Professional Documents
Culture Documents
3 Protokol Lijecenja Demencije PDF
Uploaded by
dragutinpetricOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
3 Protokol Lijecenja Demencije PDF
Uploaded by
dragutinpetricCopyright:
Available Formats
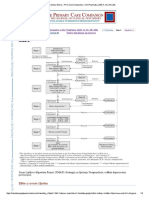
PROTOCOL FOR MANAGING BEHAVIOURAL AND PSYCHOLOGICAL SYMPTOMS IN
PATIENTS WITH DEMENTIA
(Does not cover rapid tranquillisation of acutely disturbed)
Refer to Cumbria Dementia strategy for prevention strategies and initial non-
pharmacological management
A) Primary care responsibility B) Optional primary care responsibility with secondary
care support if required or requested C) Secondary care responsibility
A) Patient
Patient hashas Behavioural
Behavioural andand Yes Does patientalso
Does patient have a a
have Yes Treat underlying acute
Yes Yes
Psychiatric Symptoms
Psychological Symptomsin Dementia
in Dementia Delirium?
Delirium? medical problems e.g.
(BPSD) (delusions, hallucinations,
(e.g. psychosis; aggression; (Short history<<21weeks
(Short history week UTI, chest infection,
agitation,
depression aggression,
combined irritability etc with
with a decline in confusion, hallucination,
hallucinations, delusions or side effects of drugs,
steady decline
cognition in cognition
over six month) over a delusion with
apathy with fluctuating
fluctuating alcohol and drug
minimum of 6 months) cognition)
cognition) withdrawal etc.
No
No
Behavioural problems
B) Apply PAAID approach and manage or treat: unresolved
Apply PAIN approach and manage or treat:
P=Physical
P=Physical problems
problems e.g.
e.g. infection,
infection, pain
pain
A=Activity-related
A=Activity-related e.g.dressing,
e.g.dressing, washing
washing
A= Anti-cholinergic
I =Iatrogenic burden-
e.g. side effectssee CPFT e.g.
of drugs Shared Medicines
anticholinergics Consider non-pharmacological approaches such
Resources on Medicines Management homepage
N= Noise and other environmental factors e.g. lighting.(link on p3) as: distraction, leave & return, activity, one-to-one
I=Intrinsic to dementia e.g. wandering care, music, aromatherapy. Carer support may
D=Depression, anxiety and psychosis improve coping ability of carer(s).
Refer to Cumbria dementia strategy for further
information
Identify the dominant target symptom group
Identify
Identify
IIIII
IIIII
Psychosis: Delusions/Hallucinations.
Only consider pharmacological treatment if there
Depression: depressed mood and /or loss of ability to enjoy is psychosis, depression or severe distress or an
previously pleasurable activities. May or may not include immediate risk of harm to the person or others. Do
apathy. NOT use for mild-moderate symptoms
Apathy: diminished motivation; listlessness; loss of drive to
engage in activities. May be perceived as laziness. Could this be Dementia with Lewy Bodies or
Parkinsons Disease Dementia?
Aggression Key features: long term (> 6 months) history of
vivid visual hallucinations or parkinsonism or
Agitation/ Anxiety fluctuating cognition.
Sleep disturbance Unsure Yes or No
Other symptoms: e.g. vocalisations; sexual disinhibition; C) Get specialist Follow guidelines
stereotypical movements etc. advice below and overleaf
In the event of General guidelines if pharmacological treatment is indicated.
continuing The use of either typical or atypical antipsychotics in patients with dementia worsens
problems, advice cognitive function; increases the risk of cerebrovascular events (~ 3 xs) and increases mortality rate
can be obtained (~2x). They should only be used after full discussion with the patient (where the patient has
from OA CMHT, capacity to understand) and carer about the possible benefits and likely risks. Risk is likely to
liaison team or increase with increasing age and if other risk factors for cerebrovascular events are present e.g.
memory service diabetes; hypertension, cardiac arrhythmias; smoking and existing evidence of stroke or vascular
dementia.
If antipsychotic treatment is considered necessary avoid typical antipsychotics. Start atypical doses
low (usually one half normal elderly dose) and increase every 2 -4 days if no response (see
specific doses suggestions p3)
There is only one drug Patients who respond to treatment should have the drug cautiously withdrawn after 6-12 weeks.
(Risperidone) licensed Gradually reduce dose and if no re-emerging symptoms, stop. Prescribe so that reductions and
specifically for the discontinuation begin on a Monday. Review again one week after stopping. If symptoms re-emerge
treatment of BPSD. For reintroduce the drug at starting dose.
other symptoms drugs BPSD can persist and treatment with atypical antipsychotics may be needed in the long term but
are used which have should be reviewed on a 3 monthly basis.
either been shown to Patients with Dementia with Lewy Bodies or Parkinsons Disease Dementia are particularly
improve these symptoms vulnerable to antipsychotic sensitivity reactions and also have marked extrapyramidal side effects.
in subjects without The management of antidepressants and hypnotics in patients with dementia has little
dementia or are licensed evidence base and should follow existing guidelines for the management of these drugs in elderly
for cognitive patients without dementia. Treatment doses should follow BNF guidelines.
enhancement in patients Memory Matters medication scrutiny tool (ref Cumbria Dementia strategy) can be used to record
with dementia. symptoms, alternative treatments used, risk benefit assessment, medication prescribed, patient/
Approved Nov 2012 carer experience and review of therapy
Prescribing Guidelines for BPSD in Dementia
For all cases of agitation and aggression in dementia, pain relief i.e. Paracetamol 1g tds should be seriously considered
as an alternative to the medications below.
Husebo et al published a recent Norwegian study in the BMJ which showed analgesia significantly reduced
agitation/aggression compared to controls- BMJ 2011;343:d 4065- http://www.bmj.com/content/343/bmj.d4065
Alzheimers Disease.
Evidence Evidence
Key symptom First line Second line
type type
Depression Sertraline, 23+ Mirtazapine 3
Citalopram#
S
Apathy Sertraline, 23 + Donepezil ; Rivastigmine 2
S S
Citalopram# ; Galantamine
Psychosis Risperidone 1 Olanzapine; Aripiprazole; 2
S
Memantine
L
Aggression Risperidone 1 Olanzapine, Aripiprazole; 2
Haloperidol 2 Carbamazepine, 2
S
Lorazepam Memantine
Moderate Agitation/ Anxiety Citalopram. # 3 Trazadone; Lorazepam; 2-4
Mirtazapine; Memantine
Severe Agitation/ Anxiety Risperidone, 1 Aripiprazole, Olanzapine, 2-4
S
Memantine Lorazepam.
Poor sleep Temazepam; 3+ Zolpidem 3
Zopiclone.
Dementia with Lewy Bodies or Parkinsons disease dementia.
Evidence Evidence
Key symptom First line Second line
type type
Depression Citalopram# 4+ Sertraline 4
S
Apathy Sertraline, 4+ Donepezil ; 2
S
Citalopram# Rivastigmine ;
S
Galantamine
S S
Psychosis* Rivastigmine . 2-3 Quetiapine 3
S S
Donepezil ; Clozapine
S
Galantamine ..
S
Aggression Quetiapine. 3 Rivastigmine 3-4
S S
Donepezil ; Galantamine
Lorazepam
S
Moderate Agitation/ Anxiety Citalopram.# 3+ Rivastigmine . 2-4
S
Sertraline Donepezil
S
Galantamine Lorazepam
S
Severe Agitation/ Anxiety Quetiapine. 3 Rivastigmine 3-4
S S
Donepezil ; Galantamine
Lorazepam
Poor sleep Temazepam; 3+ Zolpidem 3
Zopiclone.
REM sleep behaviour Clonazepam** 3
(nightmares; hyperactivity)
* consider reducing antiparkinsonian medication first. ** 500-1000 microgram nocte
L S
= Licensed indication = Secondary care initiation or recommendation under shared care
# If considering Citalopram, note MHRA guidance (contra-indication with antipsychotic and max dose in elderly 20mg) (link on p 3)
Evidence levels: 1 = Meta-analysis; 2 = RPCTs; 3 = Other studies; 4 = Expert opinion; =cost
Please note the use of mood stabilisers/anticonvulsants has very limited evidence to support use. Use should be
restricted to patients where other treatments are contra-indicated or ineffective.
Vascular dementia or stroke related dementia.
There is little evidence base for the treatment of BPSD in Vascular dementia or stroke related dementia. The cholinesterase
inhibitors (Donepezil; Rivastigmine; Galantamine) and Memantine are not licensed for the treatment of vascular dementia and
should not be used. Prescribers are advised to follow the guidance for Alzheimers disease but to use with extreme caution drugs
with an established increased cerebrovascular risk (i.e. antipsychotics)
Other BPSD and other dementias (e.g. Fronto-temporal lobe dementia).
There is little evidence base for the treatment of other BPSD or for the treatment of common BPSD in other dementias.
Specialist advice should be sought.
Drug dose guidelines for antipsychotics and anxiolytics in dementia.
Approved Nov 2012
Start at minimum recommended dose and titrate according to response (usually every 2-4 days) to maximum tolerated
dose. Cautious withdrawal may be initiated at 6-12 weeks. See guidelines on page 1 of this guidance.
Drug Starting dose Maximum dose
Risperidone** 500 microgram o.d.* 1mg b.d.
Olanzapine 2.5mg o.d. 10mg daily
Quetiapine 25mg o.d. 25-300mg daily
Aripiprazole 5mg o.d. 10mg daily
Haloperidol** 0.5mg bd-tds oral/IM 1mg tds oral/IM
Lorazepam 0.5 mg 1mg bd oral/IM 1mg bd oral/IM ***
* BNF dose250microgram bd
** Do not use haloperidol or risperidone in established or suspected Parkinsons disease or Lewy Body Dementia
*** elderly max dose
Citalopram and escitalopram warning letter MHRA November 2011
http://www.mhra.gov.uk/Safetyinformation/Safetywarningsalertsandrecalls/Safetywarningsandmessagesformedicines/Mo
nthlylistsofinformationforhealthcareprofessionalsonthesafetyofmedicines/CON134744
Anti-cholinergic burden- see Shared Medicines Resources on Medicines Management intranet pages
http://cptportal.cumbria.nhs.uk/SiteDirectory/MedicinesManagement/Web%20Pages/Shared%20Medicines%20Resources.
aspx
Further resources:
efns.org (European Federation of Neurological Societies)
ipa-online.org (International Psychogeriatric Association)
Approved: Cumbria Partnership NHS Foundation Trust Medicines Management Committee September 2012
Cumbria Area Prescribing Committee October 2012
Date for review November 2014 (or sooner if relevant guidance changes)
Based on 1.CSM CEM/CMO/2004/1(MHRA); 2.BNF (2008); 3.Faculty of Old Age Psychiatry (2008); 4. Maudsley Guidelines 2012; 5.NICE-SCIE guidelines;
6. SIGN 2006: 6. Ballard C , Current Opinions in Psychiatry 2009: Cochrane review of antipsychotics in dementia 2001/2010.
Acknowledgement to Prof C Holmes and Dr S Muthalagu, - March 2009 (Hampshire Guidelines), Dr S Wright, Ms Sue Wright, April 2011 (Rotherham guidelines)
Approved Nov 2012
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- 7 Treatment-Resistant Obsessive-Compulsiv PDFDocument7 pages7 Treatment-Resistant Obsessive-Compulsiv PDFdragutinpetricNo ratings yet
- 528 Clinical-Diagnosis PDFDocument528 pages528 Clinical-Diagnosis PDFdragutinpetricNo ratings yet
- 849 Black-s-Medical-Dictionary PDFDocument849 pages849 Black-s-Medical-Dictionary PDFdragutinpetric100% (2)
- 3838 Emergency Medicine PDFDocument3,838 pages3838 Emergency Medicine PDFdragutinpetricNo ratings yet
- 505 Management-Disorders PDFDocument505 pages505 Management-Disorders PDFdragutinpetricNo ratings yet
- 2 Algorhitm Treatment Depresion PDFDocument2 pages2 Algorhitm Treatment Depresion PDFdragutinpetric100% (2)
- 356 Mastering Psychiatry Textbook PDFDocument356 pages356 Mastering Psychiatry Textbook PDFdragutinpetricNo ratings yet
- DSM 5 MCQ PDFDocument480 pagesDSM 5 MCQ PDFeinstein100% (10)
- 356 Mastering Psychiatry Textbook PDFDocument356 pages356 Mastering Psychiatry Textbook PDFdragutinpetricNo ratings yet
- 356 Mastering Psychiatry Term-Paper PDFDocument356 pages356 Mastering Psychiatry Term-Paper PDFdragutinpetricNo ratings yet
- 329 Mastering-Psychiatry-2016 PDFDocument329 pages329 Mastering-Psychiatry-2016 PDFdragutinpetric100% (1)
- Albers, Hahn, Reist - PsychiatryDocument144 pagesAlbers, Hahn, Reist - Psychiatrypsp710No ratings yet
- 261 MHGuidebook PDFDocument261 pages261 MHGuidebook PDFdragutinpetricNo ratings yet
- Emergensi Jiwa PDFDocument217 pagesEmergensi Jiwa PDFandrio raymosNo ratings yet
- Neral PractitionersDocument216 pagesNeral PractitionersSudhir Tyagi100% (1)
- Principles in Using Psychotropic Medication in Children and AdolescentsDocument19 pagesPrinciples in Using Psychotropic Medication in Children and AdolescentsdragutinpetricNo ratings yet
- 35 Protocol Pharmacologikal Treatment PDFDocument35 pages35 Protocol Pharmacologikal Treatment PDFdragutinpetric100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)