Professional Documents
Culture Documents
Critical: Sepsis: Hypothesis
Uploaded by
Christmando Sapria AbrianOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Critical: Sepsis: Hypothesis
Uploaded by
Christmando Sapria AbrianCopyright:
Available Formats
critical care
A New for
Sepsis: Hypothesis
Pathogenesis of the Disease Process*
Roger C. Rone, MD, PhD (honorary), Master FCCP;f Charles J. Grodzin, MD;
and Robert A. Balk, MD, FCCP
and its innovative
(CHEST 1997; 112:235-43) sepsis sequelae, therapies were
and clinical trials
developed were
begun. Although
Abbreviations:
CARS=compensatory anti-inflammatory re
these trials were of the most advanced experimental
sponse syndrome; IFN^interferon; IL=interleukin; MARS = design, double-blind, randomized, and placebo con
mixed
antagonists response syndrome; MODS=multiple organ trolled, all such trials thus far have failed to
sepsis
dysfunction syndrome; SIRS=systemic inflammatory
show efficacy or
have had harmful, ambiguous, or
response syndrome; TNF=tumor necrosis factor
negative results.4 Pharmacologic interventions to
infection.
Sepsisis the
systemic response to severe
date have not improved the outcome in sepsis and
SIRS. The trials have shown how effective certain
The incidence of sepsis continues to increase. agents can be at the cellular or animal model stage
and its the of
Sepsis sequelae are
leading causes
but how ineffective these same agents can be when
death in medical and surgical ICUs.12 According to applied in clinical trials.4
the Centers for Disease Control and Prevention, the While trials addressed the proinflammatory phase of
incidence of sepsis continues to increase and is now sepsis and SIRS, there was no evidence that the
was dominant when
the third leading cause of infectious death (Fig 1). proinflammatory phase drugs
and its
Sepsis sequelae represent progressive were given. This may mean more to us as we learn
of the illness.a to
more about
compensatory anti-inflammatory re
stages same
systemic response
infection mediated via
macrophage-derived cyto-kines that sponses and mixed proinflammatory and anti-inflam
in the human with The
target end-organ receptors in
response to
matory responses sepsis.
failed initial clinical trials tested efficacy of clinical
injury or infection. Much confusion has
trials for sepsis and provided some insight into the
existed
of the cascade.
regarding terminology for sepsis. An American Col complexity immuno-inflammatory
of Chest of Critical Care This article looks at what we know about this com
lege Physicians/Society
Medicine Consensus Conference3 held in 1991 plex immuno-inflammatory cascade, and a new
hy
to relate it to
agreed to a new set of definitions that could be pothesis sepsis.
readily applied to patients in different stages of
sepsis (Table 1). New discoveries made in the last
several years have validated the conceptual appro and
Sepsis, SIRS, CARS, MARS
priateness of these terms, which has led to wide
acceptance. However, new discoveries also suggest When the American College of Chest Physicians
that we need to push these concepts further. and Society of Critical Care Medicine convened a
The
pathophysiologic state of the
systemic inflam Consensus Conference in 1991 to address the prob
matory response syndrome (SIRS) has been studied lem of confusion over use of proper terms and
terms
definitions, the bacteremia, septicemia, sepsis,
extensively. We characterize SIRS as an abnormal sepsis syndrome, and
septic shock were
being used
reaction in remote
generalized inflammatory organs
almost interchangeably, which led to confusion and
from the initial insult. When the process is due to an
terms
imprecise understanding of sepsis and related disor
infection, the sepsis and SIRS are
synony
ders. Members of the Consensus Conference agreed
mous. On the basis of the current understanding of
to a new set of definitions that could be readily
to in different of
*From
the Department of Internal Medicine, Sections of Pulmo applied patients stages sepsis:
nary and Critical Care Medicine, Rush-Presbyterian-St. Luke's bacteremia, SIRS, sepsis, severe
sepsis, septic shock,
and
Medical Center, Rush Medical College, Chicago. multiple organ dysfunction syndrome (MODS).
Deceased.
Manuscript received April 28, 1997; accepted April 29.
CHEST/112/1 /JULY, 1997
235
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
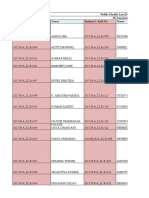
1980
? 1992
Lung AIDS Sepsis Urinary Heart Hepato TB
tract biliary
Figure 1. Leading causes
of infectious death according to the Centers for Disease Control and
Prevention.
We now to add the anti- in those disorders that often associated with
propose compensatory are
and the of
inflammatory response syndrome (CARS), organ dysfunction, pattern systemic cytokine
mixed release is dissimilar. How, then,
antagonists response syndrome (MARS) to can SIRS and
this set of clinical definitions (Table 2).
MODS be
Multiple organ dysfunction
trauma
occurs in about 30% of
explained?
patients with sepsis, and it also can be found in
patients, patients with acute pancreatitis and
other
diseases such as systemic vasculitides, and in
The Cytokine Cascade
burn victims.59 How7 of
The systemic response to infection is mediated via
dysfunction multiple organs can
be such disorders the that end-
produced by disparate puzzled macrophage-derived cytokines target
clinicians and investigators for Almost a de in to infection.
years. organ receptors response injury or
cade
ago, it was suggested that multiple organ The infection or is a
inflammatory response to
injury
dysfunction may result not from infection per se, but highly conserved and regulated reaction of the or
from a
generalized inflammatory reaction.10 Evi ganism. After
recognition that a
response is
required,
dence
today suggests that a massive inflammatory the
organism (eg, a human
being) produces soluble
reaction
resulting from systemic cytokine release is
protein and
lipid proinflammatory molecules that
the common
pathway underlying multiple organ activate cellular defenses, then produces similar
dysfunction. Also, it is now
known that most patients anti-inflammatory molecules to attenuate and halt
the Molecules known or
have evidence of dysfunction in one or more organs proinflammatory response.
before failure presumed at this time to be
proinflammatory and
anti-
long organ develops.
listed in Table 3.
Unfortunately, the more we learn about this in inflammatory are
Presumption
of is based data of it is
flammatory response, the more difficult it becomes activity on
varying quality;
to
pinpoint a
specific cytokine, or a
specific reaction,
likely that some molecules will eventually drop from
the "cause" of SIRS. Indeed, it has become clear
as
that is
this list, and others will be added.
cytokine release a
normal, healthy part of the is the
Normally cytokine response regulated by
to insult or infection.
body's response Cytokines are
intricate network of and anti-in
proinflammatory
and of
highly pleiotropic, they appear capable pro
flammatory mediators. The initial inflammatory re
different effects the
ducing markedly depending on
sponse is kept in check by down-regulating produc
hormonal milieu.
nearby Furthermore, the body has tion and
counteracting the effects of cytokines already
a network of
highly complex, rigidly regulated recep produced. The picture that emerges from analysis of
tor and other that
antagonists regulatory agents data from
patients with
sepsis is that a
mixture of and anti-in
continuously modulate the effects of cytokine re complex proinflammatory
lease. Adding to our confusion is the fact that flammatory molecules
may be
present.1112 Standard
systemic cytokine release can occur in a variety of models of
disorders without leading to organ dysfunction. Even
pathophysiologic sepsis
do not such
explain a
picture.13
236 Critical Care
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
Table 1.Standard and Table and
Definitionsfor Sepsis Organ 2.Proposed Definitionsfor Sepsis Organ
Failure Failure
Terminology Definition CARS HLA-DR on monocytes <30% and diminished
of
ability monocytes to
produce inflammatory
Infectk Microbial phenomenon characterized by an
IL-6
to the of cytokines, such as
TNF-a or
(Kox WJ, Bone
inflammatory response presence
RC, Krausch D, et al. Arch Intern Med 1997; 157:
the invasion of
microorganisms or
normally
389-93).
sterile host tissue by those organisms.
Bacteremia Presence of viable bacteria in the blood. MARS Features of SIRS in a patient with CARS.
SIRS The
systemic inflammatory response to a wide
variety of severe
clinical insults, manifested by
two or more
of the following conditions: (1)
temperature >38C or
<36C; (2) heart rate proinflammatory reaction (SIRS) or a
compensatory
rate >20 A
>90 beats/min; (3) respiratory anti-inflammatory reaction (CARS) will ensue.
breaths/min or PaC02 <32 mm Hg; and (4)
WBC count >12,000/mm3, <4,000/mm3, or rangeof clinical sequelae may then follow. These
>10% immature (band) forms. sequelae can be remembered by using the mne
Sepsis The
systemic inflammatory response to infection.
monic CHAOS (Fig 2).
In association with infection, manifestations of Currently, our concept of the pathogenesis of
sepsis are the same as those previously defined sepsis is undergoing evolution, based in part on
for SIRS. It should be determined whether
of the direct
animal models or human exposure to endotoxin, in
they are a
part systemic response
hopes of finding a "magic bullet" for sepsis.4 The
to the presence of an infectious process and
magic bullet to definitively treat sepsis has been
represent an acute alteration from baseline in
the absence of other known causes for such vigorously sought, but has not been found. More
Severe sepsis abnormalities.
associated with
than a dozen pharmacologic magic bullet candidates
Sepsis organ dysfunction,
have failed to improve outcome of sepsis in random
hypoperfusion, or
hypotension. Hypoperfusion
ized, placebo-controlled clinical trials. Magic bullet
and perfusion abnormalities may include, but
are
not limited to, lactic acidosis, oliguria, or an trials were based on an assumption that antagonism
acute alteration in mental status. of a single proinflammatory mediator can modulate
shock
Septic A subset of severe sepsis and defined as sepsis-
the cascade of events that constitutes sepsis in a
induced fluid
hypotension despite adequate heterogeneous group of patients. Hindsight indicates
resuscitation along with the presence of perfusion
abnormalities that include, but are
not
that this was simplistic, but evidence available at that
may
time was
limited to, lactic acidosis, oliguria, or an interpreted to suggest that such a strategy
acute alteration in mental status. Patients should be successful. Similarly, available evidence suggested that neutralization of endotoxin would
receiving inotropic or vasopressor agents may
be the time
no
longer hypotensive by they prevent the
proinflammatory response, but clinical
manifest hypoperfusion abnormalities or organ
trials of monoclonal antiendotoxin antibodies were
dysfunction, yet they would still be considered
not successful.1518 The design of clinical trials man
to have septic shock.
MODS Presence of altered organ function in an acutely dated that patients enrolled in the trial meet some
criteria for
ill patient such that homeostasis cannot having sepsis, ignoring any preexisting
be maintained without intervention.
Sepsis-induced condition that might have induced proinflammatory
A systolic BP <90 mm Hg or a reduction of >40 mm
mediators.19 Animal studies suggested that an endo-
hypotension Hg from baseline in the absence of other should be before or
toxin-neutralizing drug given shortly
for
causes
hypotension. after the inflammatory stimulus, but interspe-
cies variation in immunomodulation and other dif
These mediators initiate overlapping processes
ferences in animal models compared to the critically
ill ICU patient make it difficult to generalize animal
that directly influence the endothelium, cardiovascu
lar, hemodynamic, and coagulation mechanisms. The
studies to humans.20
release of many of these vasoregulators is often local.
of the Why Previous Theories Were Inadequate
Evolving concepts septic response give more
to the of local
weight importance cytokine produc
tion, not in
contradistinction to
systemic production We have understood that a massive inflammatory
but as of the total reaction underlies both SIRS and MODS, but now we
part septic-response picture.414
The duration of illness also may alter the mix of must understand that this reaction is only half the
mediators, leading to a state of metabolic disorders picture. It is now clear that quite rapidly after the
in which the body has no control over its own first proinflammatory mediators are
released, the
inflammatory response. If balance cannot be estab body mounts a
compensatory anti-inflammatory re
lished and homeostasis is not restored, a massive
action to
(CARS) the initial proinflammatory re-
CHEST/112/1 /JULY, 1997
237
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
Table 3.Partial List and Molecules
ofProinflammatory Anti-inflammatory
Molecules
Proinflammatory Anti-inflammatory Molecules
TNF-a Thromboxane IL-1 ra
IL-10 Platelet activating factor IL-4
IL-2 Soluble adhesion molecules IL-10
IL-6 Vasoactive
IL-8 neuropeptides IL-13
IL-1
IL-15 Phospholipase A2 Type II receptor
Neutrophil elastase Tyrosine kinase Transforming growth factor-p
Plasminogen activator inhibitor-1 Epinephrine
IFN-7 Free radical generation Soluble TNF-a receptors
Protein kinase
MCP-1* Neopterin Leukotriene
B4-receptor antagonism
MCP-2
CD14 Soluble recombinant CD-14
LPS
Leukemia inhibitory factor Prostacyclin binding protein*
(D-factor) Prostaglandins
^MCP^monocyte chemoattractant protein; LPS=lipopolysaccharide.
matory mediators and homeostasis is restored (Fig
The reaction be as
sponse.13 anti-inflammatory may
sometimes even In some
large as, and larger than, the proin 2). patients, however, a
variety of forces
The of this anti-inflam in
flammatory response. goal conspire to upset this balance, resulting SIRS and
matory reaction is to down-regulate synthesis of
MODS.
proinflammatory mediators and to modulate their The theories put forth to explain the development
effects, thereby restoring homeostasis. of SIRS have generally not taken this compensatory
It has recently become possible to differentiate
CARS from SIRS anti-inflammatory reaction into consideration. Many of
ongoing immunophysiology. the anti-inflammatory mediators were discovered
Zedler et al21 detailed a technique of stimulating and characterized only in the last few years, and to
peripheral blood mononuclear cells from severely
some extent, this may have led to overstatement of
injured burn patients for the purpose of cell surface the media
and intracellular
dangers presented by proinflammatory
antigen staining interferon-gamma
tors. It might almost be said that proinflammatory
(IFN-7) and interleukin-4 (IL-4) detection. IL-4, an
anti-inflammatory cytokine, was
found in excess
(el mediators became "bad guys," without taking into
in account that excessive levels can be harmful, but
evated 16-fold) the presence of downregulated
IL-2 and IFN-7. IL-4 thus served as a marker for the lower levels are required to combat pathogenic
"THrTH2 switch," a
major characteristic of the organisms and to
promote healing.
to T In Most of the evidence for the role of proinflamma
CARS response injury (TH is the helper cell).
most healthy persons, the body is able to achieve a tory mediators in the pathogenesis of SIRS and
balance between and anti-inflam- MODS came from studies using animal models,
proinflammatory which endotoxin in
experiments or
proinflammatory
into
mediators were
injected human volunteers, and
of levels of media
analysis serum
proinflammatory
C Cardiovascular tors in patients with sepsis, burn injury, or other
compromise (usually manifesting
as
severe
injuries (Fig 3). We now know that these
shock; in this setting SIRS predominates).
studies may not truly reflect what happens in criti
cally ill patients with sepsis or
SIRS. As noted earlier,
H Homeostasis (return to health; this
represents a balance of SIRS and a marked interspecies variation in cytokine release
CARS).
makes it difficult to extrapolate results of animal
A SIRS nor
Apoptosis (neither CARS predominates). studies to humans. More importantly, these experi
ments were performed on healthy animals and gen
or erally included a relatively short observation peri
O Organ dysfunction (single multiple;
od.22 Studies of human volunteers were performed
SIRS in
healthy subjects; the amount of stimulus
injected
predominates). was
sublethal; and, again, the follow-up period was
of the
S Suppression immune system (anergy
and/or increased susceptibility to
brief.23 In contrast, SIRS and MODS develop over
ill or
infection; CARS predominates).
time in
severely injured patients who have
disorders.24
multiple preexisting
Figure 2. Mnemonic of CHAOS. Serum levels of immunomodulating mediators
238 Critical Care
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
result of an immediate insult such as trauma and not
Infection
of condition such
a
consequence a
preexisting as
pancreatitis.19
Endotoxin and
other microbial toxins
\ Relating Clinical Responses
Some patients with sepsis, extensive burns,
sive traumatic injury, or other severe insults show
Cascade
to Cytokine
mas
little or no evidence of a systemic inflammatory
l
reaction or
organ dysfunction, although their recov ery
be because of the of their
may protracted severity
underlying illness. In three other categories, how
ever, are patients with sepsis or severe
other insult
state who develop the following: a mild form of SIRS and
Proinflammatory some evidence of dysfunction in one or two organs
with cytokine release early in their clinical course that usually resolves
rapidly; a massive systemic inflammatory reaction developing
and rapidly after the initial insult, with death
other often within few from
proinflammatory following days profound
a
shock; and a less severe initial course, but marked
mediators deterioration several days or more after the original
l
insult, with outright failure of one or more
organs
and death in some but not all patients.
Clinical trials have usually excluded patients with
mild of
symptoms organ dysfunction or
symptoms
Sepsis/SIRS that last for <24 or 48 h. While this was perhaps
believed necessary to the design and conduct of
I
these trials, the underlying hypothesis may have
been faulty. We should have looked better at the
proinflammatory and anti-inflammatory response to
severe insult and asked whether the inflammatory
was of an
response appropriate magnitude and if it
Shock and
multiorgan was
appropriately down-regulated. When down-reg
dysfunction and ulation is not adequate, is there a progression of
severities? Rangel-Frausto et al28 published the first
possible large study to confirm that
patients progress through
death stages of the septic process, from mild to severe.
Figure 3. Old for A New Theory of SIRS, CARS, MARS, and
paradigm sepsis.
MODS
Immunomodulation is a complex, overlapping net
of because immu-
present problems interpretation work of interactions among agents that work to
noassays can
detect only free, circulating mediators,
gether to overcome severe assaults on the body.
not mediators bound to cells or receptors.12'2526 Paradoxically, they also work to the
body's disadvan
Therefore, the amount of mediator reported may not
tage and cause the disruptions we call SIRS and
MODS. We have
be the amount present. Bioassays used to measure the presented a hypothesis-based ex planation
for the events ob in
functional activity of cytokine often lack speci apparently paradoxical served the
in the
ficity and may over-report the amount of mediator critically ill (Fig 4). The five stages
present.27 Other points to consider are the following: development of
multiple organ dysfunction are
(1) analysis of serum level is usually performed once
as follows: (1) local reaction at the site of injury or
a
day or
less often, although mediator release is
infection; (2) initial systemic response; (3) massive
most
phasic; and (2) analyses have assumed that the systemic inflammation; (4) excessive immunosup-
of mediators is direct
presence proinflammatory a
pression; and (5) immunologic dissonance.29
CHEST / 112 / 1 / JULY, 1997
239
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
Initial insult
(bacterial,
viral, traumatic,
thermal)
Systemic spillover of Systemic spillover of
pro-inflammatory mediators anti-inflammatory mediators
Cardiovascular Homeo Apoptosis Organ Suppression
compromise stasis (cell death) dysfunction of the
(shock) immune
system
SIRS CARS and Death with SIRS CARS
predominates SIRS minimal predominates predominates
balanced inflammation
Figure 4. New
concepts for the clinical sequelae of sepsis, SIRS, CARS, and MARS. (This figure is
an
adaptation of Figure 1 by Bone RC. Sir Isaac Newton, sepsis, SIRS, and CARS. Crit Care Med 1996;
24:1125-28.)
substances12-30'32 work to diminish monocytic major
1
Stage histocompatibility complex class II
expression, im
Prior to development of SIRS or MODS is some pair antigen presenting activity, and reduce the
insult such as a nidus of infection, a traumatic injury of cells to
ability produce inflammatory cytokines.
(including a
surgical wound), a
burn injury, or
that release of of Local levels of both proinflammatory and anti-in
pancreatitis prompts a
variety mediators can be
flammatory substantially higher
mediators in the microenvironment. The body's ini
tial
response is to induce a proinflammatory state in than are later
found systemically33,38 (Table 3).
which mediators have multiple overlapping effects
2
designed
whatever
to limit new damage and to ameliorate Stage
damage has already occurred. Theydestroy If the
original insult is
sufficiently severe, first
damaged tissue, promote the growth of new tissue, proinflammatory and later
anti-inflammatory media
and combat pathogenic organisms, neoplastic cells, tors will appear in the systemic circulation via a
and of mechanisms. The of
foreign antigens20-24 (Table 3). variety presence proinflam
A
compensatory anti-inflammatory response soon
matory mediators in the circulation is part of the
ensures that the effects of these proinflammatory normal response to infection and serves as a warning
mediators do not become destructive. IL-4, IL-10, signal that the microenvironment cannot control the
IL-11, IL-13, soluble tumor necrosis factor (TNF-ot) initiating insult. The
proinflammatory mediators
IL-1 recruit T
receptors, receptor antagonists, transforming help neutrophils, cells and B cells,
growth factor-(3, and other, as
yet undiscovered
platelets, and coagulation factors to the site of injury or
240 Critical Care
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
infection.24 This cascade stimulates a compensatory
5
systemic anti-inflammatory response, which nor
mally
Stage
quickly down-regulates the initial
proinflam The final stage of MODS is what we have elected
if clinical to call "immunologic dissonance."54 It is an inappro
matory response. Few, any, significant
and be priate, out-of-balance response ofthe immunomodu-
signs symptoms are
produced. Organs may In some it results from
latory system. patients,
the
affected by inflammatory cascade, but persistent, overwhelming inflammation that
may
in
significant organ dysfunction is rare. persist patients with SIRS and MODS, with
increased risk of death.115557
3 In some
patients, persistent immune
suppression
Stage Loss of of the causes immunologic dissonance. Studies have shown
regulation proinflammatory re
not
only that
monocyte deactivation
persists in
many
sponse results in a massive systemic reaction mani patients, but that such
persistent deactivation
greatly
fest as the clinical findings of SIRS. Underlying the increases the risk of death.51 In patients with persis
clinical
pathophysiologic changes that
findings are
tent immune suppression, the cause of organ failure
include the following: (1) progressive endothelial may be inhibition of the
synthesis of the
proinflam
dysfunction, leading to increased microvascular per matory agents needed to allow the organs to recover.
meability;3943 (2) platelet sludging that blocks the In
patients with immunologic dissonance, it may be
microcireulation,44 causing maldistribution of blood possible to
regain organ function if the
body can
its balance.
in
flow and possibly ischemia, which turn may cause
recover
reperfusion injury45 and induction of heat shock
proteins;46 (3) activation of the coagulation system
and
impairment ofthe
protein C-protein S
inhibitory Conclusions
pathway;47 and (4) profound vasodilation, fluid tran- Balance between proinflammatory and anti-in
forces
sudation, and maldistribution of blood flow may flammatory could conceivably be lost: (1)
in
result profound shock.4849 Organ dysfunction and, ultimately, failure result from these changes unless
when
infection, burn injury, hemorrhage, etc, is so
severe that the insult alone is sufficient to prompt
homeostasis is quickly restored. SIRS and MODS; or
(2) when patients are
"pre
Stage 4
to SIRS and MODS severe
printed" develop by preexisting
illness. (3) Most of the preexisting conditions
It is possible that a compensatory anti-inflamma are associated with abnormal cytokine levels.19
reaction can be with a The of rests on our under
tory inappropriate, resulting hypothesis prepriming
immunosuppression. What some
investigators have standing that a patient at risk for SIRS or MODS already
has a clinical and is not
called "immune significant history,
"window of imparalysis,"5051 and
human volunteer.
munodeficiency,"52 "compensatory we describe as clinically analogous to a
healthy
anti-inflammatory response syndrome" (CARS).4
CARS is the body's response to inflammation and is
more than
just immune-paralysis. CARS may explain References
such anomalies as the burn patient's increased sus 1 Tran DD, Groenveld AB, van der Meulen J, et al. Age,
chronic disease, sepsis, organ system failure, and mortality in
ceptibility to infection and even the anergy of the a medical intensive care unit. Crit Care Med 1990; 18:474-79
pancreatitis patient.2953 Recently, it has been shown 2 et
Marshall JC, Cook DJ, Christou NC, al. Multiple organ
that treatment of patients with sepsis with IFN-y not dysfunction score: a reliable
descriptor of a
complex clinical
restores the HLA-DR
only expression on
monocytes outcome. Crit Care Med 1995; 23:1638-52
but reestablishes the ability of monocytes to secrete 3 American College of Chest Physicians/Society of Critical Care
the IL-6 and TNF-a.29 One recent Medicine Consensus Conference. Definitions for sepsis and
cytokines study55
multiple organ failure, and guidelines for the use of innova
looked at a series ofpatients admitted to an ICU who tive in Crit Care
therapies sepsis. Med 1992; 20:864-74
met the criteria for SIRS. All patients demonstrated 4
Bone RC. Why sepsis trials fail. JAMA 1996; 276:565-66
CARS
immunophysiology in that monocyte surface 5
Livingston DH, Appel SH, Wellhausen SR, et al. Depressed
and
human leukocyte antigen (HLA)-DR expression was interferon-gamma production monocyte HLA-DR ex
after
reduced to <30%. The study confirmed that admin pression severe
injury. Arch Surg 1988; 123:1309-13
istration of 6 Cheadle WG, Hershman MJ, Wellhausen SR, et al. Role of
IFN-7-lb could effect up-regulation of
monocytic HLA-DR expression following trauma in predict
monocytesurface HLA-DR expression, restoration ingclinical outcome. In: Faist E, Ninnemann J, Green D, eds.
of Immune
monocyte function, and secretion of IL-6 and consequences of trauma, shock and sepsis. New
TNF-a. The resultant state rebalances CARS-SIRS York: Springer Verlag, 1989; 119-22
7 Gibbons RA, Martinez OM, Lim OC, et al. Reduction in
homeostasis.
immunophysiologic HLA-DR, HLA-DQ, and HLA-DP expression by Leu-M3 +
CHEST/112/1 /JULY, 1997
241
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
cells from the peripheral blood of patients with thermal
28 Pittet
Rangel-Frausto MS, D, Costigan M, et al. The natural
injury. Injury 1989; 19:263-66 history of the
systemic inflammatory response syndrome
8 Wakefield CH, Carey PD, Foulds S, et al. Changes in major (SIRS): a
prospective study. JAMA 1995; 272:117-23
histocompatibility complex class II expression in monocytes 29 Bone RC. Immunologic dissonance: a continuing evolution in our
and T cells of patients developing infection after surgery. Br J understanding of the systemic inflammatory response
9
Surg 1993; 80:205-09
Broader W, Williams D, Pretus H, al. Beneficial effect of
syndrome (SIRS) and the
multiple organ dysfunction syn
et
drome (MODS). Ann Intern Med 1996; 125:680-87
enhanced macrophage function in the trauma patient. Ann
30 Fisher CJ, Dhainaut JF, Opal SM, et al. Recombinant human
Surg 1990; te
211:605-12 interleukin-1 receptor antagonist in the treatment of patients
10
Goris JA, Boekhorst TPA, Nuytinck JKS, et al. Multiple- with
sepsis syndrome: results from a
randomized, double-
failure: generalized autodestructive inflammation? trial.
organ blind, placebo-controlled JAMA 1994; 271:1836-44
Arch Surg 1985; 120:1109-15 31
Abraham E, Wunderink R, Silverman H, et al. Efficacy and
11 Pinsky MR, Vincent J-L, Deviere J, et al. Serum cytokine safety7 of monoclonal antibody to human tumor necrosis
factors in with
levels in human septic shock: relation to multiple-system patients sepsis syndrome. JAMA 1995; 273:
organ failure and mortality. Chest 1993; 103:565-75 934-37
12
Dinarello CA, Gelfand JA, Wolff SM. Anticytokine strategies 32 Platzer
C, Meisel C, Vogt K, et
al. Up-regulation of monocytic
in the treatment of the
systemic inflammatory response IL-10 by tumor necrosis factors and cAMP elevating drugs.
syndrome. JAMA 1993; 269:1829-35 Intern Immunol 1995; 7:17-23
13 Goldie AS, Fearon KCH, Ross JA, et al. Natural cytokine 33
Fukushima R, Alexander JW, Gianotti L, et al. Isolated
antagonists and endogenous antiendotoxin core antibodies pulmonary infection acts as a source of systemic tumor
in sepsis syndrome. JAMA 1995; 274:172-77 necrosis factor. Crit Care Med 1994; 22:114-20
14
Moore FA, Moore EE, Read RA. Postinjury multiple organ 34
Ford HR, Hoffman RA, Wing EJ, et al. Characterization of
failure: role of extra-thoracic injury and sepsis in adult wound
cytokines in the sponge matrix model. Arch Surg 1989;
respiratory distress syndrome. New Horizons 1993; 1:538-49
124:1422-28
35 Meduri Kohler et
15 Bone RC, Balk RA, Fein AM, et al. A second large controlled GU, G, Headley S, al. Inflammatory
clinical study of E5, a monoclonal antibody to endotoxin: cytokines in the BAL of
patients with ARDS:
persistent
results of a prospective, multicenter, randomized clinical trial.
elevation over time predicts a poor outcome. Chest 1995;
Crit Care Med 1995; 23:994-1006 108:1303-14
16 Greenman RI, Schein RM, Martin MA, et al. A controlled 36 Sauder DN, Semple J, Truscott D, et al. Stimulation of
trial of E5 murine monoclonal IgM antibody to endotoxin in muscle
protein degradation by murine and human
epidermal
the treatment of
Gram-negative sepsis. JAMA 1991; 266: cytokines: relationship to thermal
injury, J Invest Dermatol
1097-1102 1986; 87:711-14
17 McCloskey RV, Straube RC, Sanders C, et al. Treatment of
37 Kupper TS, Deitch EA, Baker CC, et al. The human burn
septic shock with human monoclonal antibody HA-1A: a wound as a primary source of interleukin-1 activity. Surgery
randomized double-blind, placebo-controlled trial. Ann In
1986; 100:409-14
tern Med 1994; 121:1-5 38
Puren AJ, Feldman C, Savage N, et al. Patterns of cytokine
18 et
Ziegler EJ, Fisher CJ, Sprung CL, al. Treatment of expression in
community-acquired pneumonia. Chest
1995;
Gram-negative bacteremia and septic shock with HA-1A 107:1342-49
human monoclonal antibody against endotoxin. N Engl J Med 39
Tracey KJ, Lowry SF, Ceremi A.
Cachectin/TNF-alpha in
1991; 324:429-36 septic shock and adult
respiratory distress
syndrome [edito
19 Bone RC. Toward a the
pathogenesis of the
theory regarding Am
rial]. Rev Respir Dis 1988; 138:1377-79
systemic inflammatory response syndrome: what we do and 40
Stephens KE, Ishikaza A, Larrick JW, et al. Tumor necrosis
do not know about
cytokine regulation. Crit Care Med 1996; factor causes increased pulmonary permeability and edema:
24:163-72 comparison to
septic acute
lung injury. Am Rev Respir Dis
20 Zuckerman SH, Bendele AM. Regulation of serum tumor
41
1988; 137:1364-70
necrosis factor in glucocorticoid-sensitive and -resistant ro Ibbotson GC, Wallace JL. Beneficial effects of prostaglandin
dent endotoxin shock models. Infect Immun 1989; E2 in endotoxin shock are unrelated to effects of PAF-acether
57:3009-13 synthesis. Prostaglandins 1989; 37:237-50
21 Zedler S, Bone RC, v. Donnersmarck GH> et al. T-cell 42 Lewis RA, Austen KF, Soberman RJ. Leukotrienes and other
and its role in after
reactivity predictive immunosuppression products of the 5-lipoxygenase pathway: biochemistry and
burns
22
(submitted) on
relation to pathobiology in human diseases. N Engl J Med
Balk RA, Jacobs RF, Tryka AF, et al. Effect of ibuprofen
neutrophil function and acute in canine endotoxin
1990; 323:645-55
43 Petrak
lung injury RA, Balk RA, Bone RC. Prostaglandins, cyclo-oxygen-
23
shock. Crit Care Med 1988; 15:1121-24 ase
inhibitors, and thromboxane synthesis inhibitors in the
Suffredini AF, Fromm RE, Parker MM, et al. The pathogenesis of
multiple organ failure. Crit Care Clin 1989;
cardiovas cular response of normal humans in the 35:303-14
44
administration of endotoxin. N Engl J Med 1989; 321:280-87 Sigurdsson GH, Christenson JT, Bader el-Rakshy M, et al.
24
Bone RC.
The pathogenesis of sepsis. Ann
Intern Med 1991; Intestinal platelet trapping after traumatic and septic shock:
of and failure in ill
115:457-69 early sign sepsis multiorgan critically
an
25 Munoz
C, Carlet J, Fitting C, et al. Dysregulation of in vitro
45
patients? JAMA 1992; Cerra FB.
20:458-67
cytokine production by monocytes during sepsis. J Clin Invest
Cipolle MD, Pasquale NM, Secondary organ
1991; 88:1747-54 dysfunction: from clinical perspectives to molecular media
26 Keogh C, Fong Y, Marano MA, et al. Identification of a novel tors. Crit Care Clin 1993; 9:261-98
tumor necrosis factor a/cachectin from the livers of burned 46 Rinaldo JE, Gorry M, Streiter R, et al. Effect of endotoxin-
induced cell injury on 70-kD heat shock proteins in bovine
and infected rats. Arch Surg 1990; 125:79-85
27 Remick DG. Applied molecular biology of sepsis. J Crit Care lung endothelial cells. Am J Respir Cell Mol Biol 1990;
1995; 10:198-212 3:207-16
242 Critical Care
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
47 Levi M, ten Cate H, van
der Poll T, et al. Pathogenesis of 53 Hamilton G, Hofbauer S, Hamilton B. TNF-alpha, interleu-kin-
in 6 and parameters of the cellular immune system in
disseminated intravascular coagulation sepsis. JAMA 1993;
270:975-79 patients with intra-abdominal sepsis. Scand J Infect Dis 1992;
48
Gomez-Jimenez J, Salgado A, Mourelle M, et al. L-arginine: 24:361-68
et
54 Kox WJ, Bone RC, Krausch D, al. Interferon-7 in the
nitric oxide pathway in endotoxemia and human septic shock.
treatment of the
compensatory anti-inflammatory response
Crit Care Med 1995; 23:253-58 syndrome (CARS).a new
approach: proofof principle. Arch
49 Miyauchi T, Tomobe Y, Shiba R, et al. Involvement
55
Intern Med 1997; 157:389-93 et
of endothelin in the regulation of human vascular Fisher CJ Jr, Opal SM, Dhainaut JF, al. Influence of an
tonus. Circu lation 1990; 81:1874-80 anti-tumor necrosis factor monoclonal antibody on cyto
50 Randow F, Syrbe U, Meisel C, et al. Mechanism of endotoxin desensitization: involvement of interleukin-10 and transform ing growth factor beta. J Exp
kine levels in with
Med 1995; 181:1887-92
patients sepsis. Crit Care Med 1993;
51 Syrbe U, Meinecke A, Platzer C, et al. Improvement of 21:318-27
function.a new 56
monocyte therapeutic approach? In: Sepsis: Dofferhoff AS, Vom VJ, de Vries-Hospers HG, et al. Patterns of
current
perspectives in
pathophysiology and therapy. New cytokines, plasma endotoxin, plasminogen activator inhib
York: Springer Verlag, 1994; 473-500 itor, and acute-phase proteins during the treatment of severe
52 Mills CD, Caldwell NM, Gann DJ. Evidence of a
plasma-
mediated "window" of
immunodeficiency in rats
following 57
sepsis in humans. Crit Care Med 1992; 20:185-92
Lesser HG, Gross V, Scheibenbogen C, et al. Elevation of
trauma. J Clin Immunol 1989; 9:139-50 serum interleukin-6 concentration precedes acute-phase re
sponse and reflects severity in acute pancreatitis. Gastroen-
terology 1991; 101:782-85
CHEST/112/1 /JULY, 1997
243
Downloaded From: http://journal.publications.chestnet.org/ on 06/22/2016
You might also like
- Auto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementFrom EverandAuto-Inflammatory Syndromes: Pathophysiology, Diagnosis, and ManagementPetros EfthimiouNo ratings yet
- Pathophysiology of Sepsis and Genesis of Septic Shock The Critical Role of Mesenchymal Stem Cells MSCsDocument35 pagesPathophysiology of Sepsis and Genesis of Septic Shock The Critical Role of Mesenchymal Stem Cells MSCsrcp9706No ratings yet
- Systemic Inflammatory Response Syndrome The CurrenDocument6 pagesSystemic Inflammatory Response Syndrome The CurrenberlianNo ratings yet
- f210 PDFDocument10 pagesf210 PDFniarsari apNo ratings yet
- Bone 1997Document9 pagesBone 1997Veronica NefiruNo ratings yet
- Advances in The Management of Sepsis and The Understanding of Key Immunologic DefectsDocument14 pagesAdvances in The Management of Sepsis and The Understanding of Key Immunologic DefectsnoviNo ratings yet
- Chapter 127 - Sepsis Syndrome - Rosen's Emergency Medicine Concepts and Clinical Practice 10thDocument10 pagesChapter 127 - Sepsis Syndrome - Rosen's Emergency Medicine Concepts and Clinical Practice 10thAlex DegraciaNo ratings yet
- Treatment of Recurrent Erythema Multiforme With Adalimumab As MonotherapyDocument3 pagesTreatment of Recurrent Erythema Multiforme With Adalimumab As MonotherapyMădălina ŞerbanNo ratings yet
- A Review of GM-CSF Therapy in Sepsis: S R M - ADocument10 pagesA Review of GM-CSF Therapy in Sepsis: S R M - AAnonymous SMLzNANo ratings yet
- Antibiotic Strategies in Severe Nosocomial Sepsis: Why Do We Not De-Escalate More Often?Document7 pagesAntibiotic Strategies in Severe Nosocomial Sepsis: Why Do We Not De-Escalate More Often?Anonymous 2kPiJhIlFNo ratings yet
- Systemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Document8 pagesSystemic in Ammatory Response Syndrome (SIRS) : Where Did It Come From and Is It Still Relevant Today?Jhanu JaguarNo ratings yet
- HHS Public Access: Sepsis Definitions: Time For ChangeDocument5 pagesHHS Public Access: Sepsis Definitions: Time For ChangeDhitaNo ratings yet
- Reichman 1982Document5 pagesReichman 1982Luis Felipe Alvarenga SantosNo ratings yet
- GonorrheaDocument13 pagesGonorrheaMellisa Aslamia AslimNo ratings yet
- Understanding The Inflammatory Cytokine Response in Pneumonia and SepsisDocument9 pagesUnderstanding The Inflammatory Cytokine Response in Pneumonia and SepsisDennyNo ratings yet
- Anticorpi 2Document6 pagesAnticorpi 2Ioana SoraNo ratings yet
- Diagnosis and Management of Sepsis: Author: Tom EvansDocument4 pagesDiagnosis and Management of Sepsis: Author: Tom EvansFariqiNo ratings yet
- Sepsis-Pathophysiology and Therapeutic ConceptsDocument22 pagesSepsis-Pathophysiology and Therapeutic ConceptsJuan ZamoraNo ratings yet
- Comparison of Specific Antiviral Agents in Herpes Simplex KeratitisDocument7 pagesComparison of Specific Antiviral Agents in Herpes Simplex KeratitisWiwik SundariNo ratings yet
- ICP34.5 Deleted Herpes Simplex Virus With Enhanced Oncolytic, Immune Stimulating, and Anti-Tumour PropertiesDocument12 pagesICP34.5 Deleted Herpes Simplex Virus With Enhanced Oncolytic, Immune Stimulating, and Anti-Tumour PropertiesmostafaNo ratings yet
- Hotchkiss 2013Document13 pagesHotchkiss 2013dokteraanNo ratings yet
- Coopersmith 2016Document5 pagesCoopersmith 2016Mark TomNo ratings yet
- Post2018 Neuroprogressao TBDocument2 pagesPost2018 Neuroprogressao TBJoão Paulo AtidioNo ratings yet
- Sepsis in 2018: A Review: Learning ObjectivesDocument8 pagesSepsis in 2018: A Review: Learning ObjectivesViky DamayNo ratings yet
- Api FDocument9 pagesApi FRamon Lopez MartinezNo ratings yet
- Postgrad Med J 2005 Pope 309 14Document14 pagesPostgrad Med J 2005 Pope 309 14Mas Teguh WijayantoNo ratings yet
- A Multicenter Study Evaluating Ceftriaxone and Benzathine Penicillin G As Treatment Agents For Early Syphilis in Jiangsu, ChinaDocument6 pagesA Multicenter Study Evaluating Ceftriaxone and Benzathine Penicillin G As Treatment Agents For Early Syphilis in Jiangsu, ChinaSuryaNo ratings yet
- Review How Lytic OV Should Be Oncoimmunology 2019Document7 pagesReview How Lytic OV Should Be Oncoimmunology 2019Kudelko MatNo ratings yet
- mdw557 2Document7 pagesmdw557 2mfaddhilNo ratings yet
- Harm Worksheet: CitationDocument3 pagesHarm Worksheet: CitationDavid PakpahanNo ratings yet
- Cov Immunotherapy 2Document2 pagesCov Immunotherapy 2lakshminivas PingaliNo ratings yet
- Viru 5 36Document9 pagesViru 5 36Stephanie HellenNo ratings yet
- Systemic Infl Ammatory Response Syndrome & Sepsis: Part 1: Recognition & DiagnosisDocument7 pagesSystemic Infl Ammatory Response Syndrome & Sepsis: Part 1: Recognition & Diagnosisdiego alberto ruizNo ratings yet
- Methods: Thomas Seagraves, MD Michael Gottlieb, MD Data SourcesDocument3 pagesMethods: Thomas Seagraves, MD Michael Gottlieb, MD Data SourcesJorge BarriosNo ratings yet
- Terapeutica de TBC 2019 InglesDocument16 pagesTerapeutica de TBC 2019 InglesJesús Evangelista GomerNo ratings yet
- Sepsis: PathophysiologyDocument8 pagesSepsis: PathophysiologyDonald NashNo ratings yet
- Filgrastim SepsisDocument7 pagesFilgrastim SepsisgauravsinghalNo ratings yet
- IDSA Nec FascDocument34 pagesIDSA Nec FascShameen KhanNo ratings yet
- HK MJ 165057Document10 pagesHK MJ 165057ade_liaNo ratings yet
- Avances en Sepsis Art Ing 2022Document10 pagesAvances en Sepsis Art Ing 2022roman rodriguezNo ratings yet
- Is New Dengue Vaccine Efficacy Data A Relief or Cause For ConcernDocument6 pagesIs New Dengue Vaccine Efficacy Data A Relief or Cause For ConcernTaufiqurrokhman RofiiNo ratings yet
- Zusman 2016 (มี CRE)Document11 pagesZusman 2016 (มี CRE)Nattawat TeerawattanapongNo ratings yet
- Jurnal 6Document16 pagesJurnal 6Nurfitrianti ArfahNo ratings yet
- Idsa GuidelinesDocument34 pagesIdsa GuidelinesROSEN NNo ratings yet
- Diagnostic Value of The Physical Examination in Patients With Dyspnea - Cleve Clin J Med 2017Document9 pagesDiagnostic Value of The Physical Examination in Patients With Dyspnea - Cleve Clin J Med 2017ErnestoNo ratings yet
- Engoren 2020Document7 pagesEngoren 2020DEYVI JOHE ANGULO FLORIANNo ratings yet
- PIIS0953620523003874Document8 pagesPIIS0953620523003874bilou hertNo ratings yet
- Practice Guidelines For The Diagnosis and Management of Skin and Soft-Tissue InfectionsDocument34 pagesPractice Guidelines For The Diagnosis and Management of Skin and Soft-Tissue InfectionsNatalia MoranNo ratings yet
- CID 04 Candidiasis Guia TtoDocument29 pagesCID 04 Candidiasis Guia TtoIVANNo ratings yet
- Jama Abbasi 2021 MN 210043 1627852635.57854Document2 pagesJama Abbasi 2021 MN 210043 1627852635.57854anggaririnNo ratings yet
- Peds 2020029249Document17 pagesPeds 2020029249nana wardhaniNo ratings yet
- Contents CCCDocument4 pagesContents CCCdita megaNo ratings yet
- Jurnal 7Document10 pagesJurnal 7Efa AnggrainiNo ratings yet
- Antibiotico YPronosticoDocument6 pagesAntibiotico YPronosticoagonzale52No ratings yet
- Bmjebm 2021 111901.fullDocument6 pagesBmjebm 2021 111901.fullMonika Diaz KristyanindaNo ratings yet
- 220-Management of Genital Herpes in Pregnancy, 2020Document10 pages220-Management of Genital Herpes in Pregnancy, 2020waleedaliNo ratings yet
- Childhood Bulling Involvement Predicts Low Grade Systemic InflammationDocument6 pagesChildhood Bulling Involvement Predicts Low Grade Systemic InflammationCristiana ComanNo ratings yet
- La Respuesta Del Huesped A La SepsisDocument18 pagesLa Respuesta Del Huesped A La SepsisAngelicia Varela MuñozNo ratings yet
- The University of Chicago Press The Society For Healthcare Epidemiology of AmericaDocument5 pagesThe University of Chicago Press The Society For Healthcare Epidemiology of AmericaVarun bharathiNo ratings yet
- Sepsis 2021 A ReviewDocument9 pagesSepsis 2021 A ReviewvictorNo ratings yet
- 2014 Sepsis Management PDFDocument43 pages2014 Sepsis Management PDFAzis KazeNo ratings yet
- Absen HarianDocument1 pageAbsen HarianChristmando Sapria AbrianNo ratings yet
- Diagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaDocument18 pagesDiagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaChristmando Sapria AbrianNo ratings yet
- Journal ReadingDocument24 pagesJournal ReadingChristmando Sapria AbrianNo ratings yet
- Diagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaDocument18 pagesDiagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaChristmando Sapria AbrianNo ratings yet
- Diagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaDocument18 pagesDiagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaChristmando Sapria AbrianNo ratings yet
- Diagnosis and Management of Pre-Eclampsia and EclampsiaDocument24 pagesDiagnosis and Management of Pre-Eclampsia and Eclampsiasyaifuddin07051989No ratings yet
- Journal ReadingDocument24 pagesJournal ReadingChristmando Sapria AbrianNo ratings yet
- Diagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaDocument18 pagesDiagnostics and Prediction of Glaucoma in Patients With Familial Congenital Iris HypoplasiaChristmando Sapria AbrianNo ratings yet
- Prevention of Preeclampsia 20121Document9 pagesPrevention of Preeclampsia 20121Christmando Sapria AbrianNo ratings yet
- Pro-Oxidant Strategies - Cancer Treatments ResearchDocument71 pagesPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNo ratings yet
- These - Are - The - 41 - Thread - by - Morpheusresist - Sep 6, 22 - From - RattibhaDocument10 pagesThese - Are - The - 41 - Thread - by - Morpheusresist - Sep 6, 22 - From - RattibhaRohan MNo ratings yet
- Organization and Management at State and District Level (GUJARAT)Document26 pagesOrganization and Management at State and District Level (GUJARAT)Akriti LohiaNo ratings yet
- MDMA-assisted Therapy Significantly Reduces Eating Disorder Symptoms in A Randomized Placebo-Controlled Trial of Adults With Severe PTSDDocument8 pagesMDMA-assisted Therapy Significantly Reduces Eating Disorder Symptoms in A Randomized Placebo-Controlled Trial of Adults With Severe PTSDKayla GreenstienNo ratings yet
- Written Assignment Principles of Applied RehabilitationDocument17 pagesWritten Assignment Principles of Applied RehabilitationRuqaiyah RahmanNo ratings yet
- Pappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxDocument5 pagesPappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxVinoster ProductionNo ratings yet
- Module 1 DiversityDocument33 pagesModule 1 DiversityCatherine A. PerezNo ratings yet
- ReferencesDocument2 pagesReferencesapi-451063936No ratings yet
- Snake Bite SOPDocument5 pagesSnake Bite SOPRaza Muhammad SoomroNo ratings yet
- JUMPSTART TO SKINNY by Bob Harper: Rule #1Document8 pagesJUMPSTART TO SKINNY by Bob Harper: Rule #1Random House Publishing GroupNo ratings yet
- Test AaDocument55 pagesTest AaKaye PatanindagatNo ratings yet
- Health 8 - 1st Grading ExamDocument3 pagesHealth 8 - 1st Grading Exammaria luzNo ratings yet
- Topic ListDocument6 pagesTopic ListEdwinNo ratings yet
- Burnout Among Secondary School Teachers in Malaysia Sabah: Dr. Balan RathakrishnanDocument8 pagesBurnout Among Secondary School Teachers in Malaysia Sabah: Dr. Balan Rathakrishnanxll21No ratings yet
- Job Safety Analysis SOP Rev A 08.2017Document4 pagesJob Safety Analysis SOP Rev A 08.2017AshtosheelatikaNo ratings yet
- Set C QP Eng Xii 23-24Document11 pagesSet C QP Eng Xii 23-24mafiajack21No ratings yet
- The Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeDocument11 pagesThe Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeLana PeharNo ratings yet
- Clinical Leaflet - QUS - v2Document2 pagesClinical Leaflet - QUS - v2ultrasound tomNo ratings yet
- EVOLUTION OF MODELS OF DISABILITY Notes OnlyDocument1 pageEVOLUTION OF MODELS OF DISABILITY Notes OnlyLife HacksNo ratings yet
- Oregon SOS Audit On Child WelfareDocument49 pagesOregon SOS Audit On Child WelfareSinclair Broadcast Group - Eugene100% (1)
- Tea and Industrial RevolutionDocument4 pagesTea and Industrial RevolutionPhuong NguyenNo ratings yet
- Professions and Occupations in BoliviaDocument7 pagesProfessions and Occupations in BoliviaMaribel Jarata JulianNo ratings yet
- NCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMADocument5 pagesNCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMAMa. Elaine Carla Tating50% (2)
- Pag-Unawa Sa Mga Panganib NG Sobrang Dosis NG Alkohol: Ano Ang Isang Pamantayang Tagay?Document5 pagesPag-Unawa Sa Mga Panganib NG Sobrang Dosis NG Alkohol: Ano Ang Isang Pamantayang Tagay?Rochelle Bartocillo BasquezNo ratings yet
- ELC - Assignment Cover SheetDocument4 pagesELC - Assignment Cover Sheetbharti guptaNo ratings yet
- 50 Item Psychiatric Nursing Exam IDocument11 pages50 Item Psychiatric Nursing Exam Iɹǝʍdןnos98% (40)
- 2008 04 Lecture 1 Interface Dermatitis FrishbergDocument6 pages2008 04 Lecture 1 Interface Dermatitis FrishbergYudistra R ShafarlyNo ratings yet
- Components of Fitness, PARQ and TestingDocument29 pagesComponents of Fitness, PARQ and TestingLynNo ratings yet
- Synthesis PaperDocument7 pagesSynthesis Paperapi-379148533No ratings yet
- Personal Safety With Dance: Worksheet in Health Optimizing Physical Education 3 (HOPE3/PEH3)Document9 pagesPersonal Safety With Dance: Worksheet in Health Optimizing Physical Education 3 (HOPE3/PEH3)Cregie Brillantes QuezaNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)