Professional Documents
Culture Documents
Skullbase00004 0015 PDF
Uploaded by
Jhensczy Hazel Maye AlbaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Skullbase00004 0015 PDF
Uploaded by
Jhensczy Hazel Maye AlbaCopyright:
Available Formats
ORIGINAL ARTICLE
Current Results of the Surgical
Management of Acoustic Neuroma
Sun H. Lee, M.D., Ph.D,1 Thomas 0. Willcox Jr., M.D.,2 and
William A. Buchheit, M.D.3
ABSTRACT
A retrospective analysis of 162 consecutive cases in 160 patients who underwent microsurgical resection of vestibular schwannomas between October
1995 and June 2001 was undertaken to compare the results with those of other
treatment modalities. Patient hospital records, operative video pictures, neuroimaging studies, audiograms, and follow-up data were reviewed. The mean follow-up period was 24 months.
There were 34 small (<1.5 cm), 92 medium (1.5-3 cm), and 36 (>3 cm)
large tumors. Six were recurrent tumors. Gross total resection was accomplished in all 34 small tumors and 92 medium tumors but only in 50% of the
large tumors. Among the 126 small and medium tumors, the facial nerve was
saved anatomically in 124 patients. On long-term follow up, facial function
was preserved in 94.4% of all patients. Anatomically, the cochlear nerve was
preserved in 55.9% of the small and 20.7% of the medium tumors. Function
was preserved (Gardner-Robertson class 1 and 2) in 25% of the small and in
19.4% of the medium tumors. Cerebrospinal leakage was present in 10.5%,
meningitis in 9.9%, wound infection in 3.7%, and hematoma or contusion in
2.5%. Only one patient died (mortality rate 0.6%). Our data reflect that surgical removal should be the standard management for acoustic tumors, particularly for large and medium tumors, and can be accomplished with acceptable
complication rates.
KEYWORDS: Acoustic neuroma, complications, surgical outcome
Skull Base, volume 12, number 4, 2002. Address for correspondence and reprint requests: Sun H. Lee, M.D., Division of Neurosurgery,
UMDNJ-Robert Wood Johnson University Hospital, 125 Paterson St., Ste. 2100, New Brunswick, NJ 08901. E-mail: leesh@umdnj.edu.
lDivision of Neurosurgery, UMDNJ-Robert Wood Johnson University Hospital, New Brunswick, New Jersey; Departments of 20tolaryngology and 3Neurosurgery, Thomas Jefferson University Hospital, Philadelphia, Pennsylvania. Copyright C 2002 by Thieme Medical
Publishers, Inc., 333 Seventh Avenue, New York, NY 10001, USA. Tel: +1(212) 584-4662.1531-5010,p;2002,12,04,189,196,ftx,en;sbsOO298x.
189
190 SKULL BASE: AN INTERDISCIPLINARY APPROACH/VOLUME 12, NUMBER 4 2002
Refined microsurgical techniques, advanced
intraoperative monitoring of cranial nerve function, and improved neuroanesthesia have improved
the surgical outcomes associated with acoustic neuromas. Mortality rates have dropped below 1%, facial nerve preservation rates have improved above
90%,1,2 and hearing preservation has become a realistic goal for small tumors. Despite these advances,
microsurgical treatment is still associated with some
risks, and the potential exists for serious complications.
As radiosurgery becomes more popular and
is accepted as an alternative to microsurgery for the
treatment of selected patients, surgical outcomes
associated with the resection of acoustic neuromas
will need to be compared with the outcomes of other
treatment modalities. We analyzed our current results to compare them with other surgical series
and with radiosurgical outcomes, and discuss the
management strategy of acoustic tumors.
METHODS AND MATERIALS
Clinical Material
Between October 1995 and June 2001, 160 patients with 162 vestibular schwannomas underwent
microsurgical resection.
Ages ranged from 15 to 75 years (mean age,
47.3 years). The most prevalent age was in the 5th
decade (Table 1). There were 74 right-sided tumors and 86 left-sided tumors in 76 males and 84
females.
The size ofthe tumors was classified as small
(less than 1.5 cm maximum diameter), medium
(1.5-3 cm), and large (larger than 3 cm). There
were 34 (21%) small tumors, 92 (56.8%) medium
tumors, and 36 (22.2%) large tumors. There were 7
recurrent tumors. Among the 34 small tumors, 17
patients had intracanalicular tumors (10.5%). Five
patients had their first operations at other hospitals, and two patients underwent two operations at
our hospital because of recurrences.
The common presenting symptoms were
hearing loss in 156 (96.5%), dysequilibrium in 58
(35.9%), tinnitus in 49 (30.3%), facial weakness in
17 (10.6%), trigeminal symptoms in 14 (8.5%),
headache in 16 (9.9%), and swallowing difficulty in
3 (1.4%). The duration of symptoms ranged from 1
month to 10 years.
Two underwent a reoperation for a recurrence. One patient had a recurrence 6 months after
partial removal of a large acoustic neuroma (maximum diameter, 5.5 cm). The second patient also
had a large tumor (maximum diameter, 5 cm) that
recurred 2 years after the patient's initial subtotal
resection. One patient had neurofibromatosis type
II. The follow-up period ranged from 3 months to
4.8 years (mean follow up, 24 months). Hospital
stays ranged from 3 days to 30 days (median 5 days;
mean, 6.4 days).
Surgical Technique
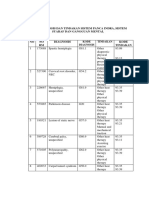
Table 1 Patients' Age by Decade and Gender
Age
<20
20-29
30-39
40-49
50-59
60-69
70<
Male
(n=76)
Female
(n=84)
Total
(n=160)
1
3
15
24
22
7
1
5
22
23
25
7
1
2
8
37
47
47
14
5
All patients underwent microsurgical resection of
their acoustic neuroma via a suboccipital approach
in the lateral position. A lumbar drain, prophylactic
antibiotics, and short-term steroids were used in
every case.
In all patients, brainstem evoked responses
(BSER) and electromyographic responses from the
facial muscles were monitored. Trigeminal nerve
function and extraocular muscle function were also
CURRENT RESULTS OFTHE SURGICAL MANAGEMENT OFACOUSTIC NEUROMA/LEE ET AL
monitored. An experienced neuro-otological surgeon assisted with drilling the internal auditory
canal.
RESULTS
94.4% of all patients showed preserved facial function. Functional recovery was achieved in 96.8% for
small and medium tumors. Facial dysfunction was
aggravated more than 2 House-Brackmann (H-B)
grades in 9 (5.6%) patients. Of the patients in whom
anatomic preservation was achieved, 19.7% showed
transient postoperative worsening of facial function.
Tumor Control
Hearing Preservation
The extent of tumor removal was classified as total,
near total, and subtotal. Even if there was no evidence of tumor mass on postoperative MRI, it was
regarded as a near total removal if the surgeon
thought that a tiny fragment of tumor was firmly
attached to the cranial nerves or brain stem. Gross
total removal was defined as tumors that were removed totally or near totally. Gross total removal
was achieved in all 34 small tumors and 92 medium
tumors (Table 2). However, gross total removal was
achieved in only 50 % of the large tumors. Three
patients developed a recurrence within 6 months, 2
years, and 9 months respectively. These three patients had very large tumors, and subtotal removals
were performed during the initial operations to decompress the brain stem. Two patients underwent
a reoperation, and one patient underwent Gamma
knife radiosurgery for their recurrence.
Facial Nerve Preservation
Among the 126 small and medium-size tumors, the
facial nerve was preserved anatomically in 124 patients (98.4%, Table 3). On long-term follow up,
Table 2 Extent of Removal of 162
Acoustic Neuromas
Extent of Small
Removal (<1.5cm)
Medium
Large
(1.5-3.0cm) (>3cm)
Total
32
76
Near total 2
16
Subtotal
Gross total: total + near total.
11
7
18
Total
(%)
119 (73.4)
23 (14.2)
18 (11.1)
Anatomically, the cochlear nerve was preserved in
55.9% of small tumors and 20.7% of medium tumors, but function (Gardner-Robertson class 1 and
2) was preserved in only 25% of small tumors and
19.4% of medium tumors (Table 4). Among the 17
intracanalicular tumors, 10 patients had serviceable
hearing preoperatively and 5 patients maintained
serviceable hearing postoperatively.
Complications
Postoperatively, one patient died (0.6%) of massive
gastrointestinal bleeding and severe brain swelling
due to a cerebral infarction involving the middle
cerebral artery territory. Other complications included 17 (10.5%) cerebrospinal fluid (CSF) leaks
and meningitis in 16 (9.9 %) patients. There were
10 (6.2%) cases of bacterial meningitis and 6 (3%)
cases of aseptic meningitis. Wound infection occurred in 6 patients (3.7%), cerebellar contusion in
4 (2.5%), hydrocephalus in 4, pneumonia in 3, exposure keratitis in 3, and lateral gaze limitation in 3.
Among the 17 patients with CSF leaks, lumbar drains were placed in 4 and a mastoidectomy
with revision was done in 13. One patient developed a delayed leak 9 months after surgery, and one
patient showed a recurrent leak after treatment
with lumbar drainage. If postoperative meningitis
was confirmed by staining and culture for lumbar
CSF, long-term intravenous antibiotics were administered. If the patient showed signs of aseptic
meningitis, slow tapering steroid therapy was used.
191
192 SKULL BASE: AN INTERDISCIPLINARY APPROACH/VOLUME 12, NUMBER 4 2002
Table 3 Facial Nerve Preservation After Resection of 162 Acoustic Neuromas
No. H-B Grade at
Last Follow-Up
No. Anatomic
Extent of Removal
5-6
3-4
S
1-2
Preservation
N
T
Tumor Size
34
83
24
34
0
2
32
Small
90
0
16
76
Medium
30
18
7
11
Large
T, total; N, near total; S, subtotal; H-B, House-Brackmann.
5
11
4
1
tumors is unclear. Autopsy studies suggest that
acoustic neuromas may be present in 2.4% of individuals dying from unrelated causes. Furthermore,
the natural history of small acoustic neuromas is
still uncertain in terms of their growth rate and the
development of hearing dysfunction.4 Three treatment options are considered for patients with an
acoustic neuroma: surgical removal, radiation therapies such as gamma knife radiosurgery or LINAC
radiosurgery, and observation with periodic audiography and MRI. Recent studies that evaluated the
growth rates of untreated tumors suggest that most
acoustic neuromas enlarge within 1 or 2 years.5-7
Most patients sought treatment for hearing
loss, which was found in 94.6%8 of the patients at
the initial examination. A gradual loss of high frequencies is most common, but some patients showed
Four patients had hydrocephalus, two of whom
needed ventriculoperitoneal shunts. Ventriculoperitoneal shunts were preoperatively placed in two patients. Eight patients with facial weakness received
gold weight lid implants, and one patient underwent facial-hypoglossal nerve anastomosis.
DISCUSSION
An estimated 2000 to 3000 new cases of unilateral
acoustic neuromas are diagnosed in the United
States each year (incidence of 1 per 100,000 per
year).3 With the use of MRI, small tumors are increasingly being detected. However, the actual incidence of both symptomatic and asymptomatic
Table 4 Hearing Preservation After Surgical Resection of 162 Acoustic Neuromas
Functional
Postop
Preop
Anatomic
Preservation
Hearing
Hearing
Preservation
Small (34)
GR class 1
19 (55.9%)
13
7
20
2
1+2
Medium (92)
GR class 1
2
1+2
Large (36)
GR class 1
2
1+2
GR, Gardner-Robertson.
5
5
5/20 (25%)
11
31
6
6
6/31 (19.4%)
2
5
7
19 (20.7%)
20
CURRENT RESULTS OFTHE SURGICAL MANAGEMENT OF ACOUSTIC NEUROMA/LEE ET AL
sudden hearing loss of about 10%.9,10 Tinnitus is
also common, and about half of patients have tinnitus preoperatively. Dizziness, unsteadiness, vertigo, and a sensation of fullness in the ear can also
follow the onset of hearing loss. As the tumor enlarges, numbness or altered sensation on the face or
tongue, headache, diplopia, unsteady gait, difficulty
with coordination, hoarseness, and difficulty swallowing may occur.
Surgical resection of acoustic neuromas has
been continuously refined and operative mortality
rates have decreased to less than 1% with good facial
nerve preservation.11'12 Intraoperative neurophysiological monitoring of the facial and cochlear nerves
facilitates preservation of these cranial nerves.13
Microsurgical resection of acoustic neuromas can be accomplished via three operative approaches: the translabyrinthine approach, middle
fossa approach, and retrosigmoid suboccipital approach.14-16 The choice of surgical approach is influenced by the size and position of the tumor, the
surgeon's preference and experience, and the likelihood of preserving hearing on the affected side.17
We used the retrosigmoid suboccipital approach
for all of our cases. In the literature on microsurgical experience, complete resection of tumors has
been achieved in almost all patients and facial nerve
function has been preserved in 65% to 100% of the
patients.1'2'18-20 The rate of hearing preservation
ranges from 13 to 82%,1,2,18,19,21-23 but there is some
disagreement over what constitutes "serviceable"
hearing.21 The incidence of tumor regrowth after
complete resection of acoustic neuromas through
the suboccipital approach has been reported to be
between 0 and 9%.1,24
CSF leakage remains the most common
complication of acoustic neuroma surgery. An
early series of operations for acoustic neuromas reported CSF leak rates as high as to 35% with large
tumors. In contrast, in a recent series the rate of
CSF leaks was less than 10%.25 Fishman and coworkers26 reported a 17% incidence of CSF leaks,
and continuous lumbar drainage stopped the leak
in 87%. We have performed early operations for
CSF leaks rather than placing lumbar drains. The
incidence of postoperative bacterial meningitis
ranges from 2% to 10% in current published series
and is usually associated with a CSF leak.25 Aseptic meningitis may occur in as many as 10% of
acoustic neuroma patients. Some patients prefer radiosurgery to surgical resection because the potential to preserve hearing and facial nerve function is
greater and the interventional risks are less.19,27-29
The long-term tumor control rates are reported to
be 86 to 95%.19 The most frequent complications
following acoustic neuroma radiosurgery are delayed and often transient cranial neuropathies that
develop 1 to 21 months after radiosurgery in 5 to
36% of patients. Facial nerve weakness has been
reported in 17% after radiosurgery and hearing
preservation in 75% after radiosurgery.19 Overall,
our surgical outcomes are comparable to reported
surgical data and to radiosurgical data (Table 5).
The rate of tumor control with resection was superior to that of radiosurgery for large tumors and
the complication rate was acceptable. The facial
nerve was preserved in more than 95%, which is
comparable to radiosurgery in the long-term follow up. However, the rate of hearing preservation
was unsatisfactory.
CONCLUSION
Most acoustic neuromas grow within several years
of diagnosis.5'7 The early detection of acoustic neuromas with MRI and treatment with either microsurgery or radiosurgery is warranted. Small and
medium-sized tumors should be removed totally
with preservation of facial function. Hearing preservation is considered only for patients with small tumors, with Class 1 and 2 hearing, and good brain
stem waves III and V. For large tumors subtotal
resection with preservation of facial nerve is warranted.
193
194 SKULL BASE: AN INTERDISCIPLINARY APPROACH/VOLUME 12, NUMBER 4 2002
0
N
CY)
CY)
ID
zz
CN
CU
_
C.,
CUoCE
CN
OD
zzz
VI
CN
U-.
'o-0
0.
C)4
,CU
0C0
LO
(C)
CY)
a)
CY)
co -
0-
(0
a)
zz
$: na ?
C/)
C/) N
A
o)
-C0
CU
oZ
0
Cl)
gC
LC)
a)
-
a)
Cl)
--O
-o
-0
-jo 0- -0 000 "
(03
LO) N N O t CN LO C0 r- CY)
a 03 03 a a3) LC)
00
C)00
C)
N0
C) IC)
N
LO
(C)
03 ra3)
Vl)
ZCL
C)
U)
00
Cl)
-0
>0
= U
C
0
-J 0-3t
"
oIC)
LC)
03
00
-Q
CY)
.ACU
OCu
La
U?
LO (N
r-
.0
l-
co
o0'
coCU
a)
Uf)
0
(1)
a-
Co
aCuU)
.0
r-
CY
00
CY)~~~~~~l
N a)
a
a)
CL
.ECo
00
0
CU
.0
0
C
aO
Cu
_R
&
c;
_
_
r-
r-
CN
CY
0)
CN
CID
C
0
0
-i
.
.0
(03
a)
3
0.
S)
CN
CY)
a3)
a)
m
CX
(D
L Oc)0
0
U)4.X
030
(0
E0
03
aT)
aY)
.0
C.)
CU
E-
CN
C-)
-j
CU
Cli
o
cn
O~~~~~~~~~00
Cs
0
-cu
co
as
Q) a)
c
EU)
003a)
E
o
WCl) (
&0
O)
cl coI Cu
-'
E
H-
CURRENT RESULTS OFTHE SURGICAL MANAGEMENT OF ACOUSTIC NEUROMA/LEE ET AL
REFERENCES
1. Ojemann RG. Management of acoustic neuromas (vestibular schwannomas) Clin Neurosurg 1993;40:498-535
2. Samii M, Matthies C, Tatagiba M. Intracanalicular acoustic neurinomas. Neurosurgery 1991;29:189-199
3. Acoustic Neuroma. In: NIH Consensus Development
Conference Consensus Statement vol. 9. National Institutes of Health, Bethesda, MD; 1991:1-24
4. Wiegand DA, Ojemann RG, Fickel V. Surgical treatment
of acoustic neuroma (vestibular schwannoma) in the
United States: Report from the acoustic neuroma registry.
Laryngoscope 1996;106:58-66
5. Bederson JB, Von Ammon K, Wichmann WW, Yasargil
MG. Conservative treatment of patients with acoustic tumors. Neurosurgery 1991;28:646-651
6. Charabi S, Thomsen J, Mantoni M, et al. Acoustic neuroma (vestibular schwannoma): Growth and surgical and
nonsurgical consequences of the wait-and see policy. Otolaryngol Head Neck Surg 1995;113:5-14
7. Deen HG, Ebersold MJ, Harner SG, et al. Conservative
management of acoustic neuroma: An outcome study.
Neurosurgery 1996;39:260-266
8. Kanzaki J, Ogawa K, Ogawa S, Yamamoto M, Ikeda S, 0Uchi T. Audiological findings in acoustic neuroma. Acta
Otolaryngol 1991;487:125-132
9. Saunders JE, Luxford WVM, Devgan KK, Fetterman BL.
Sudden hearing loss in acoustic neuroma patients. Otolaryngol Head Neck Surg 1995;113:23-31
10. Yanagihara N, Asai, M. Sudden hearing loss induced by
acoustic neuroma: Significance of small tumors. Laryngoscope 1993;103:308-311
11. House JW, Brackmann DE. Facial nerve grading system.
Otolaryngol Head Neck Surg 1985;93:146-147
12. Nutik SL. Facial nerve outcome after acoustic neuroma
surgery. Surg Neurol 1994;41:28-33
13. Lalwani AK, Butt FY,Jackler RK, Pitts LH, Yingling CD.
Facial nerve outcome after acoustic neuroma surgery: A
study from the era of cranial nerve monitoring. Otolaryngol Head Neck Surg 1994;111:561-570
14. Brackmann DR, Hitselberger WE, Beneke JE, House WF.
Acoustic neuromas. Middle fossa and translabyrinthine removal in Rand RW(ed): Microneurosurgery. St. Louis,
MO: C.V. Mosby Co.; 1985:311-334
15. Haines SJ, Levine SC. Intracanalicular acoustic neuroma:
early surgery for preservation of hearing. J Neurosurg 1993;
79:515-520
16. Hardy DG, Macfarlane R, Baguley D, Moffat DA. Surgery for acoustic neuroma. An analysis of 100 translabyrinthine operations. J Neurosurg 1989;71:799-804
17. Jackler RK, Pitts LH. Selection of surgical approach to
acoustic neuroma. Otolaryngol Clin North Am 1992;25:
361-387
18. Ebersold MJ, Harner SG, Beatty CW, Harper CM, Quast
LM. Current results of the retrosigmoid approach to
acoustic neuroma. J Neurosurg 1992;76:901-909
19. Pollock BE, Lunsford LD, Kondziolka D, et al. Outcome
analysis of acoustic neuroma management: A comparison
of microsurgery and stereotactic radiosurgery. Neurosurgery
1995;36:215-229
20. Sampath P, Holliday MJ, Brem H, Niparko JK, Long DM.
Facial nerve injury in acoustic neuroma (vestibular schwannoma) surgery: etiology and prevention. J Neurosurg 1997;
87:60-66
21. Glassock ME III, Hays JW, Minor LB, Haynes DS, Carrasco VN. Preservation of hearing in surgery for acoustic
neuromas. J Neurosurg 1993;78:864-870
22. Jannetta PJ, Moller AR, Moller MB. Technique of hearing
preservation in small acoustic neuromas. Ann Surg 1984;
200:513-523
23. Snyder WE, Pritz MB, Smith RR. Suboccipital resection
of a medial acoustic neuroma with hearing preservation.
Surg Neurol 1999;51:548-553
24. Schessel DA, Nedzelski JM, Kassel EE, Rowed DW. Recurrence rates of acoustic neuroma in hearing preservation
surgery. Am J Otol 1992;13:233-235
25. Weit RJ, Teixido M, Liang J. Complications in acoustic
neuroma surgery. Otolaryngol Clin North Am 1992;
25:389-412
26. Fishman AJ, Hoffman RA, Roland Jr T, Lebowitz RA,
Cohen NL. Cerebrospinal fluid drainage in the management of CSF leak following acoustic neuroma surgery.
Laryngoscope 1996;106:1002-1004
27. Flickinger JC, Kondziolka D, Lunsford LD. Dose and diameter relationships for facial, trigeminal and acoustic neuropathies following acoustic neuroma radiosurgery. Radiother Oncol 1996;41:215-219
28. Niranjan A, Lunsford LD, Flickinger JC, Maitz A,
Kondziolka D. Dose reduction improves hearing preservation rates after intracanalicular acoustic tumor radiosurgery.
Neurosurgery 1999;45:753-765
29. Poen JC, Golby AJ, Forster KM, et al. Fractionated stereotactic radiosurgery and preservation of hearing in patients
with vestibular schwannoma: A preliminary report. Neurosurgery 1999;45:1299-1307
Commentary
Dr. Buchheit was well known for his expertise in dealing with acoustic tumors during his active career. This review thoroughly defines the outcomes expected of surgery for acoustic neuromas by
the best surgeons currently involved. Cure of the
tumor is the rule. The mortality rate is extremely
low, but not zero. Cranial nerves are usually preserved, and satisfactory facial function can be obtained in almost all patients with smaller tumors.
195
You might also like
- Coronary Artery DiseaseDocument51 pagesCoronary Artery DiseaseJhensczy Hazel Maye AlbaNo ratings yet
- Jurnal Na6873leadershpDocument4 pagesJurnal Na6873leadershpAmanda DavisNo ratings yet
- NCM 106: Care of Clients With Problems in Cellular Aberrations, Acute Biologic Crisis, Emergency and Disaster NursingDocument41 pagesNCM 106: Care of Clients With Problems in Cellular Aberrations, Acute Biologic Crisis, Emergency and Disaster NursingJhensczy Hazel Maye AlbaNo ratings yet
- Bipolar 1 Case PresentationDocument111 pagesBipolar 1 Case PresentationJhensczy Hazel Maye AlbaNo ratings yet
- Lesson 1 LeaderDocument25 pagesLesson 1 LeaderJhensczy Hazel Maye Alba100% (1)
- Artcile CcbduDocument7 pagesArtcile CcbduJhensczy Hazel Maye AlbaNo ratings yet
- A Case Study On MeningiomaDocument87 pagesA Case Study On MeningiomaJhensczy Hazel Maye Alba50% (4)
- WFMH Living With Schizophrenia Section 2Document6 pagesWFMH Living With Schizophrenia Section 2Jhensczy Hazel Maye AlbaNo ratings yet
- Lesson 3 TheoriesDocument69 pagesLesson 3 TheoriesJhensczy Hazel Maye AlbaNo ratings yet
- Perception and Coordination 2Document58 pagesPerception and Coordination 2Jhensczy Hazel Maye AlbaNo ratings yet
- Polytechnic College of Davao Del Sur, IncDocument4 pagesPolytechnic College of Davao Del Sur, IncJhensczy Hazel Maye AlbaNo ratings yet
- Conservative Management of Acoustic NeuromaDocument7 pagesConservative Management of Acoustic NeuromaJhensczy Hazel Maye AlbaNo ratings yet
- Antibacterial SDocument1 pageAntibacterial SJhensczy Hazel Maye AlbaNo ratings yet
- Mood Dynamics in Bipolar Disorder: Research Open AccessDocument9 pagesMood Dynamics in Bipolar Disorder: Research Open AccesswulanfarichahNo ratings yet
- Chapter 2 - Basic Elements of Demand and SupplyDocument39 pagesChapter 2 - Basic Elements of Demand and SupplyJhensczy Hazel Maye Alba100% (1)
- Cleft Lip and Palate Etiology Epidemiology Preventive and Intervention Strategies 2161 0940.1000150Document6 pagesCleft Lip and Palate Etiology Epidemiology Preventive and Intervention Strategies 2161 0940.1000150Dwitiara SeptianiNo ratings yet
- Closed Reduction and External Fixation for Displaced Proximal Humeral FracturesDocument4 pagesClosed Reduction and External Fixation for Displaced Proximal Humeral FracturesJhensczy Hazel Maye AlbaNo ratings yet
- Gunshot InjuriesDocument3 pagesGunshot InjuriesJhensczy Hazel Maye AlbaNo ratings yet
- Lee - Otologic Manifestations of AN - Acta Oto - 2015Document8 pagesLee - Otologic Manifestations of AN - Acta Oto - 2015Jhensczy Hazel Maye AlbaNo ratings yet
- Breast Lung CADocument91 pagesBreast Lung CAJhensczy Hazel Maye AlbaNo ratings yet
- Subdural HematomaDocument7 pagesSubdural HematomaJhensczy Hazel Maye AlbaNo ratings yet
- Nursing Care Plan for HyperthermiaDocument2 pagesNursing Care Plan for HyperthermiaJhensczy Hazel Maye AlbaNo ratings yet
- PEDIA CPDocument45 pagesPEDIA CPJhensczy Hazel Maye AlbaNo ratings yet
- A Procedural Report On Open Reduction and Internal FixationDocument9 pagesA Procedural Report On Open Reduction and Internal FixationJhensczy Hazel Maye AlbaNo ratings yet
- Health TeachingsDocument2 pagesHealth TeachingsJhensczy Hazel Maye AlbaNo ratings yet
- IV FluidsDocument1 pageIV FluidsJhensczy Hazel Maye AlbaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Suspected Heart Failure: Section 5 Section 7 Section 8Document10 pagesSuspected Heart Failure: Section 5 Section 7 Section 8Javier TapiaNo ratings yet
- Kode Diagnosis Dan Tindakan Sistem Panca IndraDocument3 pagesKode Diagnosis Dan Tindakan Sistem Panca IndraNitaNurmalaNo ratings yet
- Diare - HarrisonDocument6 pagesDiare - HarrisonStephen MasengiNo ratings yet
- Atrophic Glossitis Causes, Symptoms, Signs, TreatmentDocument16 pagesAtrophic Glossitis Causes, Symptoms, Signs, TreatmentPutrisya Rafanael SafageNo ratings yet
- A SHITABADocument5 pagesA SHITABAiMer22No ratings yet
- Endocrine Disorders and PregnancyDocument32 pagesEndocrine Disorders and PregnancyChristine Marie BudlaoNo ratings yet
- Water Recreation and DiseaseDocument260 pagesWater Recreation and Diseasetuyetnam24No ratings yet
- English Pharmacy Chapter 4 Endocrine Lymphatic SystemsDocument1 pageEnglish Pharmacy Chapter 4 Endocrine Lymphatic SystemshutamiNo ratings yet
- Preoperative PreparationDocument22 pagesPreoperative Preparationjackyploes100% (1)
- Rabies PreventionDocument3 pagesRabies PreventionFrinkaWijaya100% (1)
- LESSON PLAN ON Hyper Emesis GravidarumDocument12 pagesLESSON PLAN ON Hyper Emesis GravidarumMadhavi ModaNo ratings yet
- Diagnosis and Prognosis of Pancreatic CancerDocument6 pagesDiagnosis and Prognosis of Pancreatic CancerAgung Eka PutriNo ratings yet
- NCM 112 - Communicable Disease: Tarlac State UniversityDocument3 pagesNCM 112 - Communicable Disease: Tarlac State UniversityDeinielle Magdangal RomeroNo ratings yet
- Communicable Disease NursingDocument44 pagesCommunicable Disease NursingFreeNursingNotes100% (17)
- CNH Construction Health DeclarationDocument1 pageCNH Construction Health DeclarationEna Ahmad PieNo ratings yet
- Lung Cancer (Nursing Care)Document5 pagesLung Cancer (Nursing Care)heiyuNo ratings yet
- Clinical Guideline For Fluid Overload Pulmonary OedemaDocument3 pagesClinical Guideline For Fluid Overload Pulmonary OedemaEka HandreanNo ratings yet
- Swine Flu in UrduDocument3 pagesSwine Flu in UrduBilawal ButtNo ratings yet
- PubH 612 Epidemiology Take Home ExamDocument6 pagesPubH 612 Epidemiology Take Home ExamGadisa TesfayeNo ratings yet
- Visitors Personal Declaration Form - COVID 19Document1 pageVisitors Personal Declaration Form - COVID 19Leoni FrancNo ratings yet
- Immune Reconstitution Inflammatory Syndrome in HivDocument37 pagesImmune Reconstitution Inflammatory Syndrome in Hivpokhara gharipatanNo ratings yet
- SCNICU Starter PackDocument7 pagesSCNICU Starter PackALIF HAIQAL MOHD HUSSEINNo ratings yet
- DRUG StudyDocument4 pagesDRUG StudyMaica LectanaNo ratings yet
- 36 - SIS in The Treatment of post-COVID Patients - ENDocument7 pages36 - SIS in The Treatment of post-COVID Patients - ENAdela NistorNo ratings yet
- NAC OSCE A Comprehensive ReviewDocument27 pagesNAC OSCE A Comprehensive ReviewNac Osce83% (29)
- GSIS vs. de Castro 185035Document2 pagesGSIS vs. de Castro 185035Juan DoeNo ratings yet
- A Screening Test For Obsessive-Compulsive DisorderDocument1 pageA Screening Test For Obsessive-Compulsive DisorderDebbie de GuzmanNo ratings yet
- The Use of Levosimendan in Children With Cancer With Severe Acute Cardiac Dysfunction Case Series and A Review of The LiteratureDocument4 pagesThe Use of Levosimendan in Children With Cancer With Severe Acute Cardiac Dysfunction Case Series and A Review of The Literaturehadi40canadaNo ratings yet
- 7492-Article Text-24895-1-10-20161230Document13 pages7492-Article Text-24895-1-10-20161230Dreyara ElleNo ratings yet
- Melioidosis - Pseudoglanders Whitmore Disease OverviewDocument31 pagesMelioidosis - Pseudoglanders Whitmore Disease OverviewAchie100% (1)