Professional Documents
Culture Documents
DM Gestasional
DM Gestasional
Uploaded by
Yunanda NA0 ratings0% found this document useful (0 votes)
6 views4 pagesDM Gestasional
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDM Gestasional
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
6 views4 pagesDM Gestasional
DM Gestasional
Uploaded by
Yunanda NADM Gestasional
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF or read online from Scribd
You are on page 1of 4
Management of Type 1 Diabetes Mellitus* During Pregnancy
Time Frame
Before conception
Prenatal
Measures
Diabetes iz controlled.
Risk iz lowest if Hb Arclavele are 26% at conception.”
Evaluation includes
# 24-hurine collection (protein excration and creatinine
clearance) to check for renal complications
+ Ophthalmologic examination to check for retinal complications
ECG te check for cardiac complications
Prenatal visits begin 22 soon 2 pregnancy iz recognized,
Frequency of visits is determined by degree of glycemic control.
Dist chould be individualized according te ADA guidelines and
coordinated with | insulin | administration,
Three meals and 3 snacks/day are recommended, with emphasis on
consistent timing,
Women are instructed in and should do plasma glucose
‘self monitoring.
Women should be cautioned about the dangers of hypoglycemia
during exercise and at night:
Women and their family members should be instructed in glucagon
administration,
Hb Arc level should be checked every trimester.
Fetal monitoring with the following should be done weekly from 32
wk to delivery (or eatlieriFindicated):
* Nonstress tests
* Biophysical profiles
* Kick counts
Amount and type of| insulin | should be individualized. In the an;
7/3 of total dose (60% NPH, 40% regular) is taken; in the mt; */3
(50% NPH, 50% regular) is taken.*
During labor and delivery Yaginal delivery at arm is possible fwemen have documented
jating criteria and good glycemic contral
Amniocentesis is not done unless indicated for another problem or
requested by the couple,
(Cesarean delivery should be reserved for obstetrical indications or
fetal macrosomia (=4300 9), which increnses rik of shoulder
jstocia,
Delivery should occur by 38-40 wk,
During delivery, » constant low-dose insulin | infusion is usually
preferred, and the usual sc administration of insulin | is stopped.
IFinduction is planned, the usual PM NPH insulin doses given
‘on the day before induction.
Postpartum and continuing diabetes care should be arranged.
Postpartum | insulin] requirements may decrease by up to 50%.
“Guidelines are only suggested; marked individual variations. require appropriate adjustments,
tHormal-values may differ depending on laboratory methods used
Some hospital programs recommend upto 4| sun | injections daly. Contnueus sc| insulin
‘infusion, which is labor-intensive, can sometimes be given in specialized diabetic research settings.
ADA = American Diabetes Association; Hb A1g = glycosylated Hb; NPH = neutral protamine Hagedorn.
Management of Type 2 Diabetes Mellitus* During Pregnancy
Time Frame
Before conception
Prenatal
During labor and delivery
Hyperslycemia is controlled.
Risk is lowest if Hb Aac levels are 38% at conception.”
Weight loss is encouraged if BMI is >27 ke/m?.
The diet should be low in fat, relatively high in complex carbohydrates,
and high in fiber.
Exercise is encouraged,
For overweight women, diet and caloric intake are individualized and
monitored to avoid weight gain of >9 kg; daytime snacks are
discouraged.
Moderate walling after meals is recommended,
‘Women are instructed in and should do plasma glucose
‘self-monitoring,
‘The 2-h postbreskfaet plasma glucoze level is checked weakly at
clinic visits
Hb Aiclevel should be checked every trimester.
Fetal monitoring with the following should be done weekly from 32 wl
to delivery (or earlier findicated):
© Nonstress tests
© Biophysical profiles
® Kick counts
Amount and tyos of! insulin | is individualized. For obese women,
regular insulin is taken before each meal, For women who are not
obese, 7/3 of total dose (60% NPH, 40% regular) is taken in the sm;
473 (50% NPH, 50% regular) is taken in the m
Management of Gestational Diabetes During Pregnancy
Time Frame Measures
Before conception ‘Women who have had gestational diabetes in previous pregnancies
should try to reach a normal weight and engage in modest exercise.
‘The diet should be low in fat, relatively high in complex
carbohydrates, and high in fiber.
Fasting plasms glucose and Hb Auclevels should be checked.
Prenatal Diet and caloric intake are individualized and monitored to prevent
sssight gain of 72 kg, Obese nomen are discouraged from daytime
Moderate exercise after meals is recommended.
Fetal monitoring with the following should be done weekly from 32 wk
to delivery (or earlier if indicated):
© Nonstress tests
© ‘Biophysical profiles
© Kick counts
Insulin | therapy is reserved for persistent hyperalycemis (fasting
plasma glucose >95 mg/dL or 2-h postprandial plasma glucose
2120 mg/dL) despite 2 trial of dietary therapy for 22 whe
The amount and type of| insulin | should be individualized. For
obese women, regular | insulin | is taken before each meal. For
women who are not obese, 2/3 oftotal dose (60% NPH, 40% regular)
is taleen in the ss; 4/3 (50% NPH, 50% regular) is taleen in the =.
During labor anddelivery Vaginal delivery st term iz possible ifwemen have a
well-documented delivery date and good diabetic control.
Amniocentesis may not be required.
(Cesarean delivery should be reserved for obstetric indications or
fetal macrosoma (©4500 gh hich nereoses sake shoulder
Delivery should occur by 38-40 wk,
HD Ate= glycosylated Hb; NPH = neutral protamine Hagedorn,
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (347)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
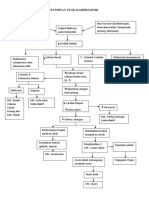
- Pohon Masalah Syok KardiogenikDocument1 pagePohon Masalah Syok KardiogenikYunanda NA100% (1)
- Sap NapzaDocument2 pagesSap NapzaYunanda NANo ratings yet
- Leaflet Pengelolaan SampahDocument3 pagesLeaflet Pengelolaan SampahAdhieguna Prasha Prasetya100% (1)
- LP Hemodialisa ALDocument24 pagesLP Hemodialisa ALYunanda NANo ratings yet
- Pohon Masalah Syok KardiogenikDocument1 pagePohon Masalah Syok KardiogenikYunanda NANo ratings yet
- Leaflet SkabiesDocument2 pagesLeaflet SkabiesYunanda NA100% (1)
- Terapi Modalitas-1Document8 pagesTerapi Modalitas-1Yunanda NANo ratings yet
- LP KekDocument5 pagesLP KekYunanda NA100% (1)
- Pemberian MedikasiDocument53 pagesPemberian MedikasiYunanda NANo ratings yet
- Rps Farmakologi 2016Document27 pagesRps Farmakologi 2016Yunanda NANo ratings yet