Professional Documents
Culture Documents
IGI - Perfint Poster PDF
IGI - Perfint Poster PDF
Uploaded by
Shubham JainOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IGI - Perfint Poster PDF
IGI - Perfint Poster PDF
Uploaded by
Shubham JainCopyright:
Available Formats
Computer Assisted Planning And Image-guided Robotics In
CT-guided Interventional Procedures
Prashanth Dumpuria, Gnanasekar Velusamya, Anjali Kulkarnia,
Arun Tirumalaia, David Gustafsona and Laura Crocettib
aPerfint Healthcare Corporation bDepartment of Surgical Pathology, Medicine, and Molecular Area Critics University of
Pisa, Italy
Introduction Therefore for a given target, two sets of distances were obtained (one for
1. showed
TM
MAXIO is a user controlled, stereotactic accessory intended to assist in the freehand insertion and the other for robotic targeting). Koethe et al
planning and manual advancement of one or more instruments during CT- that when compared to the freehand insertion, MAXIO reduced both the mean
guided percutaneous procedures such such as ablation, biopsy, drainage, needle tip-to-target error and the mean needle path-to-target error by 59%.
FNAC and pain management. MAXIOs workflow can be divided into the
following four steps: 1) See 2) Plan 3) Treat 4) Verify. Figure 1a shows a Clinical Experiences
MAXIO system with its various components and Figure 1b highlights the In a series of 147 interventional procedures completed at 9 different clinical
different steps in a typical workflow. sites between December 2012 and November 2013, we measured the 3D
Figure 1a. MAXIO docked on patients left side. A: distance between the planned and actual needle tip and results have been
Docking plate and mechanism B: Planning system C: presented in Table 2. It should be noted that needle insertions and targeting
Robotic positioner D: End effector and needle guide were done by expert clinicians in all 9 sites and clinical conditions during the
used to hold the needle in place. Zoomed inlet shows interventional procedures were not altered in any fashion. Averaging over all
the docking plate fixed to the floor of the CT suite and
the sites, the mean targeting error was found to be 2.6mm 2.1mm. It is worth
the unique asymmetrical pattern used to register the
noting that the stereotactic accuracy was either comparable or slightly better
device to the CT scanner. MAXIO uses an optical camera
and a proprietary optical registration algorithm for this even in cases where (a) multiple needles were used (34/170 needle insertions
registration. In addition there is a tilt sensor affixed to were multiple needle procedures and accuracy was found to be
the bottom of the device which ensures that the device 2.5mm1.5mm) and, (b) complex angulations and needle trajectories were
is always in its calibrated state. required because the tumors were located close to sensitive structures like
major blood vessels, bowels and lungs (37/170 needle insertions required
Image Registration Plan needle/probe complex needle trajectories and accuracy was found to be 2.3mm 1.6mm).
Execute plan
between phases path, Table 2. Stereotactic Accuracy of MAXIO measured at 9 different clinical sites
Ablation volume over a total of 147 procedures. Clinical conditions have been reported as
visualization, observed during the procedures and they were not altered or modified in any
tumor coverage fashion because of MAXIO.
Segmentation Number of
Mean Std. dev.
TREAT Clinical Conditions needle
(both in mm)
placements
Verify needle placement or Respiratory motion With Breath hold 63 2.3 1.9
treatment e.g. use post- management Without Breath hold 107 2.8 2.2
procedural ablation images
SEE PLAN and register with planned With patient immobilizer 103 2.3 1.7
Patient movement
image to check for complete Without patient
management 67 3.0 2.5
coverage immobilizer
Ablation/IRE 33 2.7 1.8
Figure 1b. Different steps in a
Biopsy 107 2.6 2.4
typical MAXIO-assisted workflow
Type of procedure Drainage 5 1.7 1.0
FNAC 2 1.0 0.0
VERIFY Pain management 21 2.4 1.2
Abdomen 49 2.3 1.6
Anatomical Region Pelvic 107 2.2 1.2
Planning Methods and Results Thorax 5 3.0 2.7
Single needle procedure 136 2.6 2.2
MAXIO uses a semi-automatic atlas-based segmentation for liver
# of needles Multiple needle
segmentation and an interactive intensity based segmentation algorithm for 34 2.5 1.5
tumors, vessels and other organs such as gall bladder, kidneys and pancreas. procedure
Once the organs and tumor have been segmented, clinicians can plan < 3cm 9 1.9 1.8
interventional procedures in 2D or 3D by selecting the target and entry points 3cm 5cm 33 2.4 1.9
Target depth 5.1cm 7.5cm 15 2.3 1.5
for the needles/probes. MAXIO facilitates ablation planning by superimposing
7.6cm 10cm 66 2.8 2.5
the ablation zone (obtained from ablation probe manufacturers) over the 3D
> 10cm 47 2.3 1.6
surface of tumor (obtained from segmentation).
Combination of cranio-
In order to asses the value of computer-assisted planning in liver ablations, 37 2.3 1.6
cadual and orbital angles
Crocetti et al2. conducted a retrospective study of 16 patients with metastatic Trajectories with no
colorectal cancer in the liver (18 lesions in total). For all 18 lesions, they Angulation in deviation about the 6 3.0 3.7
planned ablation procedures manually and using MAXIO and studied all needle trajectories orbital axis
deviations in MAXIO-assisted plans from manual plans (deviation being Trajectories with no
described as change in ablation strategy or a change in ablation protocol or a deviation about the 133 2.6 2.2
change in the planned needle path). Table 1 shows the results of their study cranio-caudal axis
and as seen in the table Crocetti et al2. observed that 3D planning using
MAXIO changed their ablation strategy in 61% of the cases (for example in Conclusions
39% of the cases they had to change the entry point for the ablation needle Comparing the plans generated using MAXIO to manual planning, Crocetti et
and in 50% of the cases they had to change either the ablation technology or al2. demonstrated the need for computer-assisted planning during ablation
use additional ablation probes. procedures. In phantom experiments we demonstrated that MAXIO improved
Deviations in MAXIO-assisted planning compared
Table 1. Results of the 16 patient the needle placement accuracy. Based on our anecdotal observations during
to manual planning (16 patients, 18 lesions)
(18 lesions total) retrospective interventional procedures it could be said that MAXIO is accurate and its
Change in Change in planned Any change study conducted at University of accuracy can be repeated across most clinical scenarios encountered during
ablation protocol needle trajectory Pisa, Italy to assess the need for
interventional procedures.
computer assisted planning in
9/18 (50%) 7/18(39%) 11/18 (61%) liver ablation procedures. Several studies3,4,5 have shown that customized ablation planning and
improved needle placement accuracy during interventional procedures may (a)
Targeting Methods and Results clinically translate to decreased complication rates (b) lead to greater sampling
success during biopsies (c) decrease recurrence rates during ablations and,
Once the planning is complete, clinicians execute their planned needle path (d) reduce radiation exposure during pain management procedures. While
with the help of stereotactic needle positioner in MAXIO. It should be noted more studies are needed, we are optimistic about the promising role for
that clinicians can plan and advance up to six needles using MAXIO in either a MAXIO in percutaneous CT-guided interventional procedures.
sequential or a simultaneous fashion. Upon executing the plan, clinicians can
obtain CT scans and using image fusion (non-rigid registration for liver ablation Acknowledgements
procedures and an intensity based rigid registration for other organs and
We would like to acknowledge the following clinicians for their time, efforts and
procedures), clinicians can compare the planned needle trajectories to the
valuable inputs: Dr. L. Khanh at 108 Military Hospital, Vietnam; Dr. K. Thomson
actual needle path. In order to evaluate the accuracy of needle placements
at Alfred Hospital, Australia; Drs. R. Santosham and Vandana at Adyar Cancer
using MAXIO, we conducted a series of phantom and in-vivo experiments. Institute, India; Dr. Shyam at Christian Medical College, India; Dr. C.
Masciocchi, San Salvatore Hospital, Italy; Drs. S. Kulkarni and N. Shetty at
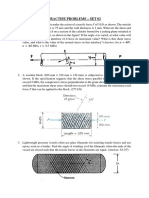
Phantom Experiments Tata Memorial Cancer Center, India; Dr. Abdullah at University of Malaysia
Using an abdominal phantom (3D abdominal Medical Center, Malaysia; Drs. Vogl and Zangos at University of Frankfurt,
phantom model 057, CIRS, Norfolk, VA, Germany, Dr. Iyangaran at Rajiv Gandhi Government Hospital, India and Drs.
USA) Koethe et al1. compared the accuracy A. M. Venkatesan and B. Wood at National Institutes of Health, USA.
of freehand single-pass needle insertions to Needle
tip-to-
insertions facilitated using MAXIO. Twenty
virtual targets were selected and targeted at
target References
distance 1. Koethe Y. et al. Eur Radiol, 2014, 24(3):723-730
complex angles (average angulation of
65deg) using 18-gauge, 15cm needles. With 2. Crocetti L. et al. WCIO 2013 (presented as a talk)
the needles still in place, CT scans were 3. Tiong L. et al., Br J Surg, 2011, 98:1210-1224
obtained and used to measure the needle Needle path-to- 4. Kobayashi K et al. Radiographics, 2012, 32:1483-1501
tip-to-target distance and needle path-to- target distance 5. Best SL et al., JURO, 2012, 187:1183-1189
target distance.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- EECS16A: Homework 3: Problem 5: Segway ToursDocument8 pagesEECS16A: Homework 3: Problem 5: Segway ToursShubham JainNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Import Data From TEMS Pocket To IBwaveDocument13 pagesImport Data From TEMS Pocket To IBwavecyo3fffNo ratings yet
- An Agent-Based Model To Simulate Motorcycle BehaviourDocument227 pagesAn Agent-Based Model To Simulate Motorcycle Behaviourhasib100% (6)
- Angular Interview Questions MochaDocument4 pagesAngular Interview Questions Mocharavishkumar_p0% (1)
- New Section 4Document1 pageNew Section 4Shubham JainNo ratings yet
- Untitled Presentation PDFDocument1 pageUntitled Presentation PDFShubham JainNo ratings yet
- Part Iii: Physics Section - I Single Correct Choice TypeDocument8 pagesPart Iii: Physics Section - I Single Correct Choice TypeShubham JainNo ratings yet
- ResonanceDocument48 pagesResonancePrakash Nik79% (92)
- Faculty: Tutorial Sheet: Review Date: 01/03/2014Document2 pagesFaculty: Tutorial Sheet: Review Date: 01/03/2014Shubham JainNo ratings yet
- Wi-Fi Instructions v1.2Document4 pagesWi-Fi Instructions v1.2Shubham JainNo ratings yet
- Computer SC NotesDocument8 pagesComputer SC NotesShubham JainNo ratings yet
- C ElectrochemistryDocument10 pagesC ElectrochemistryShubham JainNo ratings yet
- A Problem Book in Mathematical Analysis - G.N. Berman (1977)Document463 pagesA Problem Book in Mathematical Analysis - G.N. Berman (1977)Ohana Nana100% (1)
- ARM Instruction Set Quick Reference Card: Key To TablesDocument3 pagesARM Instruction Set Quick Reference Card: Key To TablesVasile MorariuNo ratings yet
- Major: Electrical Submersible Drainage PumpDocument1 pageMajor: Electrical Submersible Drainage Pumpjacques PerronNo ratings yet
- IND226Document42 pagesIND226bkssdgNo ratings yet
- Structural Control On Gold Mineralization at Walhalla VictoriaDocument25 pagesStructural Control On Gold Mineralization at Walhalla VictoriaMartin NguyenNo ratings yet
- Practise Problems Set02Document5 pagesPractise Problems Set02rohit kumarNo ratings yet
- Class 8 Exemplar 7 PDFDocument32 pagesClass 8 Exemplar 7 PDFSarvesh Kumar Rai0% (1)
- CFD Simulation Open Foam Backward Facing StepDocument6 pagesCFD Simulation Open Foam Backward Facing StepJennifer DouglasNo ratings yet
- Archive of SIDDocument14 pagesArchive of SIDBingkat MacarimbangNo ratings yet
- Ece III Network Analysis (10es34) NotesDocument111 pagesEce III Network Analysis (10es34) NotesGautam Sharma80% (10)
- Buderus Thermal Solar Systems BrochureDocument4 pagesBuderus Thermal Solar Systems Brochuree-ComfortUSA100% (1)
- AUSPOS GPS Processing Report: Geodesy@ga - Gov.auDocument7 pagesAUSPOS GPS Processing Report: Geodesy@ga - Gov.auTrhas TeameNo ratings yet
- 5 - Behaviour of GasesDocument37 pages5 - Behaviour of Gasessiaskel100% (1)
- Outdoor - Units - MOU 12HDN1 - MOUB 36HDN1 R220075500920 - MOUB 48HDN1 R220075700690 - MOUD 60HDN1 R - MOUA 60HRDN1Document48 pagesOutdoor - Units - MOU 12HDN1 - MOUB 36HDN1 R220075500920 - MOUB 48HDN1 R220075700690 - MOUD 60HDN1 R - MOUA 60HRDN1Muhidin KozicaNo ratings yet
- 2 Amount Spent On Travel: Age GenderDocument6 pages2 Amount Spent On Travel: Age GenderMayank PatelNo ratings yet
- HART ProtocolDocument18 pagesHART ProtocolAnonymous zMWvcTNo ratings yet
- Technical Specification Sandvik LH209L 06 PDFDocument3 pagesTechnical Specification Sandvik LH209L 06 PDFEnrique CalquínNo ratings yet
- Dimensioning 07-08Document50 pagesDimensioning 07-08Ankit KumarNo ratings yet
- Lesson 1 Exercises Problem No. 1Document2 pagesLesson 1 Exercises Problem No. 1Ariel GamboaNo ratings yet
- Metamorphism 4: Metamorphic Facies: GY 111 Lecture NotesDocument4 pagesMetamorphism 4: Metamorphic Facies: GY 111 Lecture NotesSukesh NayakNo ratings yet
- CutOff Report RP 2016Document17 pagesCutOff Report RP 2016AdityaBhagiNo ratings yet
- Connections and Working Principles of Three-Phase Distribution Transformers - EEPDocument13 pagesConnections and Working Principles of Three-Phase Distribution Transformers - EEPSanilBalakrishnanNo ratings yet
- Shuttle Valve PDFDocument17 pagesShuttle Valve PDFBenjamin Musa ダNo ratings yet
- E6000 Complete Operating ManualDocument154 pagesE6000 Complete Operating ManualsudeshbhagganNo ratings yet
- Xii 1 - Brochure Sihi LPHX 45008 45311 45316Document16 pagesXii 1 - Brochure Sihi LPHX 45008 45311 45316Usri AdiNo ratings yet
- Roger G Walker - TurbiditeDocument12 pagesRoger G Walker - TurbiditeJemmy HaryantoNo ratings yet
- Preformulation Studies For Amoxicillin Trihydrate and Dicloxacillin Sodium AsDocument6 pagesPreformulation Studies For Amoxicillin Trihydrate and Dicloxacillin Sodium AsMuthia FadhilaNo ratings yet