Professional Documents
Culture Documents
Notebook 10
Notebook 10
Uploaded by
api-3298066820 ratings0% found this document useful (0 votes)
11 views14 pagesOriginal Title
notebook 10
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views14 pagesNotebook 10
Notebook 10
Uploaded by
api-329806682Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 14
Notebook: Fluoroscopy Historical Timeline
Name:~« 7" Z
Date Occurrence
1895 Roentgen discovered x-rays- he placed his hand
between the tube and screen and saw his fingers
3/3/1896 & 4/18/1896 1 reports of possible bodily damage by x-
i rays & 1° skin effects noticed,
July of 1896 1* protective x-ray device created: heavy
glass plate to protect the eyes.
1896 More contributors to this technology- Salvioni of
Italy, MeGie of Princeton, and Thomas Edison
(used Clarence Daly's hand)
July of 1896 Al filter used as protection device.
May of 1898 Dark adaption prior to fluoroscopy
suggestion (allows eyes to adapt to dark
light).
October of 1904 Clarence Dally is the 1* death of an x-ray
pioneer from cumulative exposure.
1907 Photographic plate carried in pockets for
monitoring exposure by Wagner.
1915 British Roentgen Society adopts protection
recommendations
1922 Film badges for personal monitoring,
developed.
1937 Irving Langmuir patented the image intensifier
1948 4.W Caltman improved upon the design so the
image brightness increased 1000 times
1953, Westinghouse Company manufactured the first
commercial image intensifier
1940s Fluoroscopy used to x-ray permits
1950s Fluoroscopy used for shoe fitting- the salesman
would look from above while customer put foot
on «ray source
1950s cont'd The doctor looked directly through the screen in
a darkened room but was radiation dose was
extremely high |
http://www.physics.isu.edu/radinf/timeline.
htm
Notebook: Fluoroscopy Historical Timeline
Name: ~
Ina narrative, list and describe the terminology of basic visual physiology and determine its
importance in radiology image illumination.
°
Photopic vision: “daylight vision”. This is the current way that fluoroscopy is visualized.
Scotopic vision: “nighttime vision”. A dark room or special goggles help enhance this
type of vision; this was where ‘dark adapt’ came from (fluoroscopists would sit in a dark
room for 15 mins to allow their eyes to adapt which allowed for the rods in the
periphery of the retina to activate.
Ullumination that the eye can see is measured in lumens or cd/m2 (lux).
‘Anatomy and function of the eye:
* Cornea: light passes through the transparent protective coating of the eye.
© Lens: shaped disc that focuses the incoming light into the retina,
‘Iris: this anatomy is b/t the cornea and the lens and acts like a diaphragm as it
adjusts to control the amount of light coming into the retina.
‘© Bright light: iris contracts to limit the incoming light.
‘© Low light: iris dilated to allow more light to enter.
Rods (100 million) and cones (6 million) are embedded in the retina
* Rods are only in the periphery of the retina and are sensitive to low light. They
cannot respond to intense light (2 lux). This is where nighttime and dim vision
occurs- scotopic.
© Periphery allows opjects to actually be visualized,
© Cones are in a ‘pocket’ called the fovea centralis. They are less sensitive to light
and can respond to intense light (100 lux). Cones are for daylight vision and are
Aphotopic, This is also where color is formed.
oN bt
Part B: List all the components slide of mobile and fixed fluoroscopy, add a brief description of
its function or purpose.
Mobile
1._ Display monitor: high-resolution monitor to display the images.
TV camera: uses a CCD to capture the image prior to it being sent to the display monitor.
3. Image intensifier (detector): converts x-rays into visible light image. Primary beam exits
the patient and hits the input window of the Il (which is made of a fluorescent screen).
X-ray photons are then absorbed and light photons are emitted and captured by the
photocathode,
Table top to detector
Table top: radiolucent carbon fiber material and has weight limit between 300-600Ibs.
Source to table top
Linear collimation: collimates linearly; used to reduce scatter and improve visualiza
of detail through improved contrast resolution.
Iris collimator: collimates circularly.
X-ray tube (source): high voltage generator and x-ray tube where electrical energy is
converted into the beam. Radiation output can be either continuous or pulsed. AEC’s
maintain the radiation dose per frame.
10. Patient
ee
Fixed
1. TV/LCD: high-resolution monitor to display the images.
Video camera: uses a CCD to capture the image prior to it being sent to the display
monitor.
3. Image intensifier: converts x-rays into visible light image. Primary beam exits the patient
and hits the input window of the Il (which is made of a fluorescent screen). X-ray
photons are then absorbed and light photons are emitted and captured by the
photocathode.
Anti-scatter grid: reduces scatter.
Patient
Filter: reduces the entrance skin dose (ESD).
Xray tube: source of the radiation beam
nove
Part C: Describe the flow of electrons in a narrative or with bulleted statements beginning at
the source through the image intensifier.
Page 537
1
One photon (at least 50keV) enters input fluorescent screen at the bottom of the glass
envelope.
Fluorescent screen then converts the one photon into 2,000 light photons.
The light photons go through the photocathode and are then converted to electrons
that are negatively charged.
The negatively charged photoelectrons are then repelled by the negatively charged
electrostatic lens that lies within the glass envelope. This repulsion directs the electrons
towards the positively charged anode.
Those electrons are shot through the output fluorescent screen to produce more light
Photons that ends up creating the image (the one original photon has now been
Converted into 200,000 light photons which leads to the resulting image)
1, While using a image intensifier with a 10/7/5 diameters, which size is best for contrast
resolution and why? Which one is best for spatial resolution and why? Which one has
the largest field of view?
10: contrast increased, largest field of view, focus is closest to the phosphor
5: contrast decreased, best spatial resolution
2. Describe minification gain and the relationship with increasing input phosphor size, kVp,
mA, output phosphor size, and tube voltage.
Minification gain: pg. 539 photocathode is large {image is smaller- output phosphor is smaller)
The bigger the input phosphors the more minificaiton and brighter the image is with more light
photons at the output screen.
kVp: if kVp is upped by 15% thus doubling the amount of energy coming through, everything is
increased. More pt dose and no relationship to minificaiton gain,
mA: as kV/p is increased, the mA lowers and visa versa. No relationship to minificaiton gain.
Output phosphor (measurement of luminous intensity) size: the smaller the output phosphor
the more minificaiton there is and visa versa (minificaiton gain= ratio the areas of the input
photocathode to the output florescent screen: geometric size difference).
Tube voltage: no relationship, more power in the tube the brighter the image but no one cares.
This affects flux gain.
3. Describe what occurs when the image intensifier is operated in the magnification mode
as it relates to contrast resolution, spatial resolution, patient dose, the relationship of
the focal point between the input phosphor and the output phosphor.
Magnification mode is the ability of multiple diameters to be made available within one image
intensifier. The size is chosen by increasing the voltage to the electrostatic focusing lenses.
When the voltage is increased, the electron stream is “tightened” or made smaller, and these
are the only electrons that interact with the output phosphor screen. This tightening changes
the focal spot, moving it away from the output screen
Mag mode increases technique due to the closer proximity of the focal spot; spatial resolution
will be increased due to the closer focal spot.
Contrast is decreased when magnification is increased because focal spot is moved closer to the
source of the image (photocathode)- image is spread over 2x the area and therefore contrast
and density are lost.
Equations used in fluoroscopy
Flux gain = number of output light photons
Number of input x-ray photons
Brightness gain = Minification gain x Flux gain or use the conversion factor equation.
Minification on gain = (direst)?
(output)?
Conversion factor = output phosphor illumination (cd/m?|
Input exposure rate (mGy./sec.)
Magnification factor = mode 2 in multifield Image intensifier
Mode 1
‘New ESD = Original input screen size X Entrance Skin Dose
‘New input screen size
4. What is the brightness gain for a 17- em image intensifier tube with a fl
and a 2.5 cm output phosphor? x
in gain x flux gain: 17x2.5 = 42.5
gain of 120
5. A 23/15/10 (ratio diameter) image intensifier is uSéd in the 10cm mode. How much
higher is the patient dose using this mode compared to using the 23 cm mode?
Principal: when using the magnification mode, the minification gain is reduced, so fewer
photoelectrons are hitting the output phosphor. This creates a dimmer image. To
compensate for the magnification mode (maintain the same amount of brightness), the
tube mA is increased.
The increase in dose to the patient when changing from 23 cm to 10 cm is equal to the
ratio of the input phosphor diameter to the diameter used in magnification mode.
23°2/1092= 5.29
6. What is the change is dose (how much higher) when switching from a 23cm FOV to a
17cm FOV?
Use same principal as in question 5
2392/1792= 1.82 A
7. A photofluoroscopic image is obtaining using the technical factors of 80 kVp in the 15cm
mode without a grid. He measured entrance skin dose (ESD) is 0.5. mGyt What ESD
would be expected if the 25cm mode were used?
Original input screen size X ESD = New ESD
New input screen size iy
1542/2542= .36x.5=0.18
DOSE 15 SQUARED (=AREA)
8. A23cm image intensifier has an output phosphor size of 2.5cm and a flux gain of 75.
What is the brightness gain? o&
2342/2.592= 33-6.25 x (75) =247968.75 \ Na 129
Wart 1S = L34t
O
9. Create a scenario using one of the equations above with the specific factors required. Be
sure to show your work and include the answer.
What is the brightness gain for a 22cm image intensifier tube with a flux gain oft 115 nd
a 3.0 cm output phosphor?
Magnification gain: (22)42/(3)42= 53.53
Brightness gain: 53.53x115= 6155.95 ed/mR — c/) .
1. Describe how the image changes as FOV-changed phantom to a thin portion. Include
noise, technical factors
3. Noise Assown et tatlang dse changed, Here is
Nose when going, toe SO part
b. Technical Factors
Also: ~ \y--due—-to- ~decressed Size
cc. Contrast resolution : peau a sista
Trinner port > lower Oi, So lotwer ldagneBicatiah his Lor
Contrast, bot also thine adefouy w/redua's foarcrast
due PEsbieck. Conkast
d. Brightness
Wen “FOV is Smaller Lrigitress Stays the Same oS teh. factors
ole abiotted to Verp Unifottuniby wf tmagsd toll mation [ehoage ie ov
2. Explain how ABS worked in relation to magnification, and dosimetry reading in regular
and pulsed mode. pee
FOV1 Regular Pulsed © SYune pet Sec Cam’ taceh. peti
& ) SOV IS Compressed,
Mee exposoa ae 4 (unless hegpr wl isoed) 2OY FS Cont
A dain
5 Less exposore
Fov2 Abd: kth +
liven WA ot :
Name.
3. What changes occurred in the image when collimators were open versus closed, in
relationship to brightness (density), noise/fog, and contrast resolution.
AS cllination fone Aedhnigue ts modad
Boosh + iN
Aitsolvion in image,
Name.
Po
3. Describe the processed CR images and the exposure index, or film density using a
densitometer, Write your conclusion about the findings,
Location 1:
Location 2:
Location 3:
Location 4:
Name.
Lab analysis:
1. Describe how the image changes as the unit is moved from a thick part of the phantom
toa thin portion. =
a, Abdomen
Co Hip Zom-tedaniad , Thedwigve - Sor KN COtCN.. Choam. is Narrowed afin (oi Coca
OPA IS Chenging, Mom. cokput bow to wk pbosftor)
it Extremity f\b5 i (oud dite
Un vdose
2. Explain how ABS worked and what happened to the technical factors. Describe what
‘was seen at varying kVp and mA settings.
AB Woh ko change Lngtters ab atatuie location henge
las) cecors
Eo Ughap hee 65 fark Hielouns charg rity ABS.
AB toh £ brights ineneesed yf thea in tees Ractrs
wD Briqtas + nd el. Raters
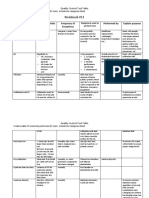
Create a chart using the Table below to compare Digital Fluoroscopy Equipment and Image Intensified
Fluoroscopic Equipment. Include information related to patient dose, contrast resolution, spatial
resolution, size of the component, distortion, tube mA’s.
Digital Fluoroscopy Equipment Components
Image Intensified Equipment Components
CCD: replacement for the “camera tube”; light
collector
Video camera
Flat panel detector: either direct capture
configured with amorphous selenium or indirect
capture that uses cesium iodide (used as
scintillator) amorphous silicon (is the
photodetector)
Light out
TFT array: operates the same way as in static
imaging
‘Output phosphor
Faster image acquisition speed
Focusing electrodes
‘Smaller size, distortion not seen
Input phosphor
Better contrast
Magnification requires higher technical factors
and x-ray exposure
‘50% lower patient dose
‘Small dynamic range
Post processing
xray detector is not sensitive
[Large dynamic range
&
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5819)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Notebook 11Document5 pagesNotebook 11api-329806682No ratings yet
- Completed Notebook 7Document3 pagesCompleted Notebook 7api-329806682No ratings yet
- Rte 141 Notebook 13 DoneDocument1 pageRte 141 Notebook 13 Doneapi-329806682No ratings yet
- Rte 141 Notebook 5 DoneDocument2 pagesRte 141 Notebook 5 Doneapi-329806682No ratings yet
- Rte 141 Notebook 1 DoneDocument3 pagesRte 141 Notebook 1 Doneapi-329806682No ratings yet