Professional Documents
Culture Documents
ENT-Lec 4 Diseases of The Salivary Glands and Hypopharynx
Uploaded by
Eliza Paula BacudOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ENT-Lec 4 Diseases of The Salivary Glands and Hypopharynx
Uploaded by
Eliza Paula BacudCopyright:
Available Formats
1st Shifting Transcription by Ray Albert R.
Cabigan
Otolaryngology (ENT)
Disorders of The Salivary Glands
(Benign)
Source: Boeis, L., Adams, G. and Hilger, P.
(1989). Fundamentals of
Otololarynglogology. Pp 282-316.
Philidelphia, W.B. Saunders Company
Transcribed by: Ray Albert Cabigan
Facial nerve leaves the skull through the
stylomastoid foramen. In the parotid gland,
the nerve separates into the cervicofacial
and termporofacial nerves.
Temporofacial nerve then separates
into the temporal and zygomatic branch
Cervicofacial separates into cervical,
marginal mandibular and buccal division
Passage of the facial nerve through the
parotid gland divides the parotid gland into
a superficial lobe and the deep lobe.
Deep lobe is in close contact with CN IX, X,
XI, XII and division of external carotid artery
in to the superficial temporal and internal
maxillary arteries
Parotid gland is the largest salivary gland.
Parotid duct (Stensens duct) is 6cm long
and arises from the anterior portion of the
gland. The duct opens at the 2nd upper
molar tooth
Submandibular gland lies beneath the
horizontal ramus of the mandible. In
digastric triangle. Whartons duct is 6cm
long and opens lateral to the lingual
frenulum
Sublingual glands lie beneath the anterior
floor of the mouth.
INFLAMMATORY DISORDERS
Acute Parotitis
Most common is mumps
Recurrent sialdenitis occurs in children
inflammation of one or both glands
Acute Suppurative Parotitis occurs in
debilitated or elderly persons who may be
partially dehydrated. Sudden inflammation.
Usual causative agent is S. aureus. IV
antibiotitcs is a must. Incision and drainage
is done as well as radiation exposure to rid
of the disease.
Acute Submandibular Gland
Sialadenitis
Rare in the submandibular gland.
Chronic Sialdenitis
Long standing, frequently recurring
episodes of glandular swelling and
discomfort from the major salivary glands
Chronic sialdenitis of the parotid associated
with recurrent calculi, mucous plugs or
strictures is known as sialodochiectasis
Sialectasis may involve one or more
salivary glands.
Parotid gland is the most frequently
involved. Where there is no observable
obstruction, dilatation of the ducts are
done.
In cases where medical intervention does
not work, parotidectomy may be done.
Salivary gland calculi (sialolithiasis)
occurs more commonly in the
submandibular gland. Fever occurs when
infection develops.
Sialdenitis of the submandibular lgand is
more frequenly treated by surgery
SYSTEMIC DISEASE
Parotid gland is most often involved.
Sarcoidosis of the parotid (Heerfordts
syndrome / uveoparotid fever). Diffusely
swollen duct with slight tenderness. Facial
nerve paralysis.
Benign lymphoepithelial disease (chronic
punctuate parotitis). Mostly in women.
Associated with rheumatoid disorders. Little
dots. Acinar atrophy. Oral dryness
Sjogrens syndrome, chronic parotitis plus
2-3 additonal entities (xerophthalmia or
xerostomia or rheumatoid disorder). Usually
involves the parotids. 44x more chance of
developing lymphoma.
SIALORRHEA
Drooling. Cerebral palsy, demyelinating
disorders, Parkinsons.
1st Shifting Transcription by Ray Albert R. Cabigan
Treated surgically rerouting; removal of
the gland; tympanectomy combined with
chorda tympani resection;
RADIOLOGICAL ASSESSMENT OF THE
MAJOR SALIVARY GLANDS
Radiosialographic Scanning
Depends on increased concentration of
iodine in saliva compared to plasma
Parotid and sumbmandibular gland.
Normal = symmetric and smooth
Tumor = area of decreased uptake
Sialography
Injection of water- or oil-soluble contrast
material into submandibular or parotid
gland.
Useful in chornic disorders of the parotid
gland such as recurrent sialdenitis,
Sjogrens or ductal obstruction.
CI in the presence of recent, acute
inflammation of the gland
Computed Tomography
Single most useful radiographic diagnostic
test of the salivary gland masses.
Normal parotid gland appears less dense
than the surrounding structures
Tumors (most common is pleomorphic
adenoma) is well defined, slightly
enhancing mass.
BENIGN TUMORS OF THE SALIVARY
GLANDS
Children
Most common benign gland tumor of
children is parotid gland hemangioma.
Bluish discoloration and fluctuation in size
of the mass when the child cries. Gradual
inrase in size during 1st 4 6 mos of life.
Lymphagioma arises also in the parotid
3rd most common tumor is the pleomorphic
adenoma and is the most common solid
tumor found in children
Tumors in children frequently involve the
parotid glands. Submandibular and minor
salivary gland areas are uncommon sites.
Adults
Primary site of origin for benign tumors is
the parapharyngeal space. From salivary
glands that arose from deep lobe of parotid
gland and from vagus nerve or cervical
sympathetic chain pushes lateral
pharyngeal wall medially.
Most common tumor of the space is
pleomorphic adenoma; second most
common is malignant adenocystic
carcinoma. The largest group of toher
tumors are of neurogenic origin
(schwannomas and neuromas).
Pleomorhpic adenoma (benign
mixed tumor)
accounts for 75% of parotid gland
tumors. No pain or facial nerve
weakness. Treated by complete
surgical resection.
Extracapsular extension of the tumor
may occur. The whole gland has to be
removed to prevent recurrence.
Recurrent tumors may undergo
malignant degeneration (< 6%
incidence)
Pleomorphic adenoma is also the
most common benign tumor of the
submandibular gland as well as the
minor salivary glands. Frequently on
the palate near the midline at the
junction of the hard and soft palates.
Papillary adenocystoma
lymphomatosum (Warthins Tumor)
Most common in 50-60 year old
males. Most common tumor to occur
bilaterally. Surgical resection,
recurrence is unlikely
Benign Laryngeal Disorders
Pain from the base of the tongue, the
epiglottis or the piriform sinus is referred to
the ear first symptom
dyspnea and stridor are usually late and
serious symptoms
SPECIFIC METHODS OF DIAGNOSIS
Indirect (mirror) laryngoscopy or fiberoptic
instrument
1st Shifting Transcription by Ray Albert R. Cabigan
Direct examination through local or general
anesthetic.
Auscultation of the larynx differentiates
laryngeal stridor from bronchial stridor
Palpation
CT and MRI
Voice recordings
Esophagogram
CONGENITAL ANOMALIES
Infants C2-C4; 7mm anteroposterior, 4mm
lateral
Adults C4-C6
Laryngomalacia
No underlyikng pathologic or progressive
disorder. Exaggeration of soft flabby state
of the larynx. Larynx collapses on
inhalation. Swallowing is unaffected. Normal
cry, weight gain and development. Stridor.
Chest retraction leading to pectus
excavatum. Occurs 7weeks and above.
Good prognosis, clears when cartilage
becomes rigid by 12th 15th month.
Congenital Subglotting Stenosis
Subglotting diameter < 4mm. stridor at
birth. Most cases require tracheotomy. More
than one congenital anomaly may exist
Webs
75% glottic, 12% subglottic, 12%
supraglottic. Airway and cry are affected.
Begins at birth. Treated surgically, laser or
dilatation
Congenital Cysts
Airway obstruction, failure to grow. Normal
voice and swallowing. Cysts from the base
of the tongue, aryepiglotting folds or false
cords.
Hemangioma
Tumor that occurs primarily in infants under
6mos of age. . 50% have an external
hemangioma. Stridor. Vascular
abnormalities. May regress by 12th month.
Normal voice or swalling. Smooth
compressible mass on the posterior or
lateral wall.
Laryngocele
Resid from a small appendix or saccus of
laryngeal ventricle. May be at any age. May
present as a mass in the neck on the same
side to which it is grows. Stridor and airway
obstruction. Diagnosed via aspiration
biopsy. Dissection is a must.
Laryngotracheoesophageal cleft
Rare. Failure of fusion of the dorsal portions
of the cricoid cartilage. Failure of the
closure of the tracheoesophageal septum.
Cyanosis, respiratory distress, recurrent
pneumonia. Changes in cry.
Neurogenic Disorders of the Newborn
Vocal cord paralysis from birth canal
trauma, meningocele, masses, etc.
Unilateral paralysis. breathy poor cry, no
respiratory distress (lateral). Stridor, DOB
(median).
Bilateral paralysis. Good cry, poor
respiratory exchange.
Paralysis recovers in 6 9 mos.
LARYNGEAL TRAUMA
Contusions of the Larynx
Internal hematoma, dislocation of
arytenoids.
Laryngeal Fracture
Hyoid fracture no airway obstruction
separation of the greater cornu from the
body
Fractures (vertical) of the thyroid cartilage
are common. s/s:
1. hx of a blow to the neck
2. hoarseness
3. inspiratory and/or espiratory stridor
4. hemoptysis
5. subcutaneous emphysema
airway obstruction, facial pain. Thyroid
cartilage cannot be palpated.
Usually accompanies cervical spine injuries.
Avulsion occurs when there is damage to
the recurrent laryngeal nerves
Laryngeal and Subglottic Stenosis
Narrowing of airway due to scars. Heroic
therapy received by some patients with
endotracheal tubes causes stenosis of the
airway.
Intubation Granuloma
1st Shifting Transcription by Ray Albert R. Cabigan
Rare. Abration of vocal process of
arytenoids leading to granuloma formation.
Mild hoarseness. No airway obstruction.
Often bilateral.
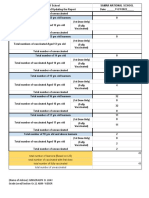
1. acute supraglottitis (epiglottitis)
rapidly fatal; sits up with open mouth
and chin forward, no hoarseness;
dysphagia
2. acute sublottic laryngitis hoarse,
Allergic Diseases of the Larynx
very croupy cough, lies down
Obstructive edema upon contact with
s/s: stridor, retraction and
allergen.
cyanosis
Rapid treatment is a must. IV insertion of
INFECTIOUS DISEASE OF THE LARYNX
fluids and inhalation of antibiotics is
Croup
recommended. Steroids to reduce
Infection of the larynx resulting to stridor
inflammation. Support should be provided if
and airway obstruction. Any age. Most
RR > 40 and PR > 160 with continuous
common in <6y.o.
restlessness
Two types
Most cases resolve in 48-72hours when
treated promptly.
Laryngotracheobronc Bacterial
Spasmodic
Supraglottis
hitis (infraglottitis)
tracheitis
croup
Incidence
36
<3
8 15
15
(age in
years)
Onset
Hours
Days
1-2 week period
Rapid onset,
of respiratory
usually
infection with
evening
rapid
deterioration
Voice
Clear
Hoarse
Barking cough
Dysphagia
Yes
None
Inspiratory stridor
Drooling
Position of
relief
Recurrence
Yes
Sitting up
No
Recumbent
-Recumbent
Rare
Yes
--
Course
Radiograph
Rapid
Supraglottic
edema
Days to weeks
Normal
Yes; intubation
needed to remove
secretions or
pseydomembrane
s
-Irregular margins
in trachea
Organisms
H. influenzae
(most
common),
strep, virus
Virus
S. aureus most
common; H.
influenzae
--
Acute Laryngitis
Occurs due to vocal abuse, toxic fumes,
infections. Usually a paninfection. Influenxa
virus, adenovirus, streep. Diphtheria if
No associated
infection
Yes; relieved
by humidity or
cold
Yes
--
---
there is (-) immunization hx and there is the
presence of a membrane. Further abuse
may result to hemorrhage and development
of nodules
1st Shifting Transcription by Ray Albert R. Cabigan
SYSTEMIC DISORDERS WITH
LARYNGEAL MANIFESTATIONS
1. Rheumatoid arthritis fixed vocal
cord
2. Hypothyroidism
3. Infiltrative disorders supraglottic
larynx, hoarseness and dysphagia.
Diffuse edema without ulceration of
the supraglottic larynx.
Histoplasmosis can cause
simultaneous ulceration of the larynx
and oral cavity. Pepmhigus vulgaris
ulcerated laryngeal surface covered
with whitish membrane
4. Chronic Granulomatous Infections
TB, syphilis, leprosy, candida
5. Androgen Therapy
CHRONIC NONSPECIFIC LARYNGITIS
Conditions characterized by hoarsenss and
long standing inflammatory changes due to
irritation by allergens, smoke or acid reflux,
in the laryngeal mucosa. Red and thickened
vocal cords. Unimpaired vocal cord motility.
Treated by removal of ffending cause and
treating underlying disorders.
BENIGN TUMORS OF THE LARYNX
Vocal Nodules
Unilateral as a result of improper use of
vocal cords. May be soft loosely edematous
tumor or firm, fibrous growth or vacular.
Diffuse Vocal Cord Polyposis
Polypoid degeneration associated with
prolonged coval use, smoking and
persistent inflammation. Aftger surgery,
smoking must be stopped otherwise
recurrence is likely
Contact ulcer
More commonly in men. Granuloma
formation due to forceful contacts of
arytenoids cartilages. Pain and vocal
change. Speech therapy aids resolution.
Juvenile Papilloma
Most common tumor of the larynx in
children. 18mos-7years. Involution at
puberty. May recur. Hoarseness and
abnormal cry. May be hormone dependent
and may enlarge enough to cause airway
obstruction. Treated by precise surgical
removal. Malignancy associated with
smoking
Granular Cell Myoblastoma
Tongue and larynx. Hoarsenss.
Pseudoepitheial hyperplasia.
Chondroma
Slow growing tumors of hyaline cartilage
arising from cricoid, thyroid, arytenoids or
epiglottic cartilages
Leukoplakia or Erythroplakia
Leuko white; erythro red. Vocal cords are
most often affected. Hoarseness. There may
be hyperkeratosis (most often), carcinoma
in situ or frank carcinoma. Surgical removal
with cessation of smoking.
NEUROGENIC DISORDERS OF THE
LARYNX
Vocal Cord Paralysis
Caused by any lesion in the course of the
recurrent laryngeal nerve. Lesions in the
CNS and brain stem that affects the larynx
also include other pathologies. May be
through compression or through trauma.
Unilateral cord paralysis may cause airway
obstruction in children because of the small
airway. Mobility of the paralyzed vocal cord
may be regained if the recurrent laryngeal
nerve is in a paramedian position such that
it can grow to compensate the loss of the
nerve on the other side (6-12mos)
Bilateral cord paralysis voice is less
affected though glottis is small. Dyspnea
even at rest. Majority requires
tracheostomy. Abducted cords are due to
trauma weak breathy voice; easy
breathing. Adducted cords are due to
neurologic lesions good voice; poor
airway.
1st Shifting Transcription by Ray Albert R. Cabigan
Superior
Laryngeal
Paralysis
Paralysis of
cricothyroid
muscle; sensory
loss in half of
larynx
Unilateral
Recurrent Nerve
Paralysis
Paralysis of all
intrinsic muscles
on one side
Bilateral
Recurrent
Nerve Paralysis
Paralysis of all
intrinsic muscles
Effect
Loss of pitch;
aspiration
Hoarse; good
airway except in
small children;
breathy voice;
poor cough
Good voice; poor
airway especially
on exertion
Similar to
corresponding
lesions of
recurrent
paralysis; more
likely to aspirate
Examinatio
n
Anterior
commissure looks
tilted to side of
lesion; areytenoid
on that side tilts in
Cord in
paramedian
position; no
lateral motion
Vocal cords do not
move laterally;
some patients
adapt and exist
with decreased
exercise tolerance
Cords are
immobile but in
intermediate
postiiokjn due to
loss of adduction
by cricothyroid
muscle.
Pathology
Idiopathic Laryngeal Aspiration
Compromised valve function = aspiration of
food or liquid
results to coughing, choking and
laryngospasms. Brain stem disorders may
result to aspiration also.
Spastic dysphonia
Strained, hoarse voice often staccato-like
due to hyperadduction of the true and false
cords. Tension larynx. Best therapy is
resectioning of he right recurrent laryngeal
nerve. Unknown etiology
Myasthenia gravis
All ages. Muscle weakness with use.
Involves eye or facial muscles.
Amyotrophic Lateral Sclerosis
Patients in 50s or 60s. swallowing and
speech dysfunction. Tongue dysfunction
with fasciculations are more common.
FUNCTIONAL DISORDERS OF THE
LARYNX
Psychogenic Aphonia
Total inability to talk. Larynx looks and
moves normally. Normal cough. Hx of
emotional disturbance
Complete
Paralysis
Vagus nerve lesion
above the superior
laryngeal nerve;
may be unilateral
or bilateral
Dysphonia Plicae Ventricularis
Phonation with false cords vibrating instead
of the true vocal cords husky voice
Normal larynx, false cords overhangs true
cords.
Vocal Weakness
Voice lacks usual tone and vigor. Voice
breaks and drops in pitch. Slightly bowed
vocal cords. More prominent among the
elderly.
Benign Disorders of The Salivary
Glands, Nasopharynx and Hypopharynx
DISEASES OF THE NASOPHARYNX
Choanal Atresia
Congenital anomalie where in during
embryonic life, the nasomembrane fails to
open up.
May be lateral or bilateral
Unilateral = persistent unilateral nasal
discharge
Bilateral atresia results to no breathing
among the infants.
May be membranous or bony.
Requires establishment of airway.
1st Shifting Transcription by Ray Albert R. Cabigan
Diagnosis
Suction catheter test automatic.
Choanagram
Axial CT scan Gold Standard
To determine laterality
To determine composition and
thickness of plate
To determine other possible
causes of upper airway
obstruction
To check for other causes of
upper airway obstruction
Treatment
Surgery; if one side only, there is no
need to operate immediately
Mitomycin C anti-granulation
prevents recurrence after surgery.
Hypertrophic Adenoditis
It is not normal to see children breathing
through the mouth.
There is hyponasality of the voice. There is
prominent outer teeth and arched palate
occurs. Conductive hearing loss occurs also.
The most common symptom is the
obstructive sleep apnea syndrome
temporary cessation of respiration during
sleep of more than a few minutes.
Persistent mouth breathing
Excessive day time sleepiness
Restless ness
High arched palate.
Pushed out upper dentition
not all obstructive sleep apnea is caused by
hypertrophic adenoids.
Central sleep apnea or Pickwinian syndrome
Enlarged adenoids also enlarge with tonsils.
Etiology
Uncontrolled allergy; infection
Exaggerated growth of the lymphoid
components of the orodigestive tract
Diagnosis
Soft tissue lateral view x-ray which
includes the oropharynx and the
nasopharynx.
Treatment surgery
Juvenile Nasophagreal Angiofibroma
Grows on the lateral wall near the pterygoid
fossa.
Patient may complain of ear problems due
to obstruction of Eustachian tube
A benign lesion composed of overgrowth of
blood vessels and fibrous tissue in the
nasopharynx. The vascularity results
predominantly profuse recurrent epistaxis,
exclusive males. Age range 7 14y.o.,
average of 15-17y.o. Profuse bleeding is
pales of blood.
Internal maxillary artery may be embolized
to reduce the vascularity of the mass using
Teflon.
The disease is histologically benign but
clinically malignant since it is capable of
involving the skull.
Indications for Adenoidectomy
1. Obstructive sleep apnea
2. Chronic purulent nasopharyngitis
3. Chronic adenoid hypertrophy
4. Acute suppurative otitis media
5. Selected cases of chronic otitis media
6. Biopsy purposes
BENIGN DISEASES OF THE SALIVARY
GLANDS
Two broad categories of salivary glands =
major and minor
Major salivary glands are located outside of
the oral cavity parotid; submandibular;
sublingual. They have a duct system.
Compound tubulo acinar glands
Minor salivary glands are located within the
oral cavity. The have a simple ductal
system.
Both categories provide serous or mucus
secretions
Acute suppurative sialadanetitis
One of the most common disease affecting
the parotid and submandibular glands
Bacterial disease. More common in the
Parotid Gland
1st Shifting Transcription by Ray Albert R. Cabigan
There is Salivary Stasis
Predisposing Factors
1. post operative conditions
2. sialolithiasis
3. duct strictures
4. dehydration
5. poor oral hygiene
a sore that gets clogged up resulting to
stasis
usually one sided. With redness
S/s
Fever, malaise, swollen tender gland;
pus from the duct orifice
Treatment
Hydration, gland massage,
antibiotics, incision and drainage
Chronic Recurrent Sialadenitis
More common in the parotid
Decreased saliva production and stasis
There is recurrent. Mild, painful gland
enlargement associated with eating, there
is scanty saliva and dry mouth
Treatment
Treat predisposing factors.
Sialogogues, gland massage, duct
ligation in refraction cases, radiation
of the gland when in old individuals
(therapeutic doses of radiation)
Sialolithiasis
Involves the submandibular gland in 80% of
cases because:
saliva is more viscous
saliva is more alkaline
greater concentration of Ca and PO4
salivation is antigravity
there is recurrent suppurative sialdenitis
Treatment
Stone removal and gland excision
Diagnosis
Majority of the stones are radiopaque
90% of stones in submandibular
gland. Stones of the parotid gland are
90% radiolucent.
Sialography should not be done when
there is acute inflammation
Sialadenosis
Non inflammatory, non-neoplastic
enlargement of the salivary gland due to
salivary stasis. Usually in the Parotid
No treatment is usually done
Etiology
Obesity, malnutrition, DM, alcoholic
acidosis,
Viral Infections
Epidemic parotitis
Salivary inclusion disease
Non tender enlargement of the parotid
gland, bilateral without redness
Cystic Lesions
Congenital dermoid, ductal, branchial
arch-groove cyst
Acquired mucocele. Opening of the duct
closes up allowing accumulation of the
saliva within the tissues. Ranula occurs
when the submandibular gland becomes
clogged up a special form of mucocele.
Granulomatous Diseases
TB
Sarcoidosis
Actinomycosis
Benign Lymphoepithelial Lesion
End-stage of chronic recurrent sialadenitis
Usually affects one gland
Presents as asymptomatic enlargement
A small percentage may become Lymphoma
or Carcinoma
a.k.a. Godwins tumor
Treatment
Symptomatic and supportive
Excision if uncosmetic
Sjogrens syndrome
Selective destruction of all salivary and
lacrimal glands. Lymphocyte0-mediated
autoimue attack. 90% of lymphoma
Bilateral parotid elargemnt. Dry eyes. Dry
mouth with halitosis.
1st Shifting Transcription by Ray Albert R. Cabigan
Definitive diagnosis is buccal biopsy (lips)
Treatment requires referral to immunologist.
Diagnosis
Buccal biopsy
Markers RF, ANA, SDA, PCA, TGA,
TMA
Benign tumors
Children
Hemangioma
Vascular proliferative tumors
Lesions
Lymphangiomas
Lympohepitheila
Tumors
Warthins Tumor
Adults
Benign mixed tumor most common now
Warthins tumor
Oncocytoma
Monomorphic adenoma
7/10 tumors occurs in the parotid. As the
gland becomes smaller, the incidence of
malignancy increases.
BENIGN TUMORS
Benign mixed tumor or the
pleomorphic adenoma
The most common benign tumor of all
major salivary glands
Most commonly found in the parotid
Warthins tumor or papillary
lymphomatosum
Exclusive to the parotid gland. Second most
common. Presents as a slow growing mass
at the tail of the parotid. May occur
bilaterally takes up Tc Tracer.
Oncocytoma
Less than 1% of all salivary glands
No other signs and symptoms
Exclusive in parotid and among the elderly.
How can one tell if a parotid mass is
malignant
1. lysis of the mandible
2. skin involvement dimpling,
ulceration, etc.
3. involvement of the facial nerve
4. rapid growth
5. spread to other areas of the face,
indicated by trismus
6. cervical lymphadenopathy
Trauma
Simple lacerations with gland or duct
involvement. May occur with blunt trauma
Benign Laryngeal Disorders
3 anatomic regions of the larynx
1. glottic area / glottis tip of the epiglottis
1 cm below the vocal cords
2. supraglottis from the tip of the
epiglottis 1 cm above the vocal cords
3. sub / infra glottis area below the glottic
area.
Two sphincter like parts of the larynx
1. aryepiglottic folds
2. false vocal cords
3. true vocal cords
3 functions of the laryn
1. respiration
2. airway protection
3. phonation
Intrinsic muscles of the larynx
innervated by the recurrent laryngeal nerve
1. posterior cricoarytenoids the only
abductor
2. interarrytenoid adductor
3. lateral cricoarytenoid adductor
4. thyroarytenoid / internal
thyroarytenoid / vocalis minor
tensor
innervated by superior laryngeal nerve
5. cricothyroid main tensor; passive
adductor
Congenital Disorders
laryngomalacia
o most common
o immaturity of the laryngeal
skeleton flaccid larynx.
Collapses whenever the child
inhales. (subglottis is sucked
in)
o omega shaped epiglottis. No
need for treatment
1st Shifting Transcription by Ray Albert R. Cabigan
inspiratory stridor (obstruction
above vocal cord) and dyspnea
subglottic stenosis
o second most common
laryngeal congenital disorder
o obstruction is right after the
true vocal cord
o inspiratory stridor
o due to an overdeveloped
cricoid cartilage or
membranous formation
adjacent to the cricoid
cartilage resulting to an
obstructed airway
o may be fatal
o membranous stenosis requires
laser incision
o over developed cricoid
requires surgery to widen the
cricoid. Bone grafts may be
inserted in between a split
cricoid to increase the airway
diameter
o no need for a definitive
treatment
webs
o web may occur in any area of
the larynx
o no airway obstruction
o aphonia may occur if located
in the glottis. There may be a
weak cry
o management requires laser
incision
o most common site is the
Glottis i.e. glottic web
cysts
o Mucus retention cyst may
occur in any area of the larynx.
Dysphagia, muffled voice
o Endoscopic excision for small
cysts
o External excision may be
required for some cases
Hemangioma
o Maintain patient in steroids
o Deformative disorder
Laryngocoele
10
Inborn but may occur in the
adult life during the second or
third decade
o May be internal or external or
both
o Treatment is through incision
o If the cyst becomes filled with
mucus, it is called a saccular
cyst.
o Progressive dyspnea without
disturbance in voice
laryngotracheoesophageal cleft
o failure of the walls between
the larynx and the esophagus
does not close
o most common symptom is
aspiration pneumonia
o surgery is done by the cardio
thoracic surgeons
neurogenetic anomalies
o
Trauma induced Disorders
Fractures
o Dyspnea may occur due to
hematoma. Immediate
problem is not the trauma
itself but the effects that it has
on the larynx. There may be
hoarseness or dysphonia.
Hemoptysis may also occur
o Electroplating is required to
restore the capacity of the
vocal cords
o Sign would be that of
flattening splaying of the
thyroid cartilage
o Airway should be made
Acquired Subglottic Stenosis
o Due to prolonged endotracheal
intubation
o Prolonged intubation increases
the risk of developing the
disease
o Membranous stenosis requires
laser incision
o Tracheal incision with end to
end anastamosis is made in
more severe cases
4 tracheal rings may be
resected beyond that,
graft must be made
1st Shifting Transcription by Ray Albert R. Cabigan
Intubation Granuloma
Infections
Acute laryngitis
o Voice abuse is the most
common cause
o Hoarseness is the most
common presentation
Epiglottitis / supraglottitis
o Supraglottitis comes in with
complaints of difficulty of
breathing or severe
odynophagia.
o Diagnosis may be done by
direct observation
o Otherwise there may be the
need of the soft tissue
rardiography of the neck which
shows a thumb sign
o Tracheostomy does not
necessarily be; endotracheal
intubation is suggested since
the disease disappears in a
couple of days
o However, if the lesion is large
tracheostomy is needed
o Crubet or an oxygen tent is
combined with epinephrine
and steroids. Voice is not
affected since it is a
suppraglottic lesion which
results to muffled voice
Subglottic laryngitis
Laryngotracheobronchitis
o Common sequela from
measles / post measles MTB
o Brassy / metallic cough
o Condition does not lead to
obstruction
o Treated with the same airway
management procedures for
supraglottitis except airway by
pass
Spasmodic croup
Benign Mucosal Disorders all conditions
result to hoarseness; diagnosed by direct /
indirect examination; all treatments are
coupled with voice rest.
11
Chronic laryngitis
o Long standing changes
thickening, changes in color
o recurrent
Vocal cord nodules
o Most common
o Anterior and middle third of
the larynx due to its location
as the point of maximum
contact. Like a callus
Vocal cord polyp
o Pedunculated and can move in
and out with respiration
Diffuse vocal cord polyposis /
Reinkes edema
o Common among smokers
Contact ulcer / granuloma
o Located at the posterior chain
of the larynx
o Treated by excision biopsy
Vocal Cord Paralysis usually a negative
etiology. i.e. all may be called idiopathic. It
is important to know which nerve is
paralyzed recurrent laryngeal nerve or
supralaryngeal
Unilateral
o Left is more affected than the
right, poor voice, good airway.
breathy voice
o Voice may be regained
o Medialization may be done to
restore voice if not regained
Bilateral
o Poor airway, good voice
o Transaction of the nerve is not
a certainty.
o Lateralization may be done to
provide air way and maintain
voice
Idiopathic
Superior laryngeal nerve paralysis results to
aspiration especially to fluids
Most common benign tumor of the upper
airway and the larynx = papilloma
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Surgical Pathology Diseases of The Thyroid and ParathyroidDocument13 pagesSurgical Pathology Diseases of The Thyroid and ParathyroidEliza Paula BacudNo ratings yet
- Brain Stimulation Methods PsychiatryDocument49 pagesBrain Stimulation Methods PsychiatryEliza Paula BacudNo ratings yet
- Surgical Pathology Thyroid GlandDocument24 pagesSurgical Pathology Thyroid GlandEliza Paula BacudNo ratings yet
- Microbiology - Fundamentals of Immunology InfectionDocument19 pagesMicrobiology - Fundamentals of Immunology InfectionEliza Paula BacudNo ratings yet
- Formulary Clinical PharmacologyDocument30 pagesFormulary Clinical PharmacologyEliza Paula BacudNo ratings yet
- Serum Markers For The Diagnosis of Myocardial InfarctionDocument4 pagesSerum Markers For The Diagnosis of Myocardial InfarctionEliza Paula BacudNo ratings yet
- Microbiology - Fundamentals of CHEMOTHERAPHYDocument21 pagesMicrobiology - Fundamentals of CHEMOTHERAPHYEliza Paula BacudNo ratings yet
- Viral Infections of The Nervous SystemDocument11 pagesViral Infections of The Nervous SystemEliza Paula BacudNo ratings yet
- Neurology: Multiple Sclerosis and Allied Demyelinative DiseasesDocument10 pagesNeurology: Multiple Sclerosis and Allied Demyelinative DiseasesEliza Paula BacudNo ratings yet
- Esophagus and Stomach Surgical Pathology 2015Document18 pagesEsophagus and Stomach Surgical Pathology 2015Eliza Paula BacudNo ratings yet
- Neurology: Degenerative Diseases of The Nervous System-Dementing DisordersDocument8 pagesNeurology: Degenerative Diseases of The Nervous System-Dementing DisordersEliza Paula BacudNo ratings yet
- 2nd SHIFTING EXAM Schedule and CoverageDocument2 pages2nd SHIFTING EXAM Schedule and CoverageEliza Paula BacudNo ratings yet
- Neurology: Degenerative Diseases of The Nervous System 2 - Movement DisordersDocument13 pagesNeurology: Degenerative Diseases of The Nervous System 2 - Movement DisordersEliza Paula BacudNo ratings yet
- Maxillofacial Injuries ManagementDocument7 pagesMaxillofacial Injuries ManagementEliza Paula BacudNo ratings yet
- Approach To A The Child With A Fever and RashDocument7 pagesApproach To A The Child With A Fever and RashlaureeateNo ratings yet
- Nutritional Pathology: Vitamins, Minerals and Their FunctionsDocument4 pagesNutritional Pathology: Vitamins, Minerals and Their FunctionsEliza Paula Bacud100% (3)
- Diarrhea (Pedia)Document8 pagesDiarrhea (Pedia)Eliza Paula BacudNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Diff Diag PDFDocument16 pagesDiff Diag PDFDana Ysabelle IbarraNo ratings yet
- MCQ FMS 3 (2016) With Answers-1Document17 pagesMCQ FMS 3 (2016) With Answers-1stella pangestikaNo ratings yet
- Kounis Syndrome A Pediatric PerspectiveDocument10 pagesKounis Syndrome A Pediatric PerspectiveAna Belén Artero CastañoNo ratings yet
- Drug Study On PpudDocument3 pagesDrug Study On PpudLezelle Mandane CardinoNo ratings yet
- Kelantan Obstetrics Shared Care Guideline Finale1 10 3Document100 pagesKelantan Obstetrics Shared Care Guideline Finale1 10 3JashveerBedi0% (1)
- Cleaning of OtDocument7 pagesCleaning of Otvinod balajiNo ratings yet
- Objective of full mouth rehabilitationDocument5 pagesObjective of full mouth rehabilitationSheeba AnilNo ratings yet
- Indications For Gingivoectomy and GingivoplastyDocument4 pagesIndications For Gingivoectomy and Gingivoplastyade ismailNo ratings yet
- List Summary of Sanjay Sharma MRCP Part 2Document22 pagesList Summary of Sanjay Sharma MRCP Part 2Ruku KhanNo ratings yet
- TORCH in PregnancyDocument122 pagesTORCH in PregnancyroserosannaNo ratings yet
- Case 3: Aortic StenosisDocument11 pagesCase 3: Aortic StenosisfmNo ratings yet
- Maternal Child NursingDocument24 pagesMaternal Child NursingRodneyDanielsdnip100% (33)
- Lupin To Market New Inhaler Under The Brand Name Loftair in India (Company Update)Document3 pagesLupin To Market New Inhaler Under The Brand Name Loftair in India (Company Update)Shyam SunderNo ratings yet
- Syncope - Approach To The Patient Dynamed 2020 PDFDocument76 pagesSyncope - Approach To The Patient Dynamed 2020 PDFHeriberto Moreno HernandezNo ratings yet
- Review Article: Chronic Inflammation in Obesity and The Metabolic SyndromeDocument10 pagesReview Article: Chronic Inflammation in Obesity and The Metabolic SyndromeBagas Umam AlwiNo ratings yet
- Acetaminophen Suppository Mechanism of Action Side Effects Nursing ResponsibilitiesDocument2 pagesAcetaminophen Suppository Mechanism of Action Side Effects Nursing ResponsibilitiesNiziu BearsNo ratings yet
- Samar National School COVID vaccination reportDocument1 pageSamar National School COVID vaccination reportCynthia LuayNo ratings yet
- Ararsa - Adherence of IFADocument49 pagesArarsa - Adherence of IFAgizachew belayNo ratings yet
- Implementation of The Filmarray Me Panel in Laboratory Routine Using A Simple Sample Selection Strategy For Diagnosis of Meningitis and EncephalitisDocument9 pagesImplementation of The Filmarray Me Panel in Laboratory Routine Using A Simple Sample Selection Strategy For Diagnosis of Meningitis and EncephalitisMohinish SNo ratings yet
- Phlebotomy Procedure 3rd PDFDocument4 pagesPhlebotomy Procedure 3rd PDFFranciska Gledy AmbaritaNo ratings yet
- Clinical Intake and MSEDocument5 pagesClinical Intake and MSEkashish behlNo ratings yet
- Colon Cleansing Kit Dosage CalendarDocument36 pagesColon Cleansing Kit Dosage CalendarYoungBodyNo ratings yet
- BLS MCQDocument22 pagesBLS MCQGeraldine Augusta100% (1)
- Invasive Cervical Traction Gardner Wells TongsDocument3 pagesInvasive Cervical Traction Gardner Wells TongsErvan Hartanto ErvanNo ratings yet
- Wound Healing, Tissue Repair, and FibrosisDocument28 pagesWound Healing, Tissue Repair, and FibrosisRibka Theodora100% (1)
- Epi NotesDocument5 pagesEpi NoteshoneykrizelNo ratings yet
- May June M&M SURGERY Presentation1Document27 pagesMay June M&M SURGERY Presentation1douglas mwaiNo ratings yet
- Nicotine Withdrawal SymptomsDocument6 pagesNicotine Withdrawal SymptomsNo OneNo ratings yet
- Prostate Biopsy - UpToDateDocument47 pagesProstate Biopsy - UpToDateCésar Aguirre RomeroNo ratings yet
- HERBOLOGY-WPS OfficeDocument110 pagesHERBOLOGY-WPS OfficeVijay KumarNo ratings yet