificans is resistant experi-
mentally and clinically to the three major classes
of antifungal agents. S. prolificans infects the CNS
through hematogenous dissemination in immu-
nocompromised patients and through traumatic
inoculation in immunocompetent hosts.
37
Unlike
S. apiospermum, S. prolificans may be recovered from
blood cultures. Therapy consists of surgical re-
section and reversal of immunosuppression.
Dematiaceous Molds
Dematiaceous fungi are a group of molds charac-
terized by the presence of melanin-like pigment
within the cell wall that is pale brown to black.
40
These organisms can be pathogens to plants or
livestock and may cause chromoblastomycosis
and black-grain mycetoma. Dematiaceous molds
may also cause deeply invasive infections (phaeo-
hyphomycosis), including infections of the CNS.
Most of the agents causing phaeohypho mycosis
grow very slowly, so classic mycologic identifi-
cation can take 3 weeks or longer. In comparison
with aspergillus, Mucorales, and fusarium, dema-
tiaceous molds commonly cause infections of the
CNS in immunocompetent hosts. Some dematia-
ceous molds within a narrow geographic range
cause cerebral phaeohyphomycosis.
41
Until October 2012, most known cases of CNS
phaeohyphomycosis were caused by Cladophialo-
phora bantiana (also called Xylohypha bantiana), Rhino-
cladiella mackenziei, and Ochroconis gallopava (also
called Dactylaria gallopava).
40
E. rostratum has since
emerged as a cause of meningitis in a nationwide
outbreak associated with tainted epidural glucocor-
ticoid injections.
42,43
Prolonged receipt of antifun-
gal chemotherapy, surgical resection of abscesses,
and reversal of immunosuppression are mainstays
of the treatment of CNS phaeohyphomycosis. Per-
sistence or recurrence of disease is common.
Mold infections of the CNS caused by C. bantiana
are manifested as a slowly expanding, space-
occupying lesion causing headache, seizure, and
localizing neurologic signs that simulate a brain
tumor.
40
Among immunocompetent patients, CNS
infection may occur in the absence of pulmonary
lesions. Patients who have survived had easily
resectable, encapsulated masses on CT or MRI
Table 2. Criteria for Neurosurgical or Neuroradiologic Intervention.
Indication Intervention Comments
CNS space-occupying lesion with
mass effects
Surgical decompression with
debulking of lesion or stereotactic
drainage
Choice of approach depends on lesion
size, location, and severity; large
masses with evidence of brain or
spinal cord compression or
herniation syndromes (with or
without increases in intracranial
pressure) should immediately be
decompressed, especially in
patients with a rapid onset of
clinical deterioration
Hydrocephalus Insertion of extraventricular drainage
catheter
Clinical deterioration with rostrocaudal
brain herniation can occur rapidly
as a result of unrecognized hydro-
cephalus; an external ventricular
drain allows monitoring of intracra-
nial pressure and collection of CSF
samples
Lesion thought to be fungal in origin
but not responding to antifungal
therapy
Surgical open biopsy or stereotactic
biopsy
Choice of approach depends on lesion
location and size
Acute hemispheric stroke with mass
effects (ischemic or hemor-
rhagic)
Hemicraniectomy for large middle-
cerebral-artery stroke; hematoma
aspiration
Skull bone removal (craniectomy)
reduces intracranial pressure and
brain herniation
Mycotic aneurysm with subarachnoid
hemorrhage
Coiling or surgical aneurysm, parent-
artery occlusion, or both
Severe subarachnoid hemorrhage
induced arterial vasospasm may
require catheter angioplasty
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Mold Infections of the Central Nervous System
n engl j med 371;2 nejm.org july 10, 2014
159
scans, whereas those who have died had a soli-
tary lesion that was not entirely resected, poorly
demarcated abscess borders, or multiple satellite
lesions.
44
There is no clearly effective antifungal
therapy.
45
Surgical resection remains the most
definitive treatment.
O. gallopava is a neurotropic dematiaceous mold
that causes pulmonary and CNS infection in
domestic poultry and in immunocompromised
humans.
46
Exposure to infested aerosolized warm
water may be a risk factor. In one study involving
transplant recipients, the CNS was involved in
50% of patients (6 of 12) with O. gallopava infec-
tion and a poor outcome.
47
The most effective
antifungal regimen for treatment of this infec-
tion is not known. Interpretive breakpoints for
in vitro antifungal susceptibility tests have not
been established for this organism. Combina-
tion antifungal therapy with voriconazole and a
lipid formulation of amphotericin B, pending
the availability of in vitro susceptibility data, is
recommended in conjunction with surgery and
reversal of immunosuppression.
E. rostratum is an opportunistic mold that un-
til recently was an uncommon cause of disease
in immunocompromised and immunocompetent
human hosts.
48
On September 18, 2012, health
officials began to react to a large, multistate out-
break of fungal meningitis traceable to three lots
of preservative-free methylprednisolone from one
compounding pharmacy in Massachusetts. This
outbreak resulted in 751 cases of CNS infection
and 64 deaths across the United States. Three
molecular assays and assays for 1,3--d-glucan
in serum and CSF have been developed and may
serve as adjunctive diagnostic tools.
49-52
Most of
the infected patients in the outbreak presented
with signs and symptoms that were consistent
with fungal meningitis; however, cases of spinal
osteomyelitis or epidural abscess and septic ar-
thritis or osteomyelitis were also reported.
1
In vitro
susceptibility data indicate that voriconazole and
amphotericin B have activity against E. rostratum;
this has led to recommendations that voriconazole,
liposomal amphotericin B, or both be used for
initial management in conjunction with neurosur-
gical consultation, when appropriate.
42,43
A more
detailed review of the management of E. rostratum
meningitis is reported elsewhere.
42,53
A compari-
son of the clinical features of less common mold
infections of the CNS is provided in Table S1 of
the Supplementary Appendix, available with the
full text of this article at NEJM.org.
Dr. Kontoyiannis reports receiving fees for serving on an advi-
sory board from Merck, personal fees from Gilead, and grant
support from Merck, Pfizer, and Astellas. Dr. Walsh reports receiv-
ing fees for serving on advisory boards from Astellas, ContraFect,
Pfizer, and iCo, consulting fees from Astellas, ContraFect, Pfizer,
iCo, Methylgene, and grant support from Astellas, Novartis,
ContraFect, Merck, and Cubist; he also reports serving as an
uncompensated consultant for Drais, SigmaTau, and Trius,
and receiving a study drug for laboratory investigation from
Pfizer. No other potential conf lict of interest relevant to this
article was reported.
Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
References
1. Smith RM, Schaefer MK, Kainer MA,
et al. Fungal infections associated with
contaminated methylprednisolone injec-
tions. N Engl J Med 2013;369:1598-609.
2. Segal BH. Aspergillosis. N Engl J Med
2009;360:1870-84.
3. Perfect JR. Iatrogenic fungal menin-
gitis: tragedy repeated. Ann Intern Med
2012;157:825-6.
4. Walsh TJ, Hier DB, Caplan LR. Fungal
infections of the central nervous system:
comparative analysis of risk factors and
clinical signs in 57 patients. Neurology
1985;35:1654-7.
5. Li DM, de Hoog GS. Cerebral phaeo-
hyphomycosis a cure at what lengths?
Lancet Infect Dis 2009;9:376-83.
6. Soeffker G, Wichmann D, Loder-
staedt U, Sobottka I, Deuse T, Kluge S.
Aspergillus galactomannan antigen for
diagnosis and treatment monitoring in
cerebral aspergillosis. Prog Transplant
2013;23:71-4.
7. Mikulska M, Furfaro E, Del Bono V, et
al. (1-3)--D-glucan in cerebrospinal fluid
is useful for the diagnosis of central ner-
vous system fungal infections. Clin Infect
Dis 2013;56:1511-12.
8. Tortorano AM, Esposto MC, Prigitano
A, et al. Cross-reactivity of Fusarium spp.
in the Aspergillus galactomannan enzyme-
linked immunosorbent assay. J Clin Micro-
biol 2012;50:1051-3.
9. Reinwald M, Buchheidt D, Hummel
M, et al. Diagnostic performance of an
Aspergillus-specific nested PCR assay in
cerebrospinal fluid samples of immuno-
compromised patients for detection of
central nervous system aspergillosis. PLoS
One 2013;8(2):e56706.
10. Johnson EM, Szekely A, Warnock DW.
In-vitro activity of voriconazole, itracon-
azole and amphotericin B against fila-
mentous fungi. J Antimicrob Chemother
1998;42:741-5.
11. Pfaller MA, Espinel-Ingroff A, Canton
E, et al. Wild-type MIC distributions and
epidemiological cutoff values for ampho-
tericin B, flucytosine, and itraconazole
and Candida spp. as determined by CLSI
broth microdilution. J Clin Microbiol
2012;50:2040-6.
12. Walsh TJ, Anaissie EJ, Denning DW, et
al. Treatment of aspergillosis: clinical
practice guidelines of the Infectious Dis-
eases Society of America. Clin Infect Dis
2008;46:327-60.
13. Schwartz S, Thiel E. Cerebral asper-
gillosis: tissue penetration is the key. Med
Mycol 2009;47:Suppl 1:S387-S393.
14. Rambach G, Hagleitner M, Mohseni-
pour I, et al. Antifungal activity of the lo-
cal complement system in cerebral asper-
gillosis. Microbes Infect 2005;7:1285-95.
15. Ben-Ami R, Lewis RE, Raad II, Kon-
toyiannis DP. Phaeohyphomycosis in a
tertiary care cancer center. Clin Infect Dis
2009;48:1033-41.
16. Katragkou A, Roilides E. Immuno-
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
n engl j med 371;2 nejm.org july 10, 2014
160
Mold Infections of the Central Nervous System
therapy of infections caused by rare fila-
mentous fungi. Clin Microbiol Infect 2012;
18:134-9.
17. Antinori S, Corbellino M, Meroni L, et
al. Aspergillus meningitis: a rare clinical
manifestation of central nervous system
aspergillosis: case report and review of
92 cases. J Infect 2013;66:218-38.
18. Pettit AC, Kropski JA, Castilho JL, et
al. The index case for the fungal meningi-
tis outbreak in the United States. N Engl
J Med 2012;367:2119-25.
19. Kourkoumpetis TK, Desalermos A,
Mu hammed M, Mylonakis E. Central
nervous system aspergillosis: a series of
14 cases from a general hospital and re-
view of 123 cases from the literature.
Medicine (Baltimore) 2012;91:328-36.
20. Iihara K, Makita Y, Nabeshima S, Tei
T, Keyaki A, Nioka H. Aspergillosis of the
central nervous system causing subarach-
noid hemorrhage from mycotic aneurysm
of the basilar artery case report. Neu-
rol Med Chir (Tokyo) 1990;30:618-23.
21. Herbrecht R, Letscher-Bru V, Oprea C,
et al. Aspergillus galactomannan detec-
tion in the diagnosis of invasive aspergil-
losis in cancer patients. J Clin Oncol
2002;20:1898-906.
22. Hammond SP, Baden LR, Marty FM.
Mortality in hematologic malignancy and
hematopoietic stem cell transplant pa-
tients with mucormycosis, 2001 to 2009.
Antimicrob Agents Chemother 2011;55:
5018-21.
23. Mantadakis E, Samonis G. Clinical
presentation of zygomycosis. Clin Micro-
biol Infect 2009;15:Suppl 5:15-20.
24. McNulty JS. Rhinocerebral mucor-
mycosis: predisposing factors. Laryngo-
scope 1982;92:1140-3.
25. Hopkins RJ, Rothman M, Fiore A,
Goldblum SE. Cerebral mucormycosis as-
sociated with intravenous drug use: three
case reports and review. Clin Infect Dis
1994;19:1133-7.
26. Ibrahim AS, Spellberg B, Walsh TJ,
Kontoyiannis DP. Pathogenesis of mucor-
mycosis. Clin Infect Dis 2012;54:Suppl
1:S16-S22.
27. Petrikkos G, Skiada A, Lortholary O,
Roilides E, Walsh TJ, Kontoyiannis DP.
Epidemiology and clinical manifestations
of mucormycosis. Clin Infect Dis 2012;54:
Suppl 1:S23-S34.
28. McDermott NE, Barrett J, Hipp J, et al.
Successful treatment of periodontal mu-
cormycosis: report of a case and literature
review. Oral Surg Oral Med Oral Pathol
Oral Radiol Endod 2010;109(3):e64-e69.
29. Greenberg RN, Mullane K, van Burik
JA, et al. Posaconazole as salvage therapy for
zygomycosis. Antimicrob Agents Chemo-
ther 2006;50:126-33.
30. Spellberg B, Ibrahim AS, Chin-Hong
PV, et al. The Deferasirox-AmBisome
Therapy for Mucormycosis (DEFEAT Mu-
cor) study: a randomized, double-blinded,
placebo-controlled trial. J Antimicrob
Chemother 2012;67:715-22.
31. Spellberg B, Ibrahim A, Roilides E, et
al. Combination therapy for mucormyco-
sis: why, what, and how? Clin Infect Dis
2012;54:Suppl 1:S73-S78.
32. Martino P, Gastaldi R, Raccah R, Gir-
menia C. Clinical patterns of Fusarium in-
fections in immunocompromised patients.
J Infect 1994;28:Suppl 1:7-15.
33. Steinberg GK, Britt RH, Enzmann DR,
Finlay JL, Arvin AM. Fusarium brain ab-
scess: case report. J Neurosurg 1983;58:
598-601.
34. Lamaris GA, Esmaeli B, Chamilos G,
et al. Fungal endophthalmitis in a tertiary
care cancer center: a review of 23 cases.
Eur J Clin Microbiol Infect Dis 2008;27:
343-7.
35. Anaissie E, Paetznick V, Proffitt R,
Adler-Moore J, Bodey GP. Comparison of
the in vitro antifungal activity of free and
liposome-encapsulated amphotericin B. Eur
J Clin Microbiol Infect Dis 1991;10:665-8.
36. Dignani MC, Anaissie E. Human fu-
sariosis. Clin Microbiol Infect 2004;10:
Suppl 1:67-75.
37. Cortez KJ, Roilides E, Quiroz-Telles F,
et al. Infections caused by Scedosporium
spp. Clin Microbiol Rev 2008;21:157-97.
38. Montejo M, Muiz ML, Zrraga S, et
al. Case reports: infection due to Scedo-
sporium apiospermum in renal transplant
recipients: a report of two cases and litera-
ture review of central nervous system and
cutaneous infections by Pseudallescheria
boydii/Sc. apiospermum. Mycoses 2002;
45:418-27.
39. Troke P, Aguirrebengoa K, Arteaga C,
et al. Treatment of scedosporiosis with vori-
conazole: clinical experience with 107 pa-
tients. Antimicrob Agents Chemother 2008;
52:1743-50.
40. Revankar SG, Sutton DA, Rinaldi MG.
Primary central nervous system phaeo-
hyphomycosis: a review of 101 cases. Clin
Infect Dis 2004;38:206-16.
41. Al-Tawfiq JA, Boukhamseen A. Cerebral
phaeohyphomycosis due to Rhinocladiella
mackenziei (formerly Ramichloridium mac-
kenziei): case presentation and literature
review. J Infect Public Health 2011;4:96-102.
42. Kauffman CA, Pappas PG, Patterson
TF. Fungal infections associated with
contaminated methylprednisolone injec-
tions. N Engl J Med 2013;368:2495-500.
43. Kainer MA, Reagan DR, Nguyen DB,
et al. Fungal infections associated with
contaminated methylprednisolone in Ten-
nessee. N Engl J Med 2012;367:2194-203.
44. Dixon DM, Walsh TJ, Merz WG, Mc-
Ginnis MR. Infections due to Xylohypha
bantiana (Cladosporium trichoides). Rev
Infect Dis 1989;11:515-25.
45. Lyons MK, Blair JE, Leslie KO. Suc-
cessful treatment with voriconazole of
fungal cerebral abscess due to Cladophia-
lophora bantiana. Clin Neurol Neurosurg
2005;107:532-4.
46. Qureshi ZA, Kwak EJ, Nguyen MH,
Silveira FP. Ochroconis gallopava: a demati-
aceous mold causing infections in trans-
plant recipients. Clin Transplant 2012;26:
E17-E23.
47. Shoham S, Pic-Aluas L, Taylor J, Cor-
tez K, et al. Transplant-associated Ochro-
conis gallopava infections. Transpl Infect
Dis 2008;10:442-8.
48. Stevens DA. Reflections on the ap-
proach to treatment of a mycologic disas-
ter. Antimicrob Agents Chemother 2013;
57:1567-72.
49. Gade L, Scheel CM, Pham CD, et al.
Detection of fungal DNA in human body
fluids and tissues during a multistate out-
break of fungal meningitis and other in-
fections. Eukaryot Cell 2013;12:677-83.
50. Zhao Y, Petraitiene R, Walsh TJ, Perlin
DS. A real-time PCR assay for rapid detec-
tion and quantification of Exserohilum
rostratum, a causative pathogen of fungal
meningitis associated with injection of
contaminated methylprednisolone. J Clin
Microbiol 2013;51:1034-6.
51. Lyons JL, Roos KL, Marr KA, et al. Ce-
rebrospinal fluid (1,3)--D-glucan detec-
tion as an aid for diagnosis of iatrogenic
fungal meningitis. J Clin Microbiol 2013;
51:1285-7.
52. Litvintseva AP, Lindsley MD, Gade L,
et al. Utility of (1-3)--D-glucan testing
for diagnostics and monitoring response
to treatment during the multistate out-
break of fungal meningitis and other
infections. Clin Infect Dis 2014;58:622-
30.
53. Kontoyiannis DP, Perlin DS, Roilides
E, Walsh TJ. What can we learn and what
do we need to know amidst the iatrogenic
outbreak of Exserohilum rostratum men-
ingitis? Clin Infect Dis 2013;57:853-9.
Copyright 2014 Massachusetts Medical Society.
IMAGES IN CLINICAL MEDICINE
The Journal welcomes consideration of new submissions for Images in Clinical
Medicine. Instructions for authors and procedures for submissions can be found
on the Journals website at NEJM.org. At the discretion of the editor, images that
are accepted for publication may appear in the print version of the Journal,
the electronic version, or both.
The New England Journal of Medicine
Downloaded from nejm.org on July 10, 2014. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
You might also like
- Microbiology PDFDocument237 pagesMicrobiology PDFchioNo ratings yet
- Remedies For Health Problems of The Organic Laying FlockDocument60 pagesRemedies For Health Problems of The Organic Laying Flockqfarms100% (1)
- Opportunistic Fungal InfectionsDocument81 pagesOpportunistic Fungal Infectionstummalapalli venkateswara raoNo ratings yet
- 100 BCQ MRCP QuestionsDocument31 pages100 BCQ MRCP QuestionsMatin Ahmad Khan100% (1)
- Allergic Fungal Sinusitis PresentationDocument50 pagesAllergic Fungal Sinusitis PresentationdrdrsuryaprakashNo ratings yet
- Viral Encephalitis PDFDocument7 pagesViral Encephalitis PDFDeborah Bravian TairasNo ratings yet
- Respiratory Passmedicin 2022Document1,020 pagesRespiratory Passmedicin 2022Faris Firas100% (1)
- Medical Mycology: Fungal Diseases and Cutaneous MycosesDocument54 pagesMedical Mycology: Fungal Diseases and Cutaneous MycosessuwarnyNo ratings yet
- PARANEOPLASTICDocument8 pagesPARANEOPLASTICMuhammad Imran MirzaNo ratings yet
- Respiratory Medicine 151 200Document31 pagesRespiratory Medicine 151 200Ahmed Kh. Abu Warda100% (2)
- Therapeutic Guidelines in Systemic Fungal Infection. 3rd Ed.Document127 pagesTherapeutic Guidelines in Systemic Fungal Infection. 3rd Ed.PrisNo ratings yet
- Manual de Aquaponia FaoDocument288 pagesManual de Aquaponia FaoYves Moreira100% (3)
- Manual de Aquaponia FaoDocument288 pagesManual de Aquaponia FaoYves Moreira100% (3)
- Meningitis: Review ArticleDocument19 pagesMeningitis: Review ArticleYo Me100% (1)
- Pulmo Viewboxes BLOCK 8Document251 pagesPulmo Viewboxes BLOCK 8U.P. College of Medicine Class 2014100% (2)
- Mecanica de Suelos - Juarez BadilloDocument629 pagesMecanica de Suelos - Juarez BadilloJesús Daza Osorio84% (58)
- Mold Infections of the Central Nervous SystemDocument15 pagesMold Infections of the Central Nervous SystemJohn TusselNo ratings yet
- Rar Vol11 Nro3Document21 pagesRar Vol11 Nro3Valentine WijayaNo ratings yet
- CNS InfectionDocument6 pagesCNS InfectionAnonymous nruHyuwtJNo ratings yet
- Central Nervous System InfectionDocument12 pagesCentral Nervous System InfectionJoseph DuffyNo ratings yet
- CNS Toxoplasmosis in HIV - Overview, Pathophysiology, EpidemiologyDocument10 pagesCNS Toxoplasmosis in HIV - Overview, Pathophysiology, EpidemiologyDauris garcia diazNo ratings yet
- Brain AbcesDocument6 pagesBrain AbcesGintar Isnu WardoyoNo ratings yet
- Bacterial Brain Abscess: Journal ReadingDocument22 pagesBacterial Brain Abscess: Journal ReadingdinarNo ratings yet
- IDSA Guidelines for Diagnosis and Treatment of EncephalitisDocument25 pagesIDSA Guidelines for Diagnosis and Treatment of EncephalitisJizus GonzalezNo ratings yet
- Research Paper Bacterial MeningitisDocument4 pagesResearch Paper Bacterial Meningitisafeebovus100% (1)
- Brain Abcess Journal 2Document4 pagesBrain Abcess Journal 2ansyemomoleNo ratings yet
- Neuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesFrom EverandNeuroimmunology: Multiple Sclerosis, Autoimmune Neurology and Related DiseasesAmanda L. PiquetNo ratings yet
- The Management of Encephalitis Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis Clinical Practice Guidelines by The Infectious Diseases Society of AmericaNana ShkodinaNo ratings yet
- WLek 202002114Document4 pagesWLek 202002114onaNo ratings yet
- Bacterial Infections of the Nervous SystemDocument2 pagesBacterial Infections of the Nervous SystemRocio LedesmaNo ratings yet
- Herpes Simplex: Encephalitis Children and Adolescents: Richard J. Whitley, MD, and David W. Kimberlin, MDDocument7 pagesHerpes Simplex: Encephalitis Children and Adolescents: Richard J. Whitley, MD, and David W. Kimberlin, MDFirah Triple'sNo ratings yet
- Paraneoplastic Syndromes in Small Cell Lung CancerDocument11 pagesParaneoplastic Syndromes in Small Cell Lung CancerFebri Dwi HaryonoNo ratings yet
- Toxoplasma gondii: An Obligate Intracellular ProtozoanDocument47 pagesToxoplasma gondii: An Obligate Intracellular ProtozoanArun KumarNo ratings yet
- J Neurol Neurosurg Psychiatry 2004 Bennetto I22 8Document8 pagesJ Neurol Neurosurg Psychiatry 2004 Bennetto I22 8Frank CavasNo ratings yet
- Neuromyelitisoptica: Sarah L. Patterson,, Sarah E. GoglinDocument13 pagesNeuromyelitisoptica: Sarah L. Patterson,, Sarah E. GoglinErji K.No ratings yet
- LiquorDocument8 pagesLiquorFanel PutraNo ratings yet
- Whitley 2005Document7 pagesWhitley 2005Firah Triple'sNo ratings yet
- Infectious MyelopathiesDocument23 pagesInfectious MyelopathiesAnonymous 7jKR9XbNo ratings yet
- Cerebral Toxoplasmosis: ClinicalpictureDocument2 pagesCerebral Toxoplasmosis: ClinicalpictureRahul RaiNo ratings yet
- 2009 Romanian Study Ms Is LymeDocument6 pages2009 Romanian Study Ms Is LymeTegorion WhiteNo ratings yet
- New 1Document12 pagesNew 1Muhammad SyaifullahNo ratings yet
- Lee 2007Document6 pagesLee 2007Luis PerezNo ratings yet
- Malignant Otitis Externa: An Emerging Complication: Original ArticleDocument3 pagesMalignant Otitis Externa: An Emerging Complication: Original ArticleWa Ode Meutya ZawawiNo ratings yet
- Asymptomatic Mycoplasma Infection Causing Acute Demyelinating Encephalomyelitis: Case Report and Review of LiteratureDocument4 pagesAsymptomatic Mycoplasma Infection Causing Acute Demyelinating Encephalomyelitis: Case Report and Review of Literatureluisalfredo_montesNo ratings yet
- 72_Progressive multifocal leukoencephalopathy in an immunocompetent patientDocument7 pages72_Progressive multifocal leukoencephalopathy in an immunocompetent patientFaras ArinalNo ratings yet
- Selulitis PDFDocument5 pagesSelulitis PDFDhisa Zainita HabsariNo ratings yet
- Pyogenic Brain Abscess A 15 Year SurveryDocument10 pagesPyogenic Brain Abscess A 15 Year SurverySilvia RoseNo ratings yet
- Encefalitis Aguda en InmunocompetentesDocument15 pagesEncefalitis Aguda en InmunocompetentesNicolas de la cruz floresNo ratings yet
- Cerebral Toxoplasmosis - 1Document2 pagesCerebral Toxoplasmosis - 1hasbi.alginaaNo ratings yet
- Meningitis Vs Ensefalitis MeganDocument10 pagesMeningitis Vs Ensefalitis MeganFandi ArgiansyaNo ratings yet
- Absceso CerebralDocument8 pagesAbsceso Cerebralgiseladelarosa2006No ratings yet
- Brain Abscess in ChildrenDocument5 pagesBrain Abscess in Childrencamelia musaadNo ratings yet
- Approach To The Patient With Suspected Infection of SNCDocument12 pagesApproach To The Patient With Suspected Infection of SNCJosé Miguel FerreiraNo ratings yet
- Viral Encephalitis: A Clinician's Guide: Practical NeurologyDocument19 pagesViral Encephalitis: A Clinician's Guide: Practical NeurologyCésar Vásquez Aguilar100% (1)
- Bacterial Meningitis in ChildrenDocument10 pagesBacterial Meningitis in ChildrenAnny AryanyNo ratings yet
- The Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaDocument25 pagesThe Management of Encephalitis: Clinical Practice Guidelines by The Infectious Diseases Society of AmericaVictor Euclides Briones MoralesNo ratings yet
- Therapy LeukemiaDocument11 pagesTherapy LeukemiaGita RahmatikaNo ratings yet
- Clinical Features, Etiologies, and Outcomes in Adult Patients WithDocument13 pagesClinical Features, Etiologies, and Outcomes in Adult Patients Withagarrido2No ratings yet
- Neurotoxoplasmosis and neurocysticercosis in AIDS patientDocument8 pagesNeurotoxoplasmosis and neurocysticercosis in AIDS patientMarcinha BauerNo ratings yet
- CNS InfectionDocument17 pagesCNS InfectionEdward PuteraNo ratings yet
- Tuberculomas of The Brain With and Without Associated Meningitis: A Cohort of 28 Cases Treated With Anti-Tuberculosis Drugs at A Tertiary Care CentreDocument4 pagesTuberculomas of The Brain With and Without Associated Meningitis: A Cohort of 28 Cases Treated With Anti-Tuberculosis Drugs at A Tertiary Care CentreDestyNo ratings yet
- Aseptic Meningitis in Adults - UpToDateDocument16 pagesAseptic Meningitis in Adults - UpToDateKondász Antal Gábor MedNo ratings yet
- Current Epidemiological Trends of Brain Abscess: A Clinicopathological StudyDocument9 pagesCurrent Epidemiological Trends of Brain Abscess: A Clinicopathological StudyNur Fadhilah KusnadiNo ratings yet
- Retrospective Analysis of 49 Cases of Brain Abscess and Review of The LiteratureDocument11 pagesRetrospective Analysis of 49 Cases of Brain Abscess and Review of The LiteraturenisaNo ratings yet
- Importancia de Las Imágenes y El Diagnóstico Etiológico en El Paciente Inmunocomprometido Con Afección Del SNCDocument9 pagesImportancia de Las Imágenes y El Diagnóstico Etiológico en El Paciente Inmunocomprometido Con Afección Del SNCFranciely GarridoNo ratings yet
- Management of EncephalitisDocument25 pagesManagement of EncephalitisOWintero OWarmoNo ratings yet
- Brucellosis DCDocument6 pagesBrucellosis DCbrahim brahimNo ratings yet
- Smith 2008Document27 pagesSmith 2008Lindia PrabhaswariNo ratings yet
- Brain AbscessDocument17 pagesBrain AbscessLaura Fernanda Soto BNo ratings yet
- Cns InfectionsDocument56 pagesCns InfectionsDinaNo ratings yet
- Intracranial Infections Clinical and Imaging CharacteristicsDocument20 pagesIntracranial Infections Clinical and Imaging CharacteristicsRiyan NuelNo ratings yet
- Preprints202309 0487 v1Document23 pagesPreprints202309 0487 v1Saul EstrellaNo ratings yet
- Bacterial Meningitis ThesisDocument8 pagesBacterial Meningitis ThesisRick Vogel100% (2)
- Hipertensión en El Embarazo ACOG2013Document10 pagesHipertensión en El Embarazo ACOG2013Ramiro Castro ApoloNo ratings yet
- Guidelines For The Management of DF and DHF in AdultsDocument46 pagesGuidelines For The Management of DF and DHF in AdultsNanda SulistyaningrumNo ratings yet
- Management of Febrile NeutropeniaDocument5 pagesManagement of Febrile NeutropeniaphoechoexNo ratings yet
- Outlook For A Dengue Vaccine: ReviewDocument3 pagesOutlook For A Dengue Vaccine: ReviewguillosarahNo ratings yet
- Optimal Strategy For The Firts Episode of Primary Spontaneous PneumothoraxDocument10 pagesOptimal Strategy For The Firts Episode of Primary Spontaneous PneumothoraxguillosarahNo ratings yet
- Thorax 2010 MacDuff Ii18 31Document15 pagesThorax 2010 MacDuff Ii18 31guillosarahNo ratings yet
- Emergency Trauma Score Still Not Quite Ready For Prime Time?Document2 pagesEmergency Trauma Score Still Not Quite Ready For Prime Time?guillosarahNo ratings yet
- Trauma Scoring Systems: ReviewDocument4 pagesTrauma Scoring Systems: ReviewguillosarahNo ratings yet
- Spontan PneumothoraxDocument3 pagesSpontan PneumothoraxSuriyani SofianNo ratings yet
- Thorax 2010 MacDuff Ii18 31Document15 pagesThorax 2010 MacDuff Ii18 31guillosarahNo ratings yet
- Bris JR Hematol 2020Document18 pagesBris JR Hematol 2020cdsaludNo ratings yet
- C 21 DDocument9 pagesC 21 Darvind769No ratings yet
- Practice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaDocument60 pagesPractice Guidelines For The Diagnosis and Management of Aspergilosis 2016 Update by AmericaNur Prasetyo Nugroho100% (1)
- Cavitary Lung Diseases: A Clinical-Radiologic Algorithmic ApproachDocument23 pagesCavitary Lung Diseases: A Clinical-Radiologic Algorithmic ApproachjhordyafsNo ratings yet
- Systemic Fungal Infections GuideDocument107 pagesSystemic Fungal Infections GuidePrincewill SeiyefaNo ratings yet
- PREP ICU 2013 Answers and Critiques - 3 - May & JuneDocument41 pagesPREP ICU 2013 Answers and Critiques - 3 - May & JuneNicholasHuffNo ratings yet
- IUMS2014, ProceedingDocument1,487 pagesIUMS2014, Proceedingamir-scribdNo ratings yet
- Tmp424e TMPDocument72 pagesTmp424e TMPFrontiersNo ratings yet
- Aspergillus Infection Nejm 2021Document14 pagesAspergillus Infection Nejm 2021El TrémoloNo ratings yet
- Aspergillosis: Aspergillus Spores Every Day Without Getting Sick. However, People WithDocument8 pagesAspergillosis: Aspergillus Spores Every Day Without Getting Sick. However, People Withvic ayoNo ratings yet
- Mikosis ParuDocument33 pagesMikosis ParuselviaNo ratings yet
- Topnotch Microbiology Supertable - KindnesstoallDocument252 pagesTopnotch Microbiology Supertable - KindnesstoallRJLeddaNo ratings yet
- DIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)Document31 pagesDIPIRO 9th PHARMACOTHERAPY-PATOPHISIOLOGY APPROACH EDISI 9 (PDF - Io)NingrumSindayaniNo ratings yet
- Aspergillus and Vaginal Colonization-2329-8731.1000e115Document2 pagesAspergillus and Vaginal Colonization-2329-8731.1000e115Hervis Francisco FantiniNo ratings yet
- Chronic Airspace DiseasesDocument31 pagesChronic Airspace DiseasesAnkita ShahNo ratings yet
- Genomics of Plants and Fungi - Prade and BohnertDocument395 pagesGenomics of Plants and Fungi - Prade and BohnertFernanda CastroNo ratings yet
- OT Air SamplingDocument41 pagesOT Air SamplingIzz JerghaNo ratings yet
- Isavuconazol & Mucor & AspergillusDocument11 pagesIsavuconazol & Mucor & AspergillusAlejandra OrtizNo ratings yet
- Opportunistic MycosisDocument59 pagesOpportunistic MycosisSisay Fesseha AmbayeNo ratings yet
- Larone S Medically Important Fungi - 2018 - Walsh - BibliographyDocument26 pagesLarone S Medically Important Fungi - 2018 - Walsh - BibliographyYenia Micol MatwiejukNo ratings yet