Professional Documents
Culture Documents
PA Cath Dvorak King
PA Cath Dvorak King
Uploaded by
sgod340 ratings0% found this document useful (0 votes)
4 views5 pagesppp
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentppp
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
4 views5 pagesPA Cath Dvorak King
PA Cath Dvorak King
Uploaded by
sgod34ppp
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 5
CAROL DVORAK-KING, RN, CCRN
PA catheter
numbers made easy.
If you're less than
comfortable interpreting
data from pulmonary
artery catheters, try
using this worksheet.
It makes analyzing
your patient's cardiac
status a snap.
CAROL DVORAKKING is an ICU
staff nurse at Good Samaritan
Hospital in Kearney, Neb.
‘STAFF EDITOR: Amy Slugg Moore
Patmonary artery (PA) catheters
are one of the most important and
reliable assessment tools available
to the critical care nurse. Used to
monitor hemodynamic status, these
catheters directly measure pros-
sures inside the right side of the
heart and in the pulmonary artery.
In doing 80, they yield valuable
clues as to how well the heart fune-
‘tions as a pump.
For a nurse who is unfamiliar
with them, though, PA cathevers
cat be a great, source of auaiely,
To make hemodynamic intor-
pretation easier—for experienced
and inexperienced nurses alike—I
suggest using the PA catheter
worksheet shown on page 46. It
can help the ICU nurse track a
patient's vandiae status, monitor
response to medications, and an-
ticipate the appropriate medical
intervention,
‘The workshoot has its limita-
tions, though. Although itis help-
ful in the evaluation of most eam
diac patients, particularly those
with a diagnosis of myocardial in-
farction (MD, congestive heart ail
ure (CHF), ur eardivgenicshuck, it
doesn't work well for every type of
cardine disease or shock state.
‘And it shouldn't be used for diag-
nostie purposes.
Before you can put the work-
Sheet to use, you need to have an
understanding of basic hemody-
namie principles. Here is a quick
review.
What the numbers:
and acronyms mean
Pulmonary artery catheters mea-
sure—either directly or through
calenlation—the following hemo-
dynamic parameters:
Right atrial pressure (RAP).
This is the pressure in the right
atrium during ventricular fling.
It’s usually consistent with right
ventricular pressure heeause, diir-
ing diastole, the open tricuspid
valve permits direct communica-
tion between the two chambers.
The RAP, therefore, isa reflection
uf right veutricular” fuuction, It's
also essentially the same as the
central venous pressure (CVP).
‘Normal RAPis 1 to7mm Hg. It
is elovated in conditions like right
ventricular failure, tricuspid valve
Gisease, pericardial tamponade,
and fluid overload; it's decreased
{in hypovolemia and vasodilation,
Pulmonary artery pressure
(PAP). This is usel to evaluate car
iae fanction and detect. problems
in the pulmonary vaseulature. The
systolie (PAS) reading indicates
the pressure in the pulmonary ar-
tery as blood is being ejected from
the right ventticle, A high PAS
NOVEMBER 1907 RN 45
‘pressure can mean right heart fail
‘ure, cardiac tamponade, or pul-
monary hypertension. A decrease
indicate hypovolemia
"The diastole (PAD) reading rep-
resents pressure in the pulmonary
artery as blood moves frum the
artery into the lung's capillaries.
‘An increase in PAD pressure can
indicate left ventricular failure or
pulmonary hypertension, A de-
erease ean signal hypovolemia,
Normal PAP is 20-30/10-15 mm.
‘Hg. The mean PAP is the averaxe
pressure in the pulmonary vascu-
Iature throughout the cardiac cy-
de. It’s usually 10-20 mm Hg.
Pulmonary artery wedge pres-
ure (PAWP). This parameter re-
fleets left ventricular function. It
is also called the pulmonary capil-
lary weaige pressure (PCWP). To
rmeassre it, the balloon at the tip
of the PA catheter is inflated.
Blood flow pushes Ue ballown vut,
of Une pulmonary artery and into
tho pulmonary capillaries, where
it “wedges” in one of these small
vveseels, So, the catheter tip is es
sentially looking at. the left atri-
uum. Because, during diaswle, the
valve between the alrium and ven-
Lricle is upen, the PAWP reflects
left ventricular pressure,
Normal PAWP ranges from 6to
15 mm Hg: Unless the patient has
pulmonary disease, the average
PAWP should correlate with the
PAD. A high PAWP occurs with
left. ventricular failure, septal de-
fects, and with mitral insufficiency.
A low PAWP can be a sign of
hypovoletnia,
Cardiae output (CO). This is
the volume of blood pamped fram
the heart in one minute. Normal
cardiae output ranges between 4
and 8 L/min, I's equal o the heart
rate multiplied by the stroke vol-
ume (SV), which is the amount of
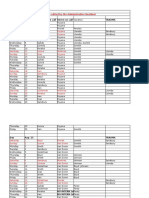
Normal
{Low to normal PAP
‘Subset It
towel
Low to normal PAWP
Carciae index (CI) Uminien?
Cbsnerheeenhs buenas
PA Catheter Worksheet
Subset tit
‘Wocmal Cl
High PAWE
Na HAS ET Hv WII Tes 16 iSTOIT IOS z0z1 ze 0s zERCET 207990
Pulmonary artery wedge pressure (PAWP) (mm Hg)
blood ejected from the left ventri
cle with each contraction. Normal
SV is between 60 and 130 ml.
Stroke volume, in turn, is deter
mined by contractility, preload,
and afterload. Contractility is the
fore with which the heart muscle
pumps. As contractility rises, 80
do SV and CO.
reload is the amount of strotch
on the myocardium at the end of
diastole. ‘The KAP reflects the
right heart’s preload and the
PAWP reflects the lefts
According to the Frank-Starling
Jaw, the more the myofibrils stretch
before systole, the stronger the
heart will contract. In other words,
increasing preload increases con-
tractlity. This holds true, howov-
er, only up to a point. Ifthe ventri-
des overstretch, contractions actu
ally beeome weaker, and stroke
volume and cardiac output drop.
‘Afterload is the impedaneeto the
é’jection of blood from the ventricle,
or the resistance that the ventricle
‘must overcame to eject blood for-
ward, Blood viseesty, vasmlar dis.
tensibility, and pressure in. the
pulmonary vasculature, aorta, and
systemic arteries all contribute to
stance, Increasing afterload will
raise the pressure against which
the heart must pamp; so & high
afterload makes the heart. work
harder, IfaRerlond is too high, SV
and CO will probably drop.
Systemie vascular resistance
(SVR) is a measure of the lef
heart's afterload (normal is 900 —
1,400 dynes/sec/em’). Pulmonary
vascular resistance (PVR) refleets
theafterload of the right heart (it's
normally 50 ~ 250 dynesisee/em®).
‘These values are caleulated from
other hemadynamie parameters.
Cardiac index. This, too, is a
calculated value. It’s determined
by dividing CO by the patient's
body surface area (BSA). ‘The
monitoring equipment calenlates
BSA from the patient's height and
‘weight. A normal CI is between
46 RN NOVEMBER 1997
| Hemodynamic subsets: Possible interventions
eT
Relow are the treatment options and possible interventions foreach clinical subset, Drugs and other
{actors that affect preload, aterioed, contractility, and heart rate are also listed.
SUBSET |
Normal Cl, low to normal PAWP
Monitor regularly
‘Administer 0,
Offer prt pai medication
Sedation red
‘These interventions are usually necessary since
most patients aron’t problem-free; they may just
have normal readings.)
SUBSET IIL
Normal Cl, high PAWP _
Kaminister 0;
Decrease pre'oad
Offer pen pain medication
Sedation as ordered
Optimize heart rate
Enhance contractility
SUBSET II
Low Cl, low to normal PAWP
SUBSET IV
Low Cl, high PAWP.
Raministor WV fluids
Administer O,
Enhance contractility
Decrease afterload
ABP
Optimize heart rate
‘Surgical intervention for a vorectable cardiac problem
‘aiminister Op
Decrease preload
Decrease afterload
Enhance contractility
Optimize heart rate
ABP
Surgicel intervention for a correctable cardiac problem
| rao
To increase: To increase:
Fluids Dovatnine (Inotropin)
Vasopressors Norepinephrine (Levephed)
To decrease: To decrease:
Diuretics ACE inhibitors
Fluid restriction Alpha blockers
Low-salt diet ‘Amrinone (Inesor)
‘Arterial vasodilators
Beta lockers
Calcium channel blockers
tage
Mitrinome (Primeccr)
Morphine
Nitrates
Nitroprusside (Nipride,
‘Nitropress)
Positive-end expiratory
pressure (PEEP)
Venous vasodilators
CONTRACTILITY TE
To increase/enhance: To increase:
‘Aminone (Inocor) Atropine
Dobutamine (Dobutrex) Cardiac. pacing
Doparnine (lnotrepin)
Calcium
Digoxin (Lanoxin)
Epinephrine (Adrenalin)
Isoproterenol (Isupre!)
Milrinane (Primacor)
Norepinephrine
(Levophed)
To decrease.
Beta blockers
Calciuin channel blockers
Epinephrine (Adrenalin)
Isouroterenol (Isupret)
To decrease:
Antiarshythmies
Beta blockers
Calcium channel blockers
Cardiac pacing
Digoxin (Lanoxin)
| aan evar otra eens =
24-4 Lémin/m®. I like to think of
{tas an individualized CO because
it takes budy size into account.
A tool that helps
plot cardiac function
tal axis,
With these basics in mind, let's
take a closer look at the PA
ealheler worksheet. The vertical
axis measures the patient's car~
iae performance, as
the CL. The PAWP, a reflection of
preload, is charted on the horizon
To use this tool, simply plot your
patient's Cl against his PAWP.
‘The point should fall into one of the
‘box's quadrants, or clinical subsets
‘Treatinent options for each subset
are listed in the table above.
For example, a cardiae patient
with a normal CI and low to nor-
mal PAWP would bo insubset I. A
patient with a low PAWP and a
ow CI would be in subset T—an
area that may reflect volume
depletion. Since this subset also
includes pationts with a low CI but
‘a normal PAWP, someone with
indicated by
NOVEMBER 1997 RN 47
plotting the CI and PAWP, be
PA Catheter Worksheet (Mr. Jay) iene eee acne
other hemodynamic parameters
as well
si i
Subset | Subset It Putting the worksheet
tow to rormat Paw [Tf LTE HEH rane to action
Day 2 To better understand how to use
10am this tool, consider the case of Mr.
Jay, a 69-year-old male with a his.
tory ofheart disease. A year and a
ydex (CI) Liminien?®
oem. half ago, he suffered an uncompli
ated but extensive anterior wall
MI. He underwent. trple-hypass
‘Subset I Subset IV surgery and went home on med-
Low cl Low cl ica ecrease the heart's
Low to normal PAIN ign PAE Sr ayers
Pa aa Ee wp lov isis 4 1SieT7 18102021 aSaNIESERTINTOIO hibitor captopril (Capoten) and
Pulmonary artery wedge pressure (PAWP) (mm Hg) isosorbide dinitrate (Isordil), De-
spite these interventions, Mr. Jay
has been having increasing dysp-
nea on exertion, wealmess, and
bradycardia that's compromising subset a patient falls, your goal is fatigue.
candine ontpt might als be in th mave him tawani subset T. Now, his wife has hronght. him
this box. Let's say, for instance, a patient to the ED because he is so weak
‘A volume overloaded patient has been overly diuresed and is that he cannot maike the trip from
with congestive heart failure tachyenrdic; his numbers put him his chair to the nearby bathroom
(CHF), for example—who has a in subset II, According to the in- without exporioncing severe short-
borderline or normal CI but ahigh terventions. worksheet, you will ness of breath. He has been sleep-
PAWP wonld fall into subset 111, administer IV fiuids—eantionsly, ing sitting mp in his chair heeanse
‘The patient in eardiogenie shock thongh, heeanse yon don’t want tit. helps him “breathe better.” His
‘would be in subset IV:he'd have a make things worse—and possibly wife tells you that his legs have
high PAWP and a low CI. vasoactive drugs. Each time you become more swollen and he has
‘These subsets are general cate- intervene or make an assessment, gained six pounds in the last few
gories that can be helpful to nurs- plot his CI and PAWD. By doing days, even though he hasn't been
‘es who care for patients at risk for this, you will be able to gauge his eating well. He denies any chest
low eardine output states. Don't response to medications and other pain.
follow them too rigidly, For exam- treatment, Suspecting acute CHF, his car
| ple, don’t be lulled into thinking To be truly helpful, the work- diologist admits him to the CCU,
‘that a patient. in subset I is fine sheet must be used before and where a PA catheter is inserted.
just because his Cand PAWP are after each intervention and when- In the meantime, Mr. Jay's labs
normal. He hasa PA catheter fora ever there is a change in the pa~ and EKG, which were done while
‘reason, und he'l still require regu-tient's condition—not just at reg- he was in the emergency depart-
Jarmonitoring and porsibly 0,,prn ularly echeduled intervals ouch aa ment, come back negative for MI,
pain relief, and sedation as well. every two hours. Although you affirming the diagnosis of CHF.
And keep in mind that not every might not sueceed in getting every You perform a physical assess-
patient. will fit neatly into the patient intosubset T, yon still want, ment and obtain the initial PA
‘worksheet's categories, ‘to move them in that direction. catheter readings at 10 a.m. You
nee you determine into which And even though you are only nove that Mr. Jay 1s restless and
48 RN NOVEMBER 1997
anxious, and he is barely able to
speak because of his labored
breathing. His skin is pale, warm,
and moist. Capillary refil time is
four seconds. Vital signs are: RR
30 (with the use of accessory mus-
los}, KF YWod; and HE 138, sinus
tachyeardia, Jugular vein disten-
sion is approximately five centi-
meters, You hear crackles posteri-
orly and a classic $3 gallop.
His PA catheter readings re-
veal a PAWP of 26 and a CI of 25.
You plot these findings on the
worksheet, a8 shown on at lef,
and ft places Mr. Jay in subset TIT.
He's given IV furosemide (Lasix)
and IV digoxin (Lanoxin) STAT;
supplemental oxygen that was
started in the ED is continued. In
some hospitals, Mr. Jay might also
have been started on dobutamine,
but that is up ta the protocol at
your facility.
By 2 pm, Mr. Jay's vitals have
improved: BP 10264; HR 98, and
RR 22. His PAWP is 16 and CT is
2.6, placing him in arms reach of
subset I—safe for now.
When you return the next day,
however, you find that Mr. Jay
has taken a tum for the worse. At
8am. his BP has fallen to 7882.
“Your assessunent reveals a weak,
rapid, and thready pulse. His skin
is cool and elammy. He can barely
breathe, and his blood gas results
are poor. His PAWP is 28 and CI
ie 15, with an SVK of 1,956
dynes/seclem®. He is now in sub-
set, TV—cardiogenie shoek—and
he is immediately intubated.
‘The canliologist asks you to be-
‘gin a dupanine infusion, adminis-
ter more furosemide, snd a bolus
of amrinone (Inocor). Mr. Jay is
also placed on a nitroprusside
(ipride, Nitropress) drip. De-
spite these interventions, his eon-
dition does not get better, so the
physician orders an intra-aortic
talloon pump (LARP) to maximize
perfusion,
Once on the pump, Mr. Jay
slowly begins to improve. By 4
pam, his BP has inereased but is
hovering around 880. Wis TR
Muctuates between 102 and 118.
Tis PAWP is 20, Cl is 18, and
SVR is down to 1,700, He's stil in
subset TV and has a way 10 £0
before he is completely stable, but
at least he's moving in the desired
direction,
Because Mr. Jay needs a new
heart, he is placed on a transplant,
list. If he continues to improve, he
will be weaned from the pump and
given dobutamine. He may even-
tually be able go hame with orders
for home infision therapy and
skilled nursing care, For the time
being, however, he remains in the
cou.
‘Although nothing can replace a
murze’s judgment, critical thinking
skills, and Imowledge, the PA eath-
eter worksheet can be dU
‘mendous help when used ws an
adjunct to patient assessment. By
providing, a visual representation
of the patient's progress, the work:
sheet helps the experienced maree
‘anticipate the appropriate care and
new nurses clearly see how vari-
ous treatments affect hemodiymam-
iestatus.1
‘SUGGESTED RFADING
1, Dally, EL. & Schroade, J. , (1994).
Tachnigucs in bedside hembajinamic man:
Itong (Sth ed). St. Louis: Musby-Year
Boot, Ine
2. Davore, G. 0. (1995). Heraxamic
‘monitoring: Invasive and noninvasive clin-
{eal appricatint (Zid ws.) Philadelphia.
WB, Saunuers Company.
2, ¥itele Cee, J. M, & O'Sulvan, C.K
(1997). Herds monitoring. In J.
Hartshorn, ML Sole, & ML. Lamborn
(Eds), Inoduction to critical care nursing
(pp. 86-121), Phiadelpnia: W. 8. Saur-
ers Company.
NOVEMBER 1997 RN 49
—
«SAFE.
PERMANENT
Nd
be
100 MUCH
TO ASK?
SPEAK UP
FOR AN ABUSED
AND NEGLECTED
CHILD IN COURT.
Is 11
Far infoomation on volunteering
cat Court lgpointed Special
ANebweate call L-NV-028-72
orwrit
Navid CAS]
100 Wi: Hare
Neth
Suite 300
Scuttle WA
asity
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Absite Review VascularDocument183 pagesAbsite Review Vascularsgod34No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Resident Hernia LectureDocument106 pagesResident Hernia Lecturesgod34No ratings yet
- Venous DiseaseDocument50 pagesVenous Diseasesgod34No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Modes of Mechanical VentilationDocument4 pagesModes of Mechanical Ventilationsgod34100% (1)
- NOAC ChartDocument2 pagesNOAC Chartsgod34No ratings yet
- Master Schedule 10-22Document65 pagesMaster Schedule 10-22sgod34No ratings yet
- Nutrition Support: Sean P Harbison MDDocument42 pagesNutrition Support: Sean P Harbison MDsgod34No ratings yet
- Surgery Preround Template SkeletonDocument2 pagesSurgery Preround Template Skeletonsgod34No ratings yet
- Veins More DistensibleDocument27 pagesVeins More Distensiblesgod34No ratings yet
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Document35 pages7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34No ratings yet
- Endoscopy TechniqueDocument8 pagesEndoscopy Techniquesgod34No ratings yet
- Colon CADocument16 pagesColon CAsgod34No ratings yet
- Anast Bleed MMDocument17 pagesAnast Bleed MMsgod34No ratings yet