Professional Documents
Culture Documents
NIH Public Access: Author Manuscript
Uploaded by
Ikhdin SaadhiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NIH Public Access: Author Manuscript
Uploaded by
Ikhdin SaadhiCopyright:
Available Formats
NIH Public Access
Author Manuscript
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Published in final edited form as:
NIH-PA Author Manuscript
J Pediatr Surg. 1975 October ; 10(5): 623–630.
Bench Surgery and Renal Autotransplantation in the Pediatric
Patient
John R. Lilly, Ronald R. Pfister, Charles W. Putnam, Ann M. Kosloske, and Thomas E. Starzl
Divisions of Pediatric Surgery, Urology, and Transplantation, Department of Surgery, University of
Colorado Medical Center, Denver, Colo.
Abstract
Surgery at the work bench has developed as a by-product of the extensive experience in renal
homotransplantation. A basic tenet of the transplant operation is organ survival outside the human
body for a finite period. Recent refinements in kidney preservation have extended the permissible
ex vivo period to several days. Consequently, extracorporeal procedures have become highly feasible
NIH-PA Author Manuscript
and a practical adjunct for operative renal surgery.
Bench surgery and autotransplantation thus far have been underexploited in pediatric surgery despite
potential applicability in a significant number of childhood lesions. At the University of Colorado
Medical Center, 14 patients have been treated by extracorporeal renal surgery and have been reported
in part.1-3 The purpose of this communication is to review the technical aspects of this new operative
procedure, present two case reports, and discuss the potential role of extracorporeal surgery and renal
autotransplantation as it pertains to the pediatric patient.
PATIENT MATERIAL
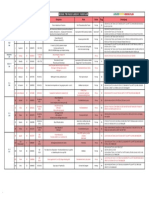
The clinical experience with extracorporeal renal surgery and autotransplantation is shown in
Table 1. There has been no mortality. Autotransplantation failed in one patient (Patient 4).4
Although partially described earlier,1,2 Patients 7 and 1 are presented in detail to illustrate
several specific indications and technical points in management.
CASE REPORTS
NIH-PA Author Manuscript
Patient 7
This was a 6-yr-old boy admitted for consideration for permanent urinary diversion. At 5 mo
old he was found to have bilateral hydronephrosis secondary to posterior urethral valves.
Multiple operative procedures performed over the ensuing 5 yr had resulted in a scarred, rigid,
distal ureter, massive ureteral reflux, marked caliectasis of the left kidney and a functionless
right kidney (Fig. 1). He continued to have recurrent urinary tract infections.
At surgical exploration, the distal one-half of the left ureter was discarded. The proximal ureter,
although dilated, was supple and appeared salvageable. An attempt to obtain ureteral length
by mobilizing the kidney was unsuccessful, and it was decided to carry out autotransplantation.
Because of long-standing hydronephrosis, the kidney was too large to be confined to the iliac
© 1975 by Grune & Stratton, Inc.
Address for reprint requests: John R. Lilly, M.D., Department of Surgery, University of Colorado Medical Center, 4200 E. Ninth Ave.,
Denver, Colo. 80220..
Presented before the 6th Annual Meeting of the American Pediatric Surgical Association, San Juan, Puerto Rico, April 10–12, 1975.
Lilly et al. Page 2
fossa and be revascularized by iliac vessels. Therefore, the left aortic bifurcation and the left
common iliac vein were prepared for subsequent renal anastomosis.
NIH-PA Author Manuscript
The left kidney and proximal ureter were removed and flushed for 10 min with chilled (5°C)
Perfudex. Revascularization was by end-to-side anastomoses of the renal artery and vein to the
aorta and left common iliac vein, respectively. Total ischemic time was 45 min. The proximal
ureter reached the bladder easily and was reimplanted by the Leadbetter-Politano technique5
after a “tailoring” procedure.6 His postoperative course was unremarkable.
Three months later excretory urogram showed increasing obstruction of the
ureteroneocystomy. At reoperation there was still sufficient ureter available to redo the
ureterovesical anastomosis, which was done by a Paquin technique.7 He has done well in the
14 mo since operation.
Patient 1
Hypertension developing in late adolescence was proved to be due to bilateral medial
fibroplasia in this 23-yr-old girl. The right renal artery was most severely involved by excretory
urography, arteriography, and the right-to-left ratio of plasma renin activity. Following bench
surgery the right kidney was autotransplanted to the left iliac fossa by end-to-end anastomosis
of the hypogastric arterial branches to three arterial branches from the main renal artery.
Postoperatively, hypertension disappeared but during the ensuing months it gradually recurred.
NIH-PA Author Manuscript
On repeat arteriography all branches to the transplanted kidney were patent, but the left renal
arterial stenosis was seen to have progressed. Consequently, the left kidney was
autotransplanted to the right iliac fossa, again using ex vivo renal arteriography, and all
visualized lesions were resected at the bench. The three segmental renal arterial branches were
individually anastomosed to the right hypogastric artery branches. The kidney was
revascularized after 5 hr and 35 min. Postoperatively, the patient has been normotensive. An
arteriogram 6 wk after the second autotransplantation showed that all six arterial anastomoses
were patent (Fig. 2).
RATIONALE
The unusual tolerance of the kidney to an ex vivo state permits a variety of special operations
that would be difficult or impossible in situ. Exposure of intrarenal lesions and dissection of
secondary arterial branches, for example, are greatly facilitated by operating on the organ in a
free state. Furthermore, a totally bloodless field allows a more deliberate and unhurried surgical
approach that might be otherwise hazardous or unsuccessful. In addition, if constant perfusion
is being used, the operative repair can be tested and revised before reimplantation.
NIH-PA Author Manuscript
It is unnecessary to point out that kidney transplantation is more expeditiously performed in
the iliac rather than the renal fossa. The iliac vessels are relatively superficial, readily accessible
and, by their proximity to the bladder, predispose to handy ureteral reimplantation. Moreover,
the trifurcation of the hypogastric artery makes several large arterial branches available for
anastomosis to segmental renal arteries that may be advantageous in certain cases of
renovascular hypertension (Patient 1). The iliac fossa is still a preferable transplant location
even if the organ is oversized, which may be the case in a solitary, hypertrophied kidney or in
long-standing hydronephrosis. In this situation, the proximity of the nearby aorta and vena
caval bifurcation make these vessels more suitable for renal revascularization (Patient 7).
TECHNIQUE
The essential components of bench surgery are: (1) nephrectomy; (2) renal perfusion; (3)
extracorporeal operation, and; (4) autotransplantation. The technical aspects of the procedure
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 3
are straightforward and, to some extent, elementary. The operation may be varied according
to the preference of the surgeon and the renal lesion to be corrected. The nephrectomy may be
done through a flank incision and, after extracorporeal reconstruction, the kidney reimplanted
NIH-PA Author Manuscript
via a standard transplant approach.8 Alternatively, the entire operation may be carried out
through a single transperitoneal incision. The ureter may be left attached to the bladder or it
may be divided, taken with the kidney to the work bench, and then reunited to bladder, ureter,
or renal pelvis. The kidney may be transplanted in its normal anatomic relationship or turned
front to back or upside down using either the ipsilateral or contralateral iliac fossa as the
transplant bed.
Flushing the kidney with chilled electrolyte solution to which procaine and/or heparin have
been added is a simple, effective method of renal preservation for 1 or 2 hr. Employment of
continuous pulsatile perfusion extends the “safe” ischemic period of the kidney to at least a
half a day and perhaps as long as 3 days.9 In addition, a continual assessment of the functional
status of the organ is permitted and the opportunity afforded to alter pressure and flow rates.
Its disadvantages are the expense and the need for a trained technician.
After removal, the kidney may be perfused and refrigerated while the operation continues or,
taken to the work bench and operated on immediately. If the ureter is left in situ, special long
tubing is required between the machine and the kidney. Under these circumstances, it is
important to keep collateral ureteric blood out of the perfusate by obstructing the ureter during
NIH-PA Author Manuscript
perfusion with an atraumatic clamp.
POTENTIAL ROLE IN THE PEDIATRIC PATIENT
Whatever the technical methodology, there are certain pediatric renal conditions in which the
operation appears to have a very specific role. These are: (1) selected cases of renovascular
hypertension; (2) some cases of congenital obstructive uropathy; (3) patients with bilateral
Wilms' tumor, and; (4) occasionally renal trauma.
Renovascular Hypertension
With a few notable exceptions10,11 operative treatment of renovascular hypertension in
children has been unsuccessful,12-14 and nephrectomy has been required despite awareness of
the significant incidence of either concomitant or subsequent disease in the other kidney.14
The high technical failure rate of angioplastic operations is primarily due to the tiny caliber of
the renal vessels. The difficulty is compounded by the obligatory inflow occlusion that
predisposes to vascular thrombosis. Conversely, renal blood is washed out during the initial
perfusion in ex vivo surgery. The resultant hypothermic state permits a meticulous and precise
vascular repair. The use of an operating microscope during surgery and high-resolution
NIH-PA Author Manuscript
arteriography after correction 1,4 are additional technical refinements available to the surgeon
at the work bench.
Cure of renovascular hypertension by extracorporeal operation in children has been reported
on several occasions.11,15 In the future, vascular repair at the work bench should be attempted
in most cases before resorting to nephrectomy.
Congenital Obstructive Uropathy
Urinary diversion by ileal conduit or other exteriorization operations has been widely employed
for treatment of certain kinds of obstructive uropathy in infants and children. As long-term
follow-up data have accumulated, it has become apparent that these procedures have a
significant incidence of delayed complications and, more importantly, have not protected from
gradual deteriorization of renal function.16,17 Hendren18 has been the principle advocate for
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 4
preservation of natural urologic anatomy and, in fact, has carried out reconstruction in 32
children who had previously undergone urinary diversion. The technical ingenuity in
reclaiming previously diverted urinary tracts using intestinal bridges is remarkable. However,
NIH-PA Author Manuscript
in a number of patients with short proximal ureters, renal autotransplantation to the iliac fossa
eliminates the problem of the ureteric-bladder gap (Patient 7). Furthermore, autotransplantation
may avoid urinary diversion in the first place in patients whose principal lesion is ureteric.
Bilateral Wilms' Tumor
In spite of major advances in adjunctive cancer chemotherapy and radiotherapy, the long-term
outlook for bilateral Wilm's tumor is poor. Fay et al.19 have reported only 13.8% 5-yr survival
in 58 patients. Since the overall incidence of tumor bilaterally is nearly 10%, the problem is
not an inconsequential one, and current recommendations for “individualization”20 of cases
seem to avoid the issue of providing definitive surgical guidelines. Of the different operative
approaches presently used in this condition, one of the most popular is total excision of the
more involved kidney and partial nephrectomy of the contralateral organ. Along with other
adjunctive therapy, limited radiation is given postoperatively to the renal remnant.
Admitting the greater malignant potential of bilateral Wilms' tumor, there are several technical
factors contributing to the high failure rate with this latter approach. Partial nephrectomy is an
inexact, imperfect, and occasionally bloody undertaking having a good chance for leaving
tumor behind either at the surgical margin or in separate, deep intrarenal locations. The
NIH-PA Author Manuscript
unavoidable renal transection and tumor handling, unthinkable in unilateral disease, must result
in tumor spillage. Additionally, the presence of the kidney remnant precludes proper lymph
node dissection of the renal fossa. Nor can suitable radiation doses be delivered to the kidney
bed because of the very real fear of radiation nephritis to the remaining renal tissue.21
The advantages of extracorporeal surgery are especially appealing in patients with bilateral
Wilms' tumor. Careful definitive tumor excision in controlled situations is possible at the work
bench not only for the less involved kidney but even for the more involved one, if necessary
(Fig. 3). Semb22 has shown that extensive partial nephrectomy, leaving as little as 15% of renal
tissue, is compatible with good health. Calne23 has carried out ex vivo bilateral excision of
renal cancer in an adult, leaving an estimated one-third of renal substance for simultaneous
autotransplantation with a good result.
Besides a more definitive tumor dissection, ex vivo excision of the nephroblastoma avoids
tumor spill into the wound; removal of the organ from the renal fossa facilitates regional lymph
node dissection, and transplantation of the organ to the iliac fossa permits full dose radiation
to the empty renal bed.
NIH-PA Author Manuscript
Renal Trauma
The most common indication for nephrectomy following blunt abdominal trauma in children
is the finding of renal hemorrhage in the presence of an associated injury, usually the spleen
or liver. The patient is often hemodynamically unstable, and the surgeon is faced with the
alternative of nephrectomy or attempted renal repair. Nephrectomy is the usual choice despite
the fact that many traumatic renal lesions are potentially correctable. A third alternative in this
situation would be nephrectomy and extracorporeal surgery. With the kidney refrigerated or
perfused, the associated injuries are tackled and the operation completed. The renal injury may
then be repaired at the bench and autotransplantation carried out either at the same time or 12–
24 hr later depending on the patient's condition.
In 1963, Hardy24 reported the first successful case of renal autotransplantation using this
general approach. In this instance, the injury was iatrogenic. Lim and colleagues25 and we1
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 5
reported treatment of renal gunshot and stab wounds, respectively, by autotransplantation
techniques.
NIH-PA Author Manuscript
SUMMARY AND CONCLUSIONS
A new operative procedure in renal surgery has evolved from the extensive recent experience
in kidney transplantation. Bench surgery and autotransplantation have not been, as yet, fully
exploited by surgeons caring for children. This approach to reconstruction of renal substance
and renal vessels has as its greatest dividend conservation of kidney tissue. The operation has
specific applicability for selected cases of: (1) renovascular hypertension; (2) congenital
obstructive uropathy; (3) bilateral Wilms' tumor, and; (4) renal trauma in children.
Acknowledgments
We acknowledge with appreciation the competent and tireless secretarial assistance of Nancy Dragoo.
Supported in part by research grants from the Veterans Administration; by NIH Grants AI-AM-08898 and AM-07772;
and by NIH Grants RR-00051 and RR-00069 from the General Clinical Research Centers Program of the Division of
Research Resources.
REFERENCES
NIH-PA Author Manuscript
1. Corman JL, Anderson JT, Taubman J, et al. Ex vivo perfusion, arteriography, and autotransplantation
procedures for kidney salvage. Surg Gynecol Obstet 1973;137:659. [PubMed: 4581056]
2. Husberg BS, Bakshandeh K, Lilly JR, et al. Five cases and five unusual indications for autogenic renal
transplantation. Acta Chir Scand. in press.
3. Putnam CW, Halgrimson CG, Stables DP, et al. Ex vivo renal perfusion and autotransplantation in
treatment of calculous disease or abdominal aortic aneurysm. Urology 1975;5:337. [PubMed:
1091064]
4. Corman JL, Girard R, Fiala M, et al. Arteriography during ex vivo renal perfusion. Urology 1973;2:222.
[PubMed: 4583817]
5. Politano VA, Leadbetter WF. An operative technique for the correction of vesicoureteral reflux. J Urol
1958;79:932. [PubMed: 13539988]
6. Hendren WH. Operative repair of mega-ureter in children. J Urol 1969;101:491. [PubMed: 5776032]
7. Paquin AJ. Ureterovesical anastomosis: The description and evaluation of a technique. J Urol
1959;82:573. [PubMed: 14430329]
8. Starzl, TJ. Experience in Renal Transplantation. Saunders; Philadelphia: 1964.
9. Belzer FO, Ashby BS, Dunphy JE. Twenty-four hour and 72 hour preservation of canine kidneys.
Lancet 1967;2:536. [PubMed: 4166894]
10. Fry WJ, Ernst CB, Stanley JC, et al. Renovascular hypertension in the pediatric Patient. Arch Surg
NIH-PA Author Manuscript
1973;107:692. [PubMed: 4200678]
11. Stoney RJ, Cooke PA, String ST. Surgery for renovascular hypertension in children. J Pediatr Surg.
in press.
12. Coran AG, Schuster SR. Renovascular Hypertension in Childhood. Surgery 1968;64:672. [PubMed:
5676610]
13. Mustard, WT.; Ravitch, MM.; Snyder, WH., Jr, et al. Pediatric Surgery. Vol. 2. Year Book; Chicago:
1972.
14. Foster JH, Pettinger WA, Oates JA, et al. Malignant hypertension secondary to renal artery stenosis
in children. Ann Surg 1966;164:700. [PubMed: 5924790]
15. Kaufman JJ, Alferez C, Navarrette RV. Autotransplantation of a solitary functioning kidney for
renovascular hypertension. J Urol 1969;102:146. [PubMed: 4894402]
16. Smith ED. Follow-up studies on 150 ileal conduits in children. J Pediatr Surg 1972;7:1. [PubMed:
5013120]
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 6
17. Delgado GE, Muecke EC. Evaluation of 80 cases of ileal conduits in children: Indication, complication
and results. J Urol 1973;109:311. [PubMed: 4685746]
18. Hendren WH. Urinary tract refunction-alization after prior diversion in children. Ann Surg
NIH-PA Author Manuscript
1974;180:494. [PubMed: 4416811]
19. Fay R, Brosman S, Williams DI. Bilateral nephroblastoma. J Urol 1973;110:119. [PubMed: 4351545]
20. Canale VC, Muecke EC. Wilm's tumor—a clinical review. Cancer J Clin 1974;24:66.
21. Perez CA, Karman HH, Keith J, et al. Treatment of Wilms' tumor and factors affecting prognosis.
Cancer 1973;32:609. [PubMed: 4353714]
22. Semb C. Conservative renal surgery. Roy Coll Surg Edinb 1964;10:9.
23. Calne RY. Treatment of bilateral hypernephromas by nephrectomy, excision of tumor and
autotransplantation. Lancet 1973;2:1164. [PubMed: 4127546]
24. Hardy JD. High ureteral injuries. Management by autotransplantation of the kidney. JAMA
1963;184:97. [PubMed: 13960761]
25. Lim RC, Eastman AB, Blaisdell FB. Renal autotransplantation: Adjunct to repair of renal vascular
lesions. Arch Surg 1972;105:847. [PubMed: 4565374]
NIH-PA Author Manuscript
NIH-PA Author Manuscript
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 7
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Fig. 1.
The preoperative excretory urogram of Patient 7. The right kidney does not function. The left
kidney shows marked caliectasis; the proximal ureter is dilated; the distal ureter is poorly
visualized and on other films is rigid and stenotic. Metallic clips are from prior attempts at
ureteral reimplantation.
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 8
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Fig. 2.
Postoperative angiogram of Patient 1. Both kidneys have been autotransplanted into the
contralateral iliac fossa. Revascularization in both instances required triple anastomoses
between the branches of the hypogastric and renal segmental arteries.
NIH-PA Author Manuscript
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Lilly et al. Page 9
NIH-PA Author Manuscript
NIH-PA Author Manuscript
NIH-PA Author Manuscript
Fig. 3.
Schematic illustration of bench surgery for bilateral Wilms' tumor. The four components of
this procedure are depicted: nephrectomy, renal perfusion, ex vivo operation, and
autotransplantation.
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
NIH-PA Author Manuscript NIH-PA Author Manuscript NIH-PA Author Manuscript
Table 1
Renal Autotransplantation (University of Colorado Series)
Patient No. Diagnosis Age Sex Autografted Kidney
Lilly et al.
(Yr) Kidney Salvaged
1* Renovascular hypertension (medial fibroplasia) 23 F R+L Yes–Yes
2 Renovascular hypertension (stob wound) 20 M R Yes
3 Renovascular hypertension (medial fibroplasia) 42 F R Yes
4* Bilateral renal cell carcinomas 45 M R+L No–No
5 Renovascular hypertension (atherosclerosis) 43 M L Yes
6 Renal cell carcinoma (solitary kidney) 52 F R Yes
7 Congenital obstructive uropathy 6 M L Yes
8 Thrombosis, homagraft renal artery 30 M Yes
9 Renovascular hypertension (renal artery stenosis after bypass graft) 44 M L Yes
10 Calculi (solitary kidney) 55 M L Yes
11 Renovascular hypertension and aortic aneurysm 63 M L Yes
12† Renovascular hypertension and aortic aneurysm 63 M R+L Yes–Yes
13† Renovascular hypertension (medial fibroplasia) 44 F R+L Yes–Yes
14 Renovascular hypertension (medial fibroplasia) 39 F R Yes
*
Bilateral autotransplantation (delayed).
†
Bilateral autotransplantation (simultaneous).
J Pediatr Surg. Author manuscript; available in PMC 2010 October 14.
Page 10
You might also like
- House OfficerDocument32 pagesHouse Officerapi-3705046100% (1)
- HydronephrosisDocument3 pagesHydronephrosisCarla AlmerolNo ratings yet
- Pi Is 2210261215001479Document3 pagesPi Is 2210261215001479hussein_faourNo ratings yet
- Complex Case of Ureteropelvic Junction Obstruction 2024 International JournaDocument3 pagesComplex Case of Ureteropelvic Junction Obstruction 2024 International JournaRonald QuezadaNo ratings yet
- Use of locking-loop nephrostomy catheters in dogs and catsDocument10 pagesUse of locking-loop nephrostomy catheters in dogs and catsBernardo BertoldiNo ratings yet
- Organ Transplantation Historial Perspective and Current PracticeDocument14 pagesOrgan Transplantation Historial Perspective and Current PracticehkdawnwongNo ratings yet
- Renal Replacement Therapy Review: Past, Present and FutureDocument11 pagesRenal Replacement Therapy Review: Past, Present and FuturerkNo ratings yet
- Anomalous Non-bifurcating Portal Vein Protected During Extended Right Hepatectomy Using Hanging ManeuverDocument7 pagesAnomalous Non-bifurcating Portal Vein Protected During Extended Right Hepatectomy Using Hanging ManeuverMARIO DCARLO TREJO HUAMANNo ratings yet
- Pearse Et Al 2018 Non Functioning KidneyDocument4 pagesPearse Et Al 2018 Non Functioning Kidneyabdalsalaam1No ratings yet
- Article 39794Document4 pagesArticle 39794d.amouzou1965No ratings yet
- Correspondence To EditorDocument2 pagesCorrespondence To Editormanfel_26No ratings yet
- Yan 2015Document4 pagesYan 2015ELIECERNo ratings yet
- Transplantation of Organs Feasible or Practical?: Wizen IsDocument32 pagesTransplantation of Organs Feasible or Practical?: Wizen IswunderfullifeNo ratings yet
- Bile Leak CaseDocument6 pagesBile Leak CaseDimas ErlanggaNo ratings yet
- Retroperitoneal Appendicitis: A Surgical Dilemma: Euroasian Journal of Hepato-Gastroenterology January 2013Document3 pagesRetroperitoneal Appendicitis: A Surgical Dilemma: Euroasian Journal of Hepato-Gastroenterology January 2013putraNo ratings yet
- Percutaneous Nephrolithotomy in Case of Crossed Fused Renal Ectopia: A Case ReportDocument3 pagesPercutaneous Nephrolithotomy in Case of Crossed Fused Renal Ectopia: A Case ReportDr.ankit AnandNo ratings yet
- Historical Article: The First Human Renal TransplantsDocument3 pagesHistorical Article: The First Human Renal TransplantsRossalia VisserNo ratings yet
- Subsidence of Hypertension in A Patient With GiantDocument4 pagesSubsidence of Hypertension in A Patient With GiantSinbijeo GinNo ratings yet
- Comparison of Open and Laproscopic Live Donor NephrectomyDocument7 pagesComparison of Open and Laproscopic Live Donor NephrectomyEhab Omar El HalawanyNo ratings yet
- 804 FullDocument8 pages804 FullNoor HadyNo ratings yet
- JOURNALDocument4 pagesJOURNALChiara FajardoNo ratings yet
- Severe Pelvic Fracture With Profound Hypotension: A Case Report and Treatment AlgorithmDocument3 pagesSevere Pelvic Fracture With Profound Hypotension: A Case Report and Treatment AlgorithmodyNo ratings yet
- 2018 Article 1089Document5 pages2018 Article 1089Andreea StreuleaNo ratings yet
- Fistula Nefrocolica Por RFADocument3 pagesFistula Nefrocolica Por RFARenan DiasNo ratings yet
- Reconstruction of Late-Onset Transplant Ureteral Stricture DiseaseDocument6 pagesReconstruction of Late-Onset Transplant Ureteral Stricture DiseaseAnanda KumarNo ratings yet
- Ureteric ComplicationsDocument7 pagesUreteric ComplicationstnsourceNo ratings yet
- Borges Dias 2016Document2 pagesBorges Dias 2016Fandi AhmadNo ratings yet
- Yu 2013Document4 pagesYu 2013raissametasariNo ratings yet
- Hepatic Subcapsular BIloma A Rare Complication of Laparoscopic CholecystectomyDocument4 pagesHepatic Subcapsular BIloma A Rare Complication of Laparoscopic CholecystectomyIndra PrimaNo ratings yet
- Metro Fan ofDocument3 pagesMetro Fan ofsahandNo ratings yet
- Management of Penile Fracture: Ahmad M. El-Taher, Hassan A. Aboul-Ella, Mohamed A. Sayed, and Atef A. GaafarDocument3 pagesManagement of Penile Fracture: Ahmad M. El-Taher, Hassan A. Aboul-Ella, Mohamed A. Sayed, and Atef A. GaafarTeja LaksanaNo ratings yet
- Use of The Appendix To Replace A Ureter. Case ReportDocument2 pagesUse of The Appendix To Replace A Ureter. Case ReportPacVitorNo ratings yet
- Timetable PosterExDocument45 pagesTimetable PosterExNeo Rodriguez AlvaradoNo ratings yet
- Retroperitoneal Appendicitis: A Surgical DilemmaDocument2 pagesRetroperitoneal Appendicitis: A Surgical DilemmaputraNo ratings yet
- Portocaval Shunt Throughout Anhepatic Phase in Orthotopic Liver Transplantation For Cirrhotic PatientsDocument5 pagesPortocaval Shunt Throughout Anhepatic Phase in Orthotopic Liver Transplantation For Cirrhotic PatientsHưng Nguyễn KiềuNo ratings yet
- Ureteroneocystostomy For Treatment of Struvite UroDocument4 pagesUreteroneocystostomy For Treatment of Struvite UroBright DerlacuzENo ratings yet
- PDF PreviewDocument9 pagesPDF PreviewSowmya ChitraNo ratings yet
- Wunderlich Syndrome Spontaneous Atraumatic Rupture of The KidneyDocument5 pagesWunderlich Syndrome Spontaneous Atraumatic Rupture of The KidneyqalbiNo ratings yet
- Nasser2015Document5 pagesNasser2015hengkileonardNo ratings yet
- Cirugi A Espan Ola: Meso-Cava Bypass As An Alternative To Multivisceral TransplantationDocument2 pagesCirugi A Espan Ola: Meso-Cava Bypass As An Alternative To Multivisceral TransplantationHưng Nguyễn KiềuNo ratings yet
- Ahn 2011Document4 pagesAhn 2011Residentes PediatríaNo ratings yet
- Complications of Percutaneous Nephrostomy Tube Placement To Treat NephrolithiasisDocument4 pagesComplications of Percutaneous Nephrostomy Tube Placement To Treat NephrolithiasisPande Made FitawijamariNo ratings yet
- Marion 2020Document7 pagesMarion 2020hezzaNo ratings yet
- Abdominopelvic Ectopic Spleen With A Comprehensive Imaging Examination: A Case ReportDocument6 pagesAbdominopelvic Ectopic Spleen With A Comprehensive Imaging Examination: A Case ReportceciliaNo ratings yet
- BRIEF CLINICAL OBSERVATIONS: Nondilated Obstructive Uropathy Due to a Ureteral CalculusDocument3 pagesBRIEF CLINICAL OBSERVATIONS: Nondilated Obstructive Uropathy Due to a Ureteral CalculusMuhammad Kholid FirdausNo ratings yet
- IVC Leiomyosarcoma Reconstruction Not Always RequiredDocument3 pagesIVC Leiomyosarcoma Reconstruction Not Always RequiredCirugía General Hospital de San JoséNo ratings yet
- Case Report Severe Dysplasia of Kidney 20082021Document15 pagesCase Report Severe Dysplasia of Kidney 20082021Nikko Caesario Mauldy SusiloNo ratings yet
- Trauma UretraDocument3 pagesTrauma UretraTita FadiahNo ratings yet
- Pediatric Bladder Injuries from Inguinal Canal SurgeryDocument4 pagesPediatric Bladder Injuries from Inguinal Canal SurgeryOscar Sanchez ParisNo ratings yet
- Review Syefira SalshabilaDocument2 pagesReview Syefira Salshabilaqueen TinaNo ratings yet
- Outcome of Septal Dermoplasty in Patients With Hereditary Hemorrhagic TelangiectasiaDocument5 pagesOutcome of Septal Dermoplasty in Patients With Hereditary Hemorrhagic TelangiectasiaalecsaNo ratings yet
- Crossed and Non-Fused Renal Ectopia of Inferior Type: G. J. Jorwekar, K. N. Dandekar, R. K. Shinde, P. K. BaviskarDocument3 pagesCrossed and Non-Fused Renal Ectopia of Inferior Type: G. J. Jorwekar, K. N. Dandekar, R. K. Shinde, P. K. BaviskarnaseebulNo ratings yet
- Total Laparoscopic Duodenopancreatectomy Case ReportDocument7 pagesTotal Laparoscopic Duodenopancreatectomy Case ReportIJAR JOURNALNo ratings yet
- Complication of Long Indwelling Urinary Catheter and StentDocument5 pagesComplication of Long Indwelling Urinary Catheter and StenteviltohuntNo ratings yet
- Undescended TestisDocument3 pagesUndescended TestisIoannis ValioulisNo ratings yet
- Jiang2018 2Document5 pagesJiang2018 2Anonymous Inj7eQNo ratings yet
- JCDR 9 PD26Document2 pagesJCDR 9 PD26ceciliaNo ratings yet
- 1 s2.0 S0022480423002895 MainDocument7 pages1 s2.0 S0022480423002895 Mainlucabarbato23No ratings yet
- Reconstruction of Late-Onset Transplant Ureteral Stricture DiseaseDocument7 pagesReconstruction of Late-Onset Transplant Ureteral Stricture DiseasetnsourceNo ratings yet
- Testicular Torsion in Undescended TestisDocument5 pagesTesticular Torsion in Undescended TestisjimNo ratings yet
- 279 285 1 SM PDFDocument6 pages279 285 1 SM PDFLainatussifah QamalNo ratings yet
- Quotation Letter Onkologi in Nov - Dec 2019-1Document4 pagesQuotation Letter Onkologi in Nov - Dec 2019-1Ikhdin SaadhiNo ratings yet
- Clinical Pathways for Rib FractureDocument1 pageClinical Pathways for Rib FractureIkhdin SaadhiNo ratings yet
- +++pappachan-Biomekanik MF Trauma PDFDocument7 pages+++pappachan-Biomekanik MF Trauma PDFmedicamedicaNo ratings yet
- Pain Management & Medicine: An Innovative Product For Pain Management: Proof From Clinical TrialDocument5 pagesPain Management & Medicine: An Innovative Product For Pain Management: Proof From Clinical TrialIkhdin SaadhiNo ratings yet
- Akomodasi SSF Rev6Document28 pagesAkomodasi SSF Rev6Ikhdin Saadhi0% (1)
- E019614 FullDocument7 pagesE019614 FullIkhdin SaadhiNo ratings yet
- Anggrek 1: Ruang PJ BED Nama Usia RM MRS Diagnosis Status Plan DPJP KeteranganDocument2 pagesAnggrek 1: Ruang PJ BED Nama Usia RM MRS Diagnosis Status Plan DPJP KeteranganIkhdin SaadhiNo ratings yet
- BTKV MappingDocument1 pageBTKV MappingIkhdin SaadhiNo ratings yet
- Traumatic Brain Injury and Treatment With Hypertonic Sodium Lactate. Will It Become The Best Management Alternative?Document15 pagesTraumatic Brain Injury and Treatment With Hypertonic Sodium Lactate. Will It Become The Best Management Alternative?Ikhdin SaadhiNo ratings yet
- 11 11 18-2Document4 pages11 11 18-2Ikhdin SaadhiNo ratings yet
- Neurofibromatosis Type I (NF1) : Presented by Lei DuDocument18 pagesNeurofibromatosis Type I (NF1) : Presented by Lei DuIkhdin SaadhiNo ratings yet
- Paper I Operative ConsultationDocument64 pagesPaper I Operative ConsultationIkhdin SaadhiNo ratings yet
- Vesicoureteral Reflux 508Document8 pagesVesicoureteral Reflux 508Ikhdin SaadhiNo ratings yet
- Ann Burns and Fire Disasters 27 209Document6 pagesAnn Burns and Fire Disasters 27 209Ikhdin SaadhiNo ratings yet
- Hirsch Pung SDocument10 pagesHirsch Pung Sotto naftariNo ratings yet
- CRG 0011 0755Document8 pagesCRG 0011 0755Ikhdin SaadhiNo ratings yet
- DSV Serial CaseDocument5 pagesDSV Serial CaseIkhdin SaadhiNo ratings yet
- VP ShuntDocument12 pagesVP ShuntBanni Aprilita PratiwiNo ratings yet
- AppendixDocument21 pagesAppendixIkhdin SaadhiNo ratings yet
- SICH Mgmt2Document9 pagesSICH Mgmt2Lennon Ponta-oyNo ratings yet
- 1501931700998Document26 pages1501931700998Ikhdin SaadhiNo ratings yet
- Neu 2014 3644Document12 pagesNeu 2014 3644Ikhdin SaadhiNo ratings yet
- 1501931700998Document26 pages1501931700998Ikhdin SaadhiNo ratings yet
- Ni Hms 865156Document8 pagesNi Hms 865156Ikhdin SaadhiNo ratings yet
- AppendixDocument21 pagesAppendixIkhdin SaadhiNo ratings yet
- Pi Is 0741521402753214Document3 pagesPi Is 0741521402753214Ikhdin SaadhiNo ratings yet
- L - GS PM 021415 Cohn PercutDocument9 pagesL - GS PM 021415 Cohn PercutIkhdin SaadhiNo ratings yet
- JSurgTechCaseReport411-2985968 081739Document5 pagesJSurgTechCaseReport411-2985968 081739Ikhdin SaadhiNo ratings yet
- Memory in AutismDocument384 pagesMemory in AutismkapsicumNo ratings yet
- Diacalauto en DT Rev03 0851501 Rev02Document8 pagesDiacalauto en DT Rev03 0851501 Rev02vijayramaswamy0% (1)
- Dexmedetomidine FAQDocument16 pagesDexmedetomidine FAQRoxana SurliuNo ratings yet
- Adult Early Warning Score Observation Chart For Cardiothoracic UnitDocument1 pageAdult Early Warning Score Observation Chart For Cardiothoracic UnitalexipsNo ratings yet
- Health Entrepreneurship in PakistanDocument44 pagesHealth Entrepreneurship in Pakistanusman-hbNo ratings yet
- Medical Mycology GuideDocument39 pagesMedical Mycology Guidehanny jammyNo ratings yet
- Yimi Catalogue2014Document60 pagesYimi Catalogue2014ariovaldofjNo ratings yet
- Assessing The Caring Behaviors of Critical Care Nurses PDFDocument9 pagesAssessing The Caring Behaviors of Critical Care Nurses PDFnasimhsNo ratings yet
- MiradryDocument4 pagesMiradryBarakat AyoubNo ratings yet
- Biology Terms Grade 9 ReviewerDocument3 pagesBiology Terms Grade 9 ReviewerGreta Uy Sevilla100% (1)
- The Pittston Dispatch 08-05-2012Document62 pagesThe Pittston Dispatch 08-05-2012The Times LeaderNo ratings yet
- 1891 Knowles Complete System of Personal InfluenceDocument154 pages1891 Knowles Complete System of Personal InfluenceJoão Marques Ferreira100% (3)
- Newborn Care Charts Guide Routine Care and ManagementDocument102 pagesNewborn Care Charts Guide Routine Care and ManagementM. KurnNo ratings yet
- Anatomy StomachDocument43 pagesAnatomy StomachBijo K BennyNo ratings yet
- Slide 11 DiagimgDocument39 pagesSlide 11 Diagimghayumbe08No ratings yet
- Teaching Practice.... Lung CancerDocument32 pagesTeaching Practice.... Lung CancernamitaNo ratings yet
- Estudo Hepasfera Versus BeadDocument6 pagesEstudo Hepasfera Versus BeadAlexandre Campos Moraes AmatoNo ratings yet
- Christa Maki Letter of Recommednation 4Document2 pagesChrista Maki Letter of Recommednation 4api-491578633No ratings yet
- English 7 1stQ ExamDocument5 pagesEnglish 7 1stQ ExamNoble MartinusNo ratings yet
- Jhonston Evaluation of Growth in Patients Belonging PetrovicsDocument12 pagesJhonston Evaluation of Growth in Patients Belonging PetrovicsMargarida Maria LealNo ratings yet
- GCSE Biology RevisionDocument2 pagesGCSE Biology RevisionsannnnnNo ratings yet
- Cupping The Great Missing Therapy (Dr. Sahbaa M. Bondok)Document240 pagesCupping The Great Missing Therapy (Dr. Sahbaa M. Bondok)Teerth KrishnanandNo ratings yet
- Click Here To Download Top 100 One Word Substitution As PDF FormatDocument3 pagesClick Here To Download Top 100 One Word Substitution As PDF FormatMrinmoy KoleyNo ratings yet
- Abdominal Distention inDocument45 pagesAbdominal Distention inArif Rahman DmNo ratings yet
- Gestational Diabetes Screening Case StudiesDocument50 pagesGestational Diabetes Screening Case Studiesdiabetes asia100% (1)
- Cost-Benefit Analysis Lesson PlanDocument2 pagesCost-Benefit Analysis Lesson PlanlaurahelenkingNo ratings yet
- Is There A Clinical Difference Between Salt Water and Fresh Water DrowningDocument2 pagesIs There A Clinical Difference Between Salt Water and Fresh Water DrowningSicilia Bunga Athifah ArnurNo ratings yet
- Herbst Appliance GuideDocument161 pagesHerbst Appliance GuideRajshekhar Banerjee100% (3)
- Shree Hospital: Bidar CT Scan Bidar CT Scan Bidar CT ScanDocument8 pagesShree Hospital: Bidar CT Scan Bidar CT Scan Bidar CT ScanhattisanjayNo ratings yet