Professional Documents
Culture Documents
Lacrimal System
Uploaded by
Soodn Kang Soodn0 ratings0% found this document useful (0 votes)
24 views13 pagesLacrimal
Original Title
Lacrimal System AllTebFamily.com
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentLacrimal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
24 views13 pagesLacrimal System
Uploaded by
Soodn Kang SoodnLacrimal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 13
Ophthalmology 2
ct a als
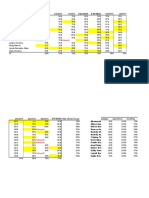
TT a6 OY 10-16mm eo
re a a
tsa
A"
Dr/ Mahmoud Medhat
@11 S00 4 907
Dr/ Mahmoud Medhat 0113004901
Anatomy of the lacrimal system
1. Secretory pai
a. The main lacrimal gland (Orbital & palpebral portions).
b. Accessory lacrimal glands (Glands of Krause & glands of Wolfring).
c. Conjunctival goblet cells.
2. Exeretory part (Drainage system):
Two puncti.
Two canaliculi.
Lacrimal sac.
Nasolacrimal duct (NLD).
acrimal gland
secretory ducts
superior canaliculus
aoee
1. Secretory part:
1. The main lacrimal
gland: Almond shaped,
lying in the lacrimal punctum
fossa, at the upper lateral
corer of the orbit.
© Divided into:
© Orbital portion: Large.
© Palpebral_part: Smaller
& resting on the superior
conjunctival fornix, so it
can be seen on lid
eversion.
© It opens by 12 duets, arising
from the orbital part >
passing through the palpebral
part © opening into the
superior fornix. (Removal of the
palpebral part prevents the secretion
from the whole gland).
© Nerve supply:
© Sensory: Lacrimal
26%
Dr/ Mahmoud Medhat 0113004901
branch from the ophthalmic.
© Parasympathetic (Secretory): Facial nerve.
co Sympathetic: The superior cervical ganglion.
2. Accessory lacrimal glands:
© Glands of Krause: Microscopic acini in the fornices
‘© Glands of Wolfring: Opposite the mid-tarsus
3. Conjunctival goblet cells: Unicellular mucinous glands
II. Lacrimal drainage system: anova
1, Two puncti: Small orifices situated
on the lacrimal papilla, at the posterior _ vertical
canaliculi ~
edge of the lid margin, 6mm from the
medial canthus.
2. Two canaliculi:
@ Fine tubes from the lacrimal
puncti to the lacrimal sac.
They unite forming a common
canaliculus (1-2mm).
© Each canaliculus is divided into
a vertical (2mm) & a horizontal
(6mm) portion.
3. Lacrimal sac: In the lacrimal fossa, at the anterior part of the
medial orbital wall.
4, Naso-Lacrimal duct (NLD):
© Passing from the lacrimal sac,
to open in the inferior meatus
of the nose (12-24mm). At that
level it is guarded by Hasener’s
flow of wars over the eye
valve © preventing passage of air or discharge from the nose.
© Direction: Downward, slightly backward & laterally.
= 27.
Dr/ Mahmoud Medhat 0113004901
Precorneal tear film = mann
Layers of the tear film:
1. Outer lipid layer:
© From meibomian glands.
© Prevents rapid
evaporation of tears &
lubricates the eyelid
above the globe.
2. Middle aqueous layer:
© From the lacrimal gland.
© Function:
© Supplies O> to the comeal epithelium
© Antibacterial (It contains lysozymes & Ig).
3. Inner mucous layer:
© From goblet cells
© Renders the corneal epithelium hydrophilic.
Dry eye
Definition: Lack or even absence of one or more of the 3 layers of the
precorneal tear film
Aetiology Lh
1. Deficiency of the lacrimal layer:
1. Congenital absence of the lacrimal gland.
Inflammations of the lacrimal gland. V4
Tumours of the lacrimal gland.
ee N
Keratoconjunetivitis sicca
‘* Autoimmune atrophy & fibrosis of the lacrimal gland,
More in females.
# Sjogren syndrome: If associated with arthritis & dry mouth.
=28-
se wires ening am ange
Dr/ Mahmoud Medhat 0113004901
2. Deficiency of the mucin layer:
1, Avitaminosis A.
2. Conjunctival scarring, due to trachoma, chemical burns, Stevens
Jhonson syndrome & ocular cicatricial pimphegoid.
3. Deficiency of the lipid layer: Meibomian Gland Dysfunction.
Symptoms
© Imitation. FB sensation.
© Lack of emotional tears & || response to irritants.
* Deficient precorneal tear film.
* Punctate epithelial erosion.
© Mucous filaments attached to the cornea.
© Conjunctival injection, loss of luster & may be bitot's spots
Investigations
1, Tear film break up time: Diminished.
2. Rose Bengal & fluorescine staining to
demonstrate the degenerated & ulcerated
epithelium, respectively
3. Conjunctival biopsy: Showing the
pathological changes.
4. Schirmer’s test:
Measuring the amount of lacrimal gland secretion by measuring
the wetting of a special filter paper, inserted into the lateral
portion of the inferior fornix.
The filter paper is left for 5 minutes:
Wetting > 15mm: Normal
Wetting < 15mm: Dry eye.
=29-
Dr/ Mahmoud Medhat 0113004901
Treatment 4
. Protective glasses & contact lenses.
1
2. Artificial tears: eye drops &/or ointment
3. Punctum occlusion to reduce drainage
4.
. Systemic steroids for the associated autoimmune cases.
Watery eye
* Lacrimation: Oversecretion of tears, due to:
1. emotional conditions
2. reflex lacrimation: Foreign body, blepharitis,
Keratitis, conjunctivitis, errors of refraction... ..... ete.
~ Epiphora: Overflow of tears over the cheek, due to inadequate
drainage. It may be due to lacrimal pump failure or obstruction
of the lacrimal passages
Epiphora
Aetiology
1. Lacrimal pump failure: >
* Lid margin: Abnormality of the
sharp posterior border
© Ectropion
© Orbicularis muscle: Atony of homer’s muscle & Bell’s palsy.
2. Obstructive epiphora:
1. Puncti:
© Congenital absence
© Post-inflammatory scarring: In trachoma
© Post-traumatic fibrosis
2. Canaliculi:
© Congenital occlusion or stenosis.
© Post-inflammatory & post-traumatic occlusion.
=30-
Dr/ Mahmoud Medhat 0113004901 JZ
© Fungal canaliculitis
3. Lacrimal sac:
© Congenital absence.
© Dacryocystitis (acute & chronic)
¢ Fracture orbit
© Tumours of the lacrimal
4. Nasolacrimal duct:
Congenital imperforation.
© Congestion of the canal veins (50% of cases).
© Fungus in the canal
© Fracture, periostitis & tumours of the maxillary antrum.
5. Nose:
© Adenoids & polyps.
© Deviated nasal septum.
© Hypertrophy of the inferior turbinate
© Rhinoscleroma.
Puncti Canaliculi Lacrimal sac NLD
Congenital | Absence Occlusion or | Absence Imperforate
stenosis,
Traum: Post- Post-traumatic | Fracture orbit | Fracture of
traumatic occlusion the maxillary
fibrosis | antrum
Inflammatory | Post- Post- Dacryocystitis | Periosteitis of
inflammatory | inflammatory the maxillary
scarringe.g. | occlusion antrum
after
trachoma |
Others FBasalash | Fungal Tumours Congestion
canaliculitis
Clinical evaluation & investigations of epiphora
1. History: Exclude lacrimation.
Bilateral_watering of the eye is usually due to lacrimation, while
unilateral watering is usually due to epiphora
2. Examinatio
© Eyelids: Exclude trichiasis, ectropion & blepharitis
© Lacrimal sac: Swelling & dacryocystitis.
© Nose: Polyps & deviated nasal septum,
Dr/ Mahmoud Medhat 0113004901
3. Investigations:
Regurgitation test: Positive in cases with NLD obstruction.
Tones test
Dacryocystography
Plain X-ray: Diagnosis of tumours & fractures.
Tuberculin test for TB.
Diagnostic probing & scintillography.
2, Jones te:
Regurgitation test: Press on the lacrimal sac
against the lacrimal bone
© +ve regurge: Reflux of pus or tears
from the puncti > NLD.
© -ve regurge: No reflux > patent
lacrimal passages.
I. Type I: Instill a
drop of fluoresein in
the conjunctival sac
& insert a cotton
pellet soaked in
xylocaine a
sneezing reflex)
under the inferior
nasal turbinate
Jones Dye Test 1
(Primary) - Positive
Jones Dye Test 1
(Primary) - Negative
© Results
1. The cotton is stained with
fluorescin > patent lacrimal
passages.
2. Not stained: Proceed to Jones
test type II.
II. Type Il: After type 1, irrigate the lacrimal
passage with saline eo
© Results:
ie
1. If fluorescin is recovered: There
is partial or functional
. Jones Dye Test 2
obstruction of the passages. (Secondary) - Negative
Dr/ Mahmoud Medhat 0113004901
2. If fluorescin is not recovered: There is complete
obstruction.
3. Dacryocystograph:
Useful for detection of the following:
¥ Tumours & calculi appearing as filling defect
¥ Time needed to fill & empty the sac.
4, Plain X-ray: To detect tumours & fractures.
Treatment
1. Treatment of the cause e.g. ectropion, nasal causes... ...et
2. Stenosis of the puncti & canaliculi:
© Dilatation & probing
«Laser punctoplasty.
© One snip ampullotomy: Vertical
snip is made in the posterior wall
of the canaliculus. oe
3. Obstruction of the puncti & canaliculi: Hocizeotal Path of Dilator
* Three snip ampullotomy: Removing a triangular area of
the posterior wall of the canaliculus.
© Dacryocystorhinostomy.
4. Nasolacrimal duct obstructio:
1. Congenital obstruction: 2. Acquired obstruction:
© Hydrostatic massage. © Dilatation & probing: fail
© Dilatation & probing, © DCR,
* DCR. © Dacryocystectomy
N
Dr/ Mahmoud Medhat 0113004901
Canaliculitis
Definition: Inflammation of the lacrimal canaliculi with
“pyogenic organism, °trachoma, specific organism or
“fungus.
Commonest cause is mycotic canaliculitis, caused by
actinomyces Israeli
Sympton
Signs:
© Chronic conjunctivitis, most marked at the medial canthus,
© Prominent & dilated lacrimal punctum (Patulous)
© Regurgitation test: Muco-purulent discharge which may contain
concretions
‘Treatment:
Canaliculotomy: Slit the posterior wall of the canaliculus, curettage of the
fungal masses & irrigation with slaine.
: Persistent epiphora, not responding to treatment.
inflammations of the lacrimal sac
(Dacryocystitis)
1. Adult dacryocystitis
* Acute dacryocystitis.
hronic dacryocystitis.
2. Infantile dacryocystitis (Congenital NLD obstruction).
Acute dacryocys
Definition: Acute suppurative inflammation of the ——-~
lacrimal sac.
Etiology
Predisposing factors:
© Nasolacrimal duct obstruction © Chronic dacryocystitis
Causative agent:
* Pneumococei * Staphylococei * Streptococci.
Symptoms
1. Severe pain. 2. Fever 3. Epiphora.
Signs
1, Tender swelling of the lacrimal sac
a4
Dr/ Mahmoud Medhat 0113004901
2. Marked edema & redness of the skin over the sac oe
3. Regurgitation test: Reflux of pus, unless pericysttis occurs.
4. Abscess formation with fluctuation.
Complications
1. Lacrimal fistula: Anterior bursting of the sac through the skin.
Pyocele: Obstruction of the canaliculi & distension of the sac with pus.
Orbital cellulites: Znding in optic nerve atrophy © blindness
Cavernous sinus thrombosis (CST)
aA Re DP
Chronic dacryocyst
Treatment
1. During the acute phase:
sstemic & topical antibioti
© Hot fomentations,
© Lotions: To clear pus.
© Incision & drainage: If an abscess forms
2. After subsidence of the acute attack:
Dacryocystorhinostomy (DCR) +/- fistulectomy.
Chronic dacryocystitis
Definitior
Chroni
inflammation of the lacrimal sac secondary to
obstruction of the nasolacrimal duct. This is the commonest lacrimal sac disorder.
Etiology
Predisposing factors:
© Nasolacrimal duct obstruction «Acute dacryocystitis
Causative agent:
* Pneumococci: 80% of cases
© Staph, Strept, Trachoma & Fungi
© TB& Syphilis: Rare.
Dr/ Mahmoud Medhat 0113004901
Symptoms
1. Watery eye. 2. Discharge.
Signs
1, Red & hyperaemic inner canthus
2, Swelling of the lacrimal sac: Below the medial palpebral ligament.
3. +ve regurgitation test: Regurgitation of mucous or pus. It becomes
-ve on formation of a mucocele.
Complications
1. Chronic conjunctivitis.
2. Vicious circle of epiphora, eczema & ectropion
Hypopyon ulcer.
eee
Endophthalmitis: Following an intraocular operation.
”
Mucocele & pyocele: If the canaliculi are obstructed
6. Acute dacryocys
Investigations: The same as epiphora
Treatment
is, abscess & lacrimal fistula.
Aim:
1, Restore communication between the lacrimal sac & the nose.
2. Treatment of infection
Lines
1, Treatment of the cause of obstruction
2. Dacryocystorhinostomy:
Principle: Connecting the lacrimal
sac to the nasal mucosa >
bypassing the obstructed NLD.
Indications:
Dr/ Mahmoud Medhat 0113004901
stitis
© Chronic dacryocy:
© Mucocele of the lacrimal sac
© Lacrimal fistula (+ fistulectomy),
Contraindications:
Extensive adhesions & neglected cases.
Nasal pathology e.g. atrophic rhinitis.
© T.B. & lacrimal sac tumours.
© Hypopyon ulcer.
3. Dacryocystectomy:
Principle: Removal of the lacrimal sac.
Indications: Neglected cases, when DCR is contraindicated.
Congenital NLD obstruction (iiantile dacryocystitis)
Etiology: Imperforate hasener’s valve (Most common).
Symptoms: Epiphora, 2-3 weeks after birth, is reported by the mother.
Signs
1. Regurgitation test > clear fluid, mucous or frank pus.
2. Recurrent conjunctivitis
Treatment
1. Hydrostatic massage: Instruct the mother to press on the lacrimal sac
in a downwards direction. This may help removing any epithelial remnants
& opening hasener's valve.
. Antibiotics.
. Repeated syringing & irri
ak wD
3
3
&
5
e
g
a
¢
g
. Intubation of the lacrimal drainage system (Silicone tube).
2
Dacryocystorhinostomy (DCR).
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Business English Course BookDocument250 pagesBusiness English Course BookSoodn Kang Soodn100% (5)
- Pharm Cvs McqsDocument30 pagesPharm Cvs McqsSoodn Kang Soodn100% (3)
- Surgery McqsDocument10 pagesSurgery McqsSoodn Kang SoodnNo ratings yet
- Uveal TractDocument11 pagesUveal TractSoodn Kang SoodnNo ratings yet
- OrbitDocument9 pagesOrbitSoodn Kang SoodnNo ratings yet
- ConjunctivaDocument23 pagesConjunctivaSoodn Kang SoodnNo ratings yet
- GlaucomaDocument24 pagesGlaucomaSoodn Kang SoodnNo ratings yet
- Eyelid 2011Document25 pagesEyelid 2011Soodn Kang SoodnNo ratings yet
- ScleraDocument2 pagesScleraSoodn Kang SoodnNo ratings yet
- RetinaDocument19 pagesRetinaSoodn Kang SoodnNo ratings yet
- 6 Diuretics UnlockedDocument17 pages6 Diuretics UnlockedSoodn Kang SoodnNo ratings yet
- Pharm DR Ahmed Abd AlrahmanDocument24 pagesPharm DR Ahmed Abd AlrahmanAmrAliTahaNo ratings yet
- Nem-Szteroid Gyulladásgátlók (Nsaids) : 1. Gyulladásgátlás 2. Fájdalomcsillapítás 3. LázcsillapításDocument34 pagesNem-Szteroid Gyulladásgátlók (Nsaids) : 1. Gyulladásgátlás 2. Fájdalomcsillapítás 3. LázcsillapításSoodn Kang SoodnNo ratings yet
- 10 CNS UnlockedDocument51 pages10 CNS UnlockedSoodn Kang SoodnNo ratings yet
- Antidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Document27 pagesAntidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Soodn Kang SoodnNo ratings yet
- Local Anaesthetics Mcqs From LouisDocument2 pagesLocal Anaesthetics Mcqs From LouisSoodn Kang SoodnNo ratings yet
- Hallgatok VeglegesDocument3 pagesHallgatok VeglegesSoodn Kang SoodnNo ratings yet
- DermatologyDocument21 pagesDermatologySoodn Kang SoodnNo ratings yet
- AntiarritmiasSzerek 2016-2-8Document30 pagesAntiarritmiasSzerek 2016-2-8Soodn Kang SoodnNo ratings yet
- LokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Document14 pagesLokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Soodn Kang SoodnNo ratings yet
- Epidemiology of CholeraDocument26 pagesEpidemiology of CholeraSoodn Kang SoodnNo ratings yet
- CardiologyDocument10 pagesCardiologySoodn Kang SoodnNo ratings yet
- Case Studies in The Management of Acs With GP Iib/Iiia InhibitorsDocument47 pagesCase Studies in The Management of Acs With GP Iib/Iiia InhibitorsSoodn Kang SoodnNo ratings yet
- ورق مذاكره Ent في 100 صفحه بسDocument100 pagesورق مذاكره Ent في 100 صفحه بسSoodn Kang SoodnNo ratings yet
- 2011 - Patient PresentationDocument12 pages2011 - Patient PresentationSoodn Kang SoodnNo ratings yet
- Angol Oktatás - VTVSSVTDocument5 pagesAngol Oktatás - VTVSSVTSoodn Kang SoodnNo ratings yet
- Diagnosis 3Document10 pagesDiagnosis 3Soodn Kang SoodnNo ratings yet
- Autonomic Drugs Flash CardsDocument16 pagesAutonomic Drugs Flash CardsSoodn Kang SoodnNo ratings yet