Professional Documents
Culture Documents
Fluids and Electrolytes
Uploaded by
Arjun SinghCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluids and Electrolytes
Uploaded by
Arjun SinghCopyright:
Available Formats
Fluids & Electrolytes
This self-directed learning module contains information
you are expected to know to protect yourself, our
patients, and our guests.
Target Audience: All CHS licensed nurses providing
patient care and/or involved in the delivery of
patient care.
Contents
Instructions ........................................................2
Learning Objectives...........................................2
Module Content .................................................3-7
Appendixes . 8-14
Job Aid ..............................................................15
Posttest .............................................................16-18
Page 1 of 18
Fluids and Electrolytes
The material in this module is an introduction to important general information. After
completing this module, contact your supervisor to obtain additional information specific to
your department.
Read this module.
If you have any questions about the material, ask your supervisor.
Complete the online post test for this module.
The Job Aid on page 15 may be customized to fit your department and then used
as a quick reference guide.
Completion of this module will be recorded under My Learning in PeopleLink
Learning Objectives:
When you finish this module, you will be able to:
Discuss the basic principles of fluid and electrolytes
Describe the imbalances related to sodium, potassium, magnesium, calcium,
phosphorus, and chloride
Identify the treatment for fluid and electrolyte imbalances
Reference:
Fluid & Electrolytes Made Incredibly Easy, 5th Ed. (2011), Lippincott, Williams &
Wilkins
Page 2 of 18
Fluids and Electrolytes
Balancing Basics: A Look at Fluids
All major organs work together to maintain the proper balance of fluid
to
maintain that balance, the amount of fluid gained throughout the day must equal
the amount lost
Body fluids have many functions:
Lubricants / solvents for metabolic processes
Carriers for nutrients (i.e. Oxygen, glucose)
Transport wastes
Regulate body temperature
Internal medium for cell metabolism
Participate in chemical & metabolic processes
Fluids are used to rehydrate cells, add fluid to the intravascular space, improve
electrolyte balance, and maintain hemodynamic balance.
Page 3 of 18
Fluids and Electrolytes
Fluid Classification and Tonicity:
Classified as a Crystalloid or Colloid and Blood Products
o Crystalloids: solutions with small molecules that flow easily from the
bloodstream into cells and tissues. May be isotonic, hypotonic, or
hypertonic. They are the least expensive and generally used for volume
resuscitation.
o Colloids: act as plasma expanders (help to maintain protein balance
and colloid osmotic pressure) examples: albumin, plasma protein
fraction, dextran, and hetastarch
o Blood products: used for fluid volume resuscitation, maintenance of
RBC and HGB levels, and coagulation factor replacement
Tonicity
o Isotonic - has the same solute (matter dissolved in solution)
concentration as another solution (i.e. 0.9% NaCl)
o Hypotonic has a lower solute concentration than another solution (i.e.
0.45% NaCl)
When giving a hypotonic IV solution you may cause too much
fluid to move into the cells. As a result the cells can swell and
burst.
o Hypertonic has a higher solute concentration than another solution
(i.e. D5W initially before the dextrose is metabolized by the cells, 3%
NaCl)
Water is drawn out of the cells and into the ECF compartment.
Therapeutic in some instances: to decrease cerebral edema.
When giving a hypertonic solution to a patient, it may cause too
much fluid to be pulled from cells into the bloodstream, and the
cells can shrink
** See AppendixA : A Look at IV Solutions for types of IV fluids, uses and
special considerations **
Page 4 of 18
Fluids and Electrolytes
A Look at Electrolytes:
Electrolytes functions include: helping to maintain homeostasis, metabolic
functions, cardiac and nerve conduction, acid-base balance and water distribution.
Major Intracellular Electrolytes
Potassium
(K+)
Magnesium
(Mg+)
Phosphorus/Phosphate
(P-)
Major Intracellular fluid (ICF) cation
Regulates cell excitability & nerve impulse conduction
Permeates cell membranes, thereby affecting the cells electrical status (resting
membrane potential)
Helps to control ICF osmolality and, consequently, ICF osmotic pressure
Regulates muscle contraction and myocardial membrane responsiveness
A leading ICF cation
Contributes to many enzymatic and metabolic processes, particularly protein
synthesis
Modifies nerve impulse transmission and skeletal muscle response (unbalanced
Mg+ concentrations dramatically affect neuromuscular processes)
Influences normal function of the cardiovascular system and Na+ and K+ ion
transportation
Main ICF anion
Promotes energy storage and carbohydrate, protein and fat metabolism
Acts as a hydrogen buffer
Major Extracellular Electrolytes
Sodium (Na+)
Chloride
(Cl-)
Calcium (Ca+)
Bicarbonate
(HCO3-)
Main extracellular fluid (ECF) cation
Helps govern normal ECF osmolality (a shift in Na+ concentration triggers a fluid
volume change to restore normal solute and water ratios)
Component of the sodium-potassium pump
Helps maintain acid base balance
Activates nerve and muscle cells
Influences water distribution (with chloride)
Main ECF anion
Helps maintain normal ECF osmolality
Affects body pH
Plays a vital role in maintaining acid-base balance
combines with hydrogen ions to
produce hydrochloric acid
A major cation in teeth and bones
Found in fairly equal concentrations in ECF and ICF
Found in cell membranes
it helps cells adhere to one another and maintain their
shape
Acts as an enzyme activator within cells (muscles must have Ca+ to contract)
Aids in coagulation
Affects cell membrane permeability and firing level
Present in ECF
Regulates acid-base balance
Page 5 of 18
Fluids and Electrolytes
Multiple organs in the body play a role in electrolyte balance:
Kidneys (regulate Na+ and K+ balance) Recommended daily Na+ intake: 2 Grams
Lungs and Liver regulate Na+ and water balance and blood pressure
Heart secretes ANP, causing Na+ excretion
Sweat glands excrete Na+, K+, Cl-, and water in sweat
GI Tract absorbs and secretes fluids and electrolytes
Parathyroid Glands secretes parathyroid hormone, which draws calcium into the blood and
helps move phosphorus to the kidneys for excretion
Thyroid Gland- secrets calcitonin, which prevents calcium release from the bone
Hypothalamus and Posterior Pituitary Gland produce and secret ADH causing water
retention, which affects solute concentration
Adrenal Glands secret Aldosterone, which influences NA+ and K+ balance in the kidneys
** See Appendix B: Electrolyte Imbalances Causes of Elevation (Hyper-)
and Decline (Hypo-)
** See Appendix C: Electrolyte Imbalances Signs/Symptoms & Treatment
Page 6 of 18
Fluids and Electrolytes
Dehydration:
Lack of water in extracellular spaces that causes fluid to shift out of the
cells, which then shrink
May be caused by any situation that accelerates fluid loss including
o Diabetes Insipidus (DI)
o Prolonged fever
o Watery diarrhea
o Renal failure
o Hyperglycemia
o Heat injury
Patients prone to dehydration:
o Comatose, confused or bedridden patients
o Infants
o Elderly
o Patients receiving highly concentrated tube feedings without enough
supplemental water
Assessment findings:
o Irritability, confusion, dizziness
o Weakness, extreme thirst
o Fever, dry skin, dry mucous membranes, sunken eyeballs
o Poor skin turgor
o Decreased urine output (with DI urine is pale and plentiful)
o Increased heart rate with falling blood pressure
Hypovolemia, Hypervolemia, Water Intoxication:
Fluid volume status is assessed using some of the following methods:
o Urine output
o Weights
o Vital signs (i.e. HR and BP changes)
o Level of consciousness (changes in mental status)
o Intake and output
o Hemodynamic monitoring (i.e. CVP, PCWP, CO etc.)
o Head-to-Toe assessment (patient signs & symptoms)
o Laboratory values
Treatment based on etiology and presenting symptoms
** See Appendix D: Hypovolemia, Hypervolemia and Water Intoxication **
Page 7 of 18
Fluids and Electrolytes
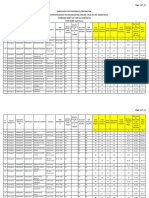
Appendix A: A Look at IV Solutions
Solution
Uses
o
Special Considerations
Fluid loss and dehydration
Dextrose 5% in water
(D5W)
o
o
(Isotonic then becomes
hypotonic)
0.9% Sodium Chloride
(NaCl or NS)
(Isotonic)
0.45% Sodium Chloride
(1/2 NS)
(Hypotonic)
Solution is isotonic initially; becomes
hypotonic when dextrose is metabolized
Dont use for resuscitation or head injured
patients; can cause hyperglycemia
Use cautiously in renal or cardiac disease;
can cause fluid overload
Doesnt provide enough daily calories for
prolonged use; may cause eventual
breakdown of protein
o
o
o
o
o
o
o
o
Shock
Hyponatremia
Used with Blood transfusions
Fluid Volume Resuscitation
Fluid challenges
Metabolic acidosis
Hypercalcemia
Fluid replacement in patients with diabetic
ketoacidosis (DKA)
o Because this replaces extracellular fluid,
o
o
Water replacement
DKA after initial normal saline solution
and before dextrose infusion
Hypertonic dehydration
Sodium and chloride depletion
Gastric fluid loss from nasogastric
suctioning or vomiting
DKA after initial treatment with NS and
NS solution prevents hypoglycemia and
cerebral edema (occurs when serum
osmolality is reduced too rapidly)
In patients with DKA, use only when
glucose falls <250 mg/dL
Hypotonic dehydration
Temporary treatment of circulatory
insufficiency and shock if plasma
expanders are not available
Syndrome of Inappropriate Antidiuretic
Hormone (SIADH) or use 3% NaCl
Addisons crisis
Severe dilutional Hypernatremia
Severe sodium depletion
Volume resuscitation
Electrolyte imbalance (i.e. salt wasting)
Use with caution in patients with cardiac or
renal disease because of danger of heart
failure and pulmonary edema
Administer cautiously to prevent pulmonary
edema
Observe infusion site closely for signs or
infiltration and tissue damage
o
o
o
o
Dextrose 5% in .45%
Normal Saline
(D5 NS)
use with caution in patients with heart
failure, edema, or Hypernatremia; can lead
to fluid volume overload and pulmonary
edema
Use cautiously; may cause cardiovascular
collapse or increased intracranial pressure
(ICP)
Dont use on patients with liver disease,
trauma or burns
(Hypertonic)
Dextrose 5% in normal
saline
(D5NS)
o
o
o
(Hypertonic)
3% Sodium Chloride
(Hypertonic)
o
o
o
o
o
Page 8 of 18
Fluids and Electrolytes
Appendix B: Electrolyte Imbalances Causes of Elevation and Decline
Normal Range
Sodium (Na):
135-145 mEq/L
Potassium (K):
3.5-5.0 mEq/L
Calcium (Ca):
8.9-10.1 mg/dL (serum)
4.4-5.3 mg/dL
(ionized)
Magnesium (Mg):
1.5-2.5 mg/dL
Chloride (Cl):
98-108mEq/L
Causes of elevation (hyper)
Causes of Decline (hypo)
Water loss, inadequate water intake,
excessive sodium intake, Diabetes
Insipidus (DI), certain diuretics, tube
feedings, hypothalamic lesions,
hyperaldosteronism, corticosteroid use,
Cushings Syndrome, in elderly (diarrhea,
low body weight, tube feeds without
adequate water replacement)
Inadequate sodium intake, excessive water
loss, or water gain, heart failure, cirrhosis,
nephrosis, syndrome of inappropriate ADH
(SIADH), sodium depletion, loss of body
fluids without replacement, laxatives,
nasogastric suctioning, hypoaldosteronism,
Medications such as anticoagulants,
anticonvulsants, antidiabetics,
antineoplastics, antipsychotics, diuretics,
sedatives
Lack of dietary intake of potassium,
vomiting, diarrhea, nasogastric suctioning,
potassium-depleting diuretics, certain
antibiotics, insulin, laxatives when used
excessively, adrenergics such as albuterol
and epinephrine, hyperaldosteronism,
hepatic disease, acute alcoholism, heart
failure, acute leukemias, salt wasting
kidney disease, major GI surgery, diuretic
therapy with inadequate potassium
replacement
Hypoparathyroidism, malabsorption,
insufficient or inactivated vitamin D,
inadequate intake of calcium,
hypoalbuminemia, Hyperphosphatemia,
diuretic therapy, diarrhea, acute
pancreatitis, bone cancer, gastric surgery,
alkalosis
Malabsorption related to GI disease,
excessive loss of GI fluids, acute
alcoholism/cirrhosis, diuretic therapy, hyperor hypothyroidism, pancreatitis,
preeclampsia, nasogastric suctioning, fistula
drainage, poor dietary intake of magnesium,
poor GI absorption of Mg, increased loss
from GI or urinary tract, pregnancy, chronic
diarrhea, hemodialysis, Hypercalcemia,
hypothermia, sepsis, burns, wound
debridement
Poor chloride intake because of a salt
restricted diet, IV fluid replacement without
electrolyte supplementation, loss of gastric
secretions, diuretic therapy, diaphoresis,
sodium or potassium deficiency or
metabolic acidosis, DKA, Addisons
Disease, rapid removal of ascetic fluid,
heart failure
Aldosterone deficiency, sodium depletion,
acidosis, trauma, burns, crush injuries,
hemolysis of red blood cells, severe
infection, potassium-sparing diuretics
(spironolactone), ACE inhibitors, betablockers, chemotherapy agents, digoxin,
heparin, NSAIDS, excessive amounts of
potassium, metabolic acidosis and insulin
deficiency decrease movement of K+ into
cells, Addisons Disease
Hemolyzed blood sample
Excessive vitamin D, immobility,
hyperparathyroidism, hyperthyroidism,
fractures, Hypophosphatemia, acidosis,
potassium-sparing diuretics, ACE
inhibitors, malignancy of bone or blood,
Vitamin D overdose
Excessive use of magnesium containing
antacids and laxatives, untreated diabetic
ketoacidosis (DKA), excessive
magnesium infusions, renal failure,
Addisons Disease, adreno-cortical
insufficiency, hemodialysis using
magnesium-rich dialysate, TPN with
excessive Mg, continuous Mg sulfate
infusion to treat certain conditions
Hypernatremia may cause
Hyperchloremia, increased water and
decreased chloride intake,
hyperparathyroidism, resp. alkalosis,
neurogenic hyperventilation, dehydration,
excessive NaCl intake, decreased
absorption of chloride from the intestines,
metabolic acidosis
Page 9 of 18
Fluids and Electrolytes
Normal Range
Phosphate (P):
2.5-4.5 mg/dL
Causes of elevation (hyper)
Renal failure, Hypoparathyroidism,
respiratory acidosis, DKA, necrosis,
rhabdomyolysis, trauma, heat stroke,
infection, over administration of
phosphorus supplements, laxatives or
enemas, excessive intake of Vitamin D,
insecticide / fertilizer poisoning, catabolic
states, neoplastic diseases
Page 10 of 18
Causes of Decline (hypo)
Respiratory alkalosis, hyperglycemia,
refeeding syndrome, malabsorption
syndrome, excessive use of phosphorusbinding antacids, diarrhea, laxative abuse,
diuretics, DKA, hyperparathyroidism,
hypocalcemia, malnutrition, starvation,
severe burns, alcoholism, Increased renal
excretion
Fluids and Electrolytes
Appendix C: Electrolyte Imbalances Signs/Symptoms & Treatment
Imbalance
Hypernatremia
Na > 145 mEq/L
Hyponatremia
Na < 135 mEq/L
Hyperkalemia
K> 5 mEq/L
Signs/Symptoms
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
Moderate:
K = 6.1 7.0 mEq/L
o
o
o
o
o
Severe:
K > 7.0 mEq/L
Treatment
Restless, agitation
Lethargy, seizures, coma
Weakness
Muscle twitching
Dry tongue fuzzy
Thirst
Dry skin & mucus membranes
Soft, sunken eyeballs
Flushed skin
Low grade fever
Confusion
Serum osmolality <280 mOsm/kg (dilute
blood)
Urine specific gravity <1.010
Abdominal cramps
Nausea & vomiting
Headache
Altered LOC-lethargy and confusion
Anorexia
Muscle twitching, tremors
Seizures
Depletional
dry mucous membranes,
orthostatic hypotension, poor skin turgor,
tachycardia
Dilutional
hypertension, rapid bounding
pulse, weight gain
o
o
Paresthesia (early sign) and irritability
Skeletal muscle weakness which may lead to
flaccid paralysis
Decreased deep tendon reflexes
nausea
abdominal cramping
diarrhea (early sign)
bradycardia, irregular pulse, hypotension,
decreased cardiac output and possibly
cardiac arrest
ECG Changes - tall, peaked T wave, flat P
wave, bundle branch block causing widened
QRS, prolonged PR interval, depressed ST
segment
Decreased arterial pH, indicating acidosis
o Reduce intake of potassium
o Administer loop diuretics (mild to moderate)
For severe cases:
o Calcium Chloride or Gluconate:
Administer 10% Calcium Gluconate (10
ml) or 10% Calcium Chloride (5 ml) IV
over 2 minutes as ordered (connect pt to
monitor)
Caution: 1 ampule of calcium chloride
has 3 x more calcium than calcium
gluconate!!!
Page 11 of 18
o
o
o
o
Varies with cause treat underlying cause
Replace vascular fluid loss with isotonic
solution
Replace gradually over 48 hrs
Avoid shifting H2O into brain cells
.45% NaCl
Restrict sodium intake
d/t Hypervolemia Fluid restriction, Oral
sodium supplements
o d/t Hypovolemia
isotonic IV fluids, high
sodium foods
o If Severe (Na <120 mEq/L) then
Hypertonic saline (3% or 5%) if symptomatic
(causes water to shift out of cells to the ECF
compartment) - administer slowly and in small
volumes
o Furosemide may also be administered
o
o
o
o
o
o
o
Bicarbonate: IV sodium bicarbonate (50
mEq) lasts 1-3 hrs
Insulin: 10 units regular insulin IV)
Glucose: D10% or D50%
Kayexalate/Sorbitol increase excretion
Dialysis
CBIGKD see big kid is the acronym
Fluids and Electrolytes
Imbalance
Hypokalemia
K < 3.5 mEq/L
Signs/Symptoms
o
o
o
o
o
o
o
o
o
o
Hypercalcemia
Serum Ca > 10.1
mg/dL
Ionized Ca > 5.3
mg/dL
o
o
o
o
o
o
o
o
o
o
Ionized Ca < 4.4
mg/dL
o
o
o
o
o
o
o
o
o
o
o
o
o
Hypomagnesemia
Mg < 1.5 mEq/L
o
o
Hypocalcemia
Serum Ca < 8.9 mg/dL
o
o
o
o
o
o
o
o
o
Treatment
Skeletal muscle weakness (especially in
legs)
Leg cramps
Flattened or inverted T-wave, depressed STsegment, U-wave
Constipation, ileus
Toxicity of digitalis glycoside
Irregular, weak pulse, palpitations
Orthostatic hypotension
Numbness (parasthesia), paralysis
Decreased or absent deep tendon reflexes
Tachycardia and tachypnea if respiratory
muscles become weak
Severe rhabdomyolysis
Anorexia, nausea, vomiting
Difficulty concentrating urine (polyuria)
Nausea, vomiting, anorexia, weight loss
Abdominal pain and constipation
Hypertension
Bone pain and bone loss
Kidney stones
Muscle hypotonicity and hyporeflexia
Confusion, lethargy, depression, altered
mental status
A-V block, short QT interval
Polyuria and extreme thirst
Muscle cramps
Hyperreflexia, tetany
Parathesia of face, fingers and toes
Chvosteks sign
Trousseaus sign
Anxiety, confusion, irritability
Laryngeal stridor
Prolonged QT interval, arrhythmias
Decreased cardiac output
Fractures
Tremors, twitching
o
o
o
o
o
o
o
o
o
o
o
o
Correct underlying imbalance
IV Calcium Gluconate more freq given
IV Calcium Chloride
Vitamin D supplement
O
ral calcium
Correct low magnesium/reduce phosphate
Skeletal muscle weakness
Altered LOC, CNS agitation, confusion,
depression
Seizures, vertigo
tetany, ataxia
Chvosteks and Trousseaus signs
tachycardia
increased BP
ventricular dysrhythmias
Vomiting
Increased/hyperactive DTRs
EKG changes: depressed ST, prolonged QT
Ventricular dysrhythmias include: PVCs, VF,
torsades de pointes
Emergency Situations: 1-2 g diluted in D5W
and given over 1-2 minutes
Nonemergency: 1-2 g diluted in 100-250 ml
of D5W over 2 hours.
Increase dietary intake of Mg
Page 12 of 18
Removing or preventing underlying cause
IV replacement 10-20 mEq/hr
Dietary high K+ and low Na+ diet
Oral replacement
Potassium-sparing diuretic, if needed
o Manage underlying cause
o Hydration encourages diuresis
o Loop diuretics
o Corticosteroids
o Bisphosphonates (if caused by malignancy)
o Plicamycin (antineoplastic)
o Decreased calcium intake
o HCO3 binds excess ionized calcium
Emergent dialysis
o
o
Fluids and Electrolytes
Imbalance
Hypermagnesemia
Mg > 2.5 mEq/L
Hypochloremia
Cl < 98 mEq/dL
Hyperchloremia
Cl > 108 mEq/dL
Signs/Symptoms
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
Hypophosphatemia
Phosphorus < 1 mg/dL
Hyperphosphatemia
Phosphorus > 6 mg/dL
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
o
Treatment
Decreased muscle and nerve activity
Hypoactive DTRs (hyporeflexia)
Generalized weakness, drowsiness and
lethargy
Facial parasthesia
Flushed appearance and diaphoresis
Slow, shallow, depressed respirations
Respiratory arrest
Nausea and vomiting
Hypotension, vasodilation
Arrhythmias and bradycardia
Coma
Hyperactive DTRs
Muscle hypertonicity and cramps
Neuromuscular irritability, tetany
Weakness
Resp. depression
Metabolic alkalosis
Hyponatremia and hypokalemia
CNS depression, lethargy, changes in
cognition
Metabolic acidosis
Decreased bicarbonate (Cl and HCO3
inversely related)
Tachypnea
Weakness
Arrhythmias, Kussmauls respirations,
decreased cardiac output, decreased LOC
that may progress to coma (with severe
metabolic acidosis)
Skeletal muscle weakness
Slurred speech
Dysphagia
Cardiomyopathy
Hypotension
Decreased cardiac output
Rhabdomyolysis
Cyanosis
Anemia, 2,3 DPG
ATP
Respiratory muscle weakness, cyanosis
Numbness, tingling, parasthesia
Hyperreflexia, tetany
Trousseaus/Chvosteks sign
Prolonged QT interval
Decreased mental status
Anorexia, nausea, vomiting
Arrhythmias, irregular heart rate, decreased
UOP, conjunctivitis, cataracts, impaired
vision
Muscle cramps & weakness
Page 13 of 18
o
o
o
o
o
o
o
Oral or IV fluids (to increase urine output of
excess Mg)
In an emergency calcium Gluconate (a Mg
antagonist) 10-20 ml of a 10% solution
Dialysis with Mg-free dialysate (for dialysis
patients)
Mechanical ventilation for severe cases
where respiratory depression present
Avoidance of Mg containing products
Increase dietary intake
Treatment of underlying cause of metabolic
alkalosis
IV saline solution with either NaCl or KCL
o
o
o
IV fluids to speed renal excretion of Cl
Restricted sodium and chloride intake
IV sodium bicarbonate for severe
Hyperchloremia
o
o
o
Oral supplements
Increased dietary intake
IV phosphorus (Potassium phosphate or
sodium phosphate)
o
o
Correct underlying problem
Low-phosphorus diet and drugs to decrease
absorption of phosphorus (aluminum,
calcium salts, Mg, phosphate binding
antacids
IV saline solution
Proximal diuretics to promote excretion
Dialysis if necessary
o
o
o
Fluids and Electrolytes
Imbalance
Etiology/Cause
Signs/Symptoms
Mild Fluid Loss:
Hypovolemia
o
o
o
o
o
Hypotonic fluid loss from extracellular
space
Bleeding (trauma, GI, etc.)
Vomiting, diarrhea
Neurogenic shock
May progress to hypovolemic shock if not
detected early and treated properly
Is caused by excessive fluid loss or third
space fluid shift
-Orthostatic hypotension
-Restlessness, anxiety
-Weight loss
-Increased heart rate
Moderate Fluid Loss:
-Confusion, dizziness, irritability
-Extreme thirst
-Nausea
-Cool, clammy skin
-Rapid Pulse
-Decreased urine output (10-30 ml/hr)
Severe Fluid Loss
-Decreased cardiac output
-Unconsciousness
-Marked tachycardia
-Hypotension
-Weak or absent peripheral pulses
-Cool, mottled skin
-Decreased urine output (<10 ml/hr)
Hypervolemia
o
o
o
o
o
o
o
Water
Intoxication
o
o
o
o
o
o
o
Excess isotonic fluid in extracellular spaces
Can lead to heart failure and pulmonary
edema, especially in prolonged or severe
Hypervolemia or in patients with poor heart
function
Mild to moderate/severe fluid gain equaling
a 5% to 10% or >10% weight gain
Excessive sodium or fluid intake
Fluid or sodium retention
Shift in fluid from interstitial space to
intravascular space
Acute or chronic renal failure
o
o
o
o
o
o
o
o
o
Tachypnea
Dyspnea, crackles
Rapid or bounding pulse
Hypertension (unless in heart failure)
Increased CVP, PAP, and PAWP
Distended neck and hand veins
Acute weight gain
Edema
S3 gallop
Excess fluid in the intracellular space from
the extracellular space
Causes increased intracranial pressure
(ICP)
May lead to seizures and coma
Syndrome of Inappropriate ADH (SIADH)
Rapid infusion of a hypotonic solution
Excessive use of tap water as an NG tube
irrigant or enema
Psychogenic polydipsia
o
o
o
o
o
o
o
o
o
o
o
Headache and personality changes
Confusion, irritability
Lethargy, Dulled sensorium
Nausea, vomiting, cramping
Muscle weakness
Twitching
Thirst
Dyspnea on exertion
Seizures & coma
Serum Na+ < 125 mEq/L
Serum osmolality < 280 mOsm/kg
Page 14 of 18
Fluids and Electrolytes
JOB AID
1. Body fluids serve as lubricants, carriers for nutrients, transport wastes,
regulate body temperature, medium for cell metabolism, and participate in
chemical and metabolic processes.
2. Fluids types include hypotonic, isotonic and hypertonic
3. Thirst is the simplest mechanism for maintaining fluid balance
4. The major extracellular electrolytes: Na+, Cl-, Ca+ and HCO35. The major intracellular electrolytes: K+, Mg+, Phosphate (P-)
6. Older adults are at risk for electrolyte imbalances because with age the kidneys
have fewer functioning nephrons
7. Phosphorus and calcium have an inverse relationship.
8. Bicarbonate and chloride are inversely related
Page 15 of 18
Fluids and Electrolytes
Posttest
Name: _____________________________________________
Date: ______________________________________________
Acknowledgement of Module Content review (Check appropriate response):
I have read the module contents: Fluids and Electrolytes
Yes
No
1. The only IV fluid that can be infused with blood is NaCl:
a.) True
b.) False
2. The main extracellular cation is:
a.) Calcium
b.) Potassium
c.) Bicarbonate
d.) Sodium
3. The recommended daily requirement of sodium for an average adult is:
a.) 2 grams
b.) 4 grams
c.) 5 grams
d.) 8 grams
Page 16 of 18
Fluids and Electrolytes
4. You have sent a blood sample to the lab for a chemistry panel. The potassium level
comes back at a critical value of 12. As you are critically thinking, what may be a
possible cause of this elevated value?
a.) The lab technician does not know how to work the machine
b.) Your patient drank an extra glass of orange juice at breakfast
c.) The sample you sent to the lab was hemolyzed
d.) You withdrew the blood from the running IV fluid line
5. Signs and symptoms of Hyponatremia include:
a.) Change in LOC, abdominal cramps, and muscle twitching
b.) Headache, rapid breathing, and high energy level
c.) Chest pain, fever, and pericardial rub
d.) Weight loss, slow pulse, and vision changes
6. A sign of Hypervolemia is:
a.) Increased urine output
b.) Clear, watery sputum
c.) Severe hypertension
d.) A rapid, bounding pulse
7. Populations at risk for dehydration include:
a.) Infants and the elderly
b.) Adolescents
b.) Patients with SIADH
d.) Young adults
Page 17 of 18
Fluids and Electrolytes
8. You are interpreting the 6-second ECG strip for your patient and notice that the Twave appears elevated/peaked. What electrolyte imbalance should you suspect?
a.) Hyponatremia
b.) Hyperkalemia
c.) Hypocalcemia
d.) Hypermagnesemia
9. A patient with a head injury has just been admitted to your unit for observation. The
IV fluid ordered is D5W at 100 ml/hr. What is your response to this order?
a.) Administer the IV fluid as ordered
b.) Use a filter when giving this IV fluid
c.) Check the patients blood sugar before administering
d.) Question this order since this patient has been admitted with a head injury
10. Medications to help treat severe Hyperkalemia include:
a.) Methylprednisolone and mannitol
b.) Mannitol and regular insulin
c.) Digoxin and diuretics
d.) 10% calcium gluconate and regular insulin
Page 18 of 18
You might also like
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- 2012-Fluid and ElectrolytesDocument192 pages2012-Fluid and ElectrolytesHarley Justiniani Dela CruzNo ratings yet
- Fluids and ElectrolytesDocument192 pagesFluids and ElectrolytesTeodora JoghiuNo ratings yet
- Fluids and ElectrolytesDocument49 pagesFluids and ElectrolytesMoon KillerNo ratings yet
- 10 CLS 382 443 Electrolytes I Na and Fluid Balance FINALDocument16 pages10 CLS 382 443 Electrolytes I Na and Fluid Balance FINALamalNo ratings yet
- Lec. 3 - Fluid and ElectrolyteDocument16 pagesLec. 3 - Fluid and Electrolyteمجيب سلطانNo ratings yet
- Electrolytes: Electrolytes Also Regulate Many Vital Processes in Our BodyDocument4 pagesElectrolytes: Electrolytes Also Regulate Many Vital Processes in Our BodyMichelle ViduyaNo ratings yet
- 2012-Fluid and ElectrolytesDocument192 pages2012-Fluid and Electrolyteskyuss2No ratings yet
- Major IntracelularDocument67 pagesMajor Intracelularfarooq shah shabbirNo ratings yet
- Homeostasis: The Kidneys' Role in Fluid and Electrolyte BalanceDocument56 pagesHomeostasis: The Kidneys' Role in Fluid and Electrolyte BalanceJennNo ratings yet
- Fluid & Electrolyte TherapyDocument38 pagesFluid & Electrolyte Therapyharjuna100% (1)
- S.No Table of Content Page NoDocument20 pagesS.No Table of Content Page NoTamilArasiNo ratings yet
- Fluid & Electrolytes Balance NewDocument21 pagesFluid & Electrolytes Balance NewPamela Ria Aguinaldo HensonNo ratings yet
- Fluids and Electrolytes FinalDocument50 pagesFluids and Electrolytes FinalOsego MokopotsaNo ratings yet
- IV FluidDocument49 pagesIV Fluidibrahimadnan040No ratings yet
- Fluid and Electrolyte Imbalance PDFDocument21 pagesFluid and Electrolyte Imbalance PDFShafaq AlamNo ratings yet
- Medical-Surgical Nursing 1Document28 pagesMedical-Surgical Nursing 1Maui Ting100% (1)
- Fluid and Electrolyte BalanceDocument41 pagesFluid and Electrolyte BalanceFev BanataoNo ratings yet
- Fluid Balance in Clinical PracticeDocument8 pagesFluid Balance in Clinical Practicefernando_vaz2010100% (1)
- Fluid and ElectrolytesDocument23 pagesFluid and ElectrolytesNanaNo ratings yet
- Tissue PerfusionDocument70 pagesTissue PerfusionAlexNo ratings yet
- Fluid Electrolyte and AcidBase BalanceDocument33 pagesFluid Electrolyte and AcidBase Balancemoncalshareen3No ratings yet
- Summary Notes For Studying Fluid and ElectrolytesDocument8 pagesSummary Notes For Studying Fluid and ElectrolytesCandace Mead100% (1)
- Fluid and Electrolytes (Acid Base)Document31 pagesFluid and Electrolytes (Acid Base)Diana TahamidNo ratings yet
- Fluid and Electrolyte - 2022Document147 pagesFluid and Electrolyte - 2022Lacangan, Thea YvonneNo ratings yet
- Fluids and ElectrolytesDocument131 pagesFluids and ElectrolytesGianna j100% (1)
- Metabolic & Acid-Base Balance: 1-When Lactic Acid Accumulates, Body Will Respond byDocument8 pagesMetabolic & Acid-Base Balance: 1-When Lactic Acid Accumulates, Body Will Respond byASGHAR ALINo ratings yet
- Basic Metabolic PanelDocument11 pagesBasic Metabolic PanelLaurenNo ratings yet
- PCH 201 L 10.11.12 13Document25 pagesPCH 201 L 10.11.12 13KellyNo ratings yet
- Lecture Notes 10, 11, 12 & 13: Water and Electrolytes HemostasisDocument25 pagesLecture Notes 10, 11, 12 & 13: Water and Electrolytes HemostasisKellyNo ratings yet
- Intravenous Fluid Therapy GuideDocument68 pagesIntravenous Fluid Therapy GuideMourian AmanNo ratings yet
- Fluid & Electrolyte TherapyDocument33 pagesFluid & Electrolyte Therapyhendra_darmawan_4No ratings yet
- Maintaining Fluid and Electrolyte HomeostasisDocument32 pagesMaintaining Fluid and Electrolyte Homeostasiskatrinasd100% (1)
- NSG IV Test 3Document4 pagesNSG IV Test 3Maria Phebe SinsayNo ratings yet
- Lecture 1 - Fluid & Electrolyre Balance 2021Document44 pagesLecture 1 - Fluid & Electrolyre Balance 2021عمار عاشورNo ratings yet
- Rudaina Alelyani MEV Assignment3.Document15 pagesRudaina Alelyani MEV Assignment3.Rudaina AlelyaniNo ratings yet
- BSFCR Cardio Case Group 1Document23 pagesBSFCR Cardio Case Group 1Qurrataini IbanezNo ratings yet
- Fluid and Electrolyte ImbalanceDocument82 pagesFluid and Electrolyte ImbalanceMinlik-alew Dejenie67% (3)
- Fluids & Electrolytes Acid/Bas Balance: DR Wael SadaqahDocument72 pagesFluids & Electrolytes Acid/Bas Balance: DR Wael Sadaqahdr wael sadaqaNo ratings yet
- Under The Guidance Of: Dr. B.Shashidharan. Professor and Chief Unit-III By, Dr. Henley Punnen AndrewsDocument63 pagesUnder The Guidance Of: Dr. B.Shashidharan. Professor and Chief Unit-III By, Dr. Henley Punnen AndrewsHenley AndrewsNo ratings yet
- Ch8 Fluid ElectrolyteDocument5 pagesCh8 Fluid ElectrolyteCatelia KulmanNo ratings yet
- Electrolyte, Acid-base and Blood GasesDocument33 pagesElectrolyte, Acid-base and Blood GasesBatrisyia BalqisNo ratings yet
- Ivfluidtherapytypesindicationsdosescalculation 130123090523 Phpapp01Document68 pagesIvfluidtherapytypesindicationsdosescalculation 130123090523 Phpapp01rainNo ratings yet
- Fluid and Electrolyte Balance GuideDocument12 pagesFluid and Electrolyte Balance Guideadadan100% (1)
- Fluid and Electrolytes: Ma. Medine L. Amorsolo RN ManDocument29 pagesFluid and Electrolytes: Ma. Medine L. Amorsolo RN ManMichael Baylon Dueñas100% (1)
- Fluids and Electrolytes A Fast and Easy Way To Understand Acid-Base Balance Without MemorizationDocument195 pagesFluids and Electrolytes A Fast and Easy Way To Understand Acid-Base Balance Without MemorizationNayely MoralesNo ratings yet
- Body Fluids and ElectrolytesDocument42 pagesBody Fluids and ElectrolytesQusaiBadr100% (1)
- Chapter 3 NFS 301Document45 pagesChapter 3 NFS 301solaveNo ratings yet
- Fluid & Electrolyte ImbalanceDocument11 pagesFluid & Electrolyte ImbalanceChino Paolo SamsonNo ratings yet
- Fluid and Electrolyte Balance: By: Rafael T. RodulfoDocument28 pagesFluid and Electrolyte Balance: By: Rafael T. RodulfoMarissa RodulfoNo ratings yet
- Basic of Fluid Therapy ImaDocument69 pagesBasic of Fluid Therapy Imal Made ArtawanNo ratings yet
- Fluid & Electrolyte Balance: Part 4: Regulation & MaintenanceDocument40 pagesFluid & Electrolyte Balance: Part 4: Regulation & MaintenanceMy MusicNo ratings yet
- Guideline, Management of HypernatremiaDocument9 pagesGuideline, Management of HypernatremiaLia Safitri Leloly100% (1)
- F and e ImbalanceDocument61 pagesF and e ImbalancegoldamierNo ratings yet
- Fluid Therapy for Dehydrated HorseDocument5 pagesFluid Therapy for Dehydrated HorsePrabina SahuNo ratings yet
- Common Electrolyte Disturbance Their Management and Anesthesia ConsiderationDocument65 pagesCommon Electrolyte Disturbance Their Management and Anesthesia ConsiderationagatakassaNo ratings yet
- Fluid and Electrolyte NewDocument54 pagesFluid and Electrolyte NewSelam Tesfaye ShebaNo ratings yet
- Fluid Therapy FinalDocument3 pagesFluid Therapy Finallaureeate100% (1)
- KidneyDocument13 pagesKidneyvitolavNo ratings yet
- Medical college Recruitment Exam questions (pgs 1-6Document10 pagesMedical college Recruitment Exam questions (pgs 1-6Arjun SinghNo ratings yet
- Memorandum PDFDocument62 pagesMemorandum PDFArjun SinghNo ratings yet
- Hydrabad Esic 19 MarchDocument34 pagesHydrabad Esic 19 MarchArjun SinghNo ratings yet
- AIIMS Nursing RecruitmentDocument5 pagesAIIMS Nursing RecruitmentArjun SinghNo ratings yet
- Hydrabad Esic 19 MarchDocument34 pagesHydrabad Esic 19 MarchArjun SinghNo ratings yet
- Esic 2nd Shift CorrectionDocument4 pagesEsic 2nd Shift CorrectionArjun SinghNo ratings yet
- Antidote Chart 2012 PDFDocument3 pagesAntidote Chart 2012 PDFRommel IrabagonNo ratings yet
- Aiims JodhpurDocument9 pagesAiims JodhpurArjun SinghNo ratings yet
- Chandigarh Esic Result 19 March 2016Document16 pagesChandigarh Esic Result 19 March 2016Arjun SinghNo ratings yet
- Drug InfoDocument11 pagesDrug InfoArjun SinghNo ratings yet
- Taa PDFDocument20 pagesTaa PDFArjun SinghNo ratings yet
- Antidote Chart 2012 PDFDocument3 pagesAntidote Chart 2012 PDFRommel IrabagonNo ratings yet
- ESIC Shift 3 2019 PaperDocument31 pagesESIC Shift 3 2019 PaperArjun SinghNo ratings yet
- Mass in A Flash 2.0 PDFDocument16 pagesMass in A Flash 2.0 PDFArjun SinghNo ratings yet
- ESIC Shift 3 2019 PaperDocument31 pagesESIC Shift 3 2019 PaperArjun SinghNo ratings yet