Professional Documents
Culture Documents
Jurnal Syok Septik 2
Uploaded by
Yulia PritaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Syok Septik 2
Uploaded by
Yulia PritaCopyright:
Available Formats
DOI: 10.7860/JCDR/2015/10812.
5640
Original Article
Prognosis of Left Ventricular Systolic
Internal Medicine
Section
Dysfunction in Septic Shock Patients
M.Mukhyaprana Prabhu1, Suresh Kumar Yalakala2, Ranjan Shetty3, Ashok Thakkar4, Tulsee Sitapara5
ABSTRACT Results: The mean age of patients were found to be 53.71 ±
Introduction: The prognosis of myocardial dysfunction in 16.76 years. The mortality rate was found to be 48.48% and
critically ill patients with sepsis and its association with mortality among them 43.75% patients had ejection fraction < 50%.
is controversial. We aim to determine the significance of left Non-survivors exhibited significantly lower mean blood pressure
ventricular systolic dysfunction in septic shock patients and (74.19 ± 10.28 versus 80.59 ± 11.31; p = 0.008), lower ejection
their associated outcome. fraction (52.59 ± 16.37 versus 62.56 ± 8.31; p = 0.029) and
higher APACHE III score (89.34 ± 15.41 versus 70.65 ± 13.27; p
Materials and Methods: A prospective, single center,
< 0.001). The receiver operating characteristic curves APACHE
observational study was carried out at an intensive care unit
III score (area under curve = 0.830) and ejection fraction (area
of a tertiary care hospital. A total of 66 patients diagnosed with
under curve = 0.656) were used to predict the mortality in septic
septic shock were enrolled in the study from September 2010 to
patients.
June 2012. The 2D echocardiography was performed for all the
patients. Ejection fraction < 50% was the diagnosing parameter Conclusion: Low ejection fraction, a marker to measure left
for the patients with systolic dysfunction in septic shock. Acute ventricular systolic dysfunction is a predictor of mortality in
Physiology and Chronic Health Evaluation III (APACHE III) score septic shock patients. However, more research is needed to
was calculated. confirm the findings.
Keywords: Echocardiography, Ejection fraction, Mortality
INTRODUCTION The patients have been diagnosed with septic shock as per the
Sepsis is a serious medical condition affecting millions of patients guidelines of ACCP/SCCM Consensus Conference Committee
each year. The average documented incidence of sepsis worldwide [12]. The inclusion criteria included organ dysfunction and acute
is 56-91 cases per 1,00,000 people, with a reported mortality rate circulatory failure characterized by (a) persistent arterial hypotension
of 30% [1]. Myocardial dysfunction is a common feature of sepsis. (defined as a systolic arterial blood pressure <90 mm Hg or
Cardiac dysfunction in septic shock is a crucial component of reduction from baseline by >40 mm Hg), despite adequate volume
multiple organ dysfunction [2] and is an important cause of fatality resuscitation (septic shock) (b) presence of infection, documented
[3,4]. Dysfunction of left ventricle (LV) associated with sepsis has or strongly suspected, with a systemic inflammatory response,
been reported decades ago [2], but was not absolutely recognised together with two or more of the following:
until the widespread use of echocardiography in intensive care - Temperature > 38°C or < 36°C
unit (ICU) [5,6]. The mechanism is still unclear and is probably - Heart Rate > 90 bpm
multifactorial [7].
- Respiratory Rate 30/min with PaCO2 < 32
The pathophysiology and various types of myocardial dysfunction
- Total leukocyte count > 12 x 109 /L or < 4x 109 /L or > 10%
are well documented in literature. Numerous echocardiographic
staff cells
parameters have been developed to assess the LV function in
sepsis [8]. Among these parameters, ejection fraction (EF) is most Exclusion criteria included patients with age lesser than 18
commonly used to evaluate LV systolic function [4,9]. years, pregnancy, patients who documented with valvular heart
disease, known ischemic heart disease, dilated cardiomyopathy,
In spite of larger data, the presence of LV systolic dysfunction and
hypertension, myocarditis, connective tissue diseases, abuse of
its relation with the outcome is still conflicting especially in septic
drugs such as alcohol and cocaine, arrhythmias, diabetes mellitus,
shock patients [5,10]. The correlation between low ejection fraction
hypothyroidism or hyperthyroidism.
and mortality is not clear [2,10,11]. The aim was to evaluate the
significance of LV systolic dysfunction in the patients with septic Baseline clinical variables were collected including age, gender,
shock and its association with the mortality in these patients. co-morbidities, hemodynamic parameters, requirement and dose
of inotropes and Acute Physiology and Chronic Health Evaluation
materials and METHODS (APACHE) III score.
Study Design and Patient Population Echocardiography
A prospective, single centre, observational study was carried out All patients underwent 12 lead electrocardiogram and 2D
at Kasturba Medical College & Hospital, Manipal, India, from echocardiography using Vivid e portable echo machine from GE
September 2010 to June 2012. A total of 66 patients with septic healthcare using 2.5 MHz transducer and Doppler echocardiography
shock were enrolled in the study after complying with inclusion and including Tissue Doppler Imaging. Left lateral position was used to
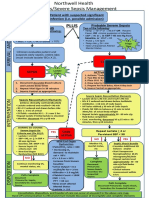
exclusion criteria. The enrollment procedure of patients is shown in analyse the patients. Assessments were made using parasternal
[Table/Fig-1]. Informed consent was obtained and the study was long axis, short axis, apical four chamber and two chamber images
approved by the Institutional Ethics Committee. (177/2010 meeting according to the American Echocardiography Association Criteria.
held on 14th December 2010). The modified Simpson’s method was used to measure the LV
Journal of Clinical and Diagnostic Research. 2015 Mar, Vol-9(3): OC05-OC08 5
M.Mukhyaprana Prabhu et al., Prognosis of Left Ventricular Systolic Dysfunction in Septic Shock patients www.jcdr.net
[Table/Fig-3]: Sources of infection in septic shock patients
Types of micro-organism Number of patients (Percentage)
E.coli 7 (10.6)
Klebsiella 5 (7.5)
[Table/Fig-1]: Enrollment procedure of study patients
Leptospirosis 4 (6.06)
Variables Septic Shock Pseudomonas 9 (13.6)
Demographic Parameters Pseudomonas + Klebsiella 1 (1.5)
Age (years) 53.71 ± 16.76 Staphylococcus aureus 3 (1)
Male, n (%) 34 (51.5%) Streptococcus 1 (1.5)
Length of hospital stay 9.76 ± 4.21 Acinetobacter 6 (9.09)
Length of ICU stay 6.09 ± 3.45 Polymicrobial 0 (0.00)
APACHE III Score 79.71 ± 17.07 Candida 2 (3.03)
Laboratory Parameters Enterococcus 2 (3.03)
Serum creatinine (mg/dL) 1.66 ± 1.18 Klebsiella + E coli 1 (1.5)
pH 7.13 ± 0.75 Rikettsial 1 (1.5)
Hemodynamic parameters Not Known 24 (36.36)
Mean blood pressure (mm Hg) 77.48 ± 11.21 [Table/Fig-4]: Types of microbes involved in septic shock patients
Noradrenaline, n (%) 27 (30.3%)
Dopamine, n (%) 13 (19.7%) The source of infection was not known in most of the patients
(42.8%). Among the known source, the most common source of
Noradrenaline + Dopamine, n (%) 20 (30.3%)
infection was pneumonia (24.2%). The other sources of infection in
No medication, n (%) 6 (9.1%)
various patients are depicted in [Table/Fig-3]. The micro-organism
Echocardiographic Parameters associated with septic shock patients was not known in majority of
Ejection Fraction 57.73 ± 13.72 patients (36.36%). Different types of microbial culture observed in
Cardiac Index 4.17 ± 0.90 septic shock patients are presented in [Table/Fig-4].
[Table/Fig-2]: Baseline characteristics of patients with septic shock A total of 18 (27.27%) patients reported LV systolic dysfunction on
the first day of admission. The mortality rate of septic shock patients
ejection fraction (EF). Left ventricular (LV) systolic dysfunction was was found to be 48.48%. The comparisons among the survivor
defined as LVEF with <50% [13-15]. Cardiac index for assessing and non survivor patients with sepsis are depicted in [Table/Fig-5].
systolic dysfunction was calculated by dividing the cardiac output
Among the inotropes used for maintaining the blood pressure in
to the body surface area of patients.
patients, 44.1% of the survivors were resuscitate with noradrenaline
and combination of noradrenaline and dopamine (59.4%) being the
Statistical Analysis most often used in non surviving septic shock patients.
All data were analysed using SPSS version 16.0. Categorical data are
presented as number of patients (percentage). Descriptive statistical Among the indices of systolic dysfunction, MBP, APACHE III score
analysis is performed for continuous variables. For comparison and ejection fraction showed significant difference among the
between groups, either student’s unpaired t-test or Mann-Whitney U survivors and non survivors. It is clear from the table that mortality
test are used for the continuous variables according to the Gaussian was linked to lower MBP. Fourteen patients among the non-survivors
distribution. The chi-square test was used to assess differences in had ejection fraction < 50%.
categorical variables. All statistical tests were carried out at 5% The ability of ejection fraction and APACHE III score to predict
level of significance. Receiver operating characteristic curve (ROC) the mortality according to ROC curve is shown in [Table/Fig-6,7]
analysis was performed to predict the association of APACHE score respectively. The area under curve for ejection fraction was observed
and ejection fraction with mortality. to be 0.656 and that of APACHE III score was found to be 0.830.
RESULTS DISCUSSION
The mean age of patients was found to be 53.71 ± 16.76 years Sepsis is the major cause of death among critically ill patients and
and 34 (51.5%) patients were male. Mean blood pressure (MBP) accounts for more than 215,000 deaths per year in the United States
was observed as 77.48 ± 11.21 mmHg. Baseline characteristics alone [16,17]. The incidence and frequency of sepsis is continuously
of the patients with septic shock are shown in [Table/Fig-2]. growing due to the factors like aging population, more number of
6 Journal of Clinical and Diagnostic Research. 2015 Mar, Vol-9(3): OC05-OC08
www.jcdr.net M.Mukhyaprana Prabhu et al., Prognosis of Left Ventricular Systolic Dysfunction in Septic Shock patients
Variables Survivors Non Survivors p-value
(n =34) (n=32)
Demographic Parameters
Age (years) 50.35 ± 17.11 57.28 ± 15.87 0.093
Male, n (%) 21 (61.8%) 13 (38.2%) 0.139
APACHE III Score 70.65 ± 13.27 89.34 ± 15.41 <0.001
Laboratory Parameters
Serum creatinine (mg/dL) 1.70 ± 1.25 1.62 ± 1.11 1.00
pH 7.07 ± 1.04 7.20 ± 0.08 0.121
Hemodynamic parameters
Mean blood pressure (mm Hg) 80.59 ± 11.31 74.19 ± 10.28 0.008
Noradrenaline, n (%) 15 (44.1%) 5 (15.6%)
Dopamine, n (%) 6 (17.6%) 7 (21.9%)
Noradrenaline + Dopamine, n (%) 8 (23.5%) 19 (59.4%) 0.006
No medication, n (%) 5 (14.7%) 1 (3.1%)
Echocardiographic Parameters
Ejection fraction 62.56 ± 8.31 52.59 ± 16.37 0.029
Ejection fraction <50%, n (%) 4 (11.76%) 14 (43.75%) 0.005
Cardiac index 4.03 ± 0.77 4.32 ± 1.01 0.311
[Table/Fig-7]: Receiver-operating characteristic curve for predicting mortality by
[Table/Fig-5]: Comparative analysis between survivors and non survivors in septic using APACHE III score. Area under curve is 0.830
shock patients
significant difference in MBP was reported in our study [7]. The
risk of subsequent renal replacement therapy increases as there is
increase in the time spent below the MAP of 75 mm Hg which was
reported by Dunser et al., [20]. Such findings suggest the importance
of addressing ischemic acute renal failure in the absence of frank
hypotension [21]. This correlates that vasoactive substance plays
an important role in septic patients.
In our study, LVEF was depressed in 18 (27.27%) septic shock
patients. A cohort study on the ICU patients by Landsberg et
al., reported 9.1% isolated systolic dysfunction [4]. Studies using
echocardiography reported a 20-60% incidence of reduced EF in
septic shock which was reversible in patients who survive [22-24].
In a landmark study by Parker and colleagues, 50% of the septic
shock patients exhibited ventricular dilatation and hypokinesia
during the first 48 h after admission [2]. Furthermore, compromised
LVEF (43.9% ± 18% versus 55% ± 15%) was observed in survivors
during the first 24 h [11]. In other similar studies [25], evidence of
septic myocardial dysfunction in survivors was shown by depressed
LVEF, although the difference in LVEF between survivors and non-
survivors is not significant [4,13]. These results are contrary to our
[Table/Fig-6]: Receiver-operating characteristic curve for predicting mortality by results. In the present study, survivors had better LVEF than non
using ejection fraction. Area under curve is 0.656
survivors signifying that the low EF is a measure of mortality in these
patients. However, a study on 57 septic patients demonstrated by
patients with compromised immune systems, and the increased Breukmann et al., found that LVEF is a tool for determining systolic
number of patients who had undergone prolonged, high risk surgery dysfunction [14].
[18]. The progression of sepsis often occurs when the host cannot
In our study, APACHE III score showed significantly higher values in
contain the primary infection, a problem frequently related to the
non-survivors. Amongst the ROC curves of APACHE III score and
characteristics of the micro-organism, the large burden of infection,
ejection fraction for predicting the mortality, APACHE III score is
persistent presence of super-antigens and other virulence factors,
resistance of phagocytosis and opsonization often associated considered as a better predictor (AUC= 0.830) of mortality in critically
with antibiotic resistance [19]. Abnormalities in cardiac function is ill patients than ejection fraction (AUC=0.656). Subsequently, other
common in sepsis. studies had reported the good association of APACHE III score and
mortality in intensive care unit patients [26,27].
In this study, the mean age of patients with septic shock was found
to be 53.71 ± 16.76 years which was comparatively less than the
studies reported by David et al., [9]. However, the APACHE III score
Conclusion
in septic shock patients (79.71 ± 17.07) was observed to be similar In a nutshell, left ventricular systolic dysfunction was observed in
with the other reported study [9]. our study with an association of mortality in septic shock patients.
Decreased ejection fraction may be considered as sole criteria for
A prospective study conducted over 106 patients by Pulido et
diagnosing systolic dysfunction and predicting mortality. However,
al., demonstrated that lower mean atrial pressure (MAP) in non-
further studies are still needed to provide clear and confirmatory
survivors is associated with mortality, although they do not show
diagnosis.
significant difference among survivors and non-survivors. The
Journal of Clinical and Diagnostic Research. 2015 Mar, Vol-9(3): OC05-OC08 7
M.Mukhyaprana Prabhu et al., Prognosis of Left Ventricular Systolic Dysfunction in Septic Shock patients www.jcdr.net
REFERENCES [13] Weng L, Liu YT, Du B, Zhou JF, Guo XX, Peng JM, et al. The prognostic value
of left ventricular systolic function measured by tissue Doppler imaging in septic
[1] Jawad I, Luksic I, Rafnsson SB. Assessing available information on the burden
shock. Crit Care. 2012;16(3):R71.
of sepsis: global estimates of incidence, prevalence and mortality. J Glob Health.
[14] Brueckmann M, Huhle G, Lang S, Haase KK, Bertsch T, Weiss C, et al. Prognostic
2012; 2(1):010404.
value of plasma N-terminal pro-brain natriuretic peptide in patients with severe
[2] Parker MM, Shelhamer JH, Bacharach SL, Green MV, Natanson C, Frederick
sepsis. Circulation. 2005;112(4):527-34.
TM, et al. Profound but reversible myocardial depression in patients with septic
[15] Parrillo JE. Pathogenetic mechanisms of septic shock. N Engl J Med. 1993;
shock. Ann Intern Med. 1984;100(4):483-90.
328(20):1471-77.
[3] Maeder M, Fehr T, Rickli H, Ammann P. Sepsis-Associated Myocardial
[16] Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J
DysfunctionDiagnostic and Prognostic Impact of Cardiac Troponins and
Med. 2003;348(2):138-50.
Natriuretic Peptides. CHEST Journal. 2006;129(5):1349-66.
[17] Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR.
[4] Landesberg G, Gilon D, Meroz Y, Georgieva M, Levin PD, Goodman S, et al.
Epidemiology of severe sepsis in the United States: analysis of incidence,
Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart
outcome, and associated costs of care. Crit Care Med. 2001;29(7):1303-10.
J. 2012; 33(7):895-903.
[18] Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the
[5] Hunter J, Doddi M. Sepsis and the heart. Br J Anaesth. 2010;104(1):3-11.
United States from 1979 through 2000. N Engl J Med. 2003;348(16):1546-54.
[6] Paulus WJ, Tschope C, Sanderson JE, Rusconi C, Flachskampf FA, Rademakers
[19] Russell JA. Management of sepsis. N Engl J Med. 2006;355(16):1699-713.
FE, et al. How to diagnose diastolic heart failure: a consensus statement on
[20] Dunser MW, Takala J, Ulmer H, Mayr VD, Luckner G, Jochberger S, et al.
the diagnosis of heart failure with normal left ventricular ejection fraction by the
Arterial blood pressure during early sepsis and outcome. Intensive Care Med.
Heart Failure and Echocardiography Associations of the European Society of
2009;35(7):1225-33.
Cardiology. Eur Heart J. 2007;28(20):2539-50.
[21] Abuelo JG. Normotensive ischemic acute renal failure. N Engl J Med.
[7] Pulido JN, Afessa B, Masaki M, Yuasa T, Gillespie S, Herasevich V, et al. Clinical
2007;357(8):797-805.
spectrum, frequency, and significance of myocardial dysfunction in severe sepsis
[22] Jardin F, Brun-Ney D, Auvert B, Beauchet A, Bourdarias JP. Sepsis-related
and septic shock. Mayo Clin Proc. 2012;87(7):620-28.
cardiogenic shock. Crit Care Med. 1990;18(10):1055-60.
[8] Dittoe N, Stultz D, Schwartz BP, Hahn HS. Quantitative left ventricular systolic
[23] Vieillard Baron A, Schmitt JM, Beauchet A, Augarde R, Prin S, Page B, et al.
function: from chamber to myocardium. Crit Care Med. 2007;35(8 Suppl):S330-
Early preload adaptation in septic shock? A transesophageal echocardiographic
39.
study. Anesthesiology. 2001;94(3):400-06.
[9] Sturgess DJ, Marwick TH, Joyce C, Jenkins C, Jones M, Masci P, et al. Prediction
[24] Bouhemad B, Nicolas-Robin A, Arbelot C, Arthaud M, Feger F, Rouby JJ. Acute
of hospital outcome in septic shock: a prospective comparison of tissue Doppler
left ventricular dilatation and shock-induced myocardial dysfunction. Crit Care
and cardiac biomarkers. Crit Care. 2010;14(2):R44.
Med. 2009; 37(2):441-47.
[10] Furian T, Aguiar C, Prado K, Ribeiro RV, Becker L, Martinelli N, et al. Ventricular
[25] Jardin F, Fourme T, Page B, Loubieres Y, Vieillard-Baron A, Beauchet A, et al.
dysfunction and dilation in severe sepsis and septic shock: relation to endothelial
Persistent preload defect in severe sepsis despite fluid loading: A longitudinal
function and mortality. J Crit Care. 2012;27(3):319 e9-15.
echocardiographic study in patients with septic shock. Chest. 1999;116(5):1354-
[11] Vieillard-Baron A, Caille V, Charron C, Belliard G, Page B, Jardin F. Actual
59.
incidence of global left ventricular hypokinesia in adult septic shock. Crit Care
[26] Shrestha GS, Gurung R, Amatya R. Comparison of Acute Physiology, Age, Chronic
Med. 2008; 36(6):1701-06.
Health Evaluation III score with initial Sequential Organ Failure Assessment score
[12] Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, et al. Definitions
to predict ICU mortality. Nepal Med Coll J. 2011;13(1):50-54.
for sepsis and organ failure and guidelines for the use of innovative therapies in
[27] Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et
sepsis. The ACCP/SCCM Consensus Conference Committee. American College
al. The APACHE III prognostic system. Risk prediction of hospital mortality for
of Chest Physicians/Society of Critical Care Medicine. 1992. Chest. 2009;136(5
critically ill hospitalized adults. Chest. 1991;100(6):1619-36.
Suppl):e28.
PARTICULARS OF CONTRIBUTORS:
1. Professor, Department of Medicine, Kasturba Medical College and Hospital, Manipal, Karnataka, India.
2. Junior Resident, Department of Medicine, Kasturba Medical College & Hospital, Manipal, Karnataka India.
3. Professor, Department of Cardiology, Kasturba Medical College & Hospital, Manipal, Karnataka India.
4. Senior Manager - Clinical Research & Medical Writing, Department of Clinical Trials, Sahajanand Medical Technologies Pvt. Ltd., Surat, Gujarat, India.
5. Trainee Medical Writer, Department of Clinical Trials, Sahajanand Medical Technologies Pvt. Ltd., Surat, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR:
Dr. Ranjan Shetty,
Professor, Department of Cardiology, Kasturba Medical College & Hospital, Manipal-576104, Karnataka, India. Date of Submission: Aug 11, 2014
E-mail : ranjanshettyk@yahoo.com Date of Peer Review: Sep 27, 2014
Date of Acceptance: Oct 20, 2014
Financial OR OTHER COMPETING INTERESTS: None. Date of Publishing: Mar 01, 2015
8 Journal of Clinical and Diagnostic Research. 2015 Mar, Vol-9(3): OC05-OC08
Copyright of Journal of Clinical & Diagnostic Research is the property of JCDR Research &
Publications Private Limited and its content may not be copied or emailed to multiple sites or
posted to a listserv without the copyright holder's express written permission. However, users
may print, download, or email articles for individual use.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Faktor Faktor Yang Berhubungan Dengan Perilaku Penggunaan Alat Kontrasepsi Non Mket Pada Wus Peserta KB Aktif Di Kecamatan Oebobo Kota KupangDocument8 pagesFaktor Faktor Yang Berhubungan Dengan Perilaku Penggunaan Alat Kontrasepsi Non Mket Pada Wus Peserta KB Aktif Di Kecamatan Oebobo Kota KupangYulia PritaNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- ID Tungau Debu Rumah Di Kelurahan RanotanaDocument5 pagesID Tungau Debu Rumah Di Kelurahan RanotanaYulia PritaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Jurnal 2Document8 pagesJurnal 2Yulia PritaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Jurnal Musik Pra Oprasi Mengalami Penurunan Kecemasan PDFDocument9 pagesJurnal Musik Pra Oprasi Mengalami Penurunan Kecemasan PDFYulia PritaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Pathophysiology and Treatment Syok Septic in PediatricDocument41 pagesPathophysiology and Treatment Syok Septic in PediatricGustomo PanantroNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- ICU-Acquired Weakness and Recovery From Critical IllnessDocument9 pagesICU-Acquired Weakness and Recovery From Critical IllnessFebrian ParuraNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- A Review of The Outpatient Treatment Methods For COVID-19: A Special Interview With Dr. Pierre KoryDocument41 pagesA Review of The Outpatient Treatment Methods For COVID-19: A Special Interview With Dr. Pierre KoryJan Willem van BorselenNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Patient With Suspected Significant Infection (I.e. Possible Admission)Document2 pagesPatient With Suspected Significant Infection (I.e. Possible Admission)Ryaa Nitaa AdyaaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Multiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundDocument6 pagesMultiple Organ Dysfunction Syndrome in Sepsis: 16 Mei 2016 BackgroundrahayuNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Clinical Case Report Powerpoint PresentationDocument24 pagesClinical Case Report Powerpoint Presentationapi-354139540100% (1)
- Resuscitation Fluids - NEJMDocument9 pagesResuscitation Fluids - NEJMJHWNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Severe Sepsisand Septic Shock GuidelinesDocument17 pagesSevere Sepsisand Septic Shock GuidelinesdrquamrulNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Sirs & ModsDocument5 pagesSirs & Modsmarlou agananNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Viarasilpa Et Al 2019 Venous Thromboembolism in Neurocritical Care PatientsDocument9 pagesViarasilpa Et Al 2019 Venous Thromboembolism in Neurocritical Care Patientsateia83No ratings yet
- Guide To The Intercollegiate MRCS Examination - Singapore 2012Document55 pagesGuide To The Intercollegiate MRCS Examination - Singapore 2012juweriyNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- BronchiolitisDocument17 pagesBronchiolitisRizky DarmawanNo ratings yet
- Use of Vasopressors and InotropesDocument16 pagesUse of Vasopressors and InotropesIrving H Torres LopezNo ratings yet
- Erythroderma: Key PointsDocument5 pagesErythroderma: Key Pointsramdani witiaNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- HemorrhageDocument239 pagesHemorrhageparmeshori100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 2012 CHD 3 Annual ReportDocument72 pages2012 CHD 3 Annual Reportjedy_08No ratings yet
- Module 7 - Meningitis and EncephalitisDocument35 pagesModule 7 - Meningitis and EncephalitisRick RanitNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Indications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateDocument39 pagesIndications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateAhmed MostafaNo ratings yet
- Kuliah Syok 2020 (DR Ahmad Yafiz Hasby SpAn)Document48 pagesKuliah Syok 2020 (DR Ahmad Yafiz Hasby SpAn)RezaNo ratings yet
- April 2007 Written Summary EMRAPDocument3 pagesApril 2007 Written Summary EMRAPAshleyNo ratings yet
- Urosepsis: Oleh: DR - Yolan Novia Ulfah Pembimbing: Dr. Prabudi, SP.B (K) Onk, M.Kes, FICSDocument30 pagesUrosepsis: Oleh: DR - Yolan Novia Ulfah Pembimbing: Dr. Prabudi, SP.B (K) Onk, M.Kes, FICSYolan Novia UlfahNo ratings yet
- SIRS, Sepsis, and Septic Shock Criteria - MDCalcDocument4 pagesSIRS, Sepsis, and Septic Shock Criteria - MDCalcMustafa AadanNo ratings yet
- SSC 2021 GuidelinesDocument59 pagesSSC 2021 GuidelinesPrasannakumar P CNo ratings yet
- Novel Tools For Hemodynamic Monitoring in Critically Ill Patients With Shock - UpToDateDocument26 pagesNovel Tools For Hemodynamic Monitoring in Critically Ill Patients With Shock - UpToDateAlex KuliaNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Assessment Diagnosis Planning Nursing Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Nursing Intervention Rationale EvaluationJoshua De Guzman MiraNo ratings yet
- Campbell 2006Document9 pagesCampbell 2006Sílvia TrindadeNo ratings yet
- Shock in Obstetrics: Dr. Hem Nath Subedi Resident ObgynDocument25 pagesShock in Obstetrics: Dr. Hem Nath Subedi Resident ObgynNinaNo ratings yet
- Fournier's Gangrene: An Experience in Tertiary Care HospitalDocument9 pagesFournier's Gangrene: An Experience in Tertiary Care HospitalKriti KumariNo ratings yet
- Role of Synthetic Proteins and Peptides in AnimalsDocument7 pagesRole of Synthetic Proteins and Peptides in AnimalsroniNo ratings yet
- Reference Intervals List - Printed Format Version 1 FinalDocument3 pagesReference Intervals List - Printed Format Version 1 FinalShady FawazNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)