Professional Documents
Culture Documents
Hypoglycemia
Uploaded by
Krystle GabriellaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypoglycemia
Uploaded by
Krystle GabriellaCopyright:
Available Formats
HYPOGLYCEMIA
Hypoglycemia are the most common complications that occur in patients with diabetes who are treated with insulin
Clinical features :
- Neuroglycopenia (insufficient glucose for normal CNS function) :
mental confusion, fatigue, seizure, stupor, coma, death
- Neurogenic (autonomic) :
adrenergic (tachycardia, palpitations, sweating, tremulousness) and parasympathetic (nausea, hunger)
Risk factors :
- Insulin doses are excessive
- Influx of exogenous glucose is reduced (during an overnight fast / missed meals)
- Insulin-independent glucose utilization is increased (during exercise)
- Insulin sensitivity is increased (intensive therapy, in the middle of the night, late after exercise, increased fitness,
weight loss)
- Endogenous glucose production is reduced
- Insulin clearance is reduced
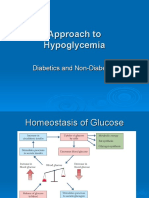
Counterregulatory responses to hypoglycemia
1. Normal counterregulation
When plasma glucose is low (falls below 70 mg/dL hormonal responses tend to begin glucagon &
epinephrine acts to counterregulate hypoglycemia
Glucagon is considered the 1st line of defense and epinephrine is to provide a backup system
2. Defective counterregulation in diabetes
For unexplained reasons, patient with type 1 diabetes uniformly lose their ability to secrete glucagon in
response to acute insulin-induced hypoglycemia
Hypoglycemia unawareness
- Refers to a loss of the warning symptoms that alert individuals to the presence of hypoglycemia
- Periods of relative or absolute therapeutic insulin excess, in the setting of absent glucose response lead to
episodes of iatrogenic hypoglycemia failure of the sympathetic nerve system to respond to hypoglycemiaz
Management
- Increase self monitoring blood glucose
- Eating frequent small snacks
- Reducing size of insulin doses
You might also like
- Approach To HypoglycemiaDocument37 pagesApproach To HypoglycemiaMiswar Abdul HalimNo ratings yet
- Complication of Diabetes Mellitus: Focus On HypoglycaemiaDocument8 pagesComplication of Diabetes Mellitus: Focus On HypoglycaemiaiikNo ratings yet
- ENCPDocument12 pagesENCPShin PenielNo ratings yet
- ENCPDocument12 pagesENCPShin PenielNo ratings yet
- Hypoglycemia UMYDocument60 pagesHypoglycemia UMYTommy AkromaNo ratings yet
- Hypoglycemia: 8 TermDocument44 pagesHypoglycemia: 8 Termswathi bsNo ratings yet
- Course 4 2019 Hypoglicemia HyperuricemiaDocument57 pagesCourse 4 2019 Hypoglicemia HyperuricemiaAmelia PricopNo ratings yet
- HypoglycemiaDocument3 pagesHypoglycemiamohamed mowafeyNo ratings yet
- Insulin and Antidiabetic Drugs: Prof - DR Asya RehmanDocument23 pagesInsulin and Antidiabetic Drugs: Prof - DR Asya RehmanGareth BaleNo ratings yet
- HypoglycemiaDocument3 pagesHypoglycemiamohamed mowafeyNo ratings yet
- HypoglycemiaDocument68 pagesHypoglycemialiaputranti100% (3)
- HypoglycemiaDocument113 pagesHypoglycemiamadelleinetNo ratings yet
- LEC#37 Anti Diabetic Drugs (Insulin)Document20 pagesLEC#37 Anti Diabetic Drugs (Insulin)alihyderabro166No ratings yet
- Hypoglycemia OralDocument2 pagesHypoglycemia OralNadia AlmahalawiNo ratings yet
- Hypoglycaemia in Diabetes: Key PointsDocument7 pagesHypoglycaemia in Diabetes: Key Pointsnot here 2make friends sorryNo ratings yet
- HypoglycemiaDocument42 pagesHypoglycemiaseem neemNo ratings yet
- Evaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Document15 pagesEvaluation of Hypoglycemia: & Insulin Autoimmune Syndrome (Hirata Disease)Anonymous B3J9sWNo ratings yet
- Drugs For Diabetes MellitusDocument50 pagesDrugs For Diabetes MellitusCherenet TomaNo ratings yet
- Assignment (Diabetes)Document9 pagesAssignment (Diabetes)Wynne EnglatieraNo ratings yet
- DM DrugsDocument46 pagesDM DrugsQuinonez Anna MarieNo ratings yet
- Endocrine CologyDocument124 pagesEndocrine CologyBehailu TejeNo ratings yet
- Hypoglycemia: Prepared By: Ahmed Rawhi DabourDocument84 pagesHypoglycemia: Prepared By: Ahmed Rawhi DabourKaterina FusaNo ratings yet
- DR - LominoqueDocument11 pagesDR - LominoqueCharisse BulasaNo ratings yet
- Unit 5 Part 2 InsulinDocument68 pagesUnit 5 Part 2 InsulinKhairunnisa Loqman100% (1)
- Diabetes Mellitus Part IIDocument12 pagesDiabetes Mellitus Part IIVictoria ArcaNo ratings yet
- NRSE 3010 Chapter 47Document52 pagesNRSE 3010 Chapter 47Karina IvanchenkoNo ratings yet
- Asuhan Keperawatan Pada Pasien HipoglikemiaDocument15 pagesAsuhan Keperawatan Pada Pasien HipoglikemiaNaela zenthaNo ratings yet
- Antidiabetic Drugs. Nurse 2024Document32 pagesAntidiabetic Drugs. Nurse 2024Ayro Business CenterNo ratings yet
- Insulin Dan Oral DiabetesDocument30 pagesInsulin Dan Oral DiabetesIrsan Fahmi ANo ratings yet
- Antidiabetic DrugsDocument53 pagesAntidiabetic Drugszmr27146No ratings yet
- 4DM PresentationDocument57 pages4DM Presentationamal nassarNo ratings yet
- Drugs Used To Treat Diabetes - MellitusDocument37 pagesDrugs Used To Treat Diabetes - MellitusjisooNo ratings yet
- Drugs For Diabetes (Part 1)Document6 pagesDrugs For Diabetes (Part 1)حوراء عارف الموسويNo ratings yet
- Pharmacology Reading Materials On DMDocument19 pagesPharmacology Reading Materials On DMJames SoeNo ratings yet
- Diabetes Drugs 1 (Insulins)Document54 pagesDiabetes Drugs 1 (Insulins)daniyal kumarNo ratings yet
- HypoglycaemiaDocument18 pagesHypoglycaemiaAli SafaaNo ratings yet
- Antidiabetic Drug PDFDocument91 pagesAntidiabetic Drug PDFAlifia ainushNo ratings yet
- Hypoglycemia - StatPearls - NCBI BookshelfDocument6 pagesHypoglycemia - StatPearls - NCBI BookshelfDhany karubuyNo ratings yet
- Hypoglycemia 2Document14 pagesHypoglycemia 2ghostmanzNo ratings yet
- Regular Insulin: A Drug Study OnDocument9 pagesRegular Insulin: A Drug Study OnSophia IbuyanNo ratings yet
- INSULINDocument39 pagesINSULINMohini GautamNo ratings yet
- Hypoglycemia - 5 MarkDocument3 pagesHypoglycemia - 5 Marksaranya amuNo ratings yet
- Classifications of Insulin2Document116 pagesClassifications of Insulin2loglesb1No ratings yet
- Insulin Therapy RevisedDocument17 pagesInsulin Therapy RevisedOluwatimilehin Olagunju100% (1)
- E SystemDocument81 pagesE SystemErsido SamuelNo ratings yet
- Danilo F. Baldemor, MD, MS, DPCP: Internist - DiabetetologistDocument93 pagesDanilo F. Baldemor, MD, MS, DPCP: Internist - DiabetetologistButch AmbataliNo ratings yet
- HypoglycemiaDocument3 pagesHypoglycemiaspicychips7No ratings yet
- Hypoglycemia and Hyperglycemia GM Eng 2022Document3 pagesHypoglycemia and Hyperglycemia GM Eng 2022kabulkabulovich5No ratings yet
- What Is Diabetes, Its Types, Role of Insulin and Hypoglycemic Agents, Mode of Action, Side Effects, Pharmacodynamics and PharmacokineticsDocument9 pagesWhat Is Diabetes, Its Types, Role of Insulin and Hypoglycemic Agents, Mode of Action, Side Effects, Pharmacodynamics and PharmacokineticsIshaani GargNo ratings yet
- Anti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Document39 pagesAnti-Diabetic Drugs: Siti Farah MD Tohid (PHD)Nurul Mursyidah ZakariaNo ratings yet
- Diabetes Mellitus (DM) : ContentDocument30 pagesDiabetes Mellitus (DM) : ContentMompati LetsweletseNo ratings yet
- Hypoglycemia: Yeditepe University Medical Faculty Department of Endocrinology and MetabolismDocument47 pagesHypoglycemia: Yeditepe University Medical Faculty Department of Endocrinology and MetabolismnawarajNo ratings yet
- Drugs of DiabetesDocument42 pagesDrugs of Diabeteskwennybiang100% (1)
- Anti Diabetic DrugsDocument58 pagesAnti Diabetic DrugsDaniel WangNo ratings yet
- Disease/Cause Risk Factors Diagnostic Test Treatment Medical MGT Nursing MGTDocument2 pagesDisease/Cause Risk Factors Diagnostic Test Treatment Medical MGT Nursing MGTChin ChanNo ratings yet
- Drugs That Alter Glucose RegulationDocument10 pagesDrugs That Alter Glucose RegulationArdrian GollerNo ratings yet
- AntidiabetesDocument51 pagesAntidiabetesPuri Ratna KartiniNo ratings yet
- Insulin PharmacologyDocument4 pagesInsulin PharmacologySunilNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Diabetes: Symptoms, Causes, and Solutions for Type 1 and 2 DiabetesFrom EverandDiabetes: Symptoms, Causes, and Solutions for Type 1 and 2 DiabetesNo ratings yet
- Opsonin and ReceptorsDocument1 pageOpsonin and ReceptorsKrystle GabriellaNo ratings yet
- Diagnosis DementiaDocument2 pagesDiagnosis DementiaKrystle GabriellaNo ratings yet
- Hyperthropic CardiomyopathyDocument2 pagesHyperthropic CardiomyopathyKrystle GabriellaNo ratings yet
- Bacteria of Oral CavityDocument1 pageBacteria of Oral CavityKrystle GabriellaNo ratings yet