Professional Documents
Culture Documents
Fungal Rhinosinusitis
Uploaded by
igorOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fungal Rhinosinusitis
Uploaded by
igorCopyright:
Available Formats
MAIN ARTICLE
The Journal of Laryngology & Otology (2013), 127, 867871.
JLO (1984) Limited, 2013
doi:10.1017/S0022215113001680
Allergic fungal sinusitis and eosinophilic mucin
rhinosinusitis: diagnostic criteria
N URI1, O RONEN1, T MARSHAK1, O PARPARA1, M NASHASHIBI2, M GRUBER1
Departments of 1Otolaryngology Head and Neck Surgery, and 2Pathology, Lady Davis Carmel Medical Center,
Bruce Rappaport Faculty of Medicine, Technion Israel Institute of Technology, Haifa, Israel
Abstract
Background: Chronic sinusitis is one of the most common otolaryngological diagnoses. Allergic fungal sinusitis
and eosinophilic mucin rhinosinusitis can easily be misdiagnosed and treated as chronic sinusitis, causing
continuing harm.
Aim: To better identify and characterise these two subgroups of patients, who may suffer from a systemic disease
requiring multidisciplinary treatment and prolonged follow up.
Methods: A retrospective, longitudinal study of all patients diagnosed with allergic fungal sinusitis or
eosinophilic mucin rhinosinusitis within one otolaryngology department over a 15-year period.
Results: Thirty-four patients were identified, 26 with eosinophilic mucin rhinosinusitis and 8 with allergic fungal
sinusitis. Orbital involvement at diagnosis was commoner in allergic fungal sinusitis patients (50 per cent) than
eosinophilic mucin rhinosinusitis patients (7.7 per cent; p < 0.05). Asthma was diagnosed in 73 per cent of
eosinophilic mucin rhinosinusitis patients and 37 per cent of allergic fungal sinusitis patients.
Conclusion: Allergic fungal sinusitis and eosinophilic mucin rhinosinusitis have the same clinical presentation
but different clinical courses. The role of fungus and the ability to confirm its presence are still problematic
issues, and additional studies are required.
Key words: Sinusitis; Fungus; Eosinophil; Mucin; Diagnosis
Introduction
Rhinosinusitis is defined as an inflammatory process
which involves the nasal and paranasal sinuses
mucosa. It is estimated that approximately 30 per cent
of the US population suffer from rhinosinusitis symptoms, and that the global cost of the disease is over 2
billion US dollars per year.1
The commonest cause of acute rhinosinusitis is
superimposed viral and bacterial infection. Chronic rhinosinusitis is linked to other aetiological factors such as
fungi, allergic reactions, mucociliary disorders, and
anatomical and systemic causes.
In recent years, the development of advanced diagnostic methods has facilitated research emphasising
the importance of fungal infections in chronic rhinosinusitis. In 1999, Ponikau and colleagues Mayo Clinic
group2 reported that 96 per cent of 210 chronic rhinosinusitis patients undergoing endoscopic sinus
surgery had a positive fungal culture, together with
signs of eosinophilic inflammation. Other study
groups described differing prevalences of positive
fungal cultures, ranging from 0 to 50 per cent.2,3
These findings support the theory that all types of
chronic rhinosinusitis are somehow related to a nonAccepted for publication 3 December 2012
allergic eosinophilic sinus inflammation secondary to
fungal infection.46
Fungal rhinosinusitis is divided into invasive and
non-invasive types. The category of invasive fungal
sinusitis includes acute invasive (fulminant) fungal
sinusitis, chronic invasive fungal sinusitis and granulomatous invasive fungal sinusitis. Non-invasive fungal
sinusitis includes fungal ball (mycetoma), allergic
fungal sinusitis and eosinophilic mucin rhinosinusitis.
Allergic fungal sinusitis was first described in 1983 as a
benign fungal disease of the sinuses in immunocompetent
patients.6 It has been estimated that this disease accounts
for 510 per cent of all patients with chronic rhinosinusitis.7 Two-thirds of allergic fungal sinusitis patients suffer
from allergic rhinitis, and approximately 90 per cent have
increased blood levels of immunoglobulin (Ig)
E. Allergic fungal sinusitis is common among adolescents and young adults, and is more common in geographical areas of high humidity. Two-thirds of patients
are atopic and half suffer from asthma.8
Allergic fungal sinusitis usually has an indolent
clinical course but late complications can occur, including proptosis, visual disturbances and facial
dysmorphism.
First published online 13 August 2013
868
There is no clear agreement regarding diagnostic criteria for allergic fungal sinusitis. In 1993, Loury et al.9
suggested criteria which included eosinophilia, elevated IgG or positive skin testing, elevated IgE for
fungal antigen, nasal polyps or nasal mucosal
oedema, typical computed tomography (CT) or magnetic resonance imaging (MRI) findings, and histological evidence of allergic mucin, fungal hyphae and lack
of invasion. In 1994, Cody et al.10 reported the Mayo
Clinic experience, and suggested that diagnostic criteria comprise only the presence of allergic mucin
and fungal hyphae, or a positive fungal culture. One
of the most popular sets of criteria was published by
Bent and Kuhn in 1994.5 It was based upon five
elements: IgE-mediated hypersensitivity, polyposis,
typical CT scan findings, eosinophilic mucin, and positive fungal culture or staining. Kupferberg and Bent11
further classified allergic fungal sinusitis into stage 0
(no oedema or allergic mucin), stage I (oedematous
mucosa), stage II (polypoid oedema) and stage III
(polyps).
In most cases of allergic fungal sinusitis, dematiaceous fungi have been isolated, such as alternaria,
bipolaris, curvularia, drechslera, exserohilum and helminthosporium; a small proportion of aspergillus has
also been isolated.
Possible findings on CT scan include sinus opacification, bone destruction and thinning of the bony structures secondary to expansion of accumulated mucus.
Long-standing disease may present with dramatic
radiological findings such as invasion of the skull
base and orbit. Calcification within the sinuses is due
to the accumulation of elements such as iron and
manganese within the mucus.12
A suggested radiological staging system was published by Wise et al.13 in 2009, ranking each destroyed
bony element or expansile lesion and giving a score of
up to 24 points. Although CT scanning is suggested,
MRI scanning is an important adjunct when considering dural involvement or intracranial expansion.
Histological staining with haematoxylin and eosin
(H&E) highlights mucus and its cellular structures.
Allergic mucin, also termed eosinophilic mucin by
some, comprises over-produced mucus, eosinophils
and branching, non-invasive fungal hyphae.
Histological analysis shows fragmented eosinophils
and CharcotLeyden crystals, produced by eosinophil
breakdown.
Another useful histological staining is Gomori
methamine silver, which colours fungi brown-black.
Haematoxylin and eosin staining is negative when
few fungal hyphae are present; in this case, Gomori
methamine silver staining is important as it can delineate fungi when hyphae are sparse.
It should be emphasised that allergic fungal sinusitis
does not involve blood vessel or tissue invasion.
During follow up of allergic fungal sinusitis patients,
it is useful to monitor blood levels of IgE (specific to
the relevant fungal type) as a marker of recurrence.
N URI, O RONEN, T MARSHAK et al.
The mainstays of allergic fungal sinusitis treatment
are surgical and medical. The usual surgical treatment
is careful endoscopic debridement, followed by a
course of systemic corticosteroids. This treatment
lowers cytokine levels, which prevents the production,
activation and migration of eosinophils. Programmed
cell death is also induced. However, there is no published standard treatment protocol. Corticosteroid treatment usually extends for two to three months,
including gradual tapering of the dose, but there is currently no consensus regarding corticosteroid dosage or
duration.7,14,15
Other systemic therapies for allergic fungal sinusitis
have been proposed, but none has been clinically
proven.
Eosinophilic mucin rhinosinusitis was first described
as a subtype of sinusitis which resembled allergic
fungal sinusitis clinically and histologically.
Eosinophilic mucin rhinosinusitis has been defined as
a systemic disease, and therefore bilateral disease is
most common. In contrast, patients with allergic
fungal sinusitis have an allergic response to fungi,
which may occur unilaterally or bilaterally depending
on the antigenic stimulation. Eosinophilic mucin rhinosinusitis is significantly associated with asthma, and an
increased incidence of aspirin sensitivity has also been
reported. Systemic corticosteroid is the treatment of
choice for eosinophilic mucin rhinosinusitis.
Computed tomography shows similar features to allergic fungal sinusitis (i.e. absence or destruction of the
medial nasal wall, hyperattenuation, and thinning of
sinus walls), but these are seen bilaterally in most
cases. The surgical appearance is of typical mucoid
material, with negative fungal cultures.16
The present study aimed to compare patients with
eosinophilic mucin rhinosinusitis and with allergic
fungal sinusitis, followed up in our rhinology clinic,
according to certain predetermined clinical criteria.
Differences between these two groups have been
rarely addressed, and there are few reports describing
patients with eosinophilic mucin rhinosinusitis.
Clarifying the criteria which differentiate these two
patient groups may facilitate quicker and more accurate
diagnosis, assisting timely and appropriate treatment.
Materials and methods
We performed a retrospective, longitudinal study
including all patients diagnosed with allergic fungal
sinusitis or eosinophilic mucin rhinosinusitis in the otolaryngology department of Carmel Medical Center,
Haifa, Israel, over a 15-year period (19962010).
Thirty-four patients were included in the study
cohort: 26 with eosinophilic mucin rhinosinusitis and
8 with allergic fungal sinusitis. All patients were operated upon by the same surgeon.
Allergic fungal sinusitis was diagnosed according to
the criteria of Bent and Kuhn, as mentioned above. The
diagnosis of eosinophilic mucin rhinosinusitis was
based on the presence of extensive, polypoid disease
ALLERGIC FUNGAL SINUSITIS DIAGNOSTIC CRITERIA
with thick, eosinophilic mucus and no fungal hyphae,
as described in the pathological report. Eosinophilic
mucin rhinosinusitis patients were monitored in our rhinology clinic before and after surgery; during this time
period, no fungus was identified from various cultures
and pathological specimens. Wegeners disease and
ChurgStrauss disease were tested for and excluded
in all patients.
Information was collected from the following
sources, for all patients: demographic data; physical
examination and nasal endoscopy; CT scans; pathology
reports (all patients had pathological specimens collected during surgery, and all such specimens were
reviewed again by the pathologist and the surgeon);
bacteriological reports; surgical records; and data on
medical treatments, recurrences and follow-up times.
This study was approved by the institutional ethical
review board.
Results and analysis
Demographical and clinical parameters were compared, using Fishers exact test for continuous variables
and Students t-test for discrete variables.
Analysis was performed for 26 patients with eosinophilic mucin rhinosinusitis and 8 patients with allergic
fungal sinusitis.
Mean age was greater for the eosinophilic mucin rhinosinusitis patients (55.9 years) than the allergic fungal
sinusitis patients (34.5 years old) ( p < 0.0001).
Disease was bilateral in 91.6 per cent of eosinophilic
mucin rhinosinusitis patients and 62.5 per cent of allergic fungal sinusitis patients ( p < 0.05). Nasal obstruction was demonstrated in 34.6 per cent of eosinophilic
mucin rhinosinusitis patients and 100 per cent of allergic fungal sinusitis patients ( p < 0.05). Nasal discharge was demonstrated in 57.7 and 37.5 per cent of
the eosinophilic mucin rhinosinusitis and allergic
fungal sinusitis patients, respectively.
More allergic fungal sinusitis patients (50 per cent)
had orbital involvement at diagnosis, compared with
eosinophilic mucin rhinosinusitis patients (7.7 per
cent; p < 0.05). The lamina papyracea was involved
by the disease process in 50 per cent of allergic
fungal sinusitis patients and 15 per cent of eosinophilic
mucin rhinosinusitis patients, a statistically significant
difference ( p < 0.05).
Asthma was diagnosed in 7 per cent of eosinophilic
mucin rhinosinusitis patients and 37 per cent of allergic
fungal sinusitis patients, although this difference was
not statistically significant.
Endoscopic surgery was undertaken for all patients.
Some cases were managed with a navigation system to
enhance safety, especially when operating upon extensive and destructive lesions (e.g. orbital involvement
and frontal sinus surgery).
Most patients needed more than one surgical procedure during the study period; the mean and median
number of surgical procedures were respectively 3.3
and 2 for the eosinophilic mucin rhinosinusitis patients,
869
and 1.4 and 1 for the allergic fungal sinusitis patients
(the difference between means was not statistically
significant).
Histological examination utilised H&E (Figure 1),
periodic acid Schiff and Gomori methamine silver
stains. Fungi were identified in 87.5 per cent of the
allergic fungal sinusitis histological block specimens,
and none of the eosinophilic mucin rhinosinusitis
specimens.
All patients were available for follow up during the
study period. The mean (median) follow-up periods
were 9.7 (10 years) for the eosinophilic mucin rhinosinusitis patients and 8 years (8 years) for the allergic
fungal sinusitis patients.
Table I summarises results for the two groups.
Discussion
It is important to identify the common elements
between the different forms of eosinophilic sinusitis,
in order to better define and subclassify this condition.
Ferguson17 reported substantial clinical and immunological differences between allergic fungal sinusitis
and eosinophilic mucin rhinosinusitis. Aetiologically,
FIG. 1
Photomicrographs showing eosinophilic mucin rhinosinusitis.
(H&E; 20)
870
N URI, O RONEN, T MARSHAK et al.
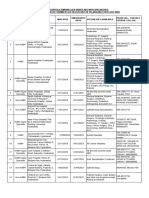
TABLE I
PATIENT DATA
Parameter
Total (n)
Age (mean (median); yr)
Males (n (%))
Females (n (%))
Bilateral disease (n (%))
Orbital involvement
(n (%))
IgE (mean; U/ml)
Asthma (n (%))
ESS (mean (median, SD); n)
AFS
EMRS
8
34.5 (31.5)
4 (50)
4 (50)
5 (62.5)
4 (50)
26
55.9 (57.0)
15 (57.7)
11 (42.3)
25 (96.1)
2 (7.7)
>500
3 (37.5)
1.4 (0.5, 1.7)
220.4
19 (73.1)
3.3 (2, 2.7)
AFS = allergic fungal sinusitis; EMRS = eosinophilic mucin rhinosinusitis; yr = years; Ig = immunoglobulin; ESS = endoscopic
sinus surgery; SD = standard deviation
allergic fungal sinusitis is based on the presence of an
immunological allergic reaction to fungi in predisposed
individuals. This tissue reaction results in the production of allergic mucus rich in eosinophils and
non-invasive fungi, together with marked elevation of
blood levels of specific IgE antibodies. Ferguson
believed that eosinophilic mucin rhinosinusitis represented a local immune reaction occurring secondary
to a systemic disorder.17 In most such cases, IgE
levels are within normal limits, with no observed
fungi, in contrast to allergic fungal sinusitis patients,
who present with elevated IgE due to fungal growth.
According to these basic differences, it is reasonable
to divide chronic rhinosinusitis patients into two
groups: fungal and non-fungal. The fungal subgroup
consists mainly of allergic fungal sinusitis patients.
The non-fungal subgroup consists of eosinophilic
mucin rhinosinusitis patients and patients with sinusitis
and aspirin-sensitive asthma (which deteriorates when
treated with non-steroidal anti-inflammatory drugs
such as aspirin).
Thick, eosinophilic mucus rich in inflammatory
debris is the hallmark of allergic fungal sinusitis.
When identified, it is the first clue that the surgeon
and pathologist should search for the presence of
fungus. But is such fungal presence the defining parameter for subgroup classification?
Another theory proposes that the first stage of
disease is the allergic reaction which prompts eosinophilic mucus production, while the second stage is
the antigenic reaction to the fungi trapped by this allergic reaction. This theory actually refers to the fungi as a
by-product, and known responses to various treatments
support this opinion. No anti-fungal treatments have
been proven to change the course of the disease. This
argument was further reinforced by a 2011 Cochrane
database review which concluded that there were no
data to support the use of such treatments.18
In 2007, Orlandi et al.19 investigated a different perspective concerning the expression of certain genes.
They examined DNA from allergic fungal sinusitis
patients, eosinophilic mucin rhinosinusitis patients
and healthy controls. Four genes were found to be
expressed in eosinophilic mucin rhinosinusitis but not
in allergic fungal sinusitis, coding for S-100 calciumbinding protein, cathepsin B, sialytransferase 1 and
ganglioside activator protein (GM2). These genes
are responsible for lysosomal activity and act as
mediators of inflammatory and tumoural processes.
Orlandi et al. suggested that the genetic profiles of
allergic fungal sinusitis and eosinophilic mucin rhinosinusitis were similar, although differences existed
and needed to be further clarified.
Ponikau et al.2 also investigated the role of fungi in
chronic sinusitis. In their study, fungus was present in
almost all hospital chronic sinusitis patients, as well
as in healthy controls. This finding questions the
nature of fungi in the aetiology of allergic fungal
sinusitis.
Most of the data on the clinical and immunological
differences between allergic fungal sinusitis and eosinophilic mucin rhinosinusitis have been derived from
Fergusons 2000 study.17 This author compared previously published data on 418 allergic fungal sinusitis
patients and 40 eosinophilic mucin rhinosinusitis
patients, together with information from a further 13
allergic fungal sinusitis patients and 29 eosinophilic
mucin rhinosinusitis patients from the authors own
database. In the latter database, 41 per cent of allergic
fungal sinusitis patients and 93 per cent of eosinophilic
mucin rhinosinusitis patients suffered from asthma; in
our study cohort, the prevalence of asthma was 37.5
and 75 per cent, respectively. In Fergusons study,
the mean patient age was 30 years in the allergic
fungal sinusitis group and 48 years in the eosinophilic
mucin rhinosinusitis group; in comparison, our
patients mean ages were 34.5 and 55.9 years, respectively. In Fergusons own cohort, bilateral disease was
present in 55 per cent of allergic fungal sinusitis
patients and 100 per cent of eosinophilic mucin rhinosinusitis patients, similar to our own data.
In our cohort, orbital complications were more
common among allergic fungal sinusitis patients (50
per cent) than eosinophilic mucin rhinosinusitis
patients (8 per cent). These orbital complications presented as diplopia, proptosis and lamina papyracea
destruction. This finding suggests a more aggressive
behaviour for allergic fungal sinusitis, and justifies
special clinical attention for this subgroup of patients.
The number of surgical procedures differed between
our two patient groups, with a mean of 1.4 procedures
for allergic fungal sinusitis patients but 3.3 procedures
for eosinophilic mucin rhinosinusitis patients, although
this difference was not statistically significant.
We cannot report accurate data on recurrence among
our eosinophilic mucin rhinosinusitis and allergic
fungal sinusitis patients. We found that patients who
presented with relevant symptoms and signs were
first diagnosed with allergic fungal sinusitis; only
later, after additional data collection from histological
analysis and fungal cultures, was the diagnosis of
871
ALLERGIC FUNGAL SINUSITIS DIAGNOSTIC CRITERIA
eosinophilic mucin rhinosinusitis considered. In some
cases, eosinophilic mucin rhinosinusitis was suspected
only after multiple surgical procedures and several
relapses, and only at that stage did the patient begin
to receive appropriate, systemic therapy.
Allergic fungal sinusitis and eosinophilic
mucin rhinosinusitis are easily misdiagnosed,
hindering effective treatment
They have the same initial clinical
presentation but different clinical courses
Eosinophilic mucin rhinosinusitis is usually
bilateral, and surgical treatment more
common
Allergic fungal sinusitis is prone to early
orbital involvement
In both, the role of fungi, and diagnostic
protocols, are unclear
Establishing diagnostic criteria to differentiate between
allergic fungal sinusitis and eosinophilic mucin rhinosinusitis is difficult. The presence of fungi is essential,
and the identification of the culprit is only possible
through the use of appropriate stains. It is possible
that some of our patients diagnosed with eosinophilic
mucin rhinosinusitis actually had allergic fungal sinusitis but that no fungi were identified. We emphasise
that the use of Gomori methamine silver staining is
essential to the diagnosis: the use of H&E staining
alone is inadequate.
Another difficulty in preparing fungal cultures from
sinus secretions arises from the differing culture protocols followed by different laboratories. This discrepancy probably explains a significant amount of the
observed variance in positive fungal culture rates:
various studies have reported rates of between 10 and
97 per cent.
Conclusion
Allergic fungal sinusitis and eosinophilic mucin rhinosinusitis have the same initial clinical presentation,
although they are different diseases with (usually) differing clinical courses. Our results indicate higher
complication rates and fewer surgical procedures in
the allergic fungal sinusitis subgroup, compared with
the eosinophilic mucin rhinosinusitis subgroup. More
specifically, the clinical course of allergic fungal sinusitis seems to be more aggressive, with a higher prevalence of orbital complications and greater associated
morbidity. The role of fungus and the ability to
confirm its presence are still problematic issues.
Additional studies are required to investigate aetiology,
diagnostic standardisation and patient care.
References
1 Lucas JW, Schiller JS, Benson V. Summary health statistics for
U.S. adults: National Health Interview Survey, 2001. Vital
Health Stat 10 2004;218:1134
2 Ponikau JU, Sherris DA, Kern EB, Homburger HA, Frigas E,
Gaffey TA et al. The diagnosis and incidence of allergic
fungal sinusitis. Mayo Clin Proc Sep 1999;74:87784
3 Corey JP. Allergic fungal sinusitis. Otolaryngol Clin North Am
1992;25:22530
4 Millar J, Lamb D. Allergic bronchopulmonary aspergillosis of
the maxillary sinuses. Thorax 1981;36:710
5 Bent JP 3rd, Kuhn FA. Diagnosis of allergic fungal sinusitis.
Otolaryngol Head Neck Surg 1994;111:5808
6 Katzenstein AL, Sale SR, Greenberger PA. Pathologic findings
in allergic aspergillus sinusitis. A newly recognized form of
sinusitis. Am J Surg Pathol 1983;7:43943
7 Schubert MS. Allergic fungal sinusitis: pathophysiology, diagnosis and management. Med Mycol 2009;47:32430
8 Manning SC, Holman M. Further evidence for allergic pathophysiology in allergic fungal sinusitis. Laryngoscope 1998;
108:148596
9 Loury MC, Leopold DA, Schaefer SD. Allergic aspergillus
sinusitis. Arch Otolaryngol Head Neck Surg 1993;119:10423
10 Cody DT 2nd, Neel HB 3rd, Ferreiro JA, Roberts GD. Allergic
fungal sinusitis: the Mayo Clinic experience. Laryngoscope
1994;104:10749
11 Kupferberg SB, Bent JP. Allergic fungal sinusitis in the pediatric
population. Arch Otolaryngol Head Neck Surg 1996;122:
13814
12 de Shazo RD, OBrien M, Chapin K, Soto-Aguilar M, Swain R,
Lyons M et al. Criteria for the diagnosis of sinus mycetoma.
J Allergy Clin Immunol 1997;99:47585
13 Wise SK, Rogers GA, Ghegan MD, Harvey RJ, Delgaudio JM,
Schlosser RJ. Radiologic staging system for allergic fungal rhinosinusitis (AFRS). Otolaryngol Head Neck Surg 2009;140:
73540
14 Schubert MS, Goetz DW. Evaluation and treatment of allergic
fungal sinusitis. I. Demographics and diagnosis. J Allergy Clin
Immunol 1998;102:38794
15 Rupa V, Jacob M, Mathews MS, Seshadri M. A prospective,
randomised, placebo-controlled trial of postoperative oral
steroid in allergic fungal sinusitis. Eur Arch Otorhinolaryngol
2010;267:2338
16 Katzenstein AL, Sale SR, Greenberger PA. Allergic aspergillus
sinusitis: a newly recognized form of sinusitis. J Allergy Clin
Immunol 1983;72:8993
17 Ferguson BJ. Eosinophilic mucin rhinosinusitis: a distinct clinicopathological entity. Laryngoscope 2000;110:799813
18 Sacks PL, Harvey RJ, Rimmer J, Gallagher RM, Sacks R.
Topical and systemic antifungal therapy for the symptomatic
treatment of chronic rhinosinusitis. Cochrane Database Syst
Rev 2011;(8):CD008263
19 Orlandi RR, Thibeault SL, Ferguson BJ. Microarray analysis of
allergic fungal sinusitis and eosinophilic mucin rhinosinusitis.
Otolaryngol Head Neck Surg 2007;136:70713
Address for correspondence:
Dr Maayan Gruber,
Department of Otolaryngolgy Head and Neck Surgery,
Lady Davis Carmel Medical Center,
7 Michal St, Haifa 34362, Israel
E-mail: maayan_gr@yahoo.com
Dr M Gruber takes responsibility for the integrity
of the content of the paper
Competing interests: None declared
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Pediatric Physiology 2007Document378 pagesPediatric Physiology 2007Andres Jeria Diaz100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Human Body PDFDocument9 pagesHuman Body PDFAnonymous W4MMefmCNo ratings yet
- Laryngeal Trauma 2Document61 pagesLaryngeal Trauma 2igor100% (1)
- Fundamentals of Pediatric Surgery Second EditionDocument893 pagesFundamentals of Pediatric Surgery Second EditionPatricia Beznea100% (3)
- Young Mania Rating Scale-MeasureDocument3 pagesYoung Mania Rating Scale-MeasureSelvaraj MadhivananNo ratings yet
- PAROTID GLAND NEOPLASM IMAGINGDocument107 pagesPAROTID GLAND NEOPLASM IMAGINGigorNo ratings yet
- MELANOMA: Risk Factors, Diagnosis, Staging and TreatmentDocument25 pagesMELANOMA: Risk Factors, Diagnosis, Staging and TreatmentFazaKhilwanAmnaNo ratings yet
- Orphan Lung DiseasesDocument623 pagesOrphan Lung Diseasescarmen84100% (1)
- Allergic Fungal Sinusitis PresentationDocument50 pagesAllergic Fungal Sinusitis PresentationdrdrsuryaprakashNo ratings yet
- Last Minute RevisionDocument108 pagesLast Minute RevisionRahul All83% (6)
- Practice Test Pediatric Nursing 100 ItemsDocument17 pagesPractice Test Pediatric Nursing 100 ItemsKarla FralalaNo ratings yet
- LIST OF HOSPITALS EMPANELLED UNDER ABS WITH SPECIALITIESDocument17 pagesLIST OF HOSPITALS EMPANELLED UNDER ABS WITH SPECIALITIESprem kumarNo ratings yet
- Pediatric Facial Fracture FINALDocument70 pagesPediatric Facial Fracture FINALigorNo ratings yet
- Cortical ERADocument37 pagesCortical ERAigorNo ratings yet
- Cogan SindromDocument4 pagesCogan SindromigorNo ratings yet
- Anosmia in COVID-19: Underlying Mechanisms and Assessment of An Olfactory Route To Brain InfectionDocument22 pagesAnosmia in COVID-19: Underlying Mechanisms and Assessment of An Olfactory Route To Brain InfectionigorNo ratings yet
- Fix Journal 1Document14 pagesFix Journal 1Lavenia Ellein MokiwangNo ratings yet
- Upper Airway and Digestive Tract Anatomy and PhysiologyDocument41 pagesUpper Airway and Digestive Tract Anatomy and PhysiologyigorNo ratings yet
- Fix Journal 1Document14 pagesFix Journal 1Lavenia Ellein MokiwangNo ratings yet
- Laryngeal TraumaDocument16 pagesLaryngeal TraumaigorNo ratings yet
- Ipi404109 PDFDocument5 pagesIpi404109 PDFigorNo ratings yet
- Laryngeal TraumaDocument16 pagesLaryngeal TraumaigorNo ratings yet
- Principles of ChemotherapyDocument31 pagesPrinciples of Chemotherapyigor100% (1)
- Responses of CD4Document10 pagesResponses of CD4igorNo ratings yet
- Allergic Rhinitis in Children Diagnosis and ManagementDocument18 pagesAllergic Rhinitis in Children Diagnosis and ManagementigorNo ratings yet
- SCITDocument12 pagesSCITigorNo ratings yet
- Chelladurai 2014Document5 pagesChelladurai 2014igorNo ratings yet
- Allergen ImmunotherapyDocument23 pagesAllergen ImmunotherapyigorNo ratings yet
- 10.1158@0008 5472.can 16 2345Document25 pages10.1158@0008 5472.can 16 2345igorNo ratings yet
- OtosclerosisDocument85 pagesOtosclerosisigorNo ratings yet
- Felder 2014Document15 pagesFelder 2014igorNo ratings yet
- Bar To Lazzi 2008Document7 pagesBar To Lazzi 2008igorNo ratings yet
- Pathophysiology of OMDocument18 pagesPathophysiology of OMigorNo ratings yet
- 2 - Rhinitis - Carmen RondonDocument35 pages2 - Rhinitis - Carmen RondonigorNo ratings yet
- ICD 9 Dan 10 THT-KLDocument30 pagesICD 9 Dan 10 THT-KLigorNo ratings yet
- Papadopoulos Et Al 2015 AllergyDocument21 pagesPapadopoulos Et Al 2015 AllergyigorNo ratings yet
- GA LEN/EAACI Pocket Guide For Allergen-Specific Immunotherapy For Allergic Rhinitis and AsthmaDocument6 pagesGA LEN/EAACI Pocket Guide For Allergen-Specific Immunotherapy For Allergic Rhinitis and AsthmaYohana VeronicaNo ratings yet
- C A Shinkwin Bon Secours GP Study Day 28 JANUARY, 2012Document23 pagesC A Shinkwin Bon Secours GP Study Day 28 JANUARY, 2012Nila HapsariNo ratings yet
- Congenital Muscular TorticollisDocument29 pagesCongenital Muscular Torticolliskashmala afzal100% (1)
- CNPASDocument3 pagesCNPASaneeshNo ratings yet
- Nurse Education in Practice: Book ReviewsDocument1 pageNurse Education in Practice: Book ReviewsUswatun HasanahNo ratings yet
- Mouth Breathing A Menace To Developing DentitionDocument7 pagesMouth Breathing A Menace To Developing DentitionLia CucoranuNo ratings yet
- Dokumen - Tips Jurnal-Traksi PDFDocument5 pagesDokumen - Tips Jurnal-Traksi PDFPrilii Ririie 'AnandaNo ratings yet
- Wvsu MC Org ChartDocument1 pageWvsu MC Org ChartquesterNo ratings yet
- Sex HDDocument2 pagesSex HDm29hereNo ratings yet
- Cardiac Conduction ExplainedDocument4 pagesCardiac Conduction ExplainedCharli VilcanNo ratings yet
- Topical Atropine Mydriasis RabbitDocument3 pagesTopical Atropine Mydriasis RabbitPadmanabha Gowda100% (1)
- Premature Rupture of MembranesDocument9 pagesPremature Rupture of MembranesYessica MelianyNo ratings yet
- AmalgamDocument3 pagesAmalgamMira AnggrianiNo ratings yet
- Melomed Pregnancy JournalDocument24 pagesMelomed Pregnancy JournalCelvin SohilaitNo ratings yet
- Assistant Professors: 327 2. C: (Vacancies Are Likely To Increase or Decrease)Document4 pagesAssistant Professors: 327 2. C: (Vacancies Are Likely To Increase or Decrease)JeshiNo ratings yet
- Apex LocatorsDocument6 pagesApex LocatorsbanupriyamdsNo ratings yet
- PPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPDocument4 pagesPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPPNor Ubudiah SetiNo ratings yet
- Folder Flexya Ita Pag AffiancateDocument2 pagesFolder Flexya Ita Pag AffiancateemikyNo ratings yet
- Medical PREFIXES and SUFIXESDocument52 pagesMedical PREFIXES and SUFIXESThirdz TylerNo ratings yet
- SDSC Eng ColourDocument2 pagesSDSC Eng ColourmerawatidyahsepitaNo ratings yet
- Tetric N-CollectionDocument8 pagesTetric N-CollectionRizky Ananda PutriNo ratings yet
- Burkitt's LymphomaDocument22 pagesBurkitt's LymphomaClementNo ratings yet
- DR - VM.Thomas - Consultant EmbryologistDocument2 pagesDR - VM.Thomas - Consultant EmbryologistdrthomasfertilitycenterNo ratings yet