Professional Documents
Culture Documents
Complications of Peripheral IV Therapy
Uploaded by
majOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Complications of Peripheral IV Therapy
Uploaded by
majCopyright:
Available Formats
i.v.
essentials
Complications of
peripheral I.V. therapy
IF YOUR PATIENT is receiving peripheral ■ Stay with your patient for 5 to 10 min-
I.V. therapy, you’ll need to watch for signs utes to detect early signs and symptoms of
and symptoms of complications, such as: hypersensitivity, such as sudden fever, joint
■ hypersensitivity swelling, rash, urticaria (hives), broncho-
Sometimes, I
■ infiltration spasm, and wheezing.
can get a bit
■ extravasation ■ If he’s receiving the drug for the first or
complicated... ■ phlebitis second time, check him every 5 to 10 min-
■ infection. utes or according to your facility’s policy.
We’ll fill you in on how to recognize these An immediate, severe reaction is life-
complications and walk you through how to threatening, so prompt recognition and
treat them, with an eye on prevention. treatment are imperative.
At the first sign of hypersensitivity:
You’re so sensitive ■ Discontinue the infusion and notify the
Before you adminis-
ter an I.V. medica-
tion, take steps to
Running down the infiltration scale
Use these classifications when documenting instances of infiltration.
find out if your pa-
tient may be prone Degree Description
to hypersensitivity: 0 • No symptoms
■ Ask him if he has 1+ • Skin blanched
any allergies, in- • Edema less than 1 inch (2.5 cm) in any direction
cluding allergies to • Cool to touch
food or pollen. • With or without pain
■ Ask if he has a 2+ • Skin blanched
family history of al- • Edema 1 to 6 inches (2.5 to 15 cm) in any direction
lergies; if he does, • Cool to touch
• With or without pain
he’s more likely to
3+ • Skin blanched, translucent
develop a drug hy-
• Gross edema more than 6 inches in any direction
persensitivity. • Cool to touch
■ If your patient is • Mild to moderate pain
an infant less than • Possible numbness
age 3 months, ask 4+ • Skin blanched, translucent, tight, leaking, discolored, bruised,
the mother about swollen
her allergy history • Gross edema more than 6 inches in any direction
because maternal • Deep, pitted tissue edema
antibodies may still • Circulatory impairment
be present. • Moderate to severe pain
• Infiltration of any blood product, irritant, or vesicant
After giving an
I.V. medication, fol-
Source: Infusion Nurses Society, Infusion Nursing Standards of Practice, Journal of Infusion
low through with Nursing, January/February 2006.
these precautions:
14 Nursing made Incredibly Easy! January/February 2008
health care provider immediately. ing vesicants:
■ Administer medications as ordered. memory ■ Strictly adhere to
■ Monitor the patient’s vital signs and pro- jogger proper administra-
vide emotional support. As soon as you spot tion techniques.
Get to know
infiltration, think of ■ Avoid using the
Just say no to infiltration the three C’s: back of the hand
the signs and
Infiltration occurs when I.V. fluid leaks into Cut off (the infusion) where tendon and symptoms to
surrounding tissue. It’s commonly caused Counteract (the
nerve damage is watch out for.
effects of the drug)
by improper placement or dislodgment of more likely.
Contain (the affect-
the catheter. When the tip of the catheter is ■ Avoid using the
ed area).
positioned near a flexion area, patient wrist and fingers be-
movement may cause the catheter to slip cause they’re hard
out or through the lumen of the vessel. The to immobilize and
risk of infiltration increases in older patients areas with previous
because their veins are thin and fragile. damage or poor circulation.
Signs and symptoms of infiltration ■ Give vesicants last when multiple drugs
include: are ordered.
■ swelling Signs and symptoms of extravasation
■ discomfort include:
■ burning ■ blanching, burning, or discomfort at the
■ tightness I.V. site
■ cool skin ■ cool skin around the I.V. site
■ blanching. ■ swelling at or above the I.V. site.
If only a small amount of an isotonic solu- If you suspect extravasation, follow your
tion or nonirritating drug infiltrates, the facility’s protocol. Take these essential steps:
patient usually experiences only mild dis- ■ Stop the I.V. flow and remove the I.V.
comfort. Here’s what you need to do: line, unless the catheter should remain in
■ Stop the infusion and remove the device place to administer the antidote.
(unless the medication is a vesicant; consult ■ Estimate the amount of extravasated so-
the health care provider and pharmacy). lution and notify the health care provider.
■ Elevate the limb to increase patient com- ■ Instill the appropriate antidote according
fort. to your facility’s protocol.
■ Check the patient’s pulse and capillary ■ Elevate the extremity.
refill time. ■ Record the extravasation site, your pa-
■ Counteract the effects of the drug as or- tient’s symptoms, the estimated amount of
dered. extravasated solution, and the treatment.
■ Perform venipuncture in a different loca- Follow the manufacturer’s recommenda-
tion and restart the infusion. tions to apply either ice packs or warm com-
■ Check the site frequently. presses to the affected areas.
■ Document your findings using the infil-
tration scale (see Running down the infiltra- Fighting phlebitis
tion scale). Phlebitis, or inflammation of a vein, is a
common complication of peripheral I.V.
Extra! Extra! Extravasation therapy that’s associated with acidic or al-
suspected! kaline solutions or those that have a high
Extravasation, the leaking of vesicant drugs osmolarity. Other factors include:
(such as antineoplastics) into surrounding ■ vein trauma during insertion
tissue, can cause severe local tissue damage, ■ using a vein that’s too small
resulting in delayed healing, infection, tis- ■ using a vascular access device that’s too
sue necrosis, disfigurement, loss of function, large
and even amputation. ■ prolonged use of the same I.V. site.
To help prevent extravasation when giv- Phlebitis can follow any infusion, but it’s
January/February 2008 Nursing made Incredibly Easy! 15
i.v. essentials
most common after continuous infusions, Use a transparent
Together,
developing 2 to 3 days after the vein is memory semipermeable
we can keep exposed to the drug or solution. It develops jogger dressing so you can
I.V. therapy more rapidly in distal veins than in veins Here’s a handy tip: see the skin distal
complication close to the heart. Phenytoin and diazepam When administering to the tip of the
free! can produce phlebitis after one or more vesicants I.V., think catheter as well as
injections at the same I.V. site. Large doses hands off! Avoid the insertion site.
the back of the hand
of potassium chloride, amino acids, dextrose If you suspect
(where damage from
solutions, and multivitamins can cause phlebitis, follow
extravasation is
phlebitis as well. Certain irritating I.V. drugs these steps:
more likely) and the
are also likely to cause phlebitis when pig- wrist and fingers ■ At the first sign
gybacked, including: (which are hard to of redness or ten-
■ erythromycin immobilize). derness, stop the
■ tetracycline infusion.
■ nafcillin ■ To ease your
■ vancomycin patient’s discomfort, apply warm packs.
■ amphotericin B. ■ Document your patient’s condition and
Take these steps to prevent phlebitis: interventions.
■ Use proper venipuncture technique. ■ If indicated, insert a new catheter at a
■ If necessary, dilute drugs correctly. different site, preferably on the opposite
■ Monitor administration rates. arm, using a larger vein or a smaller device
■ Observe the I.V. site frequently. and restart the infusion.
■ Change the infusion site regularly ac-
cording to your facility’s policy. Infection detection
Signs and symptoms of phlebitis include: A patient receiving I.V. therapy may de-
■ redness or tenderness at the tip of the velop a local or systemic infection. Monitor
catheter your patient for signs and symptoms of in-
■ puffy area over the vein fection, such as redness and discharge at
■ elevated temperature. the I.V. site or an elevated temperature. If
To detect phlebitis, inspect the I.V. site the infection is systemic:
several times a day (see Classifying phlebitis). ■ Stop the infusion.
■ Notify the health care provider.
■ Remove the device.
Classifying phlebitis ■ Culture the site and device as ordered.
Use these classifications when documenting phlebitis. ■ Administer medications as prescribed.
■ Monitor the patient’s vital signs.
Degree Description
0 • No signs and symptoms
1+ • Erythema with or without pain
Let’s not get too complicated
Complications of peripheral I.V. therapy
2+ • Erythema with pain
• Edema may or may not be present.
can be serious, but with your careful atten-
3+ • Erythema with pain tion and eye on prevention, you can help
• Edema may or may not be present. your patient avoid these pitfalls. ■
• Streak formation
• Palpable cord Learn more about it
4+ • Erythema with pain Infusion Nurses Society. Infusion Nursing Standards of
• Edema may or may not be present. Practice. Journal of Infusion Nursing. 29(1, Suppl.):S1-S92,
January/February 2006.
• Streak formation
I.V. Therapy: An Incredibly Easy Pocket Guide. Philadelphia,
• Palpable cord longer than 1 inch (2.5 cm) Pa., Lippincott Williams & Wilkins, 2006:174-177.
• Purulent drainage I.V. Therapy Made Incredibly Easy!, 3rd edition. Philadel-
phia, Pa., Lippincott Williams & Wilkins, 2006:187-189.
Source: Infusion Nurses Society, Infusion Nursing Standards of Practice, Journal of Infusion Smeltzer SC, et al. Brunner and Suddarth’s Textbook of
Nursing, January/February 2006.
Medical-Surgical Nursing, 11th edition. Philadelphia, Pa.,
Lippincott Williams & Wilkins, 2007:350-351.
18 Nursing made Incredibly Easy! January/February 2008
You might also like
- STUDENT-Sickle - Cell-FUNDAMENTAL ReasoningDocument7 pagesSTUDENT-Sickle - Cell-FUNDAMENTAL ReasoningSharon Tanveer0% (1)
- NIH Stroke Scale BookletDocument11 pagesNIH Stroke Scale Bookletcleber333100% (2)
- Breath Sounds Incredibly EasyDocument4 pagesBreath Sounds Incredibly EasyMatthew Ryan100% (3)
- Assessement Cheat SheetDocument2 pagesAssessement Cheat SheetPatty Pasarilla Passehl100% (1)
- OB Meds WorksheetDocument18 pagesOB Meds WorksheetrickyandsheenaNo ratings yet
- Nursing Laboratory and Diagnostic Tests Demystified, Second EditionFrom EverandNursing Laboratory and Diagnostic Tests Demystified, Second EditionNo ratings yet
- Nursing Made Easy ICU VisitationDocument1 pageNursing Made Easy ICU VisitationSean Mercado100% (1)
- Third Spacing - Where Has All The Fluid GoneDocument14 pagesThird Spacing - Where Has All The Fluid Gonedbryant0101100% (15)
- Leg length discrepancy in children may indicate developmental dysplasia of the hipDocument6 pagesLeg length discrepancy in children may indicate developmental dysplasia of the hipIslam AminNo ratings yet
- Ekg Chart PDF 01Document5 pagesEkg Chart PDF 01YukiMaedaNo ratings yet
- Pathophysiology Notes 1-4Document24 pagesPathophysiology Notes 1-4Scotty Banks100% (3)
- Reducing CLABSI Rates Through Proper Hand HygieneDocument1 pageReducing CLABSI Rates Through Proper Hand HygieneMomina ArshadNo ratings yet
- Sepsis Content Concepts MapDocument3 pagesSepsis Content Concepts Mapghodghod1230% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Document PDFDocument3 pagesDocument PDFChrisyenDamanikNo ratings yet
- Too Pooped To PumpDocument14 pagesToo Pooped To PumpYusar CahyadiNo ratings yet
- Pope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralDocument14 pagesPope, B. CCRN-PCCN-CMC Review Endocrine and BehavioralKeisha JenkinsNo ratings yet
- IV InfiltrationDocument4 pagesIV InfiltrationMatthew Ryan100% (1)
- CNEA - CCRN Review - Behavioral-PsychosocialDocument12 pagesCNEA - CCRN Review - Behavioral-PsychosocialalexNo ratings yet
- Add Identity To SBARDocument2 pagesAdd Identity To SBARRoslitha HaryaniNo ratings yet
- 409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and ADocument21 pages409 Pope, B. and Maillie, S. CCRN-PCCN Review Multisystem and Q and Agliftan100% (2)
- Nutrition For Patients With Heart Failure.5Document5 pagesNutrition For Patients With Heart Failure.5Eileen del RosarioNo ratings yet
- Isotonic, Hypotonic, Hypertonic IV Third Spacing Where Has All The Fluid GoneDocument14 pagesIsotonic, Hypotonic, Hypertonic IV Third Spacing Where Has All The Fluid GoneJMC5053100% (2)
- Pathophysiology Basics ExplainedDocument45 pagesPathophysiology Basics Explainedpoojap44No ratings yet
- Clinical DeterioationDocument8 pagesClinical DeterioationSarahNo ratings yet
- Nursing Pharmacolocy Part 2Document176 pagesNursing Pharmacolocy Part 2TkNo ratings yet
- TNCC Prep Packet Revised June 2016Document12 pagesTNCC Prep Packet Revised June 2016nurse2012100% (3)
- Nursing Memory Joggers PDFDocument2 pagesNursing Memory Joggers PDFdummy damnNo ratings yet
- SepsisDocument14 pagesSepsislengkong100% (9)
- 081-Medical-Surgical Nursing Made Incredibly Easy, Third Edition (Incredibly Easy Series) - LippinDocument2 pages081-Medical-Surgical Nursing Made Incredibly Easy, Third Edition (Incredibly Easy Series) - LippinAlby RajanNo ratings yet
- Increased Intracranial Pressure and Monitoring Site PDFDocument21 pagesIncreased Intracranial Pressure and Monitoring Site PDFSari RakhmawatiNo ratings yet
- Hemodynamic Assessment ParametersDocument2 pagesHemodynamic Assessment ParametersalexNo ratings yet
- Patho Exam QuestionsDocument3 pagesPatho Exam QuestionsAndin GangNo ratings yet
- CEN Guide 4: Guide For The Inclusion of Environmental Aspects in Product StandardsDocument18 pagesCEN Guide 4: Guide For The Inclusion of Environmental Aspects in Product StandardsLauren GarciaNo ratings yet
- IV Therapy Lippincott Manual of Nursing PracticeDocument20 pagesIV Therapy Lippincott Manual of Nursing PracticeHejia MagangcongNo ratings yet
- Hemodynamic Management Pocket Card PDFDocument8 pagesHemodynamic Management Pocket Card PDFjenn1722No ratings yet
- Vasopressors and InotropesDocument4 pagesVasopressors and InotropesSdNo ratings yet
- Nursing Bullets Fundamentals ReviewDocument65 pagesNursing Bullets Fundamentals Reviewjoan olanteNo ratings yet
- Obstetrics - Cardiovascular Disease in PregnancyDocument3 pagesObstetrics - Cardiovascular Disease in PregnancyJonathanNo ratings yet
- CardiacDisorders StudyGuideLongDocument7 pagesCardiacDisorders StudyGuideLongYukiMaeda100% (1)
- MedSurg Nursing Clinical-Concept Map-2Document3 pagesMedSurg Nursing Clinical-Concept Map-2adaezeNo ratings yet
- CCRN Cert Review Neuro 2Document15 pagesCCRN Cert Review Neuro 2Giovanni MictilNo ratings yet
- ACAQ Crit Care Nursing CurriculumDocument91 pagesACAQ Crit Care Nursing CurriculumAnne Julia Agustin100% (1)
- Nursing Care of PlanDocument16 pagesNursing Care of PlanDbyNo ratings yet
- CCRN-PCCN Review GastrointestinalDocument23 pagesCCRN-PCCN Review GastrointestinalGiovanni MictilNo ratings yet
- FNP Resume Jenna Gibson 2022Document2 pagesFNP Resume Jenna Gibson 2022api-619271904No ratings yet
- This Study Resource Was: G R A D E S L A B - C O MDocument8 pagesThis Study Resource Was: G R A D E S L A B - C O MHugsNo ratings yet
- Concept Maps Nursing ProcessDocument19 pagesConcept Maps Nursing Processdina0108100% (1)
- Template For NURSING NotesDocument2 pagesTemplate For NURSING Notesbngraham4No ratings yet
- ACLS Provider Manual Supplementary Material: © 2020 American Heart AssociationDocument75 pagesACLS Provider Manual Supplementary Material: © 2020 American Heart AssociationpolelNo ratings yet
- Pharm PhalshDocument206 pagesPharm PhalshJohn MichealNo ratings yet
- Basic EKG Dysrhythmia IdentificationDocument40 pagesBasic EKG Dysrhythmia IdentificationIlda Dhe Devis Spaho100% (1)
- Guide to Listening Lung SoundsDocument24 pagesGuide to Listening Lung SoundsAtu KaushalNo ratings yet
- Simple Guide For Basic Nursing InterventionsDocument13 pagesSimple Guide For Basic Nursing InterventionsMelvin NizelNo ratings yet
- References: NCSBN's Review For The NCLEX-PN ExaminationDocument5 pagesReferences: NCSBN's Review For The NCLEX-PN Examinationbapimirab6540% (1)
- Dimensional Analysis For Nursing StudentsFrom EverandDimensional Analysis For Nursing StudentsNo ratings yet
- Medical Abbreviations GlossaryDocument15 pagesMedical Abbreviations Glossarydbryant0101100% (9)
- Vancomycin Dosing and Monitoring in AdultsDocument1 pageVancomycin Dosing and Monitoring in AdultsjulialeoNo ratings yet
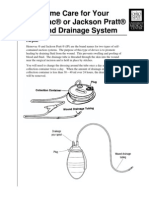
- Article Wound DrainsDocument8 pagesArticle Wound DrainsZeynab AbokarNo ratings yet
- US Army Medical Course MD0918-100 - Nursing Care Related To The Gastrointestinal and Urinary SystemsDocument137 pagesUS Army Medical Course MD0918-100 - Nursing Care Related To The Gastrointestinal and Urinary SystemsGeorges100% (1)
- Jackson PrattDocument7 pagesJackson PrattjulialeoNo ratings yet
- NGT InsertionDocument10 pagesNGT Insertionapi-3722454100% (3)
- Article Wound DrainsDocument8 pagesArticle Wound DrainsZeynab AbokarNo ratings yet
- Parsing Nursing NotesDocument28 pagesParsing Nursing NotesjulialeoNo ratings yet
- Parsing Nursing NotesDocument28 pagesParsing Nursing NotesjulialeoNo ratings yet
- British Heart Journal, 1977, 39, 1019-1025Document7 pagesBritish Heart Journal, 1977, 39, 1019-1025julialeoNo ratings yet
- Review Notes For NCLEX CGFNS - Aortic AneurysmsDocument2 pagesReview Notes For NCLEX CGFNS - Aortic Aneurysmswyndz100% (3)
- Psychiatric Nursing QaDocument20 pagesPsychiatric Nursing QajulialeoNo ratings yet
- Nurse Patient ShipDocument97 pagesNurse Patient Shipcharby12108272100% (2)
- Psych NSG Sample QuestionsDocument7 pagesPsych NSG Sample Questionspaul100% (8)
- Review Notes For NCLEX CGFNS - Aortic AneurysmsDocument2 pagesReview Notes For NCLEX CGFNS - Aortic Aneurysmswyndz100% (3)
- FellowshipbrochureDocument4 pagesFellowshipbrochurejulialeo100% (2)
- Sickle Cell AnemiaDocument5 pagesSickle Cell Anemiajulialeo100% (2)
- Sickle Cell AnemiaDocument10 pagesSickle Cell AnemiaNader Smadi100% (1)
- National Institutes of Health SicklecellbookletDocument16 pagesNational Institutes of Health Sicklecellbookletjulialeo100% (2)
- Sickle Cell AnemiaDocument23 pagesSickle Cell AnemiaJesmin_36No ratings yet
- Triage and Response: Quick LookDocument16 pagesTriage and Response: Quick LookjulialeoNo ratings yet
- Sickle Cell AnemiaDocument37 pagesSickle Cell Anemiahazelposis75% (4)
- Nursing Test Taking SkillsDocument6 pagesNursing Test Taking SkillsNurseStuffNo ratings yet
- PN Dhapter57Document5 pagesPN Dhapter57julialeoNo ratings yet
- Triage and Response: Quick LookDocument16 pagesTriage and Response: Quick LookjulialeoNo ratings yet
- Breast SurgDocument9 pagesBreast SurgjulialeoNo ratings yet
- PN Dhapter59Document4 pagesPN Dhapter59julialeoNo ratings yet
- PN Dhapter58Document7 pagesPN Dhapter58julialeoNo ratings yet