Professional Documents
Culture Documents
Resuscitation: Leif Rognås, Troels Martin Hansen, Hans Kirkegaard, Else Tønnesen
Resuscitation: Leif Rognås, Troels Martin Hansen, Hans Kirkegaard, Else Tønnesen
Uploaded by
AmrothSingerilOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Resuscitation: Leif Rognås, Troels Martin Hansen, Hans Kirkegaard, Else Tønnesen
Resuscitation: Leif Rognås, Troels Martin Hansen, Hans Kirkegaard, Else Tønnesen
Uploaded by
AmrothSingerilCopyright:
Available Formats
Resuscitation 85 (2014) 332335
Contents lists available at ScienceDirect
Resuscitation
journal homepage: www.elsevier.com/locate/resuscitation
Clinical Paper
Predicting the lack of ROSC during pre-hospital CPR: Should an
end-tidal CO2 of 1.3 kPa be used as a cut-off value?,
Leif Rogns a,b,c,d, , Troels Martin Hansen c,d , Hans Kirkegaard e , Else Tnnesen f
a
Department of Research and Development, Norwegian Air Ambulance Foundation, P.O. Box 94, 1441 Drbak, Norway
Pre-hospital Critical Care Team, Department of Anaesthesiology, Viborg Regional Hospital, Heibergs All 4, 8800 Viborg, Denmark
Pre-hospital Critical Care Team, Aarhus University Hospital, Oluf Palmes All 32, 8200 Aarhus N, Denmark
d
Department of Pre-hospital Medical Services, Central Denmark Region, Oluf Palmes All 34, 8200 Aarhus N, Denmark
e
Centre for Emergency Medicine Research, Aarhus University Hospital, Trjborgvej 72-74, Building 30, 8200 Aarhus N, Denmark
f
Department of Anaesthesiology, Aarhus University Hospital, Nrrebrogade 44, 8000 Aarhus, Denmark
b
c
a r t i c l e
i n f o
Article history:
Received 19 September 2013
Received in revised form
24 November 2013
Accepted 7 December 2013
Keywords:
Cardiac arrest
End-tidal CO2
Pre-hospital critical care
Emergency medical system
Helicopter emergency medical system
Critical decision making
a b s t r a c t
Aim: The aim of this study was to investigate if an initial ETCO2 value at or below 1.3 kPa can be used
as a cut-off value for whether return of spontaneous circulation during pre-hospital cardio-pulmonary
resuscitation is achievable or not.
Materials and methods: We prospectively registered data according to the Utstein-style template for
reporting data from pre-hospital advanced airway management from February 1st 2011 to October 31st
2012. Included were consecutive patients at all ages with pre-hospital cardiac arrest treated by eight
anaesthesiologist-staffed pre-hospital critical care teams in the Central Denmark Region.
Results: We registered data from 595 cardiac arrest patients; in 60.2% (n = 358) of these cases the prehospital critical care teams performed pre-hospital advanced airway management beyond bag-mask
ventilation. An initial end-tidal CO2 measurement following pre-hospital advanced airway management
were available in 75.7% (n = 271) of these 358 cases. We identied 22 patients, who had an initial end-tidal
CO2 at or below 1.3 kPa. Four of these patients achieved return of spontaneous circulation.
Conclusion: Our results indicates that an initial end-tidal CO2 at or below 1.3 kPa during pre-hospital CPR
should not be used as a cut-off value for the achievability of return of spontaneous circulation.
2013 The Authors. Published by Elsevier Ireland Ltd. All rights reserved.
1. Introduction
The European Resuscitation Council Guidelines for Resuscitations recommends the use of waveform capnography for
conrmation of tracheal tube placement whenever endotracheal
intubation (ETI) is performed during cardio-pulmonary resuscitation (CPR).1
Several authors,28 most recently Heradstveit et al.9 and
Qvigstad et al.,10 have suggested that measuring end-tidal carbon dioxide (ETCO2 ) may also be useful for optimising CPR quality
A Spanish translated version of the abstract of this article appears as Appendix
in the nal online version at http://dx.doi.org/10.1016/j.resuscitation.2013.12.009.
This is an open-access article distributed under the terms of the Creative
Commons Attribution-NonCommercial-No Derivative Works License, which permits non-commercial use, distribution, and reproduction in any medium, provided
the original author and source are credited.
Corresponding author at: Pre-hospital Critical Care Team, Aarhus University
Hospital, Oluf Palmes All 32, 8200 Aarhus N, Denmark.
E-mail addresses: leifrogn@rm.dk (L. Rogns), troehans@rm.dk (T.M. Hansen),
hanskirk@rm.dk (H. Kirkegaard), else.toennesen@aarhus.rm.dk (E. Tnnesen).
and as an aid for prognostication during CPR. Kolar et al. from the
emergency medical system (EMS) in Maribor, Slovenia found that
among 1086 non-traumatic adult cardiac arrest patients (collected
during a period of eight years) none of the patients in their study
with an initial ETCO2 below 1.33 kPa achieved ROSC.11 The authors
suggest using an ETCO2 of 1.33 kPa as a cut-off value for whether
return of spontaneous circulation (ROSC) following pre-hospital
cardiac arrest (CA) is achievable. We are not aware of any successful
validation of these ndings and the knowledge of the prognostic
signicance of ETCO2 measurements during pre-hospital CPR
remains limited.
1.1. Objectives
The objective of the study was to investigate if an initial ETCO2
value at or below 1.3 kPa can be used as a cut-off value for whether
ROSC during pre-hospital CPR is achievable or not.
We hypothesised that in patients with pre-hospital CA,
treated according to European Resuscitation Council Guidelines for
Resuscitation,1 an initial ETCO2 at or below 1.3 kPa is a predictor
for lack of ROSC and pre-hospital death.
0300-9572/$ see front matter 2013 The Authors. Published by Elsevier Ireland Ltd. All rights reserved.
http://dx.doi.org/10.1016/j.resuscitation.2013.12.009
L. Rogns et al. / Resuscitation 85 (2014) 332335
2. Methods
2.1. Study design
The data analysed in the present study is part of an observational study12,13 where we prospectively collected data related to
pre-hospital advanced airway management (PHAAM) in accordance with the consensus-based template made by Sollid et al.14
2.2. Setting
We investigated the anaesthesiologist-staffed pre-hospital critical care teams in the Central Denmark Region. This region covers
a mixed urban and rural area of approximately 13,000 km2 with a
population of 1,270,000, and an overall population density is 97.7
inhabitants per km2 .
The standard EU emergency telephone number (1-1-2) covers
all Denmark and there is an Emergency Medical Dispatch Centre
in each of the ve Danish regions. Emergency Medical Dispatch is
criteria based and telephone guided CPR is provided.15
The Emergency Medical Service (EMS) in the region is a twotiered system based on 64 road ambulances staffed by emergency
medical technicians (EMTs) supported by ten pre-hospital critical care teams staffed with an anaesthesiologist (with at least
4 years experience in anaesthesia) and a specially trained EMT.
Rapid response vehicles deploy nine of the pre-hospital critical
care teams; the tenth team staffs a Helicopter Emergency Medical
Service (HEMS) helicopter.
The pre-hospital critical care teams covered by this study
employ approximately 90 anaesthesiologists as part time prehospital physicians. All pre-hospital critical care anaesthesiologists
in the region primarily work in one of the ve regional emergency
hospitals or at the university hospital and they all have in-hospital
emergency anaesthesia and advanced airway management both
in- and outside the operating theatre as part of their daily work.
Intensive care is part of the Danish anaesthesiological curriculum.
EMTs and the pre-hospital critical care teams are expected
to follow the European Resuscitation Council Guidelines for
Resuscitation.1 The LUCAS automated chest compression device
is available on all the anaesthesiologist-staffed rapid response vehicles as well as on the HEMS. We have described the EMS system in
our region in more detail elsewhere.12,13,16
We collected data between February 1st 2011 and November
1st 2012.
2.3. Participants
2.3.1. Inclusion criteria
Consecutive pre-hospital cardiac arrest patients of all ages
where the pre-hospital critical care anaesthesiologist performed
PHAAM beyond bag-mask ventilation (BMV).
2.4. Endpoints and variables
Primary endpoints were: (1) initial ETCO2 after PHAAM during
CPR and (2) return of spontaneous circulation.
Secondary endpoints were: (1) Pre-hospital mortality.
We dened initial ETCO2 as the rst ETCO2 obtained after
PHAAM and return of spontaneous circulation as any period (no
time limit) of spontaneous circulation following PHAAM.
We collected all core data proposed in the consensus-based
template by Sollid et al. and we dened the variables as in this
template.14
The indications for performing PHAAM are categorised by Sollid
et al.14 We included patients where the pre-hospital critical care
physician had marked cardiac arrest as the reason for performing
PHAAM.
333
The pre-hospital critical care teams or the EMTs on the road
ambulances measured oxygen saturation, heart rate and blood
pressure by using a LifePak 12 monitor (Physio-Control, Redmond,
USA). The pre-hospital critical care teams monitored ETCO2 either
via the LifePak 12 or via a Nellcor NPB-75 capnograph (Tyco Healthcare Group LP, Pleasanton, USA). None of these devices can display
the ETCO2 as 1.33 kPa; it is either 1.3 or 1.4. Therefore, we chose at
or below 1.3 kPa as the cut-off value in this study.
The physicians registered the initial ETCO2 as a free-text variable. During data analysis, we labelled the initial ETCO2 as being
either under 1.3 kPa, at 1.3 kPa or above 1.3 kPa.
2.5. Data sources and data collection
We collected data from eight of the ten pre-hospital critical
care teams, including the HEMS. Due to substantial differences in
stafng, caseload, case mix and routines during the study period,
only eight of the ten pre-hospital critical care teams provided data
for the study.
The anaesthesiologists lled in a registration form (provided as
a Supplemental File) containing all the core data recommended by
Solid et al.14 If the patient died on-scene, we reviewed the written pre-hospital charts as well as the entry made in the electronic
patient journal for any evidence of temporary ROSC. For patients
transported during ongoing CPR, we evaluated the same sources
for evidence of temporary ROSC. If there were any doubt, whether
the patient achieved ROSC or not we included the patient in the no
ROSC group during data analysis.
2.6. Bias
To reduce the risk of recall bias and selection bias, the primary
investigator reviewed the registration forms on a day-to-day
basis. We crosschecked the registration forms with the standard
pre-hospital records from the pre-hospital critical care teams to
ensure the highest possible data coverage. In cases of missing data
or inconsistencies, we asked the attending pre-hospital critical
care physician to provide additional details for clarication.
2.7. Study size and statistical methods
In-depth discussions with an expert statistician at Aarhus University resulted in the following:
In theory, it would only take one single patient with a true initial
ETCO2 at or below 1.3 kPa and subsequent ROSC for us to have to
reject the hypothesis. However, this one case could be due to for
instance equipment malfunction and we therefore decided that we
would reject the hypothesis if two or more patients with an initial
ETCO2 at or below 1.3 kPa achieved ROSC.
Sample size calculations made by the statistician in the statistical software Stata 12 (StataCorpLP) showed that to be able to
conrm the hypothesis with a power of at least 80% and a level
of signicance of 95% we would need to include 100 patients with
an ETCO2 of less than 1.3 and no ROSC. In cases of unobtainable
missing data, we performed complete case analyses.
2.8. Ethics
No patients had their treatment altered because of the study.
All physicians participated in the study on a voluntary basis
there were no refusals.
The study did not involve any alterations from normal practice
and according to Danish law, it did not need the approval of the
Regional Ethics Committee, nor did we need the patients consent
to register and publish the data. The Danish Data Protection Agency
approved the study (Journal number 2013-41-1462).
334
L. Rogns et al. / Resuscitation 85 (2014) 332335
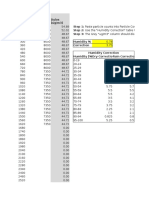
Table 1
Demographic data.
Total patients included (N)
Age (years) mean
Age < 16 years
Age < 2 years
Males
ASA-PSa -score mean
Pre-existing cardiac disease
Pre-existing hypertension
Pre-existing COPDb
Pre-existing diabetes
Pre-existing neurological disease
Other pre-existing disease
Traumatic cardiac arrest
Non-traumatic cardiac arrest
a
b
Numbers
358
63.1
11
6
232
2.32
96
29
40
18
23
99
32
326
097 (range)
3.1
1.7
64.8
14 (range)
26.8
8.1
11.2
5.0
6.4
27.7
8.9
91.1
American Society of Anesthesiologists Physical Performance.
Chronic obstructive pulmonary disease.
In a study of 575 Norwegian pre-hospital cardiac arrest patients
treated by physician-staffed HEMS, Heradstveit et al., 9 found many
confounding factors complicating the interpretation of ETCO2
monitoring during CPR. The authors could not identify a clear generalised cut-off value determining whether ROSC would be achieved
or not. Our results seem to support this view.
In our opinion, ETCO2 monitoring during CPR provides important information but the results of the current study does not allow
us to support the use of an initial ETCO2 at or below 1.3 as a cutoff value for the achievement of ROSC in pre-hospital CA patients.
Basing the decision of whether or not to terminate CPR on this cutoff value may diminish patients safety and impair patient outcome
following pre-hospital CA.
We advocate the use of ETCO2 measurements as one parameter
among others (such as the result of focused ultrasound assessment)
to guide the critical decision-making during pre-hospital CPR.
4.2. Limitations
3. Results
3.1. Participants
During the 21 months, the participating pre-hospital critical
care teams treated 24 693 patients. The teams registered data from
1081 PHAAM cases corresponding to 93.3% of PHAAM patients.
Patients in CA accounted for 55.0% (n = 595) of these cases. The prehospital critical care physicians performed PHAAM beyond BMV on
60.2% (n = 358) of the 595 patients in CA; the rest were treated with
bag-mask ventilation and in these cases ETCO2 were not routinely
measured. In 97.8% (n = 350) of the 358 cases the anaesthesiologists performed PHETI, in 2.0% (n = 7) they inserted an SAD and in
one case a surgical airway (SAW) were needed. These 358 PHAAM
patients were included in the current study.
3.2. Descriptive data
Table 1 displays demographic data of the 358 CA patients treated
with PHETI/SAD/SAW.
3.3. Main results
An initial ETCO2 was available in 271 of the CA cases.
Among these 271 cases, we identied 22 patients, who had an
initial ETCO2 after PHAAM below 1.3 kPa; additional seven patients
had an initial ETCO2 = 1.3 kPa.
Three patients with an initial ETCO2 below 1.3 kPa and one
patient with an initial ETCO2 of 1.3 kPa achieved ROSC. We describe
these four patients in detail in Table 2.
4. Discussion
4.1. Main results
Based on an retrospective analysis of over 700 pre-hospital cardiac arrest patients Kolar et al. suggests an initial ETCO2 of less than
1.33 kPa as a cut-off value to identify patients who will not achieve
ROSC.11 Our results cannot conrm their ndings. We identied
four CA patients with an initial ETCO2 at or below 1.3 kPa who all
achieved ROSC, and our hypothesis that an initial ETCO2 at or below
1.3 kPa during pre-hospital CPR can be used as a predictor of prehospital death, must therefore be rejected. It is unlikely that all four
cardiac arrest cases who achieved ROSC following an initial ETCO2
of 1.3 kPa or less should have experienced a falsely low ETCO2 value.
The results published by Callaham et al. support our ndings.17
They investigated 55 patients in CA and found that four of those
with an initial ETCO2 below 1.3 kPa achieved ROSC.
The study was designed according to the Utstein-style template
for reporting data from pre-hospital advanced airway management
by Sollid et al.,14 and not according to the template for reporting data from pre-hospital cardiac arrest.18 Consequently, readers
should interpret the non-airway management related results in the
current study with caution.
We measured the ETCO2 values on one of the two portable
capnographs and we did not routinely check the readings by measurement of ETCO2 on both capnographs or by measuring the
partial pressure of CO2 in arterial blood. Never the less, our way
of measuring ETCO2 depicts daily clinical practice.
The 23% lacking measurements of ETCO2 is a potential source
of bias. We do not know the reason for these missing data. It
could be because of equipment malfunction or unavailable equipment due to maintenance. It could also be because the attending
anaesthesiologist chose not to use capnography, which is not in
adherence with current guidelines.1 However, the missing data
does not change the fact that four patients with an initial ETCO2 at
or below 1.3 kPa achieved ROSC and it does therefore not inuence
our conclusion. In a more general perspective, our ndings indicate
a need for an increased use of ETCO2 - measurements during CPR in
our service.
We did not design this study to investigate the different factors
inuencing ETCO2 during CPR and our results are merely an attempt
to investigate the use of an initial ETCO2 at or below 1.3 kPa as a cutoff value in the critical decision making process during pre-hospital
CPR in a non-selected population of pre-hospital CA patients.
Survival beyond survival to admission was outside the scope of
this study. This is in coherence with the paper by Kolar et al.11
The attending anaesthesiologists registered all the data. They
are therefore potentially subject to registration bias (systematic
errors in the registration of data) or recall bias. The high capture
rate reduces the risk of selection bias. Based on the day-to-day
crosscheck of the registration forms against both the written
pre-hospital journals and the compulsory entries made by the
anaesthesiologists in the patients hospital records, the extent of
selection bias is probably limited.
4.3. Generalisability
This was a study from one homogenous Danish system of
anaesthesiologist-staffed pre-hospital critical care teams. This limits the ability to generalise the ndings to other systems with
different stafng, caseload or case mix. Never the less, treatment
were according to current guidelines and we believe that our results
can be of use to other physician-staffed as well as paramedic-staffed
pre-hospital services performing pre-hospital advanced airway
L. Rogns et al. / Resuscitation 85 (2014) 332335
335
Table 2
Patients with return of spontaneous circulation after an initial ETCO2 1.3 during CPR.a
Sex
Age (years)
ASA-PSb score
Pre-existing disease
Type of cardiac arrest
First ECG
First ETCO2 (kPa)
ETCO2 (kPa) in the EDc
Spontaneous circulation
in the ED
Fd
F
Mg
M
74
84
79
72
2
2
3
2
None
Other
Cardiac + other
Cardiac
Medical
Medical
Medical
Medical
Sinus rhythme
PEAf
Unknown
VF
1.1
0.8
1.3
1.2
1.3
3.3
8.0
2.5
Yes
Yes
Yes
Noh
a
b
c
d
e
f
g
h
Cardio-pulmonary resuscitation.
American Society of Anesthesiologists Physical Performance.
Emergency department.
Female.
Ventricular brillation occurred after arrival of the Emergency Medical Services.
Pulseless electrical activity/non-shock able rhythm.
Male.
Short pre-hospital period of ROSC, transported during ongoing CPR with LUCAS automated chest compression device.
management with ETCO2 monitoring during pre-hospital cardiac
arrest.
4.4. Perspectives
Further research is needed to conrm or reject the existence of a
universal cut-of value of ETCO2 for the achievement of ROSC during
pre-hospital CPR. Based on our results, we nd it doubtful whether
such a value does exist.
5. Conclusion
In this study of 271 pre-hospital cardiac arrest patients treated
with pre-hospital advanced airway management other than bagmask ventilation by pre-hospital critical care anaesthesiologists,
we identied four patients with an initial ETCO2 at or below 1.3 kPa
who achieved return of spontaneous circulation. Our results cannot conrm the hypothesis that an initial ETCO2 at or below 1.3 kPa
found during pre-hospital CPR is a predictor for the lack of return
of spontaneous circulation. We advise against using our results to
discard the use of ETCO2 measurements as one important parameter among several in the critical decision making process during
pre-hospital CPR.
Conict of interest statement
The authors declare that they have no conict of interests.
Acknowledgements
The Norwegian Air Ambulance Foundation, The Laerdal Foundation for Acute Medicine and The Central Denmark Region, founded
the study by sponsoring the salary of LR.
TMH, HK and ET were funded by their departments.
The sponsors have had no inuence on study design, data collection, data analysis and interpretation, the writing of the manuscript
or the decision to submit the paper for publication.
The authors wish to thank all the pre-hospital critical care physicians who collected the data and all the EMTs who reminded them
to do so.
A special thanks to EMT Tinna Hjmose stergaard for her
invaluable assistance in all the practicalities of the data collection.
Appendix A. Supplementary data
Supplementary data associated with this article can be found,
in the online version, at http://dx.doi.org/10.1016/j.resuscitation.
2013.12.009.
References
1. Nolan JP, Soar J, Zideman DA, et al. European Resuscitation Council Guidelines for Resuscitation 2010. Section 1. Executive summary. Resuscitation
2010;81:121976.
2. Ahrens T, Schallom L, Bettorf K, et al. End-tidal carbon dioxide measurements
as a prognostic indicator of outcome in cardiac arrest. Am J Crit Care 2001;10:
3918.
3. Dubin A, Murias G, Estenssoro E, et al. End-tidal CO2 pressure determinants during hemorrhagic shock. Intensive Care Med 2000;26:
161923.
4. Grmec S, Krizmaric M, Mally S, Kozelj A, Spindler M, Lesnik B. Utstein style
analysis of out-of-hospital cardiac arrestbystander CPR and end expired carbon
dioxide. Resuscitation 2007;72:40414.
5. Morimoto Y, Kemmotsu O, Morimoto Y, Gando S. End-tidal carbon dioxide and
resuscitation. Curr Opin Anaesthesiol 1999;12:1737.
6. Salen P, OConnor R, Sierzenski P, et al. Can cardiac sonography and capnography
be used independently and in combination to predict resuscitation outcomes?
Acad Emerg Med 2001;8:6105.
7. Sanders AB, Ewy GA, Bragg S, Atlas M, Kern KB. Expired PCO2 as a prognostic indicator of successful resuscitation from cardiac arrest. Ann Emerg Med
1985;14:94852.
8. Sanders AB, Kern KB, Otto CW, Milander MM, Ewy GA. End-tidal carbon dioxide
monitoring during cardiopulmonary resuscitation. A prognostic indicator for
survival. J Am Med Assoc 1989;262:134751.
9. Heradstveit BE, Sunde K, Sunde GA, Wentzel-Larsen T, Heltne JK. Factors
complicating interpretation of capnography during advanced life support in
cardiac arrest a clinical retrospective study in 575 patients. Resuscitation
2012;83:8138.
10. Qvigstad E, Kramer-Johansen J, Tomte O, et al. Clinical pilot study of different
hand positions during manual chest compressions monitored with capnography. Resuscitation 2013;84:12037.
11. Kolar M, Krizmaric M, Klemen P, Grmec S. Partial pressure of end-tidal carbon dioxide successful predicts cardiopulmonary resuscitation in the eld: a
prospective observational study. Crit Care 2008;12:R115.
12. Rognas L, Hansen TM, Kirkegaard H, Tonnesen E. Pre-hospital advanced airway management by experienced anaesthesiologists: a prospective descriptive
study. Scand J Trauma Resusc Emerg Med 2013;21:58.
13. Rognas L, Hansen TM, Kirkegaard H, Tonnesen E. Refraining from pre-hospital
advanced airway management: a prospective observational study of critical decision making in an anaesthesiologist-staffed pre-hospital critical care
service. Scand J Trauma Resusc Emerg Med 2013;21:75.
14. Sollid SJ, Lockey D, Lossius HM. A consensus-based template for uniform reporting of data from pre-hospital advanced airway management. Scand J Trauma
Resusc Emerg Med 2009;17:58.
15. Andersen MS, Johnsen SP, Sorensen JN, Jepsen SB, Hansen JB, Christensen EF.
Implementing a nationwide criteria-based emergency medical dispatch system: a register-based follow-up study. Scand J Trauma Resusc Emerg Med
2013;21:53.
16. Rognas LK, Hansen TM. EMS-physicians self reported airway management training and expertise; a descriptive study from the Central Region of Denmark. Scand
J Trauma Resusc Emerg Med 2011;19:10.
17. Callaham M, Barton C. Prediction of outcome of cardiopulmonary resuscitation from end-tidal carbon dioxide concentration. Crit Care Med 1990;18:
35862.
18. Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplication of the Utstein templates
for resuscitation registries, A statement for healthcare professionals from a task
force of the international liaison committee on resuscitation (American Heart
Association, European Resuscitation Council, Australian Resuscitation Council,
New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada,
InterAmerican Heart Foundation, Resuscitation Council of Southern Africa).
Resuscitation 2004;63:23349.
You might also like
- Mauser 98K - Model 48 Rifle ManualDocument20 pagesMauser 98K - Model 48 Rifle ManualMeor Amri96% (28)
- Science-9 q1 w1 Mod1 Adm-1Document62 pagesScience-9 q1 w1 Mod1 Adm-1Carla GabrielNo ratings yet
- Sailor Mini MoonDocument9 pagesSailor Mini MoonCarytoNo ratings yet
- CPR GuidelinesDocument30 pagesCPR GuidelineswvhvetNo ratings yet
- Api 576 Study QuestionsDocument9 pagesApi 576 Study Questionseragorn100% (1)
- Case 3 Analysis AdtrackmediaDocument2 pagesCase 3 Analysis Adtrackmediaapi-526105414No ratings yet
- Early Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac ArrestDocument9 pagesEarly Cardiopulmonary Resuscitation in Out-of-Hospital Cardiac ArrestHammad AjaNo ratings yet
- Blue ProtocolDocument11 pagesBlue Protocoloana florianaNo ratings yet
- 20 SundeDocument6 pages20 Sundejangkrik21No ratings yet
- Aew 1 AkaDocument8 pagesAew 1 AkaBobby AksandaNo ratings yet
- Aew 190Document8 pagesAew 190Nurul Dwi LestariNo ratings yet
- Preoperative Cerebral Oxygen Saturation and Clinical Outcomes in Cardiac SurgeryDocument12 pagesPreoperative Cerebral Oxygen Saturation and Clinical Outcomes in Cardiac SurgeryThotaNo ratings yet
- 10 1016@j Resuscitation 2019 12 042Document9 pages10 1016@j Resuscitation 2019 12 042Fia Bella KusumaNo ratings yet
- Point-Of-Care Ultrasonography in Patients Admitted With Respiratory Symptoms: A Single-Blind, Randomised Controlled TrialDocument9 pagesPoint-Of-Care Ultrasonography in Patients Admitted With Respiratory Symptoms: A Single-Blind, Randomised Controlled TrialPacoNo ratings yet
- Cost of Extracorporeal Membrane Oxygenation: Evidence From The Rikshospitalet University Hospital, Oslo, NorwayDocument4 pagesCost of Extracorporeal Membrane Oxygenation: Evidence From The Rikshospitalet University Hospital, Oslo, NorwayArief LiemNo ratings yet
- ICU Registered Nurses 2Document8 pagesICU Registered Nurses 211 - JEMELYN LOTERTENo ratings yet
- Laryngeal Mask Airway As An AlternativeDocument18 pagesLaryngeal Mask Airway As An Alternativeadink mochammadNo ratings yet
- s13049 019 0599 1 PDFDocument9 pagess13049 019 0599 1 PDFDeby WicaksonoNo ratings yet
- Outcomes of COPDDocument6 pagesOutcomes of COPDRISKINo ratings yet
- Low Body Mass Index, Airflow Obstruction, and Dyspnoea in A Primary Care COPD Patient PopulationDocument6 pagesLow Body Mass Index, Airflow Obstruction, and Dyspnoea in A Primary Care COPD Patient PopulationArizal AbdullahNo ratings yet
- Jurnal BLSDocument7 pagesJurnal BLSNirmalaRamliNo ratings yet
- Performance in The Shuttle Walk Test Is Associated With Cardiopulmonary Complications After Lung ResectionsDocument10 pagesPerformance in The Shuttle Walk Test Is Associated With Cardiopulmonary Complications After Lung ResectionsAnonymous Skzf3D2HNo ratings yet
- IcuDocument56 pagesIcurulli_pranandaNo ratings yet
- Entropy 17 02932 Detecting ApneaDocument26 pagesEntropy 17 02932 Detecting ApneadonsuniNo ratings yet
- Valtier Et Al 1998Document7 pagesValtier Et Al 1998GilbertLiemNo ratings yet
- High-Frequency Oscillation For Acute Respiratory Distress SyndromeDocument8 pagesHigh-Frequency Oscillation For Acute Respiratory Distress SyndromeLintang SuroyaNo ratings yet
- Prat 2016Document21 pagesPrat 2016Johann Fernando Orozco CastroNo ratings yet
- Metas de Oxigeno 2021Document11 pagesMetas de Oxigeno 2021Javier López CastellanosNo ratings yet
- Randomised Controlled Trial of Continuous Positive Airway Pressure and Standard Oxygen Therapy in Acute Pulmonary OedemaDocument8 pagesRandomised Controlled Trial of Continuous Positive Airway Pressure and Standard Oxygen Therapy in Acute Pulmonary OedemaAlex PiecesNo ratings yet
- Journal of Thoracic Oncology Volume Issue 2016Document30 pagesJournal of Thoracic Oncology Volume Issue 2016Daniela RoaNo ratings yet
- BURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsDocument8 pagesBURG 2014 - Cross-Sectional Changes in Lung Volume Measured by Electrical Impedance Tomography Are Representative For The Whole Lung in Ventilated Preterm InfantsRafael JustinoNo ratings yet
- Transthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Document9 pagesTransthoracic Echocardiography For Cardiopulmonary Monitoring in Intensive Care (FATE)Anish H DaveNo ratings yet
- 1 s2.0 S030095721200113X Main PDFDocument6 pages1 s2.0 S030095721200113X Main PDFRoger AvilaNo ratings yet
- Effect of ELTGOl On Mucus Clerance in Stable Patients With Chronic Bronchitis - Dormelas 11Document20 pagesEffect of ELTGOl On Mucus Clerance in Stable Patients With Chronic Bronchitis - Dormelas 11Daniel González DíazNo ratings yet
- Critical Journal Nejmoa1405796Document9 pagesCritical Journal Nejmoa1405796Aryanti'aya'MemotNo ratings yet
- JR 2 CopdDocument6 pagesJR 2 CopdDoc AwaNo ratings yet
- RCCM 202212-2300ocDocument14 pagesRCCM 202212-2300ocLucas PereiraNo ratings yet
- Preliminary Report: Dyspnea Differentiation IndexDocument5 pagesPreliminary Report: Dyspnea Differentiation IndexXenilitiurahmi RimadeiraniNo ratings yet
- Automatic Measurements of Mitral Annular Plane Systolic Excursion and Velocities To Detect Left Ventricular DysfunctionDocument9 pagesAutomatic Measurements of Mitral Annular Plane Systolic Excursion and Velocities To Detect Left Ventricular DysfunctionMiguelNo ratings yet
- Bmri2016 3068467Document5 pagesBmri2016 3068467atika sgrtNo ratings yet
- ProbableDocument6 pagesProbableDany GomezNo ratings yet
- Bertsch 2010Document14 pagesBertsch 2010Daniel ChaNo ratings yet
- 10 1111@anae 12955Document10 pages10 1111@anae 12955Cuenta LastNo ratings yet
- Assessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCADocument4 pagesAssessment of Suitability For Lung Resection: Gerard Gould FRCA Adrian Pearce FRCAsayednourNo ratings yet
- Chan 2014Document7 pagesChan 2014denanurbaniazharNo ratings yet
- Savary 2021Document6 pagesSavary 2021Karla HernandezNo ratings yet
- Vignon Echo Fluid ResponsivenessDocument46 pagesVignon Echo Fluid ResponsivenesscsquizzardNo ratings yet
- Definition, Discrimination, Diagnosis and Treatment of Central Breathing Disturbances During SleepDocument28 pagesDefinition, Discrimination, Diagnosis and Treatment of Central Breathing Disturbances During SleepgruukgruukNo ratings yet
- Idris Circulation ArticleDocument11 pagesIdris Circulation Articlejmartin4800No ratings yet
- DocumentDocument7 pagesDocumentLestiNo ratings yet
- Aneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10Document7 pagesAneurysm Brain and Hyperbaric Chamber AIT - Art - 37989-10cooleraid884No ratings yet
- ICMEffeiciencyofgastransferin ECMODocument9 pagesICMEffeiciencyofgastransferin ECMOAlmudena DelgadoNo ratings yet
- Chest Physiotherapy After Coronary Artery Bypass Graft Surgery-A Comparison of Three Different Deep Breathing TechniquesDocument6 pagesChest Physiotherapy After Coronary Artery Bypass Graft Surgery-A Comparison of Three Different Deep Breathing TechniquesmadeNo ratings yet
- Jurnal ARDSDocument8 pagesJurnal ARDSrifki yulinandaNo ratings yet
- Oxygen Therapy in Suspected Acute Myocardial InfarctionDocument10 pagesOxygen Therapy in Suspected Acute Myocardial InfarctionPutri YunandaNo ratings yet
- Watanabe 2018Document6 pagesWatanabe 2018Utami AsriNo ratings yet
- Nonsedation or Light Sedation in Critically IllDocument9 pagesNonsedation or Light Sedation in Critically IllPutra SetiawanNo ratings yet
- HospitalisasiDocument13 pagesHospitalisasiViviNo ratings yet
- End 2014 0019Document6 pagesEnd 2014 0019Manolin KinNo ratings yet
- Contin Educ Anaesth Crit Care Pain-2010-Agnew-33-7Document5 pagesContin Educ Anaesth Crit Care Pain-2010-Agnew-33-7deadbysunriseeNo ratings yet
- Yilmaz 2018Document18 pagesYilmaz 2018Hassler Barrios AcostaNo ratings yet
- We Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsDocument25 pagesWe Are Intechopen, The World'S Leading Publisher of Open Access Books Built by Scientists, For ScientistsSasmita DewiNo ratings yet
- Machine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsDocument9 pagesMachine Learning Algorithms Utilizing Functional Respiratory Imaging May Predict COPD ExacerbationsFaraz KhanNo ratings yet
- Essentials in Lung TransplantationFrom EverandEssentials in Lung TransplantationAllan R. GlanvilleNo ratings yet
- Implementing Sales 12Document566 pagesImplementing Sales 12Amer YehiaNo ratings yet
- 7 Revealing Depression Questions Answered: Health - Body - Life - SoulDocument4 pages7 Revealing Depression Questions Answered: Health - Body - Life - SoulGregorio PetteNo ratings yet
- Fillers Adaptations On Traditional and CDocument10 pagesFillers Adaptations On Traditional and CMaja SMNo ratings yet
- Asset-V1 MITx+6.86x+3T2020+typeasset+blockslides Lecture6 CompressedDocument22 pagesAsset-V1 MITx+6.86x+3T2020+typeasset+blockslides Lecture6 CompressedRahul VasanthNo ratings yet
- Slack Briefing NoteDocument2 pagesSlack Briefing NotePedro Inácio FumoNo ratings yet
- Assay Ob Borax PDFDocument14 pagesAssay Ob Borax PDFAbram Louies Hanna100% (1)
- Aging With HIV A Gay Mans GuideDocument244 pagesAging With HIV A Gay Mans Guidewolf manNo ratings yet
- Nickel SulfateDocument127 pagesNickel SulfateMayerly Giraldo AvilaNo ratings yet
- DZ 200 CdiDocument2 pagesDZ 200 CdipowerveeNo ratings yet
- Active Learning Guide 1St Edition Heuvelen Solutions Manual Full Chapter PDFDocument36 pagesActive Learning Guide 1St Edition Heuvelen Solutions Manual Full Chapter PDFtamara.hendrick989100% (17)
- 0580 Y12 Ecr P2 v2Document45 pages0580 Y12 Ecr P2 v2Kay SinghNo ratings yet
- Some Observable Classroom BehaviorDocument33 pagesSome Observable Classroom BehaviorMaNerissa Peñamora SanchezNo ratings yet
- 1 s2.0 S0278612521000601 MainDocument16 pages1 s2.0 S0278612521000601 MainPrarthanaNo ratings yet
- E646Document12 pagesE646Hillary McgowanNo ratings yet
- Dylos Conversion Education - Cehs.health - Umt.eduDocument117 pagesDylos Conversion Education - Cehs.health - Umt.eduMCNo ratings yet
- LUNG CaDocument59 pagesLUNG CaokaciaNo ratings yet
- 7SG117 Argus 7 Catalogue SheetDocument8 pages7SG117 Argus 7 Catalogue SheetHimdad TahirNo ratings yet
- Interview 4Document2 pagesInterview 4Naveen BhaiNo ratings yet
- Essays On GlobalisationDocument7 pagesEssays On Globalisationd3gxt9qh100% (2)
- Iex Dam Tam Web 2017Document65 pagesIex Dam Tam Web 2017Girish MehraNo ratings yet
- 3-2-NDT-SOIS-21 AirWinch ENF#40 MW-004314Document1 page3-2-NDT-SOIS-21 AirWinch ENF#40 MW-004314Abdou BoucheritNo ratings yet
- Economics of Animal-Rearing: Dairy and Livestock ProductionDocument6 pagesEconomics of Animal-Rearing: Dairy and Livestock ProductionRaghav BawaNo ratings yet
- 3483-Article Text-8498-2-10-20201015Document15 pages3483-Article Text-8498-2-10-20201015Nawzi kagimboNo ratings yet
- lfh101 Temperature and Humidity Transmitter 485 ProtocolDocument3 pageslfh101 Temperature and Humidity Transmitter 485 ProtocolZaki ElsayedNo ratings yet
- Mead's Theory of The SelfDocument1 pageMead's Theory of The Selfsumayya tariqNo ratings yet