Professional Documents
Culture Documents
Poertner 2005 Bioreactor Design Tissue Culture PDF
Poertner 2005 Bioreactor Design Tissue Culture PDF
Uploaded by
nurul9535Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Poertner 2005 Bioreactor Design Tissue Culture PDF
Poertner 2005 Bioreactor Design Tissue Culture PDF
Uploaded by
nurul9535Copyright:
Available Formats
JOURNAL OF BIOSCIENCE AND BIOENGINEERING
Vol. 100, No. 3, 235245. 2005
DOI: 10.1263/jbb.100.235
2005, The Society for Biotechnology, Japan
REVIEW
Bioreactor Design for Tissue Engineering
Ralf Prtner,1* Stephanie Nagel-Heyer,1 Christiane Goepfert,1
Peter Adamietz,2 and Norbert M. Meenen3
Technische Universitt Hamburg-Harburg, Bioprozess- und Bioverfahrenstechnik, Denickestr. 15, 21071 Hamburg,
Germany,1 Universittsklinikum Eppendorf, Institut fr Biochemie und Molekularbiologie II, Martinistr. 52,
20246 Hamburg, Germany,2 and Universittsklinikum Eppendorf, Unfall-, Hand- und
Wiederherstellungschirurgie, Martinistr. 52, 20246 Hamburg, Germany3
Received 7 March 2005/Accepted 31 May 2005
Bioreactor systems play an important role in tissue engineering, as they enable reproducible and
controlled changes in specific environmental factors. They can provide technical means to perform controlled studies aimed at understanding specific biological, chemical or physical effects.
Furthermore, bioreactors allow for a safe and reproducible production of tissue constructs. For
later clinical applications, the bioreactor system should be an advantageous method in terms of
low contamination risk, ease of handling and scalability. To date the goals and expectations of
bioreactor development have been fulfilled only to some extent, as bioreactor design in tissue engineering is very complex and still at an early stage of development. In this review we summarize
important aspects for bioreactor design and provide an overview on existing concepts. The generation of three dimensional cartilage-carrier constructs is described to demonstrate how the properties of engineered tissues can be improved significantly by combining biological and engineering
knowledge. In the future, a very intimate collaboration between engineers and biologists will lead
to an increased fundamental understanding of complex issues that can have an impact on tissue
formation in bioreactors.
[Key words: tissue engineering, bioreactor, design considerations, cartilage]
mensional (3D) biohybrid structure of a scaffold and cultured cells or tissue. Furthermore, non implantable tissue
structures can be applied as external support devices (e.g.,
an extracorporal liver support when a compatible donor organ is not readily available [4, 5]) or engineered tissues can
be used as in vitro physiological models for studying disease pathogenesis and developing new molecular therapeutics (e.g., drug screening [5, 6]).
The generation of 3D tissue substitutes in vitro requires
not only a biological model (e.g., an adequate source for
proliferable cells with appropriate biological functions, a
protocol for proliferating cells while maintaining the tissuespecific phenotype), but also the further development of new
culture strategies including bioreactor concepts (5, 7, 8).
Bioreactors are well established for the cultivation of microbes or mammalian cells under monitored and controlled
environmental and operational conditions (e.g., pH, temperature, oxygen tension, and nutrient supply) up to an industrial scale. However, as individual cells are mostly applied,
these concepts are inapplicable to 3D tissue constructs. Furthermore, each type of tissue construct (e.g., skin, bone,
blood vessel, and cartilage) will likely require an individualized bioreactor design (7). Therefore, tissue-specific bioreactors should be designed on the basis of comprehensive
understanding of biological and engineering aspects. Addi-
The loss and damage of tissues cause serious health problems (1). In the US, almost one-half of the costs for medical
treatments are spent on implant devices annually (2). Worldwide, 350 billion USD are expended for substitute of organs
(3). The substitution of tissues (such as bone or cartilage) or
joints with allograft materials includes the risk of infections
by viruses (such as HIV, hepatitis C) or a graft rejection. Artificial implants such as those used in knee or hip replacement, have limitations due to their limited lifespan, insufficient bonding to the bone, and allergic reactions caused by
material abrasion. New therapy concepts for practical medical applications are required. To this end, tissue engineered
substitutes generated in vitro could open new strategies for
the restoration of damaged tissues. The goal of tissue engineering can be defined as the development of cell-based
substitutes to restore, maintain or improve tissue function.
These substitutes should have organ-specific properties with
respect to biochemical activity, microstructure, mechanical
integrity and biostability (2). Cell-based concepts include the
(i) direct transplantation of isolated cells, (ii) implantation
of a bioactive scaffold for the stimulation of cell growth
within the original tissue and (iii) implantation of a three di* Corresponding author. e-mail: poertner@tuhh.de
phone: +49-40-42878-2886 fax: +49-40-42878-2909
235
236
PRTNER ET AL.
tionally, typical engineering aspects such as reliability, reproducibility, scalability and safety should be addressed (5, 8).
Several bioreactor systems have been developed and usually
the expectations are very high (5, 6). The question is, however, whether bioreactors can indeed fulfil these expectations.
In this review, key technical challenges are identified and
an overview of existing culture systems and bioreactors used
for tissue engineering is provided. These topics have been
addressed to some extent by several authors (4, 5, 716).
Therefore, they will be discussed only briefly. Particular
focus will be given to the interaction between biological and
engineering aspects. Using cartilage tissue formation as an
example, it will be shown how an increased fundamental
understanding of biological, biochemical, and engineering
aspects can significantly improve the properties of 3D tissue
constructs.
IMPORTANT ASPECTS FOR
BIOREACTOR DESIGN
With respect to tissue engineering, bioreactors are used
for different purposes such as (i) cell proliferation on a
small scale (e.g., for individual patients) and on a large scale
(e.g., for allogenic therapy concepts), (ii) generation of 3D
tissue constructs from isolated and proliferated cells in vitro
and (iii) direct organ support devices (15). These bioreactors should enable the control of environmental conditions
such as oxygen tension, pH, temperature, and shear stress
and allow aseptic operation (e.g., feeding and sampling).
Furthermore, a bioreactor system should allow for automated processing steps. This is essential not only for controlled, reproducible, statistically relevant basic studies but
also for the future routine manufacturing of tissues for clinical application (5, 17). Besides these global requirements,
specific key criteria for 3D tissue constructs based on cells
and scaffolds have to be met, including the proliferation of
cells, seeding of cells on macroporous scaffolds, nutrient
(particularly oxygen) supply within the resulting tissue, and
mechanical stimulation of the developing tissues (5).
Proliferation of cells is the first step in establishing a tissue culture. Usually, only a small number of cells can be obtained from a biopsy specimen and expansion up to several
orders of magnitude is required. The proliferation of cells is
quite often accompanied by the dedifferentiation of cells.
For example, proliferating chondrocytes show a decreased
expression level of collagen type II and an increased expression level of collagen type I (18, 19). Small culture dishes
(e.g., petri dishes, 12-well plates, and T-flasks) are generally
used for cell expansion. As these devices allow only an increase in cell number by a factor of approximately 10, several subcultivations are required. These are considered as a
major cause for the dedifferentiation of cells. Recent studies
have shown that microcarrier cultures performed in wellmixed bioreactor systems can significantly improve cell expansion (2022).
The cell seeding of scaffolds is an important step in establishing a 3D culture in a macroporous scaffold. Not only
seeding at high cell densities, but also a homogenious distribution of cells within the scaffold is essential. High initial
J. BIOSCI. BIOENG.,
cell densities have been associated with an enhanced tissue
formation including cartilage matrix production, bone mineralization and cardiac tissue structure formation (2325).
On the other hand, an inhomogeneous distribution of cells
within the scaffold can significantly affect the tissue properties. Several techniques for cell seeding were discussed by
Martin et al. (5).
Critical issues of all bioreactor concepts involve mass
transfer problems (e.g., oxygen and nutrient supply, and removal of toxic metabolites). The size of most engineered
tissues is limited as they do not have their own blood system
and the cells are only supplied by diffusion (6, 26). Oxygen
supply is particularly critical, as only cell layers of 100200
m can be supplied by diffusion (27). However, as tissue
constructs should have larger dimensions, mass-transfer limitations represent one of the greatest engineering challenges.
Various studies showed that mechanical stimulation (e.g.,
mechanical compression, hydrodynamic pressure, and fluid
flow), which are important modulators of cell physiology,
can have a positive impact on tissue formation (28), particularly in the context of musculoskeletal tissue engineering,
cartilage formation, and cardiovascular tissues among others
(11, 2934). Despite accumulating evidence that mechanical stimulation can improve the properties of engineered tissues, only little is known about specific mechanical forces
or the ranges of application (i.e., magnitude, frequency, continuous or intermittent, and duty cycle [5, 9]). Further studies of these factors have to be coupled with quantitative and
computational analyses of physical forces experienced by
cells and changes in mass transport induced by the method
used.
Bioreactors allow for different process strategies including the batch, fed-batch or continuous cultivation. In particular, continuous perfusion enables cultivation under constant
and controlled environmental conditions (3538). Martin et
al. (5) summarized some of the effects of direct perfusion
on tissue-specific properties such as growth, differentiation
and mineralized matrix deposition by bone cells, proliferation of human oral keratinocytes, rates of albumin synthesis
by hepatocytes, expression of cardiac-specific markers by
cardiomyocytes, and GAG synthesis and accumulation by
chondrocytes. On the other hand, a bioreactor system becomes more complex as additional features such as feeding
pumps, vessels for fresh and spent medium, and control
strategies are required (Fig. 1), particularly in the case of
mechanical stimulation. The bioreactor system has to be integrated into the entire cultivation scheme including biopsy,
proliferation, cell seeding, tissue formation and delivery to
the site of application (e.g., hospital). In many cases, the
bioreactor itself is only used for tissue formation. However,
for a wholistic approach from biopsy to the implantation of
tissue, the intire procedure should be coordinated to decrease the number of steps, risk of contamination, and labor
costs among others. This is particularly important with respect to the manufacture of engineered tissue constructs for
clinical applications, in which good manufacturing practice
(GMP) requirements have to be met (7, 8).
VOL. 100, 2005
BIOREACTOR DESIGN FOR TISSUE ENGINEERING
237
FIG. 1. Set-up of flow-chamber-bioreactor system consisting of flow chamber with inserts for tissue constructs, conditioning vessel, peristaltic
pump, humidifier, exhaust flask, and medium exchange bottle.
CULTURE SYSTEMS AND BIOREACTORS
USED IN TISSUE ENGINEERING
The engineering of 3D tissue constructs include cell maintenance, proliferation and tissue formation. An overview of
culture systems and bioreactors used for these purposes is
shown in Fig. 2. Cell maintenance and proliferation is usually performed in culture systems developed for the monolayer culture of adherent cells (T-flasks, petri dishes, multi
well plates). These systems enable sterile handling procedures and are easy to use, disposable and low-cost (39).
Moreover, they require individual handling as for example
in medium exchange and cell seeding; their usefulness is
limited when large quantities are required (7). This can be
overcome to some extent using sophisticated robotics (5).
Furthermore, controlling environmental parameters including pH, pO2, and temperature is generally impossible. A further drawback is the limited increase in cell number (approximately 1020 times during cultivation). The generation
of a large number of cells requires several enzymatic subcultivation steps accompanied by an increase in passage
number and cell dedifferentiation.
In recent studies, small well-mixed bioreactors (e.g., shake
flasks, stirred vessels, and super spinner) have been suggested for cell proliferation, in which the cells are grown on
microcarriers (2022). These systems were used in the cultivation of encapsulated cells (18, 19) or neural stem cells in
single-cell suspension culture (40).
In fixed bed and fluidized bed bioreactors, cells are immobilized in macroporous carriers. The carriers are arranged in
a column either packed (fixed bed) or floating (fluidized
bed). The column is permanently perfused with a conditioned medium from a medium reservoir, mostly in a circulation loop. These types of reactor are very efficient for the
long-term cultivation of mammalian cells for the production
of biopharmaceuticals (e.g., monoclonal antibodies, recom-
binant drugs including tPA, and EPO) or recombinant retroviruses for gene therapy (4143). With respect to tissue engineering they have been investigated for several applications including the cultivation of liver cells as an extracorporal liver device (4, 10, 37), proliferation of stem cells
(4446), cultivation of cardiovascular cells (11) and cartilage cells (9). As most of the scaffolds have large, interconnected pores, during seeding, cells are distributed quite
uniformly. During cultivation, medium flow through a construct enhances the mass transfer of substrates, particularly
oxygen to immobilized cells when interconnected cell free
pores are available.
In membrane bioreactors including hollow-fiber reactors
(47), the miniPerm system (48) or the tecnomouse (49),
cells are cultivated at tissuelike densities in a compartment,
which contains one or several types of membrane for nutrient and oxygen supply and removal of toxic metabolites.
Hollow-fiber systems are widely used in the production of
biopharmaceuticals including monoclonal antibodies. Several
examples of modified membrane bioreactors exist for the
3D culture of tissue cells including hepatocytes (4, 5054),
skin cells (55) or other human cells (49, 56).
Most of the culture systems and bioreactors discussed so
far were first developed for the cultivation of mammalian
cells and adapted to the engineering of 3D tissue constructs.
However, besides some exceptions, they can hardly be used
in the generation of implantable tissue constructs. Each type
of tissue intended for implantation (e.g., skin, heart valve,
blood vessel, and cartilage) requires a different geometric
structure and a specific bioreactor design, particularly when
mechanical stimulation has to be provided. Finally, engineered constructs have to be transferred from the culture
system to the patient after cultivation. Therefore, several tissue-specific culture systems and bioreactors have been suggested.
One of the most prominent culture systems is the rotat-
238
PRTNER ET AL.
J. BIOSCI. BIOENG.,
FIG. 2. Cell culture systems used in tissue engineering.
ing-wall vessel (23), in which a construct remains in a state
of free-fall through the medium with a low shear stress and
a high mass transfer rate. This system has a wide range of
practical applications (5, 7). A multipurpose culture system
was introduced by Minuth et al. (35) for perfusion cultures
under organotypic conditions. Several tissue carriers can be
placed inside a perfusion container. Depending on the type
of tissue-specific cell supports can be selected. A perfused
flow-chamber bioreactor with a new concept for aeration
has been introduced recently (20), in which tissue-specific
inserts for various types of tissue (e.g., cartilage, skin, and
bone) can be applied.
Besides these examples of multipurpose bioreactors, numerous of tissue-specific culture systems have been suggested. These are well reviewed with respect to specific tissues (5, 6, 811, 14, 15, 26, 50, 5759). Most of them are
custom-made; only very few have been commercialized.
MODELLING OF BIOREACTOR SYSTEMS
FOR TISSUE ENGINEERING
The appropriate molecular and macroscopic architecture
of 3D tissue constructs is essential to producing a phenotypically appropriate tissue (6). However, in many cases this is
not realized. The solution may lie in providing appropriate
physiological conditions during cultivation. In many cases,
the culture systems and bioreactors were not optimized in
this respect. Parameters such as perfusion rate, flow conditions, shear stress, and compression magnitude were varied,
quite often by a trial-and-error approach. Furthermore, different conditions have to be examined accurately with regard to their effect. For example, hydrostatic pressure applied during cartilage culture can lead to an improved mass
transfer of small and large molecules into the cartilage matrix, but can also induce a mechanical stimulation of embedded cells. These two effects have to be examined separately.
Particularly, when if forces (e.g., hydrostatic pressure, shear
stress induced by perfusion, shear stress or gliding forces
induced by mechanical impact, and pulsation flow) are applied, the exact local conditions experienced by the cells
have to be determined. Therefore, experimental studies
should be supported by simulation methods such as the
computational fluid dynamics (CFD) or finite-element approach. Several examples underline the potential of an integrated study of mechanical and biomechanical factors that
control the functional development of tissue engineered constructs (6066). This approach will significantly improve
bioreactor design in the near future.
As an attempt to evaluate and compare different tissue
engineering reactors, Omasa et al. (67) applied the analytic
hierarchy process (AHP). For evaluating a reactor for a bioartificial liver (BAL) support system, five criteria were identified (namely, safety, scalability, cell growth environment,
mimicking native liver functions and handling). On the basis of these criteria, six different types of BAL systems were
successfully ranked using AHP. The process is a valuable
tool for decision making in tissue engineering, not only for
BAL systems but for tissue engineering reactors in general.
INTERACTION BETWEEN BIOLOGICAL AND
ENGINEERING ASPECTS IN GENERATION
OF ARTIFICIAL CARTILAGE
The following considerations are intended to demonstrate
how the interdisciplinary application of biological and engineering knowledge can significantly improve the properties
of tissue engineered 3D cartilage constructs. Severe health
problems can arise from a lack or damage of hyaline cartilage in joints, particularly in knee joints (68). The methods of
tissue engineering enable the generation of cartilage tissue
in vitro and provide new strategies to restoring damaged
cartilage (9, 36, 58, 69). Whereas many approaches to generating tissue-engineered cartilage are based on either alginate encapsulation or the use of bioresorbable scaffolds (9,
VOL. 100, 2005
19, 58, 59, 69, 70), recently, a new concept involving the
use of a bone substitute carrier covered with a layer of
tissue-engineered cartilage without scaffolds has been presented (17). This concept consists of four steps: (i) explanted articular chondrocytes are expanded in a monolayer
culture and then seeded on a solid carrier to form a primer
layer; (ii) simultaneously, chondrocytes are suspended in
alginate gel and cultivated for two weeks to allow the formation of a pericellular matrix; (iii) redifferentiated chondrocytes are then eluted out of the alginate gel and sedimented on the primer layer; (iv) the biphasic constructs are
further cultivated for three weeks. Below, mainly different
aspects of step iv are addressed. A similar concept was suggested by Waldman et al. (71).
A critical parameter during the cultivation of cartilage
tissue is oxygen supply. The effect of oxygen during the in
vitro cultivation of chondrocytes is poorly understood, and
therefore it is presently a controversial issue (72). In several
studies, chondrocytes were immobilized in alginate beads
and cultivated under different oxygen concentrations in the
gas phase (for review see Ref. 72). ODriscoll et al. (73)
observed a limited collagen type II production at very high
(90% O2) and very low (15% O2) oxygen concentrations.
Domm et al. (19) showed a stimulatory effect of a decreased
oxygen tension (5% O2) on matrix production. In a recent
study of Malda et al. (18), the pellets of chondrocytes were
suspended in a stirred bioreactor under different oxygen
concentrations. They observed an increased production of
glycosaminoglycan at 5% and 1% O2 (v/v) in comparison
with aeration at 21% O2 (air). The increased glycosaminoglycan production is accompanied by a decrease in collagen type I level. On the other hand, several studies of
chondrocytes embedded in a 3D matrix or a scaffold have
demonstrated an enhanced matrix formation, particularly
proteoglycan synthesis under more aerobic conditions (74,
75).
The main difference between the applied methodologies
(alginate and pellet culture vs. cartilage generation in 3D
scaffolds) can be observed in oxygen gradients in the vicinity and within the formed cartilage (38, 76). In the case of
alginate and pellet culture, oxygen gradients at the surface
of constructs can be neglected, and only oxygen limitations
within the constructs are likely. For the cultivation of 3D
scaffolds, even more significant oxygen gradients within the
formed matrix are expected.
Another attempt to improve tissue-engineered cartilage is
the application of mechanical force during the cultivation to
produce a phenotypically appropriate tissue. Four main types
of force are currently used in cartilage cultivation: hydrostatic pressure, direct compression, and high- and low-shear
fluid environments. All these forces have been integrated
into culturing devices used as bioreactors for articular cartilage. The individual effects have been reviewed by Darling
and Athansiou (9).
Our work started from an engineering view point, that is,
we invastigated the oxygen transport in culture systems for
the generation of cartilage pellets and within the pellet itself
theoretically. Two culture strategies were modelled, a static
culture system with the supply of oxygen through the medium by diffusion and a perfused culture system with an
BIOREACTOR DESIGN FOR TISSUE ENGINEERING
239
oxygen-enriched medium. For a static culture system, the
oxygen supply of a cartilage pellet from the medium, which
is not flowing (static medium layer, Fig. 3A) was calculated
with the following assumptions: (i) the medium is in contact
with the atmosphere via a gas-liquid interface and the oxygen concentration at the surface is in equilibrium with the
atmosphere. (ii) The oxygen concentration cR in the static
medium layer can be described by one-dimensional diffusion (D= diffusion coefficient in the medium).
cR
2cR
(1)
---------- = D -----------x2
t
(iii) The oxygen concentration cP within a pellet can be described by Eq. 2.
X qmax
cP
dcP
d2cP
= Deff ----------(2)
--------- ---------------- ------------------V
dt
ks + cP
dx2
where X is the cell density, qmax the maximal cell-specific
oxygen uptake rate, V the volume of the cartilage and kS the
Monod constant. (iv) The mass transfer of oxygen from the
medium to the pellet is only by diffusion. At the interface,
oxygen concentration and slope are identical on both sides.
At the pellet wall, the slope of oxygen concentration is zero.
Figure 3 shows the calculated oxygen concentration profile
as a function of length scale and time with the following parameters: a cell density of 2 106 cells per pellet, a maximal
cell specific oxygen uptake rate of qmax = 1013 mol cell1 h1,
kS = 1075 105 mol l1 and Deff = 2.16 105 cm2 s1, which is
80% of the diffusion coefficient in the medium (38). As
shown in Fig. 3A, oxygen concentration in the vicinity of
the pellet decreases very rapidly to zero within a very short
time. This effect is mainly due to the very low diffusive
transport of oxygen through the boundary layer between the
cartilage pellet and the medium.
Alternatively, a perfused system was modelled, in which
an oxygen enriched medium flows over the cartilage and the
thickness of the boundary layer over the cartilage should be
significantly decreased (Fig. 3B). The oxygen concentration
cm in the flowing medium as a function of time and length
xm can be described by Eq. 3.
dcm
d2cm
4
= D -----------(3)
----------- + u --------------- (c0 cm)
dt
dxm2
dP
where U is the flow velocity, dP the pellet diameter, and c0
the oxygen concentration at xm = 0. The results of these simulations are summarised in Fig. 3B for a flow rate of 3
ml min1. These calculations show that the mass transfer
resistance in the boundary layer between the cartilage and
the medium can be significantly decreased, but still oxygen
concentration within the pellet decreases very rapidly.
For both systems, a severe oxygen limitation has to be
expected within the tissue matrix. The main reason for this
limitation is the very low rate of transport by diffusion.
Similar conclusions have been drawn elsewhere (38, 76). A
flow with an enriched medium, as in the perfused culture
system, can overcome this problem only to some extent by
decreasing the thckness of the boundary layer between the
tissue matrix and the medium. These findings lead to the
question of whether it is possible to predict the properties of
cartilage generated in these bioreactor systems on the basis
240
PRTNER ET AL.
J. BIOSCI. BIOENG.,
FIG. 3. Modelling of oxygen profiles within tissue-engineered cartilage. (A) Calculated oxygen profile in static culture system for cultivation
of artificial cartilage pellets. (B) Calculated oxygen profile in perfusion culture system for cultivation of artificial cartilage pellets.
of the above conclusions.
This will be addressed below by comparing experimental
results from different cultivation systems. The methods will
be introduced only briefly. For details, see Ref. 17. Threedimensional cartilage-carrier constructs were produced according to the protocol described above from chondrocytes
of an adult mini pig. The final step of this protocol was performed either in bioreactors (in a flow-chamber or under intermittent hydrostatic pressure) or in 12-well plates as the
control (Fig. 4). The flow-chamber bioreactor was specially
designed for the generation of three-dimensional cartilagecarrier constructs. A specific feature of the flow chamber is
a very thin medium layer for improved oxygen supply and a
counter current flow of the medium and gas (20). Another
bioreactor system was designed in which an intermittent hydrostatic pressure is applied during the cultivation. It enables the cultivation of seven cartilage-carrier constructs in
parallel. The main results of the experiments are summarized in Table 1.
Experiments at different oxygen concentrations (21% and
10% v/v O2) were performed in 12-well plates as the control
and the constructs were compared qualitatively and quantitatively. The appearance of the cartilage obtained under decreased oxygen tension seemed to be closer to the native
cartilage with respect to the shape of cells, distribution of
cells within the matrix, and smoothness of the surface
among others. The thickness of the cartilage formed by free
swelling was always in the same range as that of the native
cartilage (approximately 1 mm). For both oxygen concentrations the content of glycosaminoglycan (GAG) was similar, but still significantly lower than that in the native cartilage (data not shown). Qualitatively, the most stable attachment of the cartilage on top of the carrier was found for 10%
O2 (v/v). Furthermore, the cultivated cartilage contained a
large content of collagen type II (data not shown). From
these observations, a lower oxygen concentration in the gas
phase is recommended.
Experiments in the flow-chamber bioreactor showed a
significantly higher matrix thickness but a lower content of
GAG then cultures in 12-well plates as the control. The appearance of the cartilage obtained in the bioreactor seemed
to be closer to the native cartilage with respect to the shape
of cells, distribution of cells within the matrix, and smoothness of the surface among others. The cartilage obtained
from 12-well plates showed an inhomogeneous distribution
of cells, a more uneven surface and holes within the matrix.
Another important requirement for a successful implantation is the consistency of the cartilage. In the case of bioreactor cultures, the compaction of the cartilage and the attachment between the cartilage and carrier were very good,
indicating that the construct is appropriate for implantation. In contrast, the cartilage-carrier constructs cultivated
in 12-well plates were soft and the attachment between the
cartilage and carrier was not sufficient. In this case, the cartilage tended to slip off the carrier with only a slight mechanical impact. Furthermore, the cultivated cartilage should
VOL. 100, 2005
BIOREACTOR DESIGN FOR TISSUE ENGINEERING
241
FIG. 4. Culture systems used for generation of three-dimensional cartilage carrier constructs.
contain a significant content of collagen type II. This was
confirmed qualitatively by immunohistological analysis.
In the third set of experiments cartilage-carrier constructs
were cultivated in a bioreactor, in which intermittent hydrostatic pressure was applied during the last week of cultivation (total time, 5 weeks). A total pressure of 3 105 Pa was
applied eight times per hour for 2.5 min during this week.
Constructs cultivated under an intermittent hydrostatic pressure load and a decreased oxygen tension (10% O2 v/v)
showed a significantly higher matrix thickness and a higher
GAG content than those cultivated in 12-well plates as the
control (Table 1). The compaction of matrix as well as attachment between the cartilage and carrier was evaluated
qualitatively and found to be much better in the bioreactor
cultures with intermittent hydrostatic pressure loading than
in constructs cultivated without loading in 12-well plates.
In a small animal trial, constructs were implanted into
mini pigs. One pig recieved constructs cultivated with pressure loading and at 21% O2 v/v and anotther pig received
constructs cutlivated with pressure loading and at 10% O2
v/v. After surgery, none of the animals showed restrictions
in movement. In both pigs, the cultivated cartilage integrated into the surrounding native cartilage without the formation of gaps. The immunohistological analysis revealed
that explants cultivated at 10% O2 v/v showed a higher collagen type II content than those cultivated at 21% v/v O2
(Fig. 5). The explants cultivated at 10% O2 v/v indicated a
hyaline like cartilage, whereas those cultivated at 21% O2
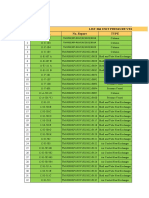
TABLE 1. Biochemical data of cartilage-carrier constructs cultivated in 12-well plates, in flow-chamber bioreactor,
under intermittent hydrostatic pressure, and for native cartilage (glycosaminoglycane, GAG)
Matrix
GAG
thickness
(g)
(mm)
12-well plate
4
1.2 0.7
162 103.5
12-well plate
4
1.3 0.6
155.9 74.4
Flow-chamber bioreactor
6
1.6 0.2
142.7 9.7
12-well plate (control)
6
1.1 0.1
238.9 22.1
Static culture under intermittent hydrostatic pressure
3
1.1 0.7
466.53 7.1
12-well plate (control)
3
0.7 0.0
268.8 74
Native cartilage
1.0 0.0
1680.1 211.8
The cultivation principle consists of the following steps (17): (i) chondrocytes are isolated from the articular cartilage of an adult mini-pig,
expanded in a monolayer culture and then seeded on a solid ceramic carrier (diameter 4.5 mm) to form a primer layer; (ii) simultaneously, chondrocytes are suspended in alginate gel and cultivated for two weeks to allow the formation of a pericellular matrix; (iii) redifferentiated chondrocytes
are then recovered from the alginate gel and sedimented on the primer layer; (iv) the biphasic constructs are further cultivated for three weeks to
allow free-swelling of the cartilage matrix. This step was performed either in a 12-well plate, a flow-chamber bioreactor (flow rate, 0.5 ml/min) or
under intermittent hydrostatic pressure (total pressure of 3 105 Pa, 82.5 min per hour, applied hourly during the last week of cultivation). Three
sets of experiments were performed: (i) cultivation of cells in passage 4 in 12-well plates at 21% and 10% oxygen tensions in the headspace;
(ii) cultivation of cells in passage 6 in a flow-chamber bioreactor and in 12-well plates (control) at 21% oxygen tension; (iii) cultivation of cells in
passage 3 in a bioreactor under intermittent hydrostatic pressure and in 12-well plates (control) at 10 % oxygen tension. Native cartilage from an
adult mini-pig; diameter, 4.5 mm; average of five samples.
Culture system
Passage
no.
O2-tension in
the gas phase
(%)
21
10
21
21
10
10
242
J. BIOSCI. BIOENG.,
PRTNER ET AL.
further investigations showed that due to the very low mass
transfer between the static culture medium and the gas
phase, oxygen concentration in the culture medium did not
increase during intervals with a higher pressure. Therefore,
other factors that explain the significantly improved matrix
properties of constructs cultivated under intermittend hydrostatic pressure compared with static cultures in 12-well
plates should be identified. Probably, the mechanical stimulation of chondrocytes is the main effect. However, to clarify this, further biochemical and cell biological studies are
required to determine, which cell biological effects are responsible for the observed phenomena.
CONCLUSIONS
FIG. 5. Images of immunohistological staining for collagen type
II of implanted cartilage-carrier construct (mini-pig) after explanation
and decalcification of carrier. Cartilage-carrier constructs were cultivated prior to implantation under loading with intermittent hydrostatic
pressure in a bioreactor aerated with 21% O2 (a, b) and 10% O2 (c, d).
Time of observation for the animals: 8 weeks. Bars indicate 500 m. 1,
Native cartilage; 2, newly formed cartilage; 3, bone; 4, extracted carrier after decalcification. The protocol for the generation of cartilagecarrier constructs is described in Table 1.
v/v showed unsatisfactory results.
The above considerations underline the idea that engineering knowledge can help improve cultivation systems
and applied strategies for tissue engineering. On the other
hand, it becomes obvious, that both engineering and fundamental studies on cell biology are required to further clarify
the observed effects. The theoretical simulations indicate
that even under ideal conditions (no mass transfer limitation
in the fluid phase) a severe oxygen limitation within the engineered tissue should be expected. If oxygen supply would
be the limiting factor during cartilage formation, a bioreactor system (flow chamber) with an improved oxygen supply
should lead to a better quality of the engineered cartilage.
On the other hand, lower oxygen concentrations in the gas
phase seem to improve some matrix properties. From the
results discussed above, these discrepancies can be solved
only to some extent. With respect to important biochemical
properties, particularly the content of GAG, the constructs
from the flow chamber bioreactor showed significantly lower
values than those from the 12-well plates, probably due to a
higher, detrimental oxygen concentration in the matrix. On
the other hand, other matrix properties, particularly the attachment between the cartilage and carrier was better for
constructs from the flow chamber than for those from 12well plates. This can be due to a better oxygen supply within
the matrix close to the surface of the carrier.
The best results were obtained from constructs cultivated
under intermittent hydrostatic pressure and a decreased oxygen concentration in the gas phase. Initially, this phenomenon is difficult to understand. As the partial pressure of oxygen in the gas phase depends on total pressure, a higher
pressure should even increase oxygen concentration significantly, leading to even worse matrix properties. However,
Bioreactors for the generation of 3D tissue constructs can
provide a better process control by taking into account different demands of cells during cultivation. Furthermore,
they can provide the technical means to perform controlled
studies aimed at understanding specific biological, chemical
or physical effects. Moreover, bioreactors enable a safe and
reproducible production of tissue constructs. An overall comparison of different culture methods shows clearly the advantages of bioreactor culture. Not only can the properties
of cultivated 3D tissue constructs be improved, aspects such
as safety of operation argue for the use of bioreactor systems. Furthermore, the bioreactor can be used to study
effects such as shear flow and/or hydrostatic pressure on the
generation of tissues. For future clinical applications, the
bioreactor system should be an advantageous method in
terms of low contamination risk, ease of handling and scalability.
To date the goals and expectations of bioreactor development have been fulfilled only to some extent, as bioreactor
design in tissue engineering is very complex and still at an
early stage of development. In the future, a very intimate
collaboration between engineers and biologists will lead to
an increased fundamental understanding of complex issues
that can have an impact on tissue formation in bioreactors.
On one hand, devices are required with a well-described
microenvironment of cells for fundamental studies. On the
other hand, a transition from a laboratory scale to an industrial scale will require a high adaptability of specialized
bioreactors in a standardized production process. These advances will aid in ensuring that tissue engineering fulfil the
expectations for revolutionizing medical care.
ACKNOWLEDGMENTS
We would like to thank Drs. Klaus Baumbach, Frank Feyerabend,
Jan-Philipp Petersen and Jens Schrder for scientific input and
help in animal trials, Sven Cammerer and Katja Schmid for modelling the cartilage reactor as well as Katharina Braun, Ditte
Siemesgelss and Richard Getto for technical support. The financial support of Biomet Deutschland GmbH, Berlin under the
BMBF grant no. 03N4012 and the city of Hamburg within the
Qualtittsoffensive Tissue Engineering is gratefully acknowledged.
VOL. 100, 2005
BIOREACTOR DESIGN FOR TISSUE ENGINEERING
NOMENCLATURE
c0 : oxygen concentration in the flowing medium layer
at xm = 0 m, mol l1
cm : oxygen concentration in flowing medium layer,
mol l1
cR : oxygen concentration in static medium layer,
mol l1
cP : oxygen concentration in cartilage matrix, mol l1
D : diffusion coefficient in medium, m2 s1
Deff : diffusion coefficient in cartilage matrix, m2 s1
dP : pellet diameter, m
kS : Monod constant, mol l1
qmax : maximal cell-specific oxygen uptake rate,
mol cell1 h1
u : flow velocity, m2 s1
V : volume of cartilage, l
X : cell density, cells l1
x : length, m
xm : length in medium, m
REFERENCES
1. Langer, R.: Tissue engineering. Mol. Ther., 1, 1215 (2000).
2. Langer, R. and Vacanti, J. P.: Tissue engineering. Science,
260, 920926 (1993).
3. Lysaght, M. J. and Loughlin, J. A.: Demographic scope and
economic magnitude of contemporary organ replacement therapies. ASAIO J., 46, 515521 (2000).
4. Chamuleau, R. A.: Artificial liver support in the third millennium. Artif. Cells Blood Substit. Immobil. Biotechnol., 31,
117126 (2003).
5. Martin, I., Wendt, D., and Heberer, M.: The role of bioreactors in tissue engineering. Trends Biotechnol., 22, 8086
(2004).
6. Griffith, L. G. and Naughton, G.: Tissue engineering current challenges and expanding opportunities. Science, 295,
10091014 (2002).
7. Ratcliffe, A. and Niklason, L. E.: Bioreactors and bioprocessing for tissue engineering. Ann. N.Y. Acad. Sci., 961, 210
215 (2002).
8. Naughton, G. K.: From lab bench to market: critical issues
in tissue engineering. Ann. N.Y. Acad. Sci., 961, 372385
(2002).
9. Darling, E. M. and Athanasiou, K. A.: Articular cartilage
bioprocesses and bioreactors. Tissue Eng., 9, 926 (2003).
10. Allen, J. W. and Bhatia, S. N.: Improving the next generation of bioartificial liver devices. Semin. Cell Dev. Biol., 13,
447454 (2002).
11. Barron, V., Lyons, E., Stenson-Cox, C., McHugh, P. E.,
and Pandit, A.: Bioreactors for cardiovascular cell and tissue
growth: a review. Ann. Biomed. Eng., 31, 10171030 (2003).
12. Godbey, W. T. and Atala, A.: In vitro systems for tissue engineering. Ann. N.Y. Acad. Sci., 961, 1026 (2002).
13. Morsi, Y. S., Birchall, I. E., and Rosenfeldt, F. L.: Artificial
aortic valves: an overview. Int. J. Artif. Org., 27, 445451
(2004).
14. Park, K. D., Kwon, I. K., and Kim, Y. H.: Tissue engineering of urinary organs. Yonsei Med. J., 41, 780788 (2000).
15. Shachar, M. and Cohen, S.: Cardiac tissue engineering, ex
vivo: design principles in biomaterials and bioreactors. Heart
Fail Rev., 8, 271276 (2003).
16. Vunjak-Novakovic, G.: The fundamentals of tissue engineering: scaffolds and bioreactors. Novartis Found Symp., 249,
3446 (2003).
243
17. Nagel-Heyer, S., Goepfert, Ch., Morlock, M. M., and
Prtner, R.: Relationship between gross morphological and
biochemical data of tissue engineered cartilage-carrier-constructs. Biotechnol. Lett., 27, 187192 (2005).
18. Malda, J., van Blitterswijk, C. A., van Geffen, M., Martens,
D. E., Tramper, J., and Riesle, J.: Low oxygen tension stimulates redifferentiation of dedifferentiated adult human nasal
chondrocytes. Osteoarthritis Cartilage, 12, 306313 (2004).
19. Domm, C., Schnke, M., Christesen, K., and Kurz, B.:
Redifferentiation of dedifferentiated bovine articular chondrocytes in alginate culture under low oxygen tension. Osteoarthritis Cartilage, 10, 1322 (2002).
20. Nagel-Heyer, S., Leist, Ch., Lnse, S., Goepfert, C., and
Prtner, R.: From biopsy to cartilage-carrier constructs by
using microcarrier cultures as sub-process, p. 139. In Proceedings of 19th ESACT meeting. European Society for Animal Cell Technology (ESACT), Harrogate, UK (2005).
21. Malda, J., van den Brink, P., Meeuwse, P., Grojec, M.,
Martens, D. E., Tramper, J., Riesle, J., and van Blitterswijk,
C. A.: Effect of oxygen tension on adult articular chondrocytes in microcarrier bioreactor culture. Tissue Eng., 10, 987
994 (2004).
22. Bardouille, C., Lehmann, J., Heimann, P., and Jockusch,
H.: Growth and differentiation of permanent and secondary
mouse myogenic cell lines on microcarriers. Appl. Microbiol.
Biotechnol., 55, 556562 (2001).
23. Freed, L. E., Langer, R., Martin, I., Pellis, N. R., and
Vunjak-Novakovic, G.: Tissue engineering of cartilage in
space. Proc. Natl. Acad. Sci. USA, 94, 1388513890 (1997).
24. Holy, C. E., Shoichet, M. S., and Davies, J. E.: Engineering
three-dimensional bone tissue in vitro using biodegradable
scaffolds: investigating initial cell-seeding density and culture
period. J. Biomed. Mater. Res., 51, 376382 (2000).
25. Carrier, R. L., Papadaki, M., Rupnick, M., Schoen, F. J.,
Bursac, N., Langer, R., Freed, L. E., and Vunjak-Novakovic,
G.: Cardiac tissue engineering: cell seeding, cultivation parameters, and tissue construct characterisation. Biotechnol.
Bioeng., 64, 580589 (1999).
26. Kannan, R. Y., Salacinski, H. J., Sales, K., Butler, P., and
Seifalian, A. M.: The roles of tissue engineering and vascularisation in the development of micro-vascular networks: a
review. Biomaterials, 26, 18571875 (2005).
27. Fassnacht, D. and Prtner, R.: Experimental and theoretical
considerations on oxygen supply for animal cell growth in
fixed bed reactors. J. Biotechnol., 72, 169184 (1999).
28. Butler, D. L., Goldstein, S. A., and Guilak, F.: Functional
tissue engineering: the role of biomechanics. J. Biomech. Eng.,
122, 570575 (2000).
29. Carver, S. E. and Heath, C. A.: Increasing extracellular matrix production in regenerating cartilage with intermittent physiological pressure. Biotechnol. Bioeng., 62, 166174 (1999).
30. Carver, S. E. and Heath, C. A.: Influence of intermittent
pressure, fluid flow, and mixing in the regenerative properties
of articular chondrocytes. Biotechnol. Bioeng., 65, 274281
(1999).
31. Hall, A. C., Urban, J. P. G., and Gehl, K. A.: The effects of
hydrostatic pressure on matrix synthesis in articular cartilage.
J. Othop. Res., 9, 110 (1991).
32. Jagodzinski, M., Cebotari, S., Tudorache, I., Zeichen, J.,
Hankemeier, S., Krettek, C., van Griensven, M., and
Mertsching, H.: Tissue engineering of long bones with a
vascular matrix in a bioreactor. Orthopade, 33, 13941400
(2004).
33. Seidel, J. O., Pei, M., Gray, M. L., Langer, R., Freed, L. E.,
and Vunjak-Novakovic, G.: Long-term culture of tissue engineered cartilage in a perfused chamber with mechanical
stimulation. Biorheology, 41, 445458 (2004).
34. Yu, X., Botchwey, E. A., Levine, E. M., Pollack, S. R., and
Laurencin, C. T.: Bioreactor-based bone tissue engineering:
244
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
PRTNER ET AL.
the influence of dynamic flow on osteoblast phenotypic expression and matrix mineralization. Proc. Natl. Acad. Sci.
USA, 101, 1120311208 (2004).
Minuth, W. W., Stckl, G., Kloth, S., and Dermietzel, R.:
Construction of an apparatus for perfusion cell cultures which
enables in vitro experiments under organotypic conditions.
Eur. J. Cell. Biol., 57, 132137 (1992).
Sittinger, M., Schultz, O., Keyser, G., Minuth, W. W., and
Burmester, G. R.: Artificial tissues in perfusion culture. Int.
J. Artif. Organs, 20, 5762 (1997).
Fassnacht, D., Rssing, S., Stange, J., and Prtner, R.:
Long-term cultivation of immortalised mouse hepatocytes in
a high cell density fixed bed reactor. Biotechnol. Tech., 12,
2530 (1998).
Nehring, D., Adamietz, P., Meenen, N. M., and Prtner,
R.: Perfusion cultures and modelling of oxygen uptake with
three-dimensional chondrocyte pellets. Biotechnol. Tech., 13,
701706 (1999).
Morgan, J. R. and Yarmush, M. L.: Tissue engineering
methods and protocols. Humanda Press, Totowa, NJ (1999).
Sen, A., Kallos, M. S., and Behie, L. A.: New tissue dissociation protocol for scaled-up production of neural stem cells in
suspension bioreactors. Tissue Eng., 10, 904913 (2004).
Fassnacht, D., Rssing, S., Singh, R., Al-Rubeai, M., and
Prtner, R.: Influence of bcl-2 expression on antibody productivity in high cell density hybridoma culture systems. Cytotechnology, 30, 95105 (1999).
Fussenegger, M., Fassnacht., D., Schwartz, R., Zanghi,
J. A., Graf, M., Bailey, J. E., and Prtner, R.: Regulated
overexpression of the survival factor bcl-2 in CHO cells increases viable cell density in batch culture and decreases
DNA release in extended fixed-bed cultivation. Cytotechnology, 32, 4561 (2000).
Nehring, D., Gonzales, R., Czermak, P., and Prtner, R.:
Mathematical model of a membrane filtration process using
ceramic membranes to increase retroviral pseudotype vector
titer. J. Membr. Sci., 237, 2538 (2004).
Noll, T., Jelinek, N., Schmid, S., Biselli, M., and Wandrey,
C.: Cultivation of hematopoietic stem and progenitor cells:
biochemical engineering aspects. Adv. Biochem. Eng. Biotechnol., 74, 111128 (2002).
Cabrita, G. J., Ferreira, B. S., da Silva, C. L., Goncalves,
R., Almeida-Porada, G., and Cabral, J. M.: Hematopoietic
stem cells: from the bone to the bioreactor. Trends Biotechnol., 21, 233240 (2003).
Schubert, H., Garrn, I., Berthold, A., Knauf, W. U., Reufi,
B., Fietz, T., and Gross, U. M.: Culture of haematopoietic
cells in a 3-D bioreactor made of Al2O3 or apatite foam. J.
Mater. Sci. Mater. Med., 15, 331334 (2004).
Davis, J. M. and Hanak, J. A.: Hollow-fiber cell culture.
Methods Mol. Biol., 75, 7789 (1997).
Weichert, H., Falkenberg, F. W., Krane, M., Behn, I.,
Hommel, U., and Nagels, H. O.: Cultivation of animal cells
in a new modular minifermenter, p. 907913. In Beuvery,
E. C., Griffiths, J. B., and Zeijlemaker, W. P. (ed.), Animal cell
technology: developments towards the 21st century. Kluwer
Academic Publishers, The Netherlands (1995).
Nagel, A., Effenberger, E., Koch, S., Lbbe, L., and Marx,
U.: Human cancer and primary cell culture in the new hybrid
bioreactor system tecnomouse, p. 296298. In Spier, R. E.,
Griffiths, J. B., and Berthold, W. (ed.), Animal cell technology: products of today, prospects for tomorrow. ButterworthHeinemann, Oxford (1994).
De Bartolo, L. and Bader, A.: Review of a flat membrane
bioreactor as a bioartificial liver. Ann. Transplant., 6, 4046
(2001).
Jasmund, I. and Bader, A.: Bioreactor developments for
tissue engineering applications by the example of the bioartificial liver. Adv. Biochem. Eng. Biotechnol., 74, 99109
J. BIOSCI. BIOENG.,
(2002).
52. Kulig, K. M. and Vacanti, J. P.: Hepatic tissue engineering.
Transpl. Immunol., 12, 303310 (2004).
53. Gerlach, J. C.: Development of a hybrid liver support system: a review. Int. J. Artif. Organs, 19, 645654 (1996).
54. Sielaff, T. D., Hu, M. Y., Amiot, B., Rollins, M. D., Rao, S.,
McGuire, B., Bloomer, J. R., Hu, W. S., and Cerra, F. B.:
Gel-entrapment bioartificial liver therapy in galactosamine
hepatitis. J. Surg. Res., 59, 179184 (1995).
55. Prenosil, J. E. and Villeneuve, P. E.: Automated production
of cultured epidermal autografts and sub-confluent epidermal
autografts in a computer controlled bioreactor. Biotechnol.
Bioeng., 59, 679683 (1998).
56. Marx, U., Matthes, H., Nagel, A., and Baehr, R. V.: Application of a hollow fiber membrane cell culture system in medicine. Am. Biotechnol. Lab., 11, 26 (1993).
57. Ratcliffe, A.: Tissue engineering of vascular grafts. Matrix
Biol., 19, 353357 (2000).
58. Risbud, M. V. and Sittinger, M.: Tissue engineering: advances
in in vitro cartilage generation. Trends Biotechnol., 20, 351
356 (2002).
59. Minuth, W. W., Strehl, R., and Schumacher, K.: Tissue
engineering from cell biology to artificial organs. WileyVCH Verlag, Weinheim (2005).
60. Lima, E. G., Mauck, R. L., Shelley, H. H., Park, S., Ng, K. W.,
Ateshian, G. A., and Hung, C. T.: Functional tissue engineering of chondral and osteochondral constructs. Biorheology,
41, 577590 (2004).
61. Raimondi, M. T., Boschetti, F., Falcone, L., Fiore, G. B.,
Remuzzi, A., Marinoni, E., Marazzi, M., and Pietrabiss,
R.: Mechanobiology of engineered cartilage cultured under
a quantified fluid-dynamic environment. Biomech. Model.
Mechanobiol., 1, 6982 (2002).
62. Connelly, J. T., Vanderploeg, E. J., and Levenston, M. E.:
The influence of cyclic tension amplitude on chondrocyte
matrix synthesis: experimental and finite element analyses.
Biorheology, 41, 377387 (2004).
63. Sengers, B. G., Oomens, C. W. J., and Baaijens, F. P. T.: An
integrated finite-element approach to mechanics, transport
and biosynthesis in tissue engineering. J. Biomech. Eng., 126,
8391 (2004).
64. Williams, K. A., Saini, S., and Wick, T. M.: Computational
fluid dynamics modelling of steady-state momentum and mass
transport in a bioreactor for cartilage tissue engineering. Biotechnol. Prog., 18, 951963 (2002).
65. Mauck, R. L., Hung, C. T., and Ateshian, G. A.: Modeling
of neutral solute transport in a dynamically loaded porous
permeable gel: implications for articular cartilage biosynthesis and tissue engineering. J. Biomech. Eng., 125, 602614
(2003).
66. Begley, C. M. and Kleis, S. J.: The fluid dynamic and shear
environment in the NASA/JSC rotating-wall perfused-vessel
bioreactor. Biotechnol. Bioeng., 70, 3240 (2000).
67. Omasa, T., Kishimoto, M., Kawase, M., and Yagi, K.: An
attempt at decision making in tissue engineering: reactor evaluation using the analytic hierarchy process (AHP). Biochem.
Eng. J., 20, 173179 (2004).
68. Petersen, J. P., Rcker, A., von Stechow, D., Adamietz, P.,
Prtner, R., Rueger, J. M., and Meenen, N. M.: Present and
future therapies of articular cartilage defects. Eur. J. Trauma,
1, 110 (2003).
69. Freed, L. E., Martin, I., and Vunjak-Novakovic, G.: Frontiers in tissue engineering. In vitro modulation of chondrogenesis. Clin. Orthop., 367 (Suppl.), 4658 (1999).
70. Buschmann, M. D,, Gluzband, Y. A., Grodzinsky, A. J.,
Kimura, J. H., and Hunziker, E. B.: Chondrocytes in agarose
culture synthesize a mechanically functional extracellular matrix. J. Orthop. Res., 10, 745758 (1992).
71. Waldman, S. D., Grynpas, M. D., Pilliar, R. M., and Kandel,
VOL. 100, 2005
R. A.: Characterization of cartilaginous tissue formed on calcium polyphosphate substrate in vitro. J. Biomed. Mater. Res.,
62, 323330 (2002).
72. Malda, J., Martens, D. E., Tramper, J., van Blitterswijk,
C. A., and Riesle, J.: Cartilage tissue engineering: controversy in the effect of oxygen. Crit. Rev. Biotechnol., 23, 175
194 (2003).
73. ODriscoll, S. W., Fitzsimmons, J. S., and Commisso, C. N.:
Role of oxygen tension during cartilage formation by periosteum. J. Orthop. Res., 15, 682687 (1997).
74. Obradovic, B., Carrier, R. L., Vunjak-Novakovic, G., and
BIOREACTOR DESIGN FOR TISSUE ENGINEERING
245
Freed, L. E.: Gas exchange is essential for bioreactor cultivation of tissue engineered cartilage. Biotechnol. Bioeng., 63,
197205 (1999).
75. Ysart, G. E. and Mason, R. M.: Responses of articular cartilage explant cultures to different oxygen tensions. Biochim.
Biophys. Acta, 1221, 1520 (1994).
76. Malda, J., Rouwkema, J., Martens, D. E., Le Comte, E. P.,
Kooy, F. K., Tramper, J., van Blitterswijk, C. A., and Riesle,
J.: Oxygen gradients in tissue-engineered PEGT/PBT cartilaginous constructs: measurement and modelling. Biotechnol.
Bioeng., 86, 918 (2004).
You might also like
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 1 1-Simplestress PDFDocument43 pages1 1-Simplestress PDFAsad KhanNo ratings yet
- Adhesion Testing MethodDocument3 pagesAdhesion Testing MethodMohd Effiezool YaserNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 303-01 - 2.3L EcoBoost - Removal and Installation - Valve CoverDocument25 pages303-01 - 2.3L EcoBoost - Removal and Installation - Valve CoverCARLOS LIMADANo ratings yet
- Design and Control of Concrete Mixtures P 251-360Document110 pagesDesign and Control of Concrete Mixtures P 251-360Narcisa RudnicNo ratings yet
- Paradoxical Twins: Acme and Omega ElectronicsDocument2 pagesParadoxical Twins: Acme and Omega ElectronicsUjjwal AiranNo ratings yet
- Primal ICC 3Document2 pagesPrimal ICC 3hongducxxxNo ratings yet
- Four Bar LinkageDocument13 pagesFour Bar LinkageMBHladilekNo ratings yet
- Enrg 307-Workshop Practice: 3D-Scanner (Handyscan 700)Document41 pagesEnrg 307-Workshop Practice: 3D-Scanner (Handyscan 700)Ali Hejji Al-GhanimNo ratings yet
- Dubai Metro Calculation Note BCLDocument392 pagesDubai Metro Calculation Note BCLFoisul Alam100% (1)
- Skyscrapers v2Document5 pagesSkyscrapers v2nato_kmqNo ratings yet
- LCR MeterDocument2 pagesLCR Meterhungphuc2010No ratings yet
- Convert Ammonia To MethanolDocument16 pagesConvert Ammonia To MethanolSuresh RamakrishnanNo ratings yet
- 12 X 16.5 FirestoneDocument1 page12 X 16.5 FirestoneAndrés GómezNo ratings yet
- Series Capacitor Compensated AC Filterless Flexible LCC HVDC With Enhanced Power Transfer Under Unbalanced FaultsDocument12 pagesSeries Capacitor Compensated AC Filterless Flexible LCC HVDC With Enhanced Power Transfer Under Unbalanced FaultsTRIAD TECHNO SERVICESNo ratings yet
- WORDNETDocument29 pagesWORDNETrishabh8590No ratings yet
- TM Uxxx PDFDocument2 pagesTM Uxxx PDFNtizz ShndrNo ratings yet
- Biology Lab - Catalase ExperimentDocument8 pagesBiology Lab - Catalase Experimentapi-253040433No ratings yet
- Compulsory Assigment K17WADocument11 pagesCompulsory Assigment K17WADevansh MishraNo ratings yet
- 2 All About Heat (Students - Copy)Document54 pages2 All About Heat (Students - Copy)Crystal HuffNo ratings yet
- CCLesson10 DIY Gamer Lessonplan New1Document20 pagesCCLesson10 DIY Gamer Lessonplan New1asmonovNo ratings yet
- UL Bloques y Conectores WainDocument2 pagesUL Bloques y Conectores WainkraikaroNo ratings yet
- Domestic Gas Stove Testing With Use of LPG: IS 4246: 2002 Bureau of Indian Standards (Fifth Revision)Document5 pagesDomestic Gas Stove Testing With Use of LPG: IS 4246: 2002 Bureau of Indian Standards (Fifth Revision)Quality Royal HomeNo ratings yet
- UPX X.XX OEP FinderDocument2 pagesUPX X.XX OEP FindermankavarNo ratings yet
- ISO 9000 or TQM: Which Approach To Adopt - A Canadian Case StudyDocument7 pagesISO 9000 or TQM: Which Approach To Adopt - A Canadian Case StudyAdrian SîrbuNo ratings yet
- CarloGavazzi Digital Panel Meters-Http://carlogavazziegypt - Eg.vg/-Egyptian Industrial SolutionsDocument20 pagesCarloGavazzi Digital Panel Meters-Http://carlogavazziegypt - Eg.vg/-Egyptian Industrial SolutionsNour Al-HattabNo ratings yet
- Phyc-2121-Week-11-20 (NEW)Document89 pagesPhyc-2121-Week-11-20 (NEW)Albern BarbacNo ratings yet
- KAT-A 2429 EROX-F Edition5 05-12-2012 EN 01Document3 pagesKAT-A 2429 EROX-F Edition5 05-12-2012 EN 01Gabriela AxinteNo ratings yet
- LIST 300 BKI-L46-10Juni2022Document31 pagesLIST 300 BKI-L46-10Juni2022Muhamad Rifky ANo ratings yet
- Dom MCQ QuestionDocument5 pagesDom MCQ QuestionRamaswamy SubbiahNo ratings yet
- Amazon Hose and Rubber CompanyDocument98 pagesAmazon Hose and Rubber CompanyAmazon Hose and Rubber80% (5)