Professional Documents
Culture Documents
Hypertensive Urgency/Emergency: Subcategory Defns... - Malignant HTN: Retinal Hemorrhages, Exudates, or Papilledema)
Uploaded by
Dhira 'Princess Kalonk' AninditaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hypertensive Urgency/Emergency: Subcategory Defns... - Malignant HTN: Retinal Hemorrhages, Exudates, or Papilledema)
Uploaded by
Dhira 'Princess Kalonk' AninditaCopyright:
Available Formats
Thayer Firm 2005-2006
HYPERTENSIVE URGENCY/EMERGENCY
Hypertensive urgency = BP alone
Hypertensie emergency = BP + end-organ damage
Subcategory defns... - malignant htn: retinal hemorrhages, exudates, or papilledema)
- malignant nephrosclerosis: renal involvement
- htnsive encephalopathy: signs of cerebral edema (from breakthru hyperperfusion)
End organs that can be involved...
Eye - retinal hemorrhages, exudates
- papilledema (Si of ICP)
Brain - ICP d/t cerebral edema: presents as h/a -> n/v -> delta MS
- stroke/bleed
- seizure
Lung - pulm edema (Si of CHF)
Heart/vessel - MI
- Ao dissection
- CHF
Kidney - ARF -> acute Cr, hematuria, proteinuria
Blood - hemolytic anemia (MAHA)
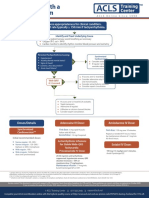
Acute management
1. Cardiac monitor; consider step-down bed or unit, particularly if emergency (consider a-line if emergency)
2. If DBP >110, lower by 10-15% or to 110 mmHg
st
3. Lower MAP by max 25% in the 1 24 hrs (any faster risks cerebral hypoperfusion)
- lower over minutes if emergency (start with IV meds)
- lower over hours if urgency (can start with either PO or IV meds)
4. Options for acute treatment...
B-blockers CCB Nitrates ACEi Other
metop po or IVP nifedipine XL po NTG gtt (not as captopril po clonidine po
labetolol IVP or gtt nicardipine gtt effective at BP) enalapralit gtt fenoldopam IV
esmolol gtt
good for HR, CP, good for ARF, good for active CP, consider in low EF,
ACS, h/o CAD, hypertensive ACS, pulm edema AR, MR, but avoid in
hypertensive encephalopathy (along with lasix & ARF
encephalopathy nitroprussside)
Note: in Ao dissection, use labetolol (or nitroprusside + esmolol); in eclampsia, use hydralazine, labetolol, or nicardipine
5. After BP controlled on IVs, start transitioning to PO meds
Chronic management
Consider work-up for secondary causes of hypertension if not already done & cause unclear.
You might also like
- Emergency Hypertension (Herbesser Injection)Document18 pagesEmergency Hypertension (Herbesser Injection)suho exoNo ratings yet
- Target Organ Damage in Hypertensive EmergenciesDocument45 pagesTarget Organ Damage in Hypertensive EmergenciesYoga YudhistiraNo ratings yet
- Final Copy HTN EmergencyDocument13 pagesFinal Copy HTN EmergencyabrarNo ratings yet
- 2019 Apr Common Treatment OrdersDocument32 pages2019 Apr Common Treatment OrdersChris Jardine LiNo ratings yet
- 2020 Apr Common Treatment OrdersDocument32 pages2020 Apr Common Treatment OrdersAlistair LauNo ratings yet
- Crisis Hypertension: Dr. Isra Sukhraini NSTDocument21 pagesCrisis Hypertension: Dr. Isra Sukhraini NSTAndika SiswantaNo ratings yet
- OSCE EmergencyDocument26 pagesOSCE EmergencyXu PeihaoNo ratings yet
- StrokeDocument6 pagesStrokekun rugerNo ratings yet
- Hypertensive Emergencies in the EDDocument37 pagesHypertensive Emergencies in the EDAyesh EKNo ratings yet
- Urgences Hypertensives-1Document27 pagesUrgences Hypertensives-1Gedeon MotsaNo ratings yet
- Hipertensi EmergencyDocument31 pagesHipertensi Emergencysar tikaNo ratings yet
- Hypertensive CrisisDocument36 pagesHypertensive Crisisashwin choubeyNo ratings yet
- A.2 Category B and e Pharma ActDocument7 pagesA.2 Category B and e Pharma ActMichael Angelo CarballoNo ratings yet
- High Yield Surgery Shelf Exam Review CompleteDocument10 pagesHigh Yield Surgery Shelf Exam Review CompleteAmir Ali100% (1)
- Hypertensive Crisis ManagementDocument27 pagesHypertensive Crisis ManagementDian Puspa100% (1)
- Crisis of Hypertension Revised 1Document57 pagesCrisis of Hypertension Revised 1Ratna Puspa RahayuNo ratings yet
- Management of Hypertensive EmergencyDocument35 pagesManagement of Hypertensive EmergencyRaditya Indah TofaniNo ratings yet
- Hipertensi KrisisDocument30 pagesHipertensi KrisisLuthfan HakimNo ratings yet
- HypertensionDocument15 pagesHypertensionAns SaroobNo ratings yet
- Tips On How To Answer An Essay Question by Doaa Kamal 2001Document9 pagesTips On How To Answer An Essay Question by Doaa Kamal 2001Amr El TaherNo ratings yet
- Managing Hypertensive CrisesDocument31 pagesManaging Hypertensive CrisesAmanda DavisNo ratings yet
- Critical Event ChecklistsDocument25 pagesCritical Event ChecklistsarisyiNo ratings yet
- Arrhythmias EmergencyDocument10 pagesArrhythmias EmergencyNITACORDEIRONo ratings yet
- Crisis of Hypertension Revised 1Document57 pagesCrisis of Hypertension Revised 1keenmunir100% (4)
- Hipertensi EmergencyDocument31 pagesHipertensi Emergencyintan trimauliaNo ratings yet
- Anesthetic Consideration in Hypertensive PatientDocument11 pagesAnesthetic Consideration in Hypertensive PatientYosiAsmaraNo ratings yet
- Emergency Internal Medicine: Hypertensive EmergenciesDocument104 pagesEmergency Internal Medicine: Hypertensive EmergenciesMotivation VoiceNo ratings yet
- Dx. StudyDocument3 pagesDx. Studymayumitanaka8042No ratings yet
- ShockDocument2 pagesShockKemal TaufikNo ratings yet
- Case Based Presentation: Hypertension in The ICU: by Noemie Chessex and Colleagues UBCDocument52 pagesCase Based Presentation: Hypertension in The ICU: by Noemie Chessex and Colleagues UBCmabs_LVNo ratings yet
- Cerebrovascular Accidents: Stroke Versus TIADocument19 pagesCerebrovascular Accidents: Stroke Versus TIASagar ShahNo ratings yet
- Nclex Study Content - UseDocument65 pagesNclex Study Content - Usesbrooks6914100% (22)
- Hypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)Document31 pagesHypertensive Emergencies: BY: Dr. Imtiyaz Hashim (PGR) Dr. Khalida Baloch (Ho)امتیاز ہاشم بزنجوNo ratings yet
- Neuro Notes Misc.Document11 pagesNeuro Notes Misc.slmrebeiroNo ratings yet
- Lecture 9Document10 pagesLecture 9Grafu Andreea AlexandraNo ratings yet
- Norepinephrine Drug CardDocument2 pagesNorepinephrine Drug CardYou know who100% (9)
- FINALS ch31Document6 pagesFINALS ch31Monica JubaneNo ratings yet
- Fundamentals of Stroke and TIADocument12 pagesFundamentals of Stroke and TIAMaria WibawaNo ratings yet
- DDX For Oral BoardsDocument10 pagesDDX For Oral BoardshufxllholmbjxwwotmNo ratings yet
- 1.1. Krisis Hipertensi - Dr. Saugi AbduhDocument29 pages1.1. Krisis Hipertensi - Dr. Saugi AbduhdmaulidaNo ratings yet
- Cardiology 2Document70 pagesCardiology 2erickNo ratings yet
- ACLS Simulation ScenariosDocument14 pagesACLS Simulation ScenariosVanessa HermioneNo ratings yet
- CVSDocument128 pagesCVSearldem1996No ratings yet
- Krisis HipertensiDocument27 pagesKrisis HipertensiAmanda Padma100% (1)
- Case Study #4 - Presenting With Headache What's The Diagnosis - AtfDocument18 pagesCase Study #4 - Presenting With Headache What's The Diagnosis - Atfjidduadithya2004No ratings yet
- Lecture 4Document4 pagesLecture 4Grafu Andreea AlexandraNo ratings yet
- ADK Final Version-UpdatedDocument135 pagesADK Final Version-UpdatedDaal ChawlNo ratings yet
- Er FinalsDocument63 pagesEr FinalsNaren RaviNo ratings yet
- Hypertensive Encwphalopathy 1Document25 pagesHypertensive Encwphalopathy 1saldy meirisandyNo ratings yet
- Cardiac AnesthesiologyDocument48 pagesCardiac AnesthesiologyNiaNo ratings yet
- Acute Stroke Lecture (Fall 2021) 2Document47 pagesAcute Stroke Lecture (Fall 2021) 2shahad alghamdiNo ratings yet
- Drugs For ShockDocument3 pagesDrugs For Shockrenz bartolomeNo ratings yet
- Hypertensive Crises - Current ApproachDocument35 pagesHypertensive Crises - Current ApproachShre RanjithamNo ratings yet
- Heart Failure: Christian Rey Cayabyab Y3 Medical Student University of LimerickDocument16 pagesHeart Failure: Christian Rey Cayabyab Y3 Medical Student University of LimerickChristian CayabyabNo ratings yet
- Nclex Pharm ReviewDocument10 pagesNclex Pharm ReviewRuiqi YangNo ratings yet
- Propranolol side effects nursing implicationsDocument4 pagesPropranolol side effects nursing implicationsLiza M. PurocNo ratings yet
- Hypertensiveemergencies RullDocument60 pagesHypertensiveemergencies RullagustinaNo ratings yet
- Raised Intracranial Pressure: BY DR - Tallat Pervaiz AliDocument37 pagesRaised Intracranial Pressure: BY DR - Tallat Pervaiz AliCh Khurram HasnainNo ratings yet
- Acls Drug OverviewDocument2 pagesAcls Drug OverviewShannon Davis100% (1)
- DIAGNOSING HYPERTENSION: BLOOD PRESSURE MEASUREMENT GUIDEDocument37 pagesDIAGNOSING HYPERTENSION: BLOOD PRESSURE MEASUREMENT GUIDEDhira 'Princess Kalonk' AninditaNo ratings yet
- Algo Tachycardia PDFDocument1 pageAlgo Tachycardia PDFYudhistira AdiNo ratings yet
- Fluid and Electrolytes PDFDocument67 pagesFluid and Electrolytes PDFAsti UtariNo ratings yet
- Fire Risk Assessment TemplateDocument39 pagesFire Risk Assessment TemplateDhira 'Princess Kalonk' Anindita67% (3)
- Fluid and Electrolyte TherapyDocument12 pagesFluid and Electrolyte TherapyDhira 'Princess Kalonk' AninditaNo ratings yet
- Effects of Hypothermia on Childhood Outcomes After Perinatal AsphyxiaDocument20 pagesEffects of Hypothermia on Childhood Outcomes After Perinatal AsphyxiaDhira 'Princess Kalonk' AninditaNo ratings yet
- Hospital Incident Command System Guidebook 2006Document113 pagesHospital Incident Command System Guidebook 2006Dhira 'Princess Kalonk' AninditaNo ratings yet
- Drug Policy in The NetherlandsDocument19 pagesDrug Policy in The NetherlandsDhira 'Princess Kalonk' AninditaNo ratings yet
- How It Works - Human BodyDocument180 pagesHow It Works - Human BodyMargo Sun94% (36)
- Chamber One-The Neuro Chemistry of Sex-Level 2Document9 pagesChamber One-The Neuro Chemistry of Sex-Level 2Atyeb Ba Atum Re100% (1)
- Syllabus DresserDocument2 pagesSyllabus DresserVikash Aggarwal50% (2)
- IKD 2 - Imaging Renal InfectionDocument49 pagesIKD 2 - Imaging Renal InfectionRenal Association MauritiusNo ratings yet
- Digestive System GuideDocument25 pagesDigestive System GuideprabuNo ratings yet
- Extrahepatic Biliary ObstructionDocument44 pagesExtrahepatic Biliary ObstructionOssama Abd Al-amierNo ratings yet
- Medical Neuroscience Tutorial Notes: Overview of Neural SignalingDocument2 pagesMedical Neuroscience Tutorial Notes: Overview of Neural SignalingOmar AlemánNo ratings yet
- TSH Conversion PDFDocument1 pageTSH Conversion PDFMarianNo ratings yet
- St. Paul School Science Exam PrepDocument3 pagesSt. Paul School Science Exam PrepIrish Jhaizel Kaye FuentesNo ratings yet
- DLL in GEN BIODocument14 pagesDLL in GEN BIOBernadette Jeane Aquino GarciaNo ratings yet
- Lecture: Adrenal DisordersDocument78 pagesLecture: Adrenal DisordersOchendo KingxNo ratings yet
- Test Bank For Fundamentals of Human Physiology 4th Edition by Sherwood PDFDocument9 pagesTest Bank For Fundamentals of Human Physiology 4th Edition by Sherwood PDFa693443706No ratings yet
- Summary of CT Brain Reporting PDFDocument15 pagesSummary of CT Brain Reporting PDFMainak DeNo ratings yet
- Unusual Presentation of Uterine Leiomyoma: Samer Al Hadidi, Tabrez Shaik Mohammed, Ghassan BachuwaDocument3 pagesUnusual Presentation of Uterine Leiomyoma: Samer Al Hadidi, Tabrez Shaik Mohammed, Ghassan BachuwaSafira SalsabilaNo ratings yet
- Physioloical Integrity Acute Biologic CrisisDocument42 pagesPhysioloical Integrity Acute Biologic CrisisJohn Paul M. TagapanNo ratings yet
- Endocrine System Worksheet AnswersDocument3 pagesEndocrine System Worksheet AnswersmariaNo ratings yet
- Chapter 3 Leukocyte Circulation and Migration Into TissuesDocument24 pagesChapter 3 Leukocyte Circulation and Migration Into Tissues13701319477No ratings yet
- 12 Pairs of Cranial Nerves and Their FunctionsDocument37 pages12 Pairs of Cranial Nerves and Their FunctionsCiprian RataNo ratings yet
- Digestion LabDocument7 pagesDigestion LabnicewanNo ratings yet
- The artery most likely to be eroded in perforation of the posterior wall of the first part of the duodenum is the superior pancreaticoduodenal artery. It is a branch of the gastroduodenal arteryDocument33 pagesThe artery most likely to be eroded in perforation of the posterior wall of the first part of the duodenum is the superior pancreaticoduodenal artery. It is a branch of the gastroduodenal arteryWahida Amalin Ab RazakNo ratings yet
- Insuficiencia Renal CronicaDocument13 pagesInsuficiencia Renal CronicaCarlos DNo ratings yet
- Test Bank For Medical Terminology Simplified A Programmed Learning Approach by Body System 6th Edition Barbara A Gylys Regina M Masters DownloadDocument15 pagesTest Bank For Medical Terminology Simplified A Programmed Learning Approach by Body System 6th Edition Barbara A Gylys Regina M Masters Downloadchristinemays21121993bgw100% (21)
- Hydrocephalus Teori FinalDocument19 pagesHydrocephalus Teori Finalaurelia_rlNo ratings yet
- Hemodialysis+Hemoperfusion Improves ESRD ComplicationsDocument32 pagesHemodialysis+Hemoperfusion Improves ESRD ComplicationsAzzis MualifNo ratings yet
- UB Human Physiology Syllabus 2012Document5 pagesUB Human Physiology Syllabus 2012Anonymous MPdGkx87bNo ratings yet
- Brain FactsDocument71 pagesBrain FactsDavid Wang100% (1)
- Digestive System Grade 6Document1 pageDigestive System Grade 6Adrin MacarandanNo ratings yet
- Physiological Functions and Metabolism of Essential Dietary Element IodineDocument4 pagesPhysiological Functions and Metabolism of Essential Dietary Element IodinefitrizeliaNo ratings yet
- RRT in ElderlyDocument8 pagesRRT in ElderlySupandy HasanNo ratings yet
- Above Normal: (After A Meal)Document2 pagesAbove Normal: (After A Meal)Uzma AdnanNo ratings yet