Professional Documents
Culture Documents
Alfa Bloqueo Anestesia RM
Uploaded by
Martin CanaleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Alfa Bloqueo Anestesia RM
Uploaded by
Martin CanaleCopyright:
Available Formats
CORRESPONDENCE
The need for preoperative a-adrenergic blockade
for ganglioneuroma excision
SIRGanglioneuromas (GNs) are rare, benign, fully differentiated tumors that arise most commonly from the
sympathetic ganglia in the posterior mediastinum in
adolescents and young adults. The treatment involves
complete surgical excision and has an excellent prognosis. Compared with malignant neuroblastomas and
ganglioneuroblastomas, which frequently produce catecholamines, GNs secrete catecholamines only occasionally. The release of catecholamines during surgery,
which is one of the most feared complications, can be
catastrophic and difficult to manage. For this reason,
the British Paediatric Society of Endocrinology and Diabetes (BPSED) (1) and the panel of experts at the First
International Symposium on Pheochromocytoma (2)
have recommended that all patients with a biochemically positive pheochromocytoma should receive mandatory a-adrenergic blockade before any surgical
intervention. GNs are usually excised without such precaution, and there are no recommendations to suggest
the need for preoperative a-adrenergic blockade in these
cases. We report a unique case of ganglioneuroma excision that was unexpectedly complicated by the episodic
hypertensive spells upon tumor manipulation.
A 4-year-old boy presented with two-day history of
progressive ataxia to pediatric accident and emergency
three weeks after having chickenpox. At presentation,
he had broad-based gait with tendency to fall on right
side. His reflexes were slightly brisk in lower limbs. The
rest of neurological examination and blood pressure was
normal. His blood glucose, serum electrolytes, and full
blood picture were normal. The serum and urine toxicology screen was negative. Neurology opinion was sought,
and the ataxic gait was thought to be consistent with
cerebellitis. Chest X-ray showed a large lobulated posterior mediastinal mass projecting over right hemithorax
with pressure erosion of the right third rib. Computed
tomography (CT) of chest and abdomen showed a posterior mediastinal mass with numerous stippled features
in keeping with neurogenic tumor. Urinary catecholamines were requested, and thoracoscopic biopsy was performed to identify the tumor, which confirmed the
diagnosis of ganglioneuroma. There were no spikes in
blood pressure intraoperatively.
A week later, due to worsening ataxia and inability to
bear weight, magnetic resonance imaging (MRI) of chest
and spine was performed and revealed epidural extension of the tumor through wide intervertebral foramina
from the level of 1st thoracic/2nd thoracic intervertebral
2013 John Wiley & Sons Ltd
disc cranially to the level of 5th thoracic/6th thoracic
caudally with spinal cord compression. He then had
spinal laminectomy to relieve the cord compression.
During this surgery, he started having cyclical spikes of
blood pressure with systolic blood pressures ranging
from 50 to 200 mmHg. This was attempted to be controlled with glyceryl trinitrite infusion and phenylepherine boluses. Postoperatively, plasma normetanephrine
was noted to be increased at 3454 pmoll 1 (normal
range 1201180). Urine catecholamine/creatinine ratios
were increased for norepinephrine at 478 nmolmmol 1
creat (normal range 17194) and for dopamine at
1204 nmolmmol 1 creat (normal range 59901) with
urinary creatinine being 3.5 mM (normal range 7
18 mM). Testing for vanilylmandelic acid (VMA) and
homovanillic acid (HVA) is not available in this institution. A follow-up CT spine after 8 weeks showed small
residual intraspinal tumor with minimally increased thoracic component of the tumor that continued to displace
the mediastinal structures. MRI spine performed
6 months later showed no residual intraspinal soft tissue
component with minimally increased right paramediastinal mass. He then had further surgical excision, and this
time, it was performed with preoperative a-adrenergic
blockade using phenoxybenzamine as per BPSED pheochromocytoma guidelines. He stayed very stable during
the surgery with no hypertensive crises.
The literature regarding childhood GN is scarce, especially on such a relevant issue of surgical approach. A
retrospective study by the Italian Co-operative Neuroblastoma Group concerning a large number of patients
registered as GN over a 27-year period also did not
report any case of surgery complicated by hypertensive
crisis (3). Also, a literature search on the perioperative
management of neuroblastomas was also carried out
with inconclusive results and recommendations. A large
review of 20 years (4) experience showed <3% incidence
of intraoperative hypertension during neuroblastoma
resection and recommended only a-blocking those
patients with significant preoperative signs and symptoms of catecholamine excess. Another large review of
11 years (5) experience confirmed the same and did not
recommend any specific optimal anesthetic regimen. The
downside to routine recommendation of a-adrenergic
blockade for all neurogenic tumors is the subsequent
delay in surgery in newly diagnosed neuroblastomas and
the potential detrimental effect this can have on prognosis of the child.
1
Correspondence
In conclusion, this case highlights the need for the recognition of the fact that, like pheochromocytomas, safe
surgical excision of ganglioneuromas may require
appropriate a-adrenergic blockade and guidelines need
to devised for perioperative management in such
patients. Further studies are needed to compare preoperative urinary catecholamines quantitatively to surgical
complications as a result of catecholamine release which
might provide criteria for a-adrenergic blockade in specific patients. In the meantime, surgeons and anesthetists
need to be aware of this possible complication and be
prepared for hypertensive crises that can occur.
Conflict of interest
No conflict of interests declared.
Chandan Gupta, Noina Abid, Keith Bailie, Mark Terris,
Alistair Dick & Anthony McCarthy
Royal Belfast Hospital for Sick Children, Belfast, UK
Email: chandan_gupta60@yahoo.com
doi:10.1111/pan.12335
References
1 BSPED | British Society for
Paediatric Endocrinology and
Diabetes | Clinical [Internet]. Available
at: http://www.bsped.org.uk/clinical/
clinical_endorsedguidelines.html. Accessed
13, February 2013.
2 Pacak K, Eisenhofer G, Ahlman H et al.
Pheochromocytoma: recommendations for
clinical practice from the First International
Symposium. Nat Clin Pract Endocrinol Metab
2007; 3: 92102.
3 De Bernardi B, Gambini C, Haupt R et al.
Retrospective study of childhood ganglioneuroma. J Clin Oncol 2008; 26: 17101716.
4 Haberkern CM, Coles PG, Morray
JP et al. Intraoperative hypertension
during surgical excision of neuroblastoma.
Case report and review of 20 years
experience. Anesth Analg 1992; 75:
854858.
5 Kain ZN, Shamberger RS, Holzman RS.
Anesthetic management of children with
neuroblastoma. J Clin Anesth 1993; 5:
486491.
2013 John Wiley & Sons Ltd
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Breast Unit SOP: Checklist While Giving ROIS AppointmentDocument7 pagesBreast Unit SOP: Checklist While Giving ROIS AppointmentAbhinav Ingle100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Health Referral System Manual - Central VisayasDocument103 pagesHealth Referral System Manual - Central VisayasAlfred Russel Wallace50% (10)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Simple Technique To Measure The Volume of Removed Buccal FatDocument3 pagesA Simple Technique To Measure The Volume of Removed Buccal FatGuilherme GuerraNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Updates in Ophthalmic Anaesthesia in AdultsDocument7 pagesUpdates in Ophthalmic Anaesthesia in AdultsJossiel OlivaresNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Clinical Application of Nightingale TheoryDocument9 pagesClinical Application of Nightingale TheoryHina Nizar100% (2)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- To Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesDocument4 pagesTo Evaluate The Efficacy of Ultrasonography Guided Pectoral Nerve Block For Postoperative Analgesia in Breast SurgeriesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Batu Ren, Batu Ureter Dan Onko NewDocument29 pagesBatu Ren, Batu Ureter Dan Onko Newilham masdarNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Revised Dentist (Code Od Ethics) Regulations, 2014 PDFDocument10 pagesThe Revised Dentist (Code Od Ethics) Regulations, 2014 PDFRohit AgrawalNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 279667.locs IiiDocument16 pages279667.locs IiiSiomay IkanNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Tam MannaDocument2 pagesTam MannaYashwanth GowdaNo ratings yet
- Como Analizar Un ArticuloDocument4 pagesComo Analizar Un ArticuloAlvaro Alvarez RiveraNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Career GuidanceDocument19 pagesCareer GuidanceAbdul JalilNo ratings yet
- General Surgery&plastic Surgery Board-Part One Exam Blueprint (v.1)Document4 pagesGeneral Surgery&plastic Surgery Board-Part One Exam Blueprint (v.1)Mohammed S. Al Ghamdi100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 4.2 MDS01 - Definition Table of The MDS Items - Ver0.94Document7 pages4.2 MDS01 - Definition Table of The MDS Items - Ver0.94AriniDwiLestariNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Operating Room ConceptsDocument47 pagesOperating Room ConceptsLoungayvan Batuyog100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
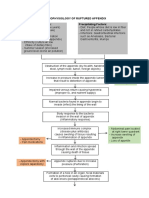
- Pathophysiology of Ruptured AppendixDocument2 pagesPathophysiology of Ruptured AppendixAya PaquitNo ratings yet
- Minor Surgical Procedures in Maxillofacial SurgeryDocument65 pagesMinor Surgical Procedures in Maxillofacial SurgerydrzibranNo ratings yet
- Hubungan Tindakan Perawatan Luka Dengan f8dc88cdDocument8 pagesHubungan Tindakan Perawatan Luka Dengan f8dc88cdRD OfficialNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Incisions January June 2014Document40 pagesIncisions January June 2014Raine Bow100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Financial Planning and ForecastingDocument6 pagesFinancial Planning and ForecastingMaryam UmairNo ratings yet
- ERAS - ProtocolDocument5 pagesERAS - ProtocolShakya WeeraratneNo ratings yet
- Daftar Harga Indosopha 2012 Bp. Edward Roy Palangkaraya PDFDocument5 pagesDaftar Harga Indosopha 2012 Bp. Edward Roy Palangkaraya PDFBoyke WinterbergNo ratings yet
- NCLEX Test Questions With RationaleDocument46 pagesNCLEX Test Questions With Rationaletetmetrangmail.com tet101486No ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Cleft Lip and Palate: Current Surgical ManagementDocument3 pagesCleft Lip and Palate: Current Surgical ManagementFarisa BelaNo ratings yet
- Organizational Structure - ApolloDocument13 pagesOrganizational Structure - ApolloIpreetponnamma86% (7)
- MediCAD Brochure 2D + 3D (Except Shoulder)Document16 pagesMediCAD Brochure 2D + 3D (Except Shoulder)kocis_pNo ratings yet
- Isjna Vol 17 2 Summer 2018Document72 pagesIsjna Vol 17 2 Summer 2018Nissa KurniaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- CH 5Document153 pagesCH 5sojithesouljaNo ratings yet
- 5.2spatial Translations Administrative Office Matrix DiagramDocument3 pages5.2spatial Translations Administrative Office Matrix DiagramAthena AciboNo ratings yet
- Exam 2Document4 pagesExam 2Azra MuzafarNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)