Professional Documents
Culture Documents
Nej Mo A 1412082
Uploaded by
tom24Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nej Mo A 1412082
Uploaded by
tom24Copyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Nivolumab in Previously Untreated
Melanoma without BRAF Mutation
Caroline Robert, M.D., Ph.D., Georgina V. Long, M.D., Ph.D., Benjamin Brady, M.D.,
Caroline Dutriaux, M.D., Michele Maio, M.D., Laurent Mortier, M.D.,
Jessica C. Hassel, M.D., Piotr Rutkowski, M.D., Ph.D., Catriona McNeil, M.D., Ph.D.,
Ewa Kalinka-Warzocha, M.D., Ph.D., Kerry J. Savage, M.D.,
Micaela M. Hernberg, M.D., Ph.D., Celeste Lebb, M.D., Ph.D.,
Julie Charles, M.D., Ph.D., Catalin Mihalcioiu, M.D., Vanna Chiarion-Sileni, M.D.,
Cornelia Mauch, M.D., Ph.D., Francesco Cognetti, M.D., Ana Arance, M.D., Ph.D.,
Henrik Schmidt, M.D., D.M.Sc., Dirk Schadendorf, M.D., Helen Gogas, M.D.,
Lotta Lundgren-Eriksson, M.D., Christine Horak, Ph.D., Brian Sharkey, Ph.D.,
Ian M. Waxman, M.D., Victoria Atkinson, M.D., and Paolo A. Ascierto, M.D.
A BS T R AC T
BACKGROUND
The authors affiliations are listed in the Nivolumab was associated with higher rates of objective response than chemo-
Appendix. Address reprint requests to Dr. therapy in a phase 3 study involving patients with ipilimumab-refractory metastatic
Robert at Dermatology Service, INSERM
Unit 981, Gustave Roussy, VillejuifParis melanoma. The use of nivolumab in previously untreated patients with advanced
Sud, France, or at caroline.robert@ melanoma has not been tested in a phase 3 controlled study.
gustaveroussy.fr.
METHODS
Drs. Atkinson and Ascierto contributed We randomly assigned 418 previously untreated patients who had metastatic melanoma
equally to this article.
without a BRAF mutation to receive nivolumab (at a dose of 3 mg per kilogram of body
This article was published on November 16, weight every 2 weeks and dacarbazine-matched placebo every 3 weeks) or dacarbazine
2014, at NEJM.org. (at a dose of 1000 mg per square meter of body-surface area every 3 weeks and nivolu
N Engl J Med 2015;372:320-30. mab-matched placebo every 2 weeks). The primary end point was overall survival.
DOI: 10.1056/NEJMoa1412082
Copyright 2014 Massachusetts Medical Society.
RESULTS
At 1 year, the overall rate of survival was 72.9% (95% confidence interval [CI], 65.5 to
78.9) in the nivolumab group, as compared with 42.1% (95% CI, 33.0 to 50.9) in the
dacarbazine group (hazard ratio for death, 0.42; 99.79% CI, 0.25 to 0.73; P<0.001).
The median progression-free survival was 5.1 months in the nivolumab group versus
2.2 months in the dacarbazine group (hazard ratio for death or progression of dis-
ease, 0.43; 95% CI, 0.34 to 0.56; P<0.001). The objective response rate was 40.0% (95%
CI, 33.3 to 47.0) in the nivolumab group versus 13.9% (95% CI, 9.5 to 19.4) in the
dacarbazine group (odds ratio, 4.06; P<0.001). The survival benefit with nivolumab
versus dacarbazine was observed across prespecified subgroups, including subgroups
defined by status regarding the programmed death ligand 1 (PD-L1). Common ad-
verse events associated with nivolumab included fatigue, pruritus, and nausea. Drug-
related adverse events of grade 3 or 4 occurred in 11.7% of the patients treated with
nivolumab and 17.6% of those treated with dacarbazine.
CONCLUSIONS
Nivolumab was associated with significant improvements in overall survival and
progression-free survival, as compared with dacarbazine, among previously un-
treated patients who had metastatic melanoma without a BRAF mutation. (Funded
by Bristol-Myers Squibb; CheckMate 066 ClinicalTrials.gov number, NCT01721772.)
320 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
T
he global incidence of melanoma has been approved in the United States on the
continues to rise, and the mortality associ- basis of an objective response rate of 24% among
ated with unresectable or metastatic mela- patients with advanced melanoma that progressed
noma remains high.1 Globally, 132,000 new cas- after ipilimumab, as well as treatment with a
es of melanoma are diagnosed and an estimated BRAF inhibitor if the patient had a BRAF V600
48,000 persons die from advanced melanoma mutation.18 Here, we report the results of a phase
each year.2,3 Ipilimumab has been shown to im- 3, randomized, double-blind study conducted to
prove the rate of survival at 2 years, as compared determine whether nivolumab, as compared with
with a vaccine control, among previously treated dacarbazine, improves overall survival among pre-
patients with metastatic melanoma as well as viously untreated patients who have advanced
among previously untreated patients who also melanoma without a BRAF mutation.
received dacarbazine.4,5 BRAF and MEK inhibi-
tors are approved agents that, as monotherapy, ME THODS
have been associated with a survival advantage as
compared with chemotherapy, with a median PATIENTS
overall survival of 13 to 20 months.6-8 Although Eligible patients had confirmed, unresectable,
the objective response rate is high with these previously untreated stage III or IV melanoma
agents (45 to 53%), the median duration of re- without a BRAF mutation. Other eligibility crite-
sponse is less than 1 year.6-10 ria included an age of 18 years or more, an East-
Recently, a combination of anti-BRAF and ern Cooperative Oncology Group (ECOG) perfor-
anti-MEK agents has been associated with a mance-status score of 0 or 1 (on a scale of 0 to 5,
higher response rate and longer duration of re- with 0 indicating no symptoms and 1 indicating
sponse, as compared with anti-BRAF mono- mild symptoms), and the availability of tumor
therapies.11,12 However, the use of these targeted tissue from a metastatic or unresectable site for
agents, as monotherapy or in combination, is PD-L1 biomarker analysis. Key exclusion criteria
limited to the approximately 40% of patients were active brain metastases, uveal melanoma,
who have melanoma with a BRAF V600 muta- and a history of serious autoimmune disease. Pa-
tion. Dacarbazine is associated with a median tients who had received adjuvant therapy previ-
overall survival of 5.6 to 7.8 months and re- ously were not excluded.
mained until recently a commonly used therapy
in patients with previously untreated melanoma STUDY DESIGN AND TREATMENT
without a BRAF mutation.5,13 Despite new treat- Patients were randomly assigned in a 1:1 ratio to
ment options, there remains a substantial unmet receive by means of intravenous infusion either
need for treatments that extend survival and 3 mg of nivolumab per kilogram of body weight
provide a better quality of life. every 2 weeks, plus a dacarbazine-matched pla-
Nivolumab is a fully human IgG4 pro- cebo every 3 weeks, or 1000 mg of dacarbazine
grammed death 1 (PD-1) immune-checkpoint per square meter of body-surface area every
inhibitor antibody that selectively blocks the in- 3weeks, plus a nivolumab-matched placebo ev-
teraction of the PD-1 receptor with its two ery 2 weeks. Randomization was stratified ac-
known programmed death ligands, PD-L1 and cording to tumor PD-L1 status (positive vs. nega-
PD-L2, disrupting the negative signal that regu- tive or indeterminate) and metastasis stage (M0,
lates T-cell activation and proliferation.14 In a M1a, or M1b vs. M1c, defined according to the
phase 1 study, nivolumab was associated with tumornodemetastasis system of the American
promising antitumor activity and a favorable safety Joint Committee on Cancer and the International
profile in patients with solid tumors, including Union against Cancer). Treatment continued
advanced melanoma.15,16 In an open-label, ran- until there was disease progression, as assessed
domized, phase 3 study involving patients with by the investigator, or an unacceptable level of
ipilimumab-refractory melanoma, nivolumab was toxic effects. Treatment after disease progres-
associated with a higher rate of objective re- sion was permitted for patients who had a clin-
sponse than chemotherapy (32% vs. 11%).17 Re- ical benefit and did not have substantial adverse
cently, another antiPD-1 antibody, pembroli- effects with the study drug, as determined by
zumab, has shown robust clinical activity and the investigator (Fig. S1 in the Supplementary
n engl j med 372;4nejm.orgjanuary 22, 2015 321
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Appendix, available with the full text of this ar- mittee recommended that the study be unblind-
ticle at NEJM.org). ed and amended to allow patients enrolled in the
The primary end point was overall survival. dacarbazine group to receive nivolumab. Re-
Secondary end points included investigator-as- ported here are the results from the double-blind
sessed progression-free survival, objective re- portion of the study before the amendment
sponse rate, and PD-L1 expression in the tumor (clinical data cutoff on June 24, 2014).
as a predictive biomarker of overall survival.
PD-L1 ASSESSMENT
ASSESSMENT Before randomization, the expression of PD-L1
Tumor response was assessed according to the on the surface of the tumor cells was assessed
Response Evaluation Criteria in Solid Tumors in a central laboratory with the use of an auto-
(RECIST), version 1.1,19 at 9 weeks after random- mated immunohistochemical assay (collabora-
ization, every 6 weeks thereafter for the first tively developed by Bristol-Myers Squibb and
year, and then every 12 weeks until disease pro- Dako), as described previously.21 PD-L1 positiv-
gression or treatment discontinuation. Assess- ity was defined as at least 5% of tumor cells
ments for survival were performed every 3 showing cell-surface PD-L1 staining of any inten-
months. Safety evaluations were performed for sity in a section containing at least 100 tumor
patients who received at least one dose of the cells that could be evaluated. Indeterminate sta-
study treatment, and the severity of adverse tus was attributed to samples for which tumor
events was graded according to the National cellsurface expression could not be discerned
Cancer Institute Common Terminology Criteria because of melanin content or strong cytoplas-
for Adverse Events, version 4.0.20 mic staining. PD-L1 status was prospectively
determined, and the results were used to strat-
STUDY OVERSIGHT ify randomization, which was performed by
The study protocol, available at NEJM.org with means of a fully automated interactive voice-
the most recent version of the statistical analysis response system. Statistical analyses were pre-
plan, was approved by the institutional review specified to assess the predictive value of PD-L1
board at each participating center. The study was expression.
conducted in accordance with the Declaration of
Helsinki and the International Conference on STATISTICAL ANALYSIS
Harmonisation Guidelines for Good Clinical A sample of approximately 410 patients, random-
Practice. All the patients provided written in- ly assigned in a 1:1 ratio to the two treatment
formed consent to participate in the study. Data groups, was planned. Overall survival and pro-
were collected by the sponsor, Bristol-Myers gression-free survival were compared between
Squibb, and analyzed in collaboration with the the two treatment groups with the use of a two-
academic authors. All the authors vouch for the sided log-rank test stratified according to PD-L1
accuracy and completeness of the data and analy- status (positive vs. negative or indeterminate)
ses reported and for the fidelity of the study to and metastasis stage (M0, M1a, or M1b vs. M1c).
the protocol. The first draft of the manuscript The hazard ratios for the nivolumab group, as
was written by the first and last authors, with all compared with the dacarbazine group, and cor-
the authors contributing to subsequent drafts. responding confidence intervals were estimated
Medical-writing support, funded by the sponsor, with the use of a stratified Cox proportional-
was provided by StemScientific. hazards model. Survival curves for each treat-
A data and safety monitoring committee was ment group were estimated with the use of
established to provide oversight of safety and theKaplanMeier product-limit method. Rates
efficacy considerations. On June 10, 2014, the at fixed time points were derived from the
monitoring committee reviewed an expedited KaplanMeier estimate, along with their corre-
report after noting a potential difference in over- sponding log-logtransformed 95% confidence
all survival during an earlier safety review. Data interval.
from the abbreviated report, which was based on The objective response rate was compared
an unplanned interim database lock, showed a between the two treatment groups with the use
significant difference in overall survival in favor of a two-sided CochranMantelHaenszel test.
of nivolumab. As a result, the monitoring com- The efficacy analyses were performed in the
322 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
population of patients who underwent random- EFFICACY
ization (the intention-to-treat population). The The median overall survival was not reached in
safety analyses were performed in the popula- the nivolumab group and was 10.8 months (95%
tion of patients who received at least one dose of confidence interval [CI], 9.3 to 12.1) in the dacar-
a study drug. At the time of data analysis, 146 bazine group. The overall survival rate at 1 year
patients had died. The boundary for statistical was 72.9% (95% CI, 65.5 to 78.9) in the nivolu
significance, which was based on the Lan mab group and 42.1% (95% CI, 33.0 to 50.9) in
DeMets alpha-spending function with OBrien the dacarbazine group. A significant benefit with
and Flemingtype boundaries, required the log- respect to overall survival was observed in the
rank P value to be less than 0.0021, correspond- nivolumab group, as compared with the dacarba-
ing to a 99.79% confidence interval. zine group (hazard ratio for death, 0.42; 99.79%
CI, 0.25 to 0.73; P<0.001) (Fig. 1A).
R E SULT S The median progression-free survival was 5.1
months (95% CI, 3.5 to 10.8) in the nivolumab
group and 2.2 months (95% CI, 2.1 to 2.4) in the
PATIENTS AND TREATMENT dacarbazine group (Fig. 1B). A significant ben-
From January 2013 through February 2014, a to- efit with respect to progression-free survival was
tal of 518 patients were enrolled at 80 centers in observed in the nivolumab group, as compared
Europe, Israel, Australia, Canada, and South with the dacarbazine group (hazard ratio for
America. A total of 418 patients underwent ran- death or progression of disease, 0.43; 95% CI,
domization: 210 patients were assigned to the 0.34 to 0.56; P<0.001).
nivolumab group and 208 to the dacarbazine The objective response rate in the nivolumab
group (Fig. S1 in the Supplementary Appendix). group was 40.0% (95% CI, 33.3 to 47.0), which
One patient randomly assigned to the nivolumab was significantly higher than the rate in the
group and 3 randomly assigned to the dacarba- dacarbazine group, which was 13.9% (95% CI,
zine group were inadvertently enrolled in the 9.5 to 19.4) (odds ratio, 4.06; P<0.001). The per-
study, despite having an ECOG performance-sta- centage of patients with a complete response
tus score of 2; 1 additional patient in the nivolu was higher with nivolumab than with dacarba-
mab group did not report an ECOG performance- zine (7.6% vs. 1.0%) (Fig. 2 and Table 2). Among
status score. Baseline characteristics were patients who had a response, the median dura-
balanced between the two groups. A total of tion of response was not reached in the nivolu
61.0% of patients had stage M1c disease, 36.6% mab group and was 6.0 months in the dacarba-
had an elevated lactate dehydrogenase level, and zine group (95% CI, 3.0 to not reached) (Fig. 2C).
35.4% had a positive PD-L1 status (Table 1). In the nivolumab group, a reduction of 30%
At the time of the database lock, 95 of 206 pa- or more in the tumor burden in the target lesion,
tients (46.1%) treated with nivolumab and 13 of representing an unconventional response pat-
205 (6.3%) treated with dacarbazine were continu- tern sometimes seen with immunotherapies,
ing the study treatment. The most frequent reason was achieved or maintained in 17 of 54 patients
for discontinuation was disease progression, in 96 who were treated beyond progression (8.1% of
of 206 patients (46.6%) in the nivolumab group patients randomly assigned to nivolumab) (Fig.
and 175 of 205 (85.4%) in the dacarbazine group S4A in the Supplementary Appendix). In the da-
(Table S1 in the Supplementary Appendix). After carbazine group, this unconventional response
the discontinuation of study treatment, 63 of 210 was achieved or maintained in 8 of the 49 pa-
patients (30.0%) in the nivolumab group and 114 tients who were treated beyond progression
of 208 (54.8%) in the dacarbazine group received (3.8% of patients randomly assigned to dacarba-
systemic therapy, most commonly ipilimumab (in zine) (Fig. S4B in the Supplementary Appendix).
45 of 63 patients and 79 of 114, respectively) (Table
S2 in the Supplementary Appendix). All the pa- SUBGROUP ANALYSES
tients who underwent randomization were fol- Regardless of PD-L1 status, nivolumab-treated
lowed for up to 16.7 months at the time of data- patients had improved overall survival, as com-
base lock on August 5, 2014, which was 5.2 pared with dacarbazine-treated patients (unad-
months after the first visit of the last patient who justed hazard ratio for death among patients
had undergone randomization. with positive PD-L1 status, 0.30 [95% CI, 0.15 to
n engl j med 372;4nejm.orgjanuary 22, 2015 323
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
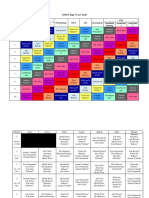
Table 1. Baseline Characteristics of the Patients.*
Nivolumab Dacarbazine Total
Characteristic (N=210) (N=208) (N=418)
Age yr
Median 64 66 65
Range 1886 2687 1887
Sex no. (%)
Male 121 (57.6) 125 (60.1) 246 (58.9)
Female 89 (42.4) 83 (39.9) 172 (41.1)
Geographic region no. (%)
Europe or Canada 145 (69.0) 145 (69.7) 290 (69.4)
Israel, Australia, or South America 65 (31.0) 63 (30.3) 128 (30.6)
ECOG performance-status score
no. (%)
0 148 (70.5) 121 (58.2) 269 (64.4)
1 60 (28.6) 84 (40.4) 144 (34.4)
2 1 (0.5) 3 (1.4) 4 (1.0)
Metastasis stage no. (%)
M1c 128 (61.0) 127 (61.1) 255 (61.0)
M0, M1a, or M1b 82 (39.0) 81 (38.9) 163 (39.0)
Lactate dehydrogenase no. (%)
ULN 120 (57.1) 125 (60.1) 245 (58.6)
>ULN 79 (37.6) 74 (35.6) 153 (36.6)
2 ULN 178 (84.8) 177 (85.1) 355 (84.9)
>2 ULN 21 (10.0) 22 (10.6) 43 (10.3)
Not reported 11 (5.2) 9 (4.3) 20 (4.8)
History of brain metastases no. (%)
Yes 7 (3.3) 8 (3.8) 15 (3.6)
No 203 (96.7) 200 (96.2) 403 (96.4)
PD-L1 status no. (%)
Positive 74 (35.2) 74 (35.6) 148 (35.4)
Negative or indeterminate 136 (64.8) 134 (64.4) 270 (64.6)
BRAF status no. (%)
Mutation 0 0 0
No mutation 202 (96.2) 204 (98.1) 406 (97.1)
Not reported 8 (3.8) 4 (1.9) 12 (2.9)
Prior systemic therapy no. (%)
Adjuvant therapy 32 (15.2) 36 (17.3) 68 (16.3)
Neoadjuvant therapy 1 (0.5) 1 (0.5) 2 (0.5)
* There were no significant between-group differences in the baseline characteristics. ULN denotes upper limit of the
normal range.
An Eastern Cooperative Oncology Group (ECOG) performance-status score of 0 indicates no symptoms, 1 mild symp-
toms, and 2 moderate symptoms, with the patient being ambulatory and capable of all self-care but unable to carry out
any work activities. One patient randomly assigned to the nivolumab group and three randomly assigned to the dacar-
bazine group were inadvertently enrolled in the study, despite having an ECOG performance-status score of 2. One ad-
ditional patient in the nivolumab group underwent randomization in error without having an ECOG performance-status
report.
The metastasis stage was defined according to the tumornodemetastasis system of the American Joint Committee
on Cancer and the International Union against Cancer.
A positive status for programmed death ligand 1 (PD-L1) was defined as at least 5% of the tumor cells having cell-sur-
face PD-L1 staining of any intensity in a section containing at least 100 tumor cells that could be evaluated. Indetermi-
nate status was attributed to samples for which tumor cell-surface expression could not be discerned because of mela-
nin content or strong cytoplasmic staining.
324 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
0.60]; unadjusted hazard ratio for death among
A Overall Survival
those with PD-L1 negative or indeterminate PD-
100 Hazard ratio for death, 0.42 (99.79% CI, 0.250.73)
L1 status, 0.48 [95% CI, 0.32 to 0.71]) (Fig. S2 in P<0.001
90
the Supplementary Appendix). In the nivolumab
80
group, the median overall survival was not Nivolumab
Patients Surviving (%)
70
reached in either PD-L1 subgroup. In the dacar- Dacarbazine
bazine group, the median overall survival was 60
slightly longer in the subgroup with positive PD- 50
L1 status than in the subgroup with negative or 40
indeterminate PD-L1 status (12.4 vs. 10.2 months) 30
Patients Who Died Median Survival
(Fig. S3 in the Supplementary Appendix). 20 no./total no. mo (95% CI)
In the two PD-L1 subgroups, nivolumab- 10 Nivolumab 50/210 Not reached
Dacarbazine 96/208 10.8 (9.312.1)
treated patients had improved rates of objective 0
response, as compared with dacarbazine-treated 0 3 6 9 12 15 18
patients. In the subgroup with positive PD-L1 Months
status, the objective response rate was 52.7% No. at Risk
Nivolumab 210 185 150 105 45 8 0
(95% CI, 40.8 to 64.3) in the nivolumab group Dacarbazine 208 177 123 82 22 3 0
versus 10.8% (95% CI, 4.8 to 20.2) in the dacar-
bazine group. In the subgroup with negative or B Progression-free Survival
indeterminate PD-L1 status, the objective re- Patients Who Died Median
100 or Had Disease Progression-free
sponse rate was 33.1% (95% CI, 25.2 to 41.7) in Progression Survival
the nivolumab group versus 15.7% (95% CI, 10.0 90 no./total no. mo (95% CI)
to 23.0) in the dacarbazine group. The survival Nivolumab 108/210 5.1 (3.510.8)
Patients without Progression (%)
80
Dacarbazine 163/208 2.2 (2.12.4)
benefit with nivolumab versus dacarbazine was
70
also observed across prespecified subgroups
based on age, sex, metastasis stage, ECOG per- 60 Nivolumab
formance-status score, status with respect to a 50
history of brain metastases, baseline lactate de-
40
hydrogenase level, and geographic region (Fig. Hazard ratio for death or disease
S2 in the Supplementary Appendix). 30 progression, 0.43 (95% CI, 0.340.56); P<0.001
Dacarbazine
20
ADVERSE EVENTS
10
The incidence of treatment-related adverse events
of any grade was similar in the nivolumab group 0
0 3 6 9 12 15 18
and the dacarbazine group (74.3% and 75.6%,
Months
respectively). However, treatment-related adverse
No. at Risk
events of grade 3 or 4 were reported less fre- Nivolumab 210 116 82 57 12 1 0
quently in the nivolumab group than in the da- Dacarbazine 208 74 28 12 0 0 0
carbazine group (11.7% vs. 17.6%) (Table 3, and Figure 1. Survival End Points.
Table S3 in the Supplementary Appendix). The Panel A shows the KaplanMeier curves for overall survival. The median
most common adverse events related to nivolu follow-up for overall survival was 8.9 months in the nivolumab group and
mab treatment were fatigue (in 19.9% of pa- 6.8 months in the dacarbazine group. Panel B shows the KaplanMeier
tients), pruritus (in 17.0%), and nausea (in curves for progression-free survival.
16.5%). In the dacarbazine group, common treat-
ment-related adverse events were consistent with
those in previous reports and included gastroin- ing to adverse events was 6.8% in the nivolumab
testinal and hematologic toxic events. The fre- group and 11.7% in the dacarbazine group. No
quency of treatment-related serious adverse deaths were attributed to study-drug toxicity in
events of grade 3 or 4 was similar in the two either group.
groups (5.8% in the nivolumab group and 5.9% Selected adverse events defined as those
in the dacarbazine group). The percentage of pa- with a potential immunologic cause were
tients who discontinued the study treatment ow- analyzed according to organ category. Grade 3
n engl j med 372;4nejm.orgjanuary 22, 2015 325
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A Target-Lesion Change in Nivolumab Group Figure 2. Characteristics of Response.
100 The waterfall plots show the maximum change from
baseline in the sum of the reference diameters of the
75 target lesion in patients receiving nivolumab (Panel A)
Maximum Change from Baseline (%)
and those receiving dacarbazine (Panel B). Data are
50 shown for all the patients who had a response that
could be evaluated in the target lesion at baseline and
25 who underwent at least one tumor assessment during
treatment. The percentage increase was truncated at
0 100% (red squares). Red dots indicate patients who
had a response to treatment according to the Response
25 Evaluation Criteria in Solid Tumors, version 1.1. The
dashed lines in Panels A and B indicate a 30% reduc-
50 tion in the tumor burden in the target lesion. Kaplan
Meier curves for the duration of response (Panel C)
75 show that the median duration of response in the 84
patients in the nivolumab group who had a response
100 was not reached; 12 of these patients did not have a
Patients durable response. Of the 29 patients in the dacarba-
zine group who had a response, 14 did not have a du-
B Target-Lesion Change in Dacarbazine Group rable response. The dashed line in Panel C indicates
100 the median duration of response.
75
Maximum Change from Baseline (%)
or 4 selected adverse events that were considered
50
to be related to nivolumab treatment were infre-
25 quent and included diarrhea and an elevated ala-
nine aminotransferase level (each in 1.0% of
0 patients) (Table S4 in the Supplementary Appen-
dix). The majority of selected adverse events of
25
grade 3 or 4 resolved quickly with a delay in the
50 study treatment, glucocorticoid administration,
or both, as recommended in the safety manage-
75 ment guidelines for nivolumab (Table S5 in the
Supplementary Appendix).
100
Patients
DISCUSSION
C Duration of Response
100 This phase 3, double-blind, randomized, con-
90 trolled study showed an overall survival benefit
Patients with Complete or Partial
Nivolumab
80 with nivolumab, an antiPD-1 antibody. The risk
70 of death decreased by 58% with nivolumab, as
Response (%)
Dacarbazine
60 compared with dacarbazine, among previously
50 untreated patients with advanced melanoma.
40 The survival benefit was consistent across all the
30 prespecified subgroups, including patients with
Patients without a Median Duration
20 Durable Response of Response poor prognostic factors.
10 no./total no. mo (95% CI) The 1-year survival rate associated with
0
Nivolumab 12/84 Not reached nivolumab in this study (73%) is consistent with
Dacarbazine 14/29 6.0 (3.0not reached)
the results in a phase 1 study15,16,22 and was
0 3 6 9 12 15
significantly higher than the rate associated
Months
with dacarbazine. Dacarbazine was chosen as
No. at Risk
Nivolumab 84 65 50 23 1 0
the comparator because, until recently, it was a
Dacarbazine 29 19 6 1 0 0 standard first-line treatment in many countries
for patients who had melanoma without a BRAF
326 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
Table 2. Response to Treatment.*
Nivolumab Dacarbazine
Response (N=210) (N=208)
Best overall response no. (%)
Complete response 16 (7.6) 2 (1.0)
Partial response 68 (32.4) 27 (13.0)
Stable disease 35 (16.7) 46 (22.1)
Progressive disease 69 (32.9) 101 (48.6)
Could not be determined 22 (10.5) 32 (15.4)
Objective response
No. of patients (% [95% CI]) 84 (40.0 [33.347.0]) 29 (13.9 [9.519.4])
Difference percentage points 26.1 (18.034.1)
(95% CI)
Estimated odds ratio (95% CI) 4.06 (2.526.54)
P value <0.001
Time to objective response mo
Median 2.1 2.1
Range 1.27.6 1.83.6
Mean 2.61.3 2.50.7
Duration of response mo
Median (95% CI) Not reached 6.0 (3.0not reached)
Range 0.012.5 1.110.0
* Plusminus values are means SD.
The best overall response was assessed by the investigator with the use of the Response Evaluation Criteria in Solid
Tumors, version 1.1.19
Data include patients with a complete response and those with a partial response. The calculation of the confidence in-
terval was based on the ClopperPearson method. The estimate of the difference (the rate in the nivolumab group minus
the rate in the dacarbazine group) was based on the CochranMantelHaenszel method of weighting, with adjustment
for PD-L1 status and metastasis stage as entered into the interactive voice-response system. The odds ratio and two-
sided P value for an objective response with nivolumab as compared with dacarbazine were calculated with the use of
a CochranMantelHaenszel test stratified according to PD-L1 status and metastasis stage.
The median was calculated with the use of the KaplanMeier method. Data were censored for the range values because
the observations are ongoing. The cutoff date for clinical data was August 5, 2014, with a range of follow-up from 5.2 to
16.7 months.
mutation. In this group of patients, only ipilim- uating both nivolumab monotherapy and combi-
umab in combination with dacarbazine has been nation therapy with nivolumab plus ipilimumab,
associated with a survival benefit, as compared as compared with ipilimumab alone, in previ-
with dacarbazine alone, in a phase 3, controlled ously untreated patients with melanoma is cur-
trial.5 When the present study was planned in rently under way. The activity of ipilimumab is
2012, ipilimumab had not been approved for use probably reflected in the performance of the
as a first-line treatment for advanced melanoma dacarbazine group in the present study. The me-
in most regions outside the United States. How- dian survival in the dacarbazine group (10.8
ever, during the course of this study, it was ap- months) in this study is higher than that previ-
proved for first-line therapy in most regions. ously reported,5 possibly because 38% of the
Nevertheless, dacarbazine is still used as a first- dacarbazine-treated patients received ipilimum-
line therapy for metastatic melanoma in many ab after stopping the study treatment.
countries. The objective response rate (40%) and dura-
An additional phase 3 study (CheckMate 067; tion of response associated with nivolumab that
ClinicalTrials.gov number, NCT01844505), eval- were observed in this study are in line with
n engl j med 372;4nejm.orgjanuary 22, 2015 327
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 3. Adverse Events.*
Nivolumab Dacarbazine
Event (N=206) (N=205)
Any Grade Grade 3 or 4 Any Grade Grade 3 or 4
no. of patients with event (%)
Any adverse event 192 (93.2) 70 (34.0) 194 (94.6) 78 (38.0)
Treatment-related adverse event 153 (74.3) 24 (11.7) 155 (75.6) 36 (17.6)
Fatigue 41 (19.9) 0 30 (14.6) 2 (1.0)
Pruritus 35 (17.0) 1 (0.5) 11 (5.4) 0
Nausea 34 (16.5) 0 85 (41.5) 0
Diarrhea 33 (16.0) 2 (1.0) 32 (15.6) 1 (0.5)
Rash 31 (15.0) 1 (0.5) 6 (2.9) 0
Vitiligo 22 (10.7) 0 1 (0.5) 0
Constipation 22 (10.7) 0 25 (12.2) 0
Asthenia 21 (10.2) 0 25 (12.2) 1 (0.5)
Vomiting 13 (6.3) 1 (0.5) 43 (21.0) 1 (0.5)
Neutropenia 0 0 23 (11.2) 9 (4.4)
Thrombocytopenia 0 0 21 (10.2) 10 (4.9)
Adverse event leading to discontinuation 14 (6.8) 12 (5.8) 24 (11.7) 19 (9.3)
of treatment
Serious adverse event
Any event 64 (31.1) 43 (20.9) 78 (38.0) 54 (26.3)
Treatment-related event 19 (9.2) 12 (5.8) 18 (8.8) 12 (5.9)
* The severity of adverse events was graded according to the National Cancer Institute Common Terminology Criteria for
Adverse Events, version 4.0.20
The treatment-related adverse events listed here were reported in at least 10% of the patients in either study group.
those in previous reports.15-17,22 It has generally tion regimens in patients with a BRAF V600
been accepted that immunotherapy is associated mutation11,12; however, for patients who have
with long-term responses in a subset of patients, melanoma without a BRAF mutation, treatment
whereas targeted therapies, such as BRAF in- options beyond ipilimumab are limited. Al-
hibitors, are associated with high response rates though the target population of our study was
and a rapid effect, but the responses are often restricted to patients with melanoma who did
short-lived.4-7,9,10,23 The present study shows that not have a BRAF mutation, previous studies have
nivolumab is associated with a high response shown that nivolumab had similar clinical activ-
rate, a rapid median time to response (2.1 ity regardless of the patients BRAF mutation
months, which is similar to the time to response status.17,24
for dacarbazine), and a durable response (the Previous studies, which have used various
median duration of response was not reached, methodologic approaches, have shown a correla-
but the duration of follow-up was short). These tion between PD-L1 expression and objective
results are in agreement with the long-term fol- response in patients with metastatic melanoma
low-up data from a phase 1 study of nivolumab, treated with antiPD-1 or antiPD-L1 antibod-
which showed a median duration of response of ies.21,22,24-28 In our study, given the magnitude of
almost 2 years and an objective response rate of the clinical benefit observed in patients receiv-
32% among patients with advanced melanoma.22 ing nivolumab versus those receiving dacarba-
The response rate with a BRAF or MEK in- zine, PD-L1 status alone, as assessed with the
hibitor was recently surpassed by new combina- use of the methods presented here, does not
328 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
seem to be useful in the selection of patients for In conclusion, nivolumab was associated with
nivolumab treatment. Also, because there was a significant improvement in overall survival and
little difference in median overall survival be- progression-free survival, as compared with da-
tween the two subgroups of dacarbazine-treated carbazine. Nivolumab was associated with a low
patients defined according to PD-L1 status (pos- risk of high-grade toxic effects.
itive vs. negative or indeterminate), the prognos-
Supported by Bristol-Myers Squibb.
tic role of PD-L1 status remains to be deter- Disclosure forms provided by the authors are available with
mined. the full text of this article at NEJM.org.
The safety profile of nivolumab in this study We thank the patients who volunteered to participate in this
study and the staff members at the study sites who cared for
was similar to that observed previously.15-17,22 The them; the members of the data and safety monitoring commit-
frequency of selected adverse events with a poten- tee; representatives of the sponsors who were involved in data
tial immunologic cause was similar to the fre- collection and analyses (particularly Arvin Yang, M.D., Ph.D.,
Susan Parker, Ph.D., and Diana Birle, M.D.); and Wayne Peng,
quency observed in a previous phase 3 trial,17 and Ph.D., and Karin McGlynn, B.A., of StemScientific for editorial
the events resolved in the majority of our patients. and writing assistance with an earlier version of the manuscript.
APPENDIX
The authors affiliations are as follows: Gustave Roussy and INSERM Unit 981, VillejuifParis Sud (C.R.), Hpital Saint Andr Centre
Hospitalier Universitaire, Bordeaux (C.D.), Hpital Claude Huriez, Lille (L.M.), Assistance PubliqueHpitaux de Paris Dermatology and
Centre dInvestigation Clinique Hpital Saint Louis Paris 7 University, INSERM Unit 976, Paris (C.L.), and Grenoble University Hospi-
tal, INSERM Unit 823, Joseph Fourier University, Grenoble (J.C.) all in France; Melanoma Institute Australia, University of Sydney,
and Mater Hospital, Sydney (G.V.L.), Cabrini Health, Melbourne, VIC (B.B.), Chris OBrien Lifehouse, Melanoma Institute Australia and
Royal Prince Alfred Hospital, Camperdown, NSW (C. McNeil), Princess Alexandra Hospital, Woolloongabba, and Gallipoli Medical
Research Foundation, Greenslopes Private Hospital, Greenslopes, QLD (V.A.) all in Australia; University Hospital of Siena, Siena
(M.M.), Oncology Institute of Veneto Istituto di Ricovero e Cura a Carattere Scientifico, Padua (V.C.-S.), Division Oncology, Regina
Elena Institute, Rome (F.C.), and Istituto Nazionale Tumori Fondazione Pascale, Naples (P.A.A.) all in Italy; University Hospital
Heidelberg and National Center for Tumor Diseases, Heidelberg (J.C.H.), Department of Dermatology, University Hospital Cologne and
Centrum fr Integrierte Onkologie Kln, Bonn (C. Mauch), and Department of Dermatology, University of Essen, Essen (D.S.) all in
Germany; Maria Sklodowska-Curie Memorial Cancer Center and Institute of Oncology, Warsaw (P.R.), and Wojewdzki Szpital Spec-
jalistyczny im. M. Kopernika, Lodz (E.K.-W.) both in Poland; British Columbia Cancer Agency, Vancouver (K.J.S.), and Royal Victo-
ria Hospital, Montreal (C. Mihalcioiu) both in Canada; Department of Oncology, Helsinki University Central Hospital, Helsinki
(M.M.H.); Hospital Clnic Barcelona, Barcelona (A.A.); Department of Oncology, Aarhus University Hospital, Aarhus, Denmark (H.S.);
University of Athens Medical School, Laiko General Hospital, Athens (H.G.); Department of Clinical Sciences, Division of Oncology,
Lund University, Lund, Sweden (L.L-E.); Bristol-Myers Squibb, Lawrenceville, NJ (C.H., I.M.W.); and Bristol-Myers Squibb, Wallingford,
CT (B.S.).
REFERENCES
1. American Cancer Society. Melanoma C, et al. Safety and efficacy of vemu- melanoma. N Engl J Med 2014;371:1877-
skin cancer (http://www.cancer.org/acs/ rafenib in BRAFV600E and BRAFV600K 88.
groups/cid/documents/ mutation-positive melanoma (BRIM-3): 13. Espinosa E, Grob JJ, Dummer R, et al.
webcontent/003120-pdf.pdf). extended follow-up of a phase 3, ran- Treatment algorithms in stage IV mela-
2. World Health Organization. Ultravio- domised, open-label study. Lancet Oncol noma. Am J Ther 2014 January 9 (Epub
let radiation and the INTERSUN Pro- 2014;15:323-32. ahead of print).
gramme; skin cancers (http://www.who 8. Flaherty KT, Robert C, Hersey P, et al. 14. Wang C, Thudium KB, Han M, et al.
.int/uv/faq/skincancer/en/index1.html). Improved survival with MEK inhibition in In vitro characterization of the anti-PD-1
3. American Cancer Society. Cancer BRAF-mutated melanoma. N Engl J Med antibody nivolumab, BMS-936558, and in
facts and figures 2014 (http://www 2012;367:107-14. vivo toxicology in non-human primates.
.cancer.org/acs/groups/content/@research/ 9. Hauschild A, Grob JJ, Demidov LV, et Cancer Immunol Res 2014;2:846-56.
documents/webcontent/acspc-042151.pdf). al. Dabrafenib in BRAF-mutated meta- 15. Topalian SL, Hodi FS, Brahmer JR, et
4. Hodi FS, ODay SJ, McDermott DF, et static melanoma: a multicentre, open- al. Safety, activity, and immune correlates
al. Improved survival with ipilimumab in label, phase 3 randomised controlled tri- of antiPD-1 antibody in cancer. N Engl J
patients with metastatic melanoma. al. Lancet 2012;380:358-65. Med 2012;366:2443-54.
N Engl J Med 2010;363:711-23. [Erratum, 10. Sosman JA, Kim KB, Schuchter L, et 16. Topalian SL, Sznol M, McDermott DF,
N Engl J Med 2010;363:1290.] al. Survival in BRAF V600-mutant ad- et al. Survival, durable tumor remission,
5. Robert C, Thomas L, Bondarenko I, et vanced melanoma treated with vemu- and long-term safety in patients with ad-
al. Ipilimumab plus dacarbazine for pre- rafenib. N Engl J Med 2012;366:707-14. vanced melanoma receiving nivolumab.
viously untreated metastatic melanoma. 11. Larkin J, Ascierto PA, Dreno B, et al. J Clin Oncol 2014;32:1020-30.
N Engl J Med 2011;364:2517-26. Combined vemurafenib and combimetinib 17. Weber JS, Minor D, DAngelo SP, et al.
6. Chapman PB, Hauschild A, Robert C, in BRAF-mutated melanoma. N Engl J Med A phase 3 randomized, open-label study
et al. Improved survival with vemurafenib 2014;371:1867-76. of nivolumab (anti-PD-1; BMS-936558;
in melanoma with BRAF V600E mutation. 12. Long GV, Stroyakovskiy D, Gogas H, ONO-4538) versus investigators choice
N Engl J Med 2011;364:2507-16. et al. Combined BRAF and MEK inhibi- chemotherapy (ICC) in patients with ad-
7. McArthur GA, Chapman PB, Robert tion versus BRAF inhibition along in vanced melanoma with prior anti-CTLA-4
n engl j med 372;4nejm.orgjanuary 22, 2015 329
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
Nivolumab in Untreated Melanoma without BR AF Mutation
therapy. Presented at the European Soci- al. Long-term survival of ipilimumab- (pts) with melanoma (MEL). J Clin Oncol
ety for Medical Oncology 2014 Congress, naive patients (pts) with advanced mela- 2014;32:Suppl:5s. abstract.
Madrid, September 2630, 2014. abstract. noma (MEL) treated with nivolumab 26. Hamid O, Sosman JA, Lawrence DP, et
18. Keytruda (pembrolizumab) prescrib- (anti-PD-1; BMS-936558, ONO-4538) in a al. Clinical activity, safety, and biomark-
ing information. Whitehouse Station, NJ: phase 1 trial. Presented at the European ers of MPDL3280A, an engineered PD-L1
Merck (http://www.merck.com/product/usa/ Society for Medical Oncology 2014 Con- antibody in patients with locally advanced
pi_circulars/k/keytruda/keytruda_pi.pdf). gress, Madrid, September 2630, 2014 or metastatic melanoma (mM). J Clin On-
19. Eisenhauer EA, Therasse P, Bogaerts J, (poster). col 2013;31:Suppl:9010. abstract.
et al. New response evaluation criteria in 23. Ribas A. Combination therapies 27. Grosso J, Horak CE, Inzunza D, et al.
solid tumours: revised RECIST guideline building on the efficacy of CTLA4 and Association of tumor PD-L1 expression
(version 1.1). Eur J Cancer 2009;45:228-47. BRAF inhibitors for metastatic melano- and immune biomarkers with clinical ac-
20. NCI Common Terminology Criteria ma. Am Soc Clin Oncol Educ Book tivity in patients (pts) with advanced solid
for Adverse Events (CTCAE) v.4 data files. 2012:675-8. tumors treated with nivolumab (anti-
Bethesda, MD: National Cancer Institute 24. Weber JS, Kudchadkar RR, Yu B, et al. PD-1; BMS-936558; ONO-4538). J Clin On-
(http://evs.nci.nih.gov/ftp1/CTCAE/About Safety, efficacy, and biomarkers of col 2013;31:Suppl:3016. abstract.
.html). nivolumab with vaccine in ipilimumab- 28. Weber JS, Kudchadkar RR, Gibney
21. Wolchok JD, Kluger H, Callahan MK, refractory or -naive melanoma. J Clin On- GT, et al. Phase I/II trial of PD-1 antibody
et al. Nivolumab plus ipilimumab in ad- col 2013;31:4311-8. nivolumab with peptide vaccine in pa-
vanced melanoma. N Engl J Med 2013; 25. Ribas A, Hodi SF, Kefford R, et al. Ef- tients naive to or that failed ipilimumab.
369:122-33. ficacy and safety of the anti-PD-1 mono- J Clin Oncol 2013;31:Suppl:9011. abstract.
22. McDermott DF, Kluger H, Sznol M, et clonal antibody MK-3475 in 411 patients Copyright 2014 Massachusetts Medical Society.
330 n engl j med 372;4nejm.orgjanuary 22, 2015
The New England Journal of Medicine
Downloaded from nejm.org on November 1, 2017. For personal use only. No other uses without permission.
Copyright 2015 Massachusetts Medical Society. All rights reserved.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- 2010 Rapid Review of Radiology (2010) (True PDF) (4.5-Star) PDFDocument353 pages2010 Rapid Review of Radiology (2010) (True PDF) (4.5-Star) PDFtom24100% (2)
- MicroRNA in CancerDocument148 pagesMicroRNA in CancerDevvvNo ratings yet
- Weight-For-Height BOYS: 2 To 5 Years (Z-Scores)Document1 pageWeight-For-Height BOYS: 2 To 5 Years (Z-Scores)Malisa Lukman100% (1)
- Master Techniques in Orthopaedic Surgery - Orthopaedic Oncology and Complex Reconstruction (PDFDrive) PDFDocument424 pagesMaster Techniques in Orthopaedic Surgery - Orthopaedic Oncology and Complex Reconstruction (PDFDrive) PDFsandeep nemaNo ratings yet
- Atlas of PET-CT Imaging in Oncology - A Case-Based Guide To Image Interpretation (PDFDrive)Document479 pagesAtlas of PET-CT Imaging in Oncology - A Case-Based Guide To Image Interpretation (PDFDrive)WilverCarbonelLuyo100% (2)
- Dr. Rosi - CPAPDocument65 pagesDr. Rosi - CPAPtom24No ratings yet
- Pancreatic PDFDocument11 pagesPancreatic PDFneela kantaNo ratings yet
- Anti Epileptic Drugs Effect On GrowthDocument17 pagesAnti Epileptic Drugs Effect On Growthtom24No ratings yet
- Nej Mo A 1503093Document12 pagesNej Mo A 1503093tom24No ratings yet
- Cover Jurnal ReadingDocument1 pageCover Jurnal Readingtom24No ratings yet
- Nej Mo A 1314768Document10 pagesNej Mo A 1314768tom24No ratings yet
- Nej Mo A 1610020Document14 pagesNej Mo A 1610020Nurul Khairiyah AmriNo ratings yet
- Weight Gain and Height Growth During Infancy, Childhood, and Adolescence As Predictors of Adult Cardiovascular RiskDocument12 pagesWeight Gain and Height Growth During Infancy, Childhood, and Adolescence As Predictors of Adult Cardiovascular Risktom24No ratings yet
- Jadwal Jaga Co Ass AnakDocument5 pagesJadwal Jaga Co Ass Anaktom24No ratings yet
- Balloon Tamponade in The Management ofDocument7 pagesBalloon Tamponade in The Management oftom24No ratings yet
- Congenital and Acquired Bone Marrow Failure: 1st EditionDocument9 pagesCongenital and Acquired Bone Marrow Failure: 1st EditiontotoirsyadNo ratings yet
- Stase Anak Periode 28 NovemberDocument2 pagesStase Anak Periode 28 Novembertom24No ratings yet
- Dr. Sudung - Tata Laksana Krisis HipertensiDocument30 pagesDr. Sudung - Tata Laksana Krisis Hipertensitom24No ratings yet
- Kementerian Kesehatan Republik Indonesia Jilid 2Document1 pageKementerian Kesehatan Republik Indonesia Jilid 2tom24No ratings yet
- Jurnal FixDocument12 pagesJurnal FixYogi Ardhi IrafaniNo ratings yet
- Modul 2Document54 pagesModul 2tom24No ratings yet
- Modul 1Document40 pagesModul 1tom24No ratings yet
- NeuroblastomaDocument30 pagesNeuroblastomaFaisal MoidunnyNo ratings yet
- Imaging - Lecture 6 (Mammography I)Document8 pagesImaging - Lecture 6 (Mammography I)Adham MohamedNo ratings yet
- AACR 2012 - Ovarian Cancer Model and Microenvironment Differences - Dr. Rao PapineniDocument1 pageAACR 2012 - Ovarian Cancer Model and Microenvironment Differences - Dr. Rao PapineniPapineni LabsNo ratings yet
- Liver Fibrosis Causes and Methods of Assessment ADocument11 pagesLiver Fibrosis Causes and Methods of Assessment AmichaelNo ratings yet
- Review On Canine Oral Melanoma: An Undervalued Authentic Genetic Model of Human Oral Melanoma?Document9 pagesReview On Canine Oral Melanoma: An Undervalued Authentic Genetic Model of Human Oral Melanoma?Equilibrium EduardoNo ratings yet
- Tto QX Metastasis Cerebrales PDFDocument8 pagesTto QX Metastasis Cerebrales PDFmilagro meza poloNo ratings yet
- Kuliah Class Inter 2Document39 pagesKuliah Class Inter 2dewiswahyuNo ratings yet
- Staging of Oesophageal and Gastric Cancer: Graeme CouperDocument19 pagesStaging of Oesophageal and Gastric Cancer: Graeme CouperLuis FelipeNo ratings yet
- Klasifikasi Tumor Jaringan Lunak PDFDocument10 pagesKlasifikasi Tumor Jaringan Lunak PDFzakibonnie100% (1)
- Differentiated Thyroid Cancer: Presenter: DR Aakriti Athavale Moderated By: GP Capt (DR) PK SahuDocument43 pagesDifferentiated Thyroid Cancer: Presenter: DR Aakriti Athavale Moderated By: GP Capt (DR) PK SahuAakritiNo ratings yet
- Case Study: Breast CancerDocument72 pagesCase Study: Breast CancerJoy Mariel Isadora BurgosNo ratings yet
- Colorectal Cancer: - Dr. Suneet KhuranaDocument36 pagesColorectal Cancer: - Dr. Suneet KhuranaCarlo ToledooNo ratings yet
- Ales 04 96Document8 pagesAles 04 96Daniel Gonzales LinoNo ratings yet
- Biology Project OncolgyDocument23 pagesBiology Project OncolgyAyaan Raza KhanNo ratings yet
- Pathology Of: NeoplasiaDocument23 pagesPathology Of: NeoplasiaBryan de GuzmanNo ratings yet
- Breast CancerDocument129 pagesBreast CancerHope LeeNo ratings yet
- The Breast - Part 2 Dr. Roberto B. Acuña: Hormonal Non-HormonalDocument14 pagesThe Breast - Part 2 Dr. Roberto B. Acuña: Hormonal Non-HormonalMaf BNo ratings yet
- Rare Tumour - Sebaceous Carcinoma of The ScalpDocument2 pagesRare Tumour - Sebaceous Carcinoma of The ScalpInternational Organization of Scientific Research (IOSR)No ratings yet
- NLR To Ovarian CancerDocument8 pagesNLR To Ovarian CancersririniaNo ratings yet
- 1.understanding Cancer PPT LectureDocument184 pages1.understanding Cancer PPT LectureCherry Lou GuanzingNo ratings yet
- CV Ruby GuptaDocument4 pagesCV Ruby GuptaAshish PatilNo ratings yet
- Nano DrugsDocument37 pagesNano Drugsapi-277275270No ratings yet
- Piedmont Studies TableDocument3 pagesPiedmont Studies Tableapi-654365619No ratings yet
- 2 21 PDX and Organoids Model Therapy Response in Prostate CancerDocument13 pages2 21 PDX and Organoids Model Therapy Response in Prostate CancerShuang LiNo ratings yet
- Capecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal CancerDocument6 pagesCapecitabine Monotherapy For Recurrent and Metastatic Nasopharyngeal Cancertrifamonika23No ratings yet
- Cyclopalladated Benzophenone Imines: Synthesis, Antitumor Activity, Cell Accumulation, DNA Interaction, and Cathepsin B InhibitionDocument9 pagesCyclopalladated Benzophenone Imines: Synthesis, Antitumor Activity, Cell Accumulation, DNA Interaction, and Cathepsin B InhibitionsherajekiNo ratings yet