Professional Documents
Culture Documents
Jurnal The Role of Imaging Methods in Identifying The Causes of Extrahepatic Cholestasis
Uploaded by
wizardebm0 ratings0% found this document useful (0 votes)
28 views7 pagescccfvbvbvcbvbvb
Original Title
Jurnal the Role of Imaging Methods in Identifying the Causes of Extrahepatic Cholestasis
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentcccfvbvbvcbvbvb
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
28 views7 pagesJurnal The Role of Imaging Methods in Identifying The Causes of Extrahepatic Cholestasis
Uploaded by
wizardebmcccfvbvbvcbvbvb
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 7
Imaging of extrahepatic cholestasis
J Gastrointestin Liver Dis
September 2006 Vol.15 No.3, 265-271
Address for correspondence: Professor Ion Rogoveanu, MD,PhD
1
st
Medical Clinic-Gastroenterology
Tabaci Str.1
200642, Craiova, Romania
E-mail: digheonea@rdslink.ro
CLINICAL IMAGING
The Role of Imaging Methods in Identifying the Causes
of Extrahepatic Cholestasis*
Ion Rogoveanu, Dan Ionu Gheonea, Adrian Sftoiu, Tudorel Ciurea
1
st
Medical Clinic Gastroenterology Department, University of Medicine and Pharmacy Craiova*
* All illustrations belong to the collection of the Medical I Clinic
Gastroenterology Department, University of Medicine and
Pharmacy Craiova, Romania
Abstract
Transabdominal ultrasonography is the first choice
examination used for the etiological diagnosis of
extrahepatic cholestasis because it is a noninvasive, rapid
method and presently widely accessible. In this article we
discuss the accuracy of transabdominal ultrasonography,
computed tomography (CT), endoscopic retrograde
cholangiopancreatography (ERCP), magnetic resonance
cholangiopancreatography (MRCP) and endoscopic
ultrasonography (EUS) in detecting the main causes of
extrahepatic colestasis. Although in bile duct pathology,
and especially in the evaluation of patients with jaundice,
transabdominal ultrasonography is the first choice
exploration, helicoidal CT, ERCP and MRCP are often
required to establish the local cause of jaundice, local and
distant consequences evaluation, appreciation of surgical
intervention opportunity and choice of the right therapeutic
method.
Key words
Transabdominal ultrasonography - extrahepatic
cholestasis - imaging methods
Introduction
Extrahepatic cholestasis is defined as the impossibility
of inflow into the duodenum of a normal quantity of bile
due to into lesions or obstacles at the level of the
choledochus or the common hepatic duct.
The main causes of extrahepatic cholestasis are: common
bile duct (CBD) stones, cholangiocarcinoma, ampullary
carcinoma, pancreatic diseases (pancreatic head carcinoma,
pseudotumoral chronic pancreatitis, pancreatic head
pseudocysts), CBD strictures and congenital malformations
(cysts, Caroli disease), duodenal diverticulas, ascaridiasis,
hemobilia. CBD dilatation can appear in some particular
conditions (postcholecystectomy or in elderly people)
without pathological significance.
Transabdominal ultrasonography (TUS) is the first
choice examination used for the etiological diagnosis of
extrahepatic cholestasis because it is a noninvasive, fast
method and presently widely accessible. The main
ultrasonographic sign is the dilatation of the principle bile
duct over 7 mm, associated, in most cases with intrahepatic
bile duct dilatations and/or gallbladder dilatation.
Presently, authors agree that the most accurate asses-
sment for extrahepatic bile ducts obstacle is the increase of
the common hepatic duct over 5 mm or the intrahepatic bile
ducts diameters over 40% of the accompanying portal branch
caliber.
A particular situation is represented by cases with
extrahepatic cholestasis without CBD dilatation in patients
with transitory or intermittent bile ducts obstruction. In these
situations transient increase of bilirubin and cholestasis
enzymes is detected but no ultrasonografic modifications
of CBD caliber (stone passage).
US evaluation of CBD size frequently leads to lower
values compared with radiological procedures as
intravenous cholangiography or ERCP. These differences
are determined by measurements effectuated at different
levels, radiological magnification, choleretic and distension
effects due to the contrast substance. Ultrasonographic
measurements are performed in the proximal part of the bile
duct while the radiological measurements are peformed in
the maximum diameter of the bile duct (usually the distal
part).
TUS permits distinction between extrahepatic and
intrahepatic cholestasis, but has a lower sensibility (50-80%)
in identifying the etiology of biliary obstruction. For this
Rogoveanu et al 266
reason, in many situations, it is necessary to combine it
with other imaging techniques - endoscopic retrograde
cholangiopancreatography (ERCP), computed tomography
(CT), endoscopic ultrasonography (EUS) or magnetic
resonance cholangiography (MRCP) - that increase the
diagnosis accuracy to 95-99%.
CBD stones
Ultrasonographic identification of bile duct dilatations
represents an important indicator of stone presence.
The CBD dilatation realizes at the level of hepatic hilum
the double shot gun sign. A particular ultrasonographic
aspect is represented by passage choledoch. Small
gallbladder stones can pass through CBD and can be
spontaneously eliminated without realizing a permanent
biliary obstacle. The recurrence of this obstruction leads to
loss of the CBD wall elastic properties and persistence of
dilatation.
Ultrasound specificity for CBD stones diagnosis is 95-
100% but, the sensitivity is lower (58-68%) and even lower
if the stones have less than 1 cm (1-4) (Fig.1).
Ultrasonographic modern methods (tissue harmonic
imaging, 3D examination) increase the examination sensibility
and allow to obtain images as accurate as ERCP or MRCP.
TUS is also necessary for selecting patients who will
undergo ERCP examination before laparoscopic cholecystec-
tomy. Rigorous criteria of selection must be used (CBD
stones ultrasonographically visualized and/or jaundice),
criteria which permit a significant decrease of incidents and
accidents inherent to an invasive procedure (Fig.2).
MRCP visualizes pancreatic and billiary ducts and
obtains similar images as ERCP, without using contrast
substance (5). CBD stones are easily identified on T
2
ponderate images, but the method has a higher cost than
TUS.
EUS allows evaluation of extrahepatic cholestasis
because of the excellent visualization of extrahepatic bile
ducts by duodenal placing of the transductor and avoiding
of intestinal gas. Intrahepatic bile duct visualization is more
difficult especially for the right lobe because of the
ultrasound limited penetration. Small CBD stones (under 3-
4 mm) can be observed at ERCP with superior accuracy even
if they do not have acoustic shadow. EUS permits the
establishing of the number, location and stone size, cystic
and bile ducts diameters, cystic duct implantation,
gallbladder aspect (Fig.3). The sensitivity of the method is
over 90% and its specificity is over 95% for CBD stones
diagnosis, with higher accuracy than TUS or CT. The
disadvantages are long-time learning and the high cost of
necessary equipment.
In conclusion, TUS remains the first method used to
diagnose bile duct stones because of its simplicity and high
specificity. Tissue harmonics and 3D examination lead to
high quality images and obviously the improvement of the
methods sensitivity.
Cholangiocarcinoma
Bile ducts carcinoma (cholangiocarcinoma) can spread
to the entire billiary tract and, when situated in the hepatic
hilum invading the hepatic confluence, it is called Klatskin
tumor.
At TUS, it is visualized as a tissular formation which is
prominent in the bile duct lumen and determines their
proximal dilatation. Some forms progress only with a discreet
thickness of the bile ducts wall without direct visualization
of the tumor. The distal forms evolve with the dilatation of
the entire billiary tract, inclusively the gallbladder and,
sometimes, with portal vein invasion (malignant thrombosis)
(6,7) (Fig.4).
Klatskin tumor determines only intrahepatic bile ducts
dilatations, with impossible visualization of right and left
hepatic duct confluent. Cholangiocarcinoma must be
ultrasonographically differentiated from hepatocarcinoma
or gallbladder carcinoma with bile duct invasion (for Klatskin
tumor), or by pancreatic head carcinoma and ampullary
carcinoma (for distal cholangiocarcinoma). Intrahepatic bile
duct tumors must be differentiated by primary sclerosing
cholangitis (intrahepatic bile ducts dilatations not so
obvious) (8-10).
TUS in these situations must be associated with other
imaging methods.
Technical progress in EUS allows visualization of hepatic
hilum by using low frequency transductors (5 MHz) with
high penetration or intraductal EUS with endoscopically or
percutaneously introduced transductors (11) (Fig.5).
CT and CT cholangiography have a better accuracy
compared with TUS, especially the spiral technique, which
allows a precise evaluation of the transition area between
dilated and undilated zone of CBD. Blunt termination of
CBD is a cholangiographical sign correlated with
malignancy, while progressive narrowing is an argument for
benign stenosis. Focal, excentric thickening of the main bile
duct proximal to obstruction is suggestive for a cholangio-
carcinoma.
ERCP and MRCP sensitivity are similar in cholangio-
carcinoma diagnosis; one of the major advantages of ERCP
is the possibility of collecting tissue samples by brush
procedure for etiological diagnosis of biliary stenosis (Fig.
6).
Ampullary carcinoma
TUS shows indirect signs of the tumor: intra and
extrahepatic bile duct dilatations, gallbladder enlargement
with sludge in high quantity. Rarely is the ampular tumor
visualized as a round or oval hypoechoic formation relatively
well defined, which is situated between the dilated CBD and
duodenum (Fig.7).
TUS shows secondary changes (hepatic metastases,
hepatic hilum lymph nodes and ascites in peritoneand
carcinomatosis) and color Doppler technique is useful for
the appreciation of local vascular invasion (12,13).
Imaging of extrahepatic cholestasis 267
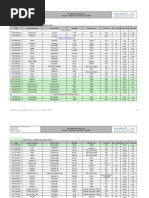
Fig.1 Transabdominal ultrasonography: common bile duct stone. Fig.4 Transabdominal ultrasonography: cholangiocarcinoma
(billiary tract dilatation).
Fig.2 Endoscopic retrograde cholangiopancreatography: common
bile duct stone.
Fig.5 Endoscopic ultrasonography: cholangiocarcinoma
visualisation of hepatic hilum.
Fig.3 Endoscopic ultrasonography: common bile duct stone. Fig.6 Endoscopic retrograde cholangiopancreatography: cholangio-
carcinoma.
CT scan detects periampullary formations over 2 cm with
accuracy over 90% but it does not permit differential
diagnosis of these tumors. If the ampullary carcinoma is
small (under 2 cm), the CT scan shows only bile duct or
pancreatic duct dilatation (14,15).
EUS allows visualization of duodenal papilla as a round
or oval hypoechoic formation with over 5 mm size (normal
diameter of Vaters ampulla) from which dilated pancreatic
and CBD start. The method permits detection of ampullary
Rogoveanu et al 268
Fig.7 Transabdominal ultrasonography: ampullary carcinoma. Fig.10 Transabdominal ultrasonography: pancreatic head pseudo-
cyst.
Fig.8 Endoscopic image in ampullary carcinoma. Fig.11 Computed tomography: pancreatic pseudocyst.
Fig.9 Endoscopic ultrasonography: ampullary carcinoma. Fig.12 Endoscopic retrograde cholangiopancreatography: stenoses
and dilatations of Wirsung duct in chronic pancreatitis.
tumors in 93% of the cases comparatively with 7% by TUS
and respectively 29% by CT (16-18) (Figs. 8,9).
Although ERCP is essential for ampullary carcinoma
diagnosis, local tumor extension and regional lymph node
metastasis can be evaluated only by EUS. The two methods
are complementary because EUS does not allow
differentiation between benign and malignant ampular
tumors. Upper digestive endoscopy and ERCP remain the
principal diagnostic methods for ampullary carcinoma
because they permit correct localization and biopsy col-
Imaging of extrahepatic cholestasis 269
Fig.13 Endoscopic ultrasonography: chronic pancreatitis. Fig.16 Endoscopic ultrasonography: pancreatic head adeno-
carcinoma.
Fig.14 Endoscopic ultrasonography: pancreatic pseudocyst. Fig.17 Endoscopic retrograde cholangiopancreatography:
pancreatic head adenocarcinoma with retrograde dilatations of bile
ducts and Wirsung duct.
Fig.15 Transabdominal ultrasonography: pancreatic head
adenocarcinoma.
Fig.18 Transabdominal ultrasonography: common bile duct cyst.
excluding other causes of extrahepatic cholestasis and for
therapeutic interventions (ampullectomy, endoscopic
sphincterotomy with/without stenting) (19).
lecting under directly visually control. Lateral view
endoscope tubes facilitate papilla visualization and biopsy
or brush procedure from stenosis. ERCP is also useful for
Rogoveanu et al 270
Pancreatic diseases which cause
extrahepatic cholestasis
Acute pancreatitis. TUS has a limited role because of
examination difficulties caused by dynamic ileus or obesity.
The method is efficient in tracking down the trigger causes
(gallbladder lithiasis with migrated stones) or in visualizing
complications (pancreatic head pseudocysts which
determine extrahepatic cholestasis and for percutane
drainage of these collections (20,21).
CT scan is superior to TUS because it permits a better
visualization of glandular changes and those from pancreatic
area, quantification of lesion severity and visualization of
local and distal complications (22).
Chronic pancreatitis pseudotumoral form. At TUS
the pancreas structure appears intensely inhomogeneous,
with visualization of some nodular, tissular formations,
relatively well defined which imposes differential diagnosis
with pancreatic tumors and frequently realizes compression
on neighboring structures (CBD, duodenum, stomach, splenic
vein). The absence of neighboring lymph node and hepatic
metastases pleads for pancreatic benign tumors, but EUS-
guided fine needle aspiration is required to be certain.
Pancreatic head pseudocysts which appear in chronic
pancreatitis can be ultrasonographically visualized as
transonic formations well delimitated distorting the capsule
and the border of the organ. In evolution, the wall of these
tumors becomes thicker (over 3 mm) and indicates surgical
intervention. The echoic circumscribed images inside the
pseudocysts are suggestive for the presence of sequesters
(23) (Fig.10).
CT is necessary when the information offered by TUS is
insufficient and inconclusive. It is a sensible method which
shows small calcifications unvisualized by other methods,
pancreatic pseudocysts and also their contacts with
neighboring vessels and organs (Fig.11).
ERCP is the most precise method for diagnosing
obstructive chronic pancreatitis because it permits visuali-
zation of Wirsung collaterals which are dilated and with
irregular caliber even in early phases of the disease. In the
case of pseudocysts, ERCP shows the number, localization
and size as well as eventual communication with
intrapancreatic canales (Fig.12).
EUS has a better sensitivity as compared with TUS and
CT (88% versus 56% respectively 75%). The method permits
an early diagnosis of morphological changes before the
alteration of pancreatic functional tests and allows also
invasive procedures (EUS-guided fine needle aspiration or
drainage of localized collections) (Figs.13,14).
Pancreatic head adenocarcinoma
The adenocarcinoma is visualized at TUS as a tissular
tumor with a hypoechoic aspect compared with the rest of
pancreatic parenchyma, which has signs of invasion or
compression on CBD with significant dilatation. On oblique
sections at the level of hepatic hilum, terminal CBD shows
narrowing with pencil top aspect, secondary to tumoral
compression. Wirsung duct is proximally dilated (caliber over
20 mm) (24,25) (Fig.15).
CT is superior to TUS because it allows a better
visualization of pancreatic tumors inclusively in obese
patients and in patients with meteorism. Its accuracy is 95%
in detecting pancreatic cancer and its sensibility is 92% (for
helicoidal CT). The optimal sequences are obtained on arterial
and portal phases, with in bolus introduction of contrast to
determine the high levels of pancreatic capture. The
helicoidal CT examination is useful also for appreciating
distal invasion at the level of the liver, peritoneum, lymph
nods or vessels and for guiding fine needle aspiration for
tumor diagnosis (26,27).
MRI and MRCP do not offer significant advantages over
CT because of the movement artifacts, intestinal gas opacities
and spatial resolution inferior to helicoidal CT (28).
EUS is useful for pancreatic cancer staging and in the
appreciation of vascular invasion (accuracy 72-90%) but
does not allow visualization of distant hepatic and lymph
node metastases (Fig. 16). Helicoidal CT is inferior to EUS in
small tumor detection and staging, and for the assessment
of tumor resectability (accuracy 83% vs 91%) but has the
advantage of good visualization of metastases.
ERCP is considered the best imaging method for
pancreatic head cancer diagnosis with a sensitivity of 95%
and specificity of 85%, and the cytological sample obtained
from pancreatic duct can establish the malignancy diagnosis
with a sensitivity of 60% (Fig.17).
CBD cysts
TUS visualization of cystic dilatations is easy (29)
(Fig.18), but differential diagnosis difficulties with
gallbladder malformations, simple hepatic cysts, pancreas
head cysts etc. can appear, which can hinder the information
offered by CT, ERCP or EUS.
Conclusions
In bile duct pathology and especially in patients with
jaundice, TUS is the first choice exploration following
medical history and clinical examination.
TUS offers rapid information which allows in most cases
the differentiation between extrahepatic and intrahepatic
cholestasis.
The use of the new techniques (Doppler, tissue
harmonic, contrast agents, 3D examination) improves
significantly the image quality and facilitates the etiological
diagnosis in extrahepatic malignant cholestasis.
The association between EUS, helicoidal CT, ERCP or
MRCP is often necessary for identifying the cause of
jaundice, for local and systemic evaluation, for indicating
the surgical intervention and choosing the right therapeutic
method.
References
1. Costi R, Sarli L, Caruso G et al. Preoperative ultrasonographic
assessment of the number and size of gallbladder stones: is it a
Imaging of extrahepatic cholestasis
useful predictor of asymptomatic choledochal lithiasis? J
Ultrasound Med 2002; 21: 971-976.
2. Moparty B, Bhutani MS. Endoscopic Ultrasonograpy for
Choledocholithiasis and Biliary Malignancy. Curr Treat Options
Gastroenterol 2005; 8: 135-142.
3. Stabile Ianora AA, Memeo M, Scardapane A et al. Oral contrast-
enhanced three-dimensional helical-CT cholangiography:
clinical applications. Eur Radiol 2003; 13: 867-873.
4. Okada M, Fukada J, Toya K, Ito R, Ohashi T, Yorozu A. The
value of drip infusion cholangiography using multidetector-
row helical CT in patients with choledocholithiasis. Eur Radiol
2005; 15: 2140-2145.
5. Ng KK, Wan YL, Lui KW et al. Three-dimensional magnetic
resonance cholangiopancreatography for evaluation of
obstructive jaundice. J Formos Med Assoc 1997; 96: 586-592.
6. Chahal P, Baron TH. Cholangiocarcinoma. Curr Treat Options
Gastroenterol 2005; 8: 493-502.
7. Mansfield SD, Barakat O, Charnley RM et al. Management of
hilar cholangiocarcinoma in the North of England: pathology,
treatment, and outcome.World J Gastroenterol 2005; 11: 7625-
7630.
8. Khan SA, Thomas HC, Davidson BR, Taylor-Robinson SD.
Cholangiocarcinoma. Lancet 2005; 366: 1303-1314.
9. Stroszczynski C, Hunerbein M. Malignant biliary obstruction:
value of imaging findings. Abdom Imaging 2005; 30: 314-323.
10. Albu S, Tantau M, Sparchez Z et al. Diagnosis and treatment of
extrahepatic cholangiocarcinoma: results in a series of 124
patients. Rom J Gastroenterol 2005; 14: 33-36.
11. Tio TL, Tytgat GN. Endoscopic ultrasonography of bile duct
malignancy and the preoperative assessment of local
resectability. Scand J Gastroenterol Suppl 1986; 123: 151-157.
12. Kamisawa T, Tu Y, Egawa N et al. Clinicopathologic features of
ampullary carcinoma without jaundice. J Clin Gastroenterol
2006; 40: 162-166.
13. Martin JA, Haber GB.Ampullary adenoma: clinical
manifestations, diagnosis, and treatment. Gastrointest Endosc
Clin N Am 2003; 13: 649-669.
14. Midwinter MJ, Beveridge CJ, Wilsdon JB, Bennett MK, Baudouin
CJ, Charnley RM. Correlation between spiral computed
tomography, endoscopic ultrasonography and findings at
operation in pancreatic and ampullary tumours. Br J Surg 1999;
86: 189-193.
15. Lim JH, Lee DH, Ko YT, Yoon Y. Carcinoma of the ampulla of
Vater: sonographic and CT diagnosis. Abdom Imaging 1993;
18: 237-241.
16. Shin HJ, Lahoti S, Sneige N. Endoscopic ultrasound-guided fine-
needle aspiration in 179 cases: the M. D. Anderson Cancer
Center experience. Cancer 2002; 96: 174-180.
17. Zhang Q, Nian W, Zhang L, Liang J. Endoscopic
ultrasonography assessment in preoperative staging for
carcinoma of ampulla of Vater and extrahepatic bile duct. Chin
Med J 1996; 109: 622-625.
18. Buscail L, Pages P, Berthelemy P, Fourtanier G, Frexinos J,
Escourrou J. Role of EUS in the management of pancreatic and
ampullary carcinoma: a prospective study assessing resectability
and prognosis. Gastrointest Endosc 1999; 50: 34-40.
19. Brambs HJ, Claussen CD. Pancreatic and ampullary carcinoma.
Ultrasound, computed tomography, magnetic resonance imaging
and angiography. Endoscopy 1993; 25: 58-68.
20. Brocchi E, Piscaglia F, Bonora M et al. Echo-enhanced
ultrasonography: is it the future gold standard of imaging in
acute pancreatitis? JOP 2005; 6: 464-466.
21. Yeung YP, Lo SF, Yip AW. Role of ERCP in the management of
predicted mild acute biliary pancreatitis. Asian J Surg 2003; 26:
197-201.
22. Gurleyik G, Emir S, Kilicoglu G, Arman A, Saglam A. Computed
tomography severity index, APACHE II score, and serum CRP
concentration for predicting the severity of acute pancreatitis.
JOP 2005; 6: 562-567.
23. Nemes R, Curca T, Paraliov T et al. Cystic tumors of the
pancreas. Considerations upon 34 operated cases. Rom J
Gastroenterol 2002; 11: 303-308.
24. Freelove R, Walling AD. Pancreatic cancer: diagnosis and
management. Am Fam Physician 2006; 73: 485-492.
25. Yassa NA, Yang J, Stein S, Johnson M, Ralls P. Gray-scale and
color flow sonography of pancreatic ductal adenocarcinoma. J
Clin Ultrasound 1997; 25: 473-480.
26. Taouli B, Vilgrain V, OToole D, et al. Intraductal papillary
mucinous tumors of the pancreas: helical CT with
histopathologic correlation. Radiology 2000; 217: 757-764.
27. Heinrich S, Goerres GW, Schafer M et al. Positron emission
tomography/computed tomography influences on the
management of resectable pancreatic cancer and its cost-
effectiveness. Ann Surg 2005; 242: 235-243.
28. Ly JN, Miller FH. MR imaging of the pancreas: a practical
approach. Radiol Clin North Am 2002; 40: 1289-1306.
29. Todani T, Watanabe Y, Toki A, Morotomi Y. Classification of
congenital biliary cystic disease: special reference to type Ic
and IVA cysts with primary ductal stricture. J Hepatobiliary
Pancreat Surg 2003; 10: 340-344.
271
You might also like
- Developmental Status of 1-Year-Old Infants Fed Breast Milk, Cow's MilkDocument9 pagesDevelopmental Status of 1-Year-Old Infants Fed Breast Milk, Cow's MilkwizardebmNo ratings yet
- SitusDocument1 pageSituswizardebmNo ratings yet
- Types of Leukemia ExplainedDocument4 pagesTypes of Leukemia ExplainedwizardebmNo ratings yet
- Three Randomized Controlled Trials of Early Long-Chain PolyunsaturatedDocument9 pagesThree Randomized Controlled Trials of Early Long-Chain PolyunsaturatedwizardebmNo ratings yet
- Types of Leukemia ExplainedDocument4 pagesTypes of Leukemia ExplainedwizardebmNo ratings yet
- Recommended Adult Immunization ScheduleDocument14 pagesRecommended Adult Immunization SchedulewizardebmNo ratings yet
- From Emerging Infectious DiseasesDocument2 pagesFrom Emerging Infectious DiseaseswizardebmNo ratings yet
- Newborn Copy 2Document7 pagesNewborn Copy 2wizardebmNo ratings yet
- Non-Cirrhotic Portal Hypertension - Diagnosis and ManagementDocument8 pagesNon-Cirrhotic Portal Hypertension - Diagnosis and ManagementwizardebmNo ratings yet
- Cholecystitis Gallbladder Liver Gallbladder: Cholecystitis - Overview What Is Cholecystitis?Document4 pagesCholecystitis Gallbladder Liver Gallbladder: Cholecystitis - Overview What Is Cholecystitis?wizardebmNo ratings yet
- Non-Cirrhotic Portal Hypertension - Diagnosis and ManagementDocument8 pagesNon-Cirrhotic Portal Hypertension - Diagnosis and ManagementwizardebmNo ratings yet
- Cholecystitis Gallbladder Liver Gallbladder: Cholecystitis - Overview What Is Cholecystitis?Document4 pagesCholecystitis Gallbladder Liver Gallbladder: Cholecystitis - Overview What Is Cholecystitis?wizardebmNo ratings yet
- From Emerging Infectious DiseasesDocument2 pagesFrom Emerging Infectious DiseaseswizardebmNo ratings yet
- Sepsis Induced CholestasisDocument12 pagesSepsis Induced CholestasisYusuf Hakim AjiNo ratings yet
- Update on Surviving Sepsis 2008 GuidelinesDocument34 pagesUpdate on Surviving Sepsis 2008 GuidelineswizardebmNo ratings yet
- Aetiology and Outcome of Neonatal Cholestasis in MalaysiaDocument6 pagesAetiology and Outcome of Neonatal Cholestasis in MalaysiawizardebmNo ratings yet
- 2004 Concise Review DX Hemolytic AnemiaDocument8 pages2004 Concise Review DX Hemolytic AnemiaKrishnakant PrajapatiNo ratings yet
- Syndrome of Inappropriate Anti Diuretic Hormone Secretion Complicated With Stem Cell TransplantationDocument7 pagesSyndrome of Inappropriate Anti Diuretic Hormone Secretion Complicated With Stem Cell TransplantationwizardebmNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Formulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemideDocument3 pagesFormulation Science & Bioavailability: Pharmacological Parameters Study On Loop Diuretic Drug - FurosemidevivianNo ratings yet
- Brandon A. Gaudiano - Incorporating Acceptance and Mindfulness Into The Treatment of Psychosis - Current Trends and Future Directions (2015, Oxford University Press)Document305 pagesBrandon A. Gaudiano - Incorporating Acceptance and Mindfulness Into The Treatment of Psychosis - Current Trends and Future Directions (2015, Oxford University Press)Vartax100% (2)
- Herbal Hair CareDocument52 pagesHerbal Hair CareRam PrasadNo ratings yet
- Waste Water Treatment For Dairy IndustryDocument34 pagesWaste Water Treatment For Dairy IndustryNational WaterNo ratings yet
- Capstone Project PDFDocument38 pagesCapstone Project PDFapi-461805331No ratings yet
- A Project ReportDocument80 pagesA Project ReportShakun VidyottamaNo ratings yet
- Pharmed First CaseDocument5 pagesPharmed First Casesajal kumarNo ratings yet
- Investigations in UrologyDocument19 pagesInvestigations in UrologyMohammed AadeelNo ratings yet
- 5 Sore ThroatDocument45 pages5 Sore ThroatNurul Wandasari SNo ratings yet
- Brain WavesDocument2 pagesBrain WavesAntonio PlanellesNo ratings yet
- Handbook of Transfusion MedicineDocument96 pagesHandbook of Transfusion MedicineJoana Bessa83% (6)
- Hospital Document Hospital Information Form (PSP)Document7 pagesHospital Document Hospital Information Form (PSP)DR.Umesh PatkarNo ratings yet
- Infection Control Product CatalogDocument48 pagesInfection Control Product CatalogStericycleNo ratings yet
- Shiatsu and Drug and Substance and Alcohol AbuseDocument7 pagesShiatsu and Drug and Substance and Alcohol AbuseStreza G VictorNo ratings yet
- Abu Dhabi Plan Drug ListDocument45 pagesAbu Dhabi Plan Drug ListicebreakNo ratings yet
- The Effect of Massage Therapy On Chemotherapy-Induced Nausea and Vomiting in Pediatric CancerDocument7 pagesThe Effect of Massage Therapy On Chemotherapy-Induced Nausea and Vomiting in Pediatric CancerAgito Dedi100% (2)
- Anger ManagementDocument4 pagesAnger ManagementAmron Azman100% (1)
- Getshredded2 0Document39 pagesGetshredded2 0Carlos Alberto Acevedo80% (5)
- Medication Use in Older Adults by Rose Knapp, MSN, RN, APRN-BC, ANPDocument34 pagesMedication Use in Older Adults by Rose Knapp, MSN, RN, APRN-BC, ANPJose Antonio Tous OlagortaNo ratings yet
- Consumer Medicine Information Arrow - Ranitidine: What Is in This LeafletDocument8 pagesConsumer Medicine Information Arrow - Ranitidine: What Is in This LeafletmustikaarumNo ratings yet
- Form Sop SampleDocument12 pagesForm Sop SampleAlka AzzwarsNo ratings yet
- Fba Functional Behavior Assessment Template 1 - 3Document4 pagesFba Functional Behavior Assessment Template 1 - 3api-338037250No ratings yet
- Rehabilitation Guidelines For Posterior Cruciate Ligament ReconstructionDocument6 pagesRehabilitation Guidelines For Posterior Cruciate Ligament ReconstructionMono MostafaNo ratings yet
- AMTA Covered Modalities ListDocument8 pagesAMTA Covered Modalities Listbackch9011No ratings yet
- Mccann2015 Chori BarDocument15 pagesMccann2015 Chori BarMarko BrzakNo ratings yet
- Dreams as a Portal to Inner Wisdom: A Guide to Clinical Dream InterpretationDocument16 pagesDreams as a Portal to Inner Wisdom: A Guide to Clinical Dream InterpretationLeslie Rodriguez FranciscoNo ratings yet
- Case Study OBDocument19 pagesCase Study OBLele Alwayzthesame KearneyNo ratings yet
- PsychiatryDocument23 pagesPsychiatryharpalmehanNo ratings yet
- Improving Sleep QualityDocument10 pagesImproving Sleep Qualityapi-349689592No ratings yet
- CASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationDocument4 pagesCASP Randomised Controlled Trial Standard Checklist: Main Issues For ConsiderationIful SaifullahNo ratings yet