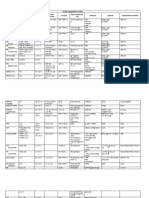
BLOOD COMPONENTS
BLOOD COMPONENTS AND
PLASMA DERIVATIVES
A. BLOOD COMPONENTS :
1. Whole blood
6. Granulocyte pheresis
2. Red blood cell
7. Platelet conc. (random donor)
3. Leukocyte reduced RBC 8. Platelet pheresis
4. Washed red blood cell
9. Leukocyte- reduced platelet
5. Frozen / deglycerolized RBC 10. RBC adenine saline added
B. PLASMA DERIVED COMPONENTS:
1. Fresh frozen plasma
2. Plasma
3. Cryoprecipitate
4. Factor VIII concentrate
5. Factor IX concentrate
6. Anti- inhibitor coagulation complex
7. Immune globulin
8. Albumin/plasma protein factor
�DIFFERENT SPEEDS USED IN THE PREPARATION OF
BLOOD COMPONENTS|:
HARD SPIN OR HEAVY SPIN :
5000 g - 5 minutes ( PRBC & PC)
5000 g - 7 minutes ( CRYOPPT, LP-RBC, OR
CELL FREE PLASMA)
LIGHT SPIN OR SOFT SPIN :
2000 g - 3 minutes ( PRP)
Preparation of Platelet Concentrate : centrifugation at
RT
Other blood components centrifugation at 1-6 0
�WHOLE BLOOD
*
For oxygen carrying capacity & volume replacement
For massive bleeding
*
*
*
No viable platelets or WBC
Decreased labile coagulation factors (Factors V & VIII)
Not an efficient utilization of blood
�PACKED RED BLOOD CELLS
* Treatment symptomatic anemia where
oxygen carrying capacity is needed
* For patient who cannot tolerate an increased
blood volume
�RBC ALIQUOTS
* For neonates
* For the treatment of anemia caused by :
* spontaneous fetomaternal hemorrhage
* obstetric accidents
* internal hemorrhage
�LEUKOCYTE REDUCED RED BLOOD
CELLS
* average unit of RBC contains 2X109 leukocytes
* a reduced leukocyte content to less than 5X 108
prevents repeated non- hemolytic febrile trans.
rxns.
* less than 5X106 prevent HLA sensitization
* reduces immunosuppression of recipient by
donor WBC
�* decreases post- operative surgical infections
due reduced immunosuppession
* reduced CMV transmission
* does not prevent graft versus disease
�WASHED RED BLOOD CELLS
* AIHA
* Paroxysmal nucturia hemoglobinuria
* for the rare patients with IgA deficiency
�FROZEN RED BLOOD CELLS
* used for :
* rare blood types for patients with
multiple antibodies
* autologous blood for a postponed
operation
�(GAMMA) IRRADIATED RBC s
* RBCs & platelets are exposed to gamma
irradiation at 25 rads for 4.5 minutes
* inactivates T lymphocytes in the donor unit &
prevents graft versus host disease in an
immunocompromised recipient
�FRESH FROZEN PLASMA (FFP)
* 200- 250 ml. of plasma frozen at - 180 C C
within 8 hours of collection
* no platelets available
* contains all coagulation factors
* an unconcentrated source of fibrinogen
( use cryo to correct a low fibrinogen level)
* needs 20-30 mins. lead time to thaw prior to
use
�* used in patients with multiple coagualtion factor
deficiencies :
* liver disease
* Vit. K deficiency
* DIC
* warfarin toxicity
* massive transfusin
* indicatated when PT /PTT are >17/55 sec.
* not used if non bleeding or for volume
replacement
�CRYPRECIPITATED AHF OR
CRYOPRECIPITATE
* the cold insoluble portion of plasma that
precipitates when FFP has been thawed bet.
1-6 0C.
* volume is 10- 15 ml.
* 30 mins. is needed for thawing & pooling
�* used primarily for the replacement of fibrinogen
which is indicated among patients with :
* liver failure
* DIC
* massive transfusion
or among those with congenital fibrinogen
deficiency.
* can also be a source of :
* Factor VIII
* Factor XIII
* Von Willebrand factor
�* No
longer considered a product of choice
for FVIII deficiency or Von Willebrands
disorder. These conditions are better
treated with :
* Factor VIII concentrate or
* with desmopressin acetate: DDAVP
( 1- deamino[ 8- D arginine]-vasopressin)
Quality Control:
1 U cryoprecipitate = 80-120 IU Factor VIII
150-250 mg fibrinogen
40-70% Von Willebrand factor
20-30% factor XIII
�Storage : 1 year if frozen at 18 0C
6 hours if thawed at 20-24 0 C
4 hours if pooled
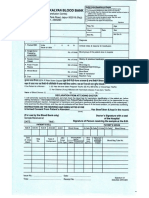
Application 1 : Cryoprecipitate transfusion for correcting
Fibrinogen level .
NOTE:
1.(Given weight in kilogram) x 70 ml/ [Link] weight= estimated
[Link] ( mL)
2. Estimated blood volume x ( 1.0- hematocrit) = estimated plasma
volume (mL)
�Required amount of fibrinogen =
[ Desired final fibrinogen ( mg/mL) Initial Fibrinogen (mg/ml] x
plasma volume
[ If concentration is expressed in mg/dL , simply divide by 100 to
convert to mg/L.]
1 U cryoprecipitate = 150 mg fibrinogen or
1 U cryoprecipitate = 250 mg fibrinogen
�Application 2 : Cryoprecipitate transfusion for correcting FVIII level.
1.(Given weight in kilogram) x 70 ml/ [Link] weight= estimated
[Link] ( mL)
2. Estimated blood volume x ( 1.0- hematocrit) = estimated plasma
volume (mL)
3. Required amount of FVIII=
[ Desired Final FVIII ( Units/ mL) Initial FVIII (Units/ mL] x plasma
volume
( If concentration is expressed in % , simply drop of % sign and write
units/ dL
To convert it to Units/mL., move 2 decimal places to the left.
1 U cryoprecipitate = 80 U FVIII
PLATELET CONCENTRATE
* Platelets are essential in primary hemostasis.
* Maybe prepared by processing unrefrigerated WB
within 6-8 hours after phlebotomy or through apheresis.
* Used among bleeding patients suffering from thrombocytopenia as a
result of problem in platelets:
* defective production or decreased function
* induced destruction as a result of radiation and chemotherapy.
QUALITY CONTROL:
* Random Donor Platelets ( RDP) : 5.5 x 10 10 platelets
* Single donoa Platelets (SDP) : 3.0 x 1011 platelets
* Storage : 20-24 0C ( RT or aircon temperature ) with constant
agitation
* Shelf Life : 3-5 days ( if pooled platelets within 4 hours of pooling
* ph 6.0
Each unit of platelet is expected to provide the following increase in
platelet count: ( Assume a typical 70 kg human)
RDP : 5,000 = 10,000/ uL
SDP : 20,000- 60,000/uL ( same effect with 4-6 pools of RDP)
Assesstment is made by calculating Corrected Count Increment (CCI)
* CCI RDP = ( Posttransfusion PC Pretransfusion PC x BSA
number of RDP transfused x 0.55
* CCI SDP
( Postransfusion PC Pretransfusion PC x BSA
number of SDP transfused x 3
Interpretation: > 10,000/uL (after 1 hr. posttransfusion) good increment
,< 5,000/uL (after 1 hr. posttransfusion) refractoriness
�GRANULOCYTE CONCONTRATE/ LEUKOCYTE
CONCENTRATE
* prepared by cytapheresis
* each product contain 1.0 x 1010 granulocytes if
steroids or HES or both are used
* granulocyte concentrate contain 200-600 mL of plasma
stored at 20-24 0C without agitation
� Granulocyte transfusions are done in :
cases of fever
septicemia or bacterial infection unresponsive
to antibiotic
reversible bone marrow hypoplasia
reasonable chance for patient survival
neonates with impaired neutrophil function
severe neutropenia
�PLASMA
* Formerly known as a liquid plasma or cryoprecipitate
poor plasma
* Has small amounts of Factors V and VIII
* Not recommended for patients with deficiency of either
of these clotting factors
* Recommended for :
the treatment of stable coagulation deficiency esp.
Factor XI
source of plasma for pts. undergoing plasma
exchange
�FACTOR VIII CONCENTRATE
* prepared by pharmaceutical firms by fractionation and
lyophilization of pooled plasma
* derived from plasma obtained by plasmapheresis
* stored at refrigerated temperature and is reconstituted
with saline at the time of infusion
* used to treat patients with hemophilia A or FVIII
deficiency
�CRYOSUPERNATE
* Plasma left after separation from WB of the
cellular components and cryoprecipitate
* Used for the treatment of :
bleeding disorders other than hemophilia
hypofibrinogemia
hypovolemia
�AUTOLOGOUS TRANSFUSION
Use of patients own blood, particularly useful in elective
surgery
Accounts for 5% of transfusions in USA
Reduces need for allogeneic BT
Reduces risk of postoperative complications
(e.g. infection, tumor recurrence)
�FOUR DIFFERENT TYPES OFAUTOLOGOUS
TRANSFUSION
1. Preoperative collection
2. Acute normovolemic heimodilution
3. Intraoperative collection
4. Postoperative collection
Duration of autologous transfusion:
Donor- patient may donate blood every 3 days but not
within 72 hrs. surgery ( to allow the patient plasma to
return to normal before surgery)
� 320 mg ferrous sulfate or ferrous gluconate is given 3X
daily as iron supplement if several units are required
within a few weeks.