Professional Documents
Culture Documents
Lumbar Disc Disease: The Natural History: N G. B, M.D
Uploaded by
AfonsoAragãoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lumbar Disc Disease: The Natural History: N G. B, M.D
Uploaded by
AfonsoAragãoCopyright:
Available Formats
Neurosurg Focus 13 (2):Article 2, 2002, Click here to return to Table of Contents
Lumbar disc disease: the natural history
NEVAN G. BALDWIN, M.D.
Texas Tech University Health Sciences Center, Lubbock, Texas
Symptomatic lumbar disc disease represents a major cost to societies providing modern care for these conditions.
The impact of any treatment cannot be assessed without an understanding of the natural history of the disease process.
The majority of individuals with degenerative disc disease are asymptomatic. Although the natural history of sciatica
is associated with a good overall prognosis, that of discogenic low-back pain is less promising. For patients with symp-
tomatic lumbar disc herniations, the results of discectomy are better than those predicted by the natural history of the
disease process.
KEY WORDS • lumbar spine • intervertebral disc • natural history • outcome
“Timing has an awful lot to do with the outcome of a rain dance.” Conventional Cowboy Wisdom
Symptomatic lumbar disc disease is responsible for a controversial. In numerous studies investigators have
tremendous cost to society. It is believed to be a major demonstrated that, during lumbar surgeries performed af-
contributor to the estimated 60 to 80% lifetime incidence ter administration of a local anesthesia, pressure to the
of low-back pain in the general population.8,24 The cost of anulus fibrosis results in low-back pain. Falconer, et al.,5
treatment for low-back pain in the United States alone is noted that the application of pressure to lumbar discs gen-
measured in 10s of billions of dollars per year.6 Patients erated low-back pain during such operations. Kuslich, et
with radiculopathy represent another large segment of the al.,14 were able to generate back pain similar to the preop-
population who consume care costs related to lumbar disc erative pain in 70% of the patients in a consecutive series
disease. Several relatively recent innovative technologies of 193 cases when stimulation was applied to the anulus
have been developed for the treatment of lumbar disc dis- fibrosis or the posterior longitudinal ligament.14 This pain
ease. As with most new technologies, there are associated response was blocked with the application of a local an-
costs. Although high-tech innovations may ultimately re- esthetic.
duce the cost of treating lumbar disc disease, the cost-re- The existence of discogenic back pain is perhaps the
lated advantage or disadvantage associated with these subject of the most controversy relating to the anatomical
technologies cannot be determined without a clear knowl- arguments for its presence. Opponents of the discogenic
edge of the natural history of the disease process. Apply- pain hypothesis have argued that because there are no pain
ing an expensive treatment to a disease that has a high receptors within the intervertebral discs, discogenic pain
likelihood of spontaneous improvement may well yield cannot occur. The presence of the sinuvertebral nerve to
results similar to those of a well-timed rain dance. the spinal canal was described in the 19th century.6 More
recent staining techniques, however, have allowed precise
anatomical description of this neurological structure.
LUMBAR DISC DISEASE AND LOW-BACK PAIN Groen, et al.,11 identified the sinuvertebral nerve as a de-
Whereas lower-extremity radicular pain is well accept- rivative of the rami communicantes arising as a postgan-
ed as a symptom of lumbar disc disease, the role of disc glionic structure branching into segments ending in the
disease as a cause of nonradicular back pain remains more posterior longitudinal ligament and the outer lamina of the
anulus fibrosis. Arguments for the existence of discogenic
low-back pain are therefore supported by both empirical
Abbreviation used in this paper: MR = magnetic resonance. clinical data and neuroanatomical research.
Neurosurg. Focus / Volume 13 / August, 2002 1
N. G. Baldwin
Natural History or posterlateral aspect of the disc. Posterior protrusion
Although lumbar disc disease may well be a cause of may be visualized as a bulging disc or, if the outer fibers
low-back pain, it is important to note that disc degenera- of the anulus are penetrated, as an extruded disc. The
tion can occur in the absence of back pain or any other phenomenon, when it occurs in conjunction with clinical
symptoms. Paajanen, et al.,20 found that in 35% of healthy symptoms, most commonly occurs in individuals between
male volunteers significant disc degeneration was demon- the ages of 30 and 50 years.26 Although it is seen in both
strated on MR imaging. In a series of 600 autopsy speci- younger and older individuals, acute disc herniation is far
mens, Miller, et al.,17 showed that 90% of all lumbar discs less commonly observed in these populations. There is no
had evidence of degeneration in individuals by the age of definitive information regarding the incidence or preva-
50 years. The presence of disc degeneration and the pres- lence of disc herniations in a sizable population that would
ence or absence of low-back pain may be considered anal- define the norm. Risk factors for disc herniation include
ogous to the occurrence of gallstones and abdominal pain. driving of motor vehicles, sedentary occupation, vibra-
Although most individuals with gallstones are asympto- tion, smoking, previous full-term pregnancy, physical in-
matic, if a patient has gallstones and the appropriate symp- activity, increased body mass, and a tall stature.19,26 With
toms, those symptoms may be attributed to the gallstones. regard to occupations that require strength, it has been
Although low-back pain results in significant disability, shown that an increasing degree of disparity between the
95% of these patients return to their previous employment strength required and the strength of the individual results
within 3 months of symptom onset.6 Failure to return to in higher rates of symptomatic low-back injury.4,12
work within 3 months may be considered a poor prog- Preventative efforts in lumbar disc disease, other than
nostic sign. In patients who experience total disability by modification of the aforementioned risk factors, have
after 1 year, the likelihood of returning to work is less than not been successful. Intuitively, one might assume that
20%. After 2 years of disability, the probability of return- physical fitness would be preventative with regard to disc
ing to work is less than 2%.1 rupture. Although the literature on this topic is not entire-
Numerous imaging studies have demonstrated that with ly uniform in opinion, the strongest evidence probably
nonsurgical treatment lumbar disc herniations will subside suggests that physical fitness does little to protect or pro-
over time in the majority of cases.2,13,23 In a series of 32 voke attacks of sciatica. Physical fitness, however, likely
patients studied with serial MR imaging, Matsubara, et is advantageous as a factor affecting rehabilitation after
al.,15 found regression of disc herniations in 62%. They disc surgery.25
also demonstrated that the more degeneration seen ini- It is well supported by clinical evidence that sciatica can
tially in the discs, and the larger the initial herniation, the be managed by lumbar surgery.10,16 The early recovery rate
more the size of the herniated disc fragment was observed and the rate of return to work are improved following sur-
to decrease. gical intervention. Postoperatively, recovery of the effer-
Although degenerative disc disease is common in ent conduction system is considerably better than that seen
asymptomatic populations, large compressive lesions are in the afferent portion.
uncommon. Patients with large compressive lesions are The mechanism for radiculopathy-related pain produc-
also generally believed to be more ideally suited to surgi- tion has been a subject of considerable debate. Compres-
cal intervention. These same patients, however, are those sion of the nerve has been shown to create edema forma-
most likely to experience spontaneous regression of their tion and eventually lead to intraneural inflammation and
lesions and they have a high rate of clinical improvement hypersensitivity.21 This then results in increased mechan-
with noninvasive treatments.23 osensitivity of the nerve root with regard to compression
Clinical improvement following a symptomatic lumbar and the induction of pain. It is now generally accepted that
disc herniation does not necessarily correlate with the a combination of mechanical and abnormal biochemical
radiographically documented resolution of the herniation. events is involved in the generation of radicular pain.22
Fraser, et al.,7 performed a study in which they examined It has been shown that most patients hospitalized for
the MR imaging findings in patients who had undergone sciatica will have suffered their first episode of acute low-
treatment for lumbar disc herniation 10 years earlier. back pain while in their third decade of life.25 The initial
Approximately one third of these patients had undergone episode is usually provoked by an acute traumatic event.
a saline injection as a control treatment for the study of An approximate mean of 10 years will pass before the
chymopapain as a treatment for lumbar disc herniation. onset of the first radicular symptoms. Weber25 attributed
Overall, a persistent herniated disc was found in 37%, and this long interval between onset of low-back pain and the
the incidence of persistent herniation was similar in pa- onset of radicular pain to intradiscal degeneration and re-
tients treated with chymopapain, surgery, or saline injec- generation forces. Weber and colleagues27 were also able
tion. Interestingly, the presence or absence of persistent to demonstrate improvement over the course of 4 weeks
disc herniation had no significant bearing on outcome. in 70% of their 208 nonhospitalized patients with sciatica
Analysis of their findings indicated that long-term im- in whom nonsurgical intervention was performed. Sixty
provement of symptoms after treatment of a disc her- percent of those patients returned to work by the 4-week
niation may occur with or without resolution of the herni- interval.
ated disc. Saal, et al.,23 reported on a series of 64 patients with ver-
The term "disc herniation" in this article refers to a pro- ified herniated lumbar discs who received nonsurgical
cess in which there has been rupture of the anulus fibers treatment during a 1-year period. Treatments included
and subsequent displacement of the central mass of the epidural steroid injection as well as oral steroid therapy,
disc in the intervertebral space, common to the posterior transcutaneous electrical nerve stimulation, acupuncture,
2 Neurosurg. Focus / Volume 13 / August, 2002
Natural history of lumbar disc disease
exercises, and physical therapy modalities, in addition to shown that for the best results, surgery should be per-
nonsteroidal antiinflammatory drugs. In that 1-year trial, formed preferably within the first 3 months of the onset of
satisfactory recovery was demonstrated in 90% of the pa- sciatica. The value of repeated surgery for persistent ra-
tients. diculopathy after an initial operation is usually question-
Bush, et al.,3 reported on 165 consecutive patients (mean able. Nachemson18 reported that only 25% of patients
age 41 years) who suffered sciatica due to lumbosacral undergoing revision surgery experienced any improve-
nerve root compression. The patients were treated primar- ment within a 3-year follow-up period. Nachemson rec-
ily with epidural steroid injections and local anesthetics. ommended repeated surgery only if a new disc herniation
All but 23 of these patients (14%) experienced satisfacto- was demonstrated. In patients suffering low-back pain
ry clinical recovery at 1 year. Those 23 patients in whom and/or sciatica for more than 6 months, the likelihood of
no improvement occurred underwent decompressive successful rehabilitation is only approximately 40%.
surgery. Although the use of epidural steroid injections to An evidence-based review of the existing data on the
treat acute radiculopathy and/or acute low-back pain is surgical treatment of lumbar disc disease supports the use
somewhat controversial, there is evidence to suggest that of discectomy in carefully selected patients with sciatica
a favorable effect is more likely when its used to treat pa- due to lumbar disc herniation.9,10 Discectomy has been
tients with acute onset of symptoms. shown to provide faster relief from the acute attack, al-
In the aforementioned studies, the authors obtained though the effect of surgery, positive or negative, on the
excellent results with nonsurgical interventions. In fact, lifetime natural history of disc disease remains unclear.
those results are so good that one would be hard pressed There is evidence of moderate scientific quality that the
to suggest that surgery could improve upon such impres- clinical outcomes of microdiscectomy are comparable
sive rates of satisfactory outcome. In controlled trials in with those of standard discectomy.9,10,16 There is moderate
which patients were randomized to surgical and nonsurgi- evidence that automated percutaneous discectomy pro-
cal treatment groups, however, surgery has been shown to duces poorer clinical results than standard discectomy or
be advantageous.25–27 chemonucleolysis.9,10 There is suitable evidence to under-
It has long been accepted that there are definite indica- score that discectomy (or microdiscectomy) affects the
tions for surgical intervention. These include the cauda disease outcome in a manner that exceeds the expected
equina syndrome, progressive loss of motor strength, and outcomes associated with the natural history alone.9,10
severe intractable pain. The empirically observed rates of
halting disease progression in cases in which these indica-
References
tions exist is so good that, given such symptoms, random-
ized clinical trials would be unethical. Such patients, how- 1. Andersson GB, Svensson HO, Oden A: The intensity of work
ever, represent a minority of the lumbar disc herniation recovery in low back pain. Spine 8:880–884, 1983
population and study of the far larger group who are less 2. Boos N, Semmer N, Elfering A, et al: Natural history of indi-
symptomatic is therefore warranted. Weber25 reported on viduals with asymptomatic disc abnormalities in magnetic res-
herniated lumbar discs in 208 patients among whom 126 onance imaging: predictors of low back pain-related medical
were incapacitated by sciatica but in whom indications for consultation and work incapacity. Spine 25:1484–1492, 2000
3. Bush K, Cowan N, Katz DE, et al: The natural history of sci-
surgery were believed to be uncertain. This subgroup was atica associated with disc pathology. A prospective study
therefore randomized to surgical and nonsurgical treat- with clinical and independent radiologic follow-up. Spine 17:
ment for purposes of comparison. The patients were then 1205–1212, 1992
followed for a 10-year period postoperatively.25 In this 4. Chaffin DB: Manual materials handling: the cause of over-exer-
controlled prospective randomized trial Weber found a tion injury and illness in industry. J Environ Pathol Toxicol
statistically significant improvement at 1 year in cases in 2:31–66, 1979
which surgery was performed. Ninety percent of those 5. Falconer MA, McGeorge M, Begg AC: Cause and mechanism
patients who had undergone surgery reported a good out- of symptom-production in sciatica and low-back pain. J Neurol
come compared with 60% in the control group. Seventeen Neurosurg Psychiatry 11:13–26, 1948
patients in the control group had also undergone surgery 6. Fischgrund JS, Montgomery DM: Diagnosis and treatment of
discogenic low back pain. Orthop Rev 22:311–318, 1993
for persistent or worsening pain. After 4 years, the sur- 7. Fraser RD, Sandhu A, Gogan WJ: Magnetic resonance imaging
gery-treated patients continued to experience better results findings 10 years after treatment for lumbar disc herniation.
than those in the control group. At the 4-year interval, the Spine 20:710–714, 1995
differences were not statistically significant. At 10 years 8. Frymoyer JW, Cats-Baril WL: An overview of the incidences
posttreatment, results in the groups were essentially iden- and costs of low back pain. Orthop Clin North Am 22:
tical. Motor deficits in both groups resolved nearly com- 263–271, 1991
pletely. More than one third of the patients suffered per- 9. Gibson JN, Grant IC, Waddell G: The Cochrane review of sur-
sistent sensory deficits at the conclusion of the study. A gery for lumbar disc prolapse and degenerative lumbar spondy-
key finding was also that in patients in whom symptoms losis. Spine 24:1820–1832, 1999
10. Gibson JNA, Grant IC, Waddell G: Surgery for lumbar disc
persisted for more than 3 months preoperatively, a far prolapse (Cochrane Review), in The Cochrane Library, issue
worse prognosis was demonstrated. 2. Oxford: Update Software, 2002
11. Groen GJ, Baljet B, Drukker J: Nerves and nerve plexuses of
the human vertebral column. Am J Anat 188:282–296, 1990
CONCLUSIONS 12. Keyserling WM: Strength testing as a method of evaluating
ability to perform strenuous work, in Stanton-Hicks M, Boas
A few tenets of surgical treatment of lumbar disc dis- RA (eds): Chronic Low Back Pain. New York: Raven Press,
ease are well supported by multiple studies. It has been 1982, pp 149–156
Neurosurg. Focus / Volume 13 / August, 2002 3
N. G. Baldwin
13. Komori H, Shinomiya K, Nakai O, et al: The natural history An experimental study of the pig cauda equina. Spine 16:
of herniated nucleus pulposus with radiculopathy. Spine 21: 487–493, 1991
225–229, 1996 22. Saal JA: Natural history and nonoperative treatment of lumbar
14. Kuslich SD, Ulstrom C, Michael CJ: The tissue origin of low disc herniation. Spine 21 (Suppl 24):2S–9S, 1996
back pain and sciatica: a report of pain response to tissue stim- 23. Saal JA, Saal JS, Herzog RJ: The natural history of lumbar
ulation during operations on the lumbar spine using local anes- intervertebral disc extrusions treated nonoperatively. Spine 15:
thesia. Othop Clin North Am 22:181–187, 1991 683–686, 1990
15. Matsubara Y, Kato F, Mimatsu K, et al: Serial changes on MRI 24. van Dieen JH, Weinans H, Toussaint HM: Fractures of the lum-
in lumbar disc herniations treated conservatively. Neuroradiol- bar vertebral endplate in the etiology of low back pain: a hy-
ogy 37:378–383, 1995 pothesis on the causative role of spinal compression in aspecif-
16. McCulloch JA: Focus issue on lumbar disc herniation: macro- ic low back pain. Med Hypotheses 53:246–252, 1999
and microdiscectomy. Spine 21 (Suppl 24):45S–56S, 1996 25. Weber H: Lumbar disc herniation. A controlled, prospective
17. Miller JA, Schmatz C, Schultz AB: Lumbar disc degeneration: study with ten years of observation. Spine 8:131–140, 1983
correlation with age, sex, and spine level in 600 autopsy speci- 26. Weber H: The natural history of disc herniation and the influ-
mens. Spine 13:173–178, 1988 ence of intervention. Spine 19:2233–2238, 1994
18. Nachemson AL: Advances in low-back pain. Clin Orthop 200: 27. Weber H, Holme I, Amlie E: The natural course of acute sciat-
266–278, 1985 ica with nerve root symptoms in a double-blind placebo-con-
19. Nachemson AL: Prevention of chronic back pain. The ortho- trolled trial evaluating piroxicam. Spine 18:1433–1438, 1993
paedic challenge for the 80's. Bull Hosp Jt Dis Orthop Inst
44:1–15, 1984
20. Paajanen H, Erkintalo M, Kuusela T, et al: Magnetic resonance Manuscript received July 8, 2002.
study of disc degeneration in young low-back pain patients. Accepted in final form July 23, 2002.
Spine 14:982–985, 1989 Address reprint requests to: Nevan G. Baldwin, M.D., Texas
21. Rydevik BL, Pedowitz RA, Hargens AR, et al: Effects of acute, Tech University Medical Office Plaza, 3502 9th Street, Suite 240,
graded compression on spinal nerve root function and structure. Lubbock, Texas 79407. email: nevan3@cox.net.
4 Neurosurg. Focus / Volume 13 / August, 2002
You might also like
- Lumbar Disc HerniationDocument7 pagesLumbar Disc HerniationkairalmurielNo ratings yet
- Discogenic LBP Revised September 2017Document13 pagesDiscogenic LBP Revised September 2017Clinton Franda Markus SitanggangNo ratings yet
- Herniated Lumbar Intervertebral Disk: Epidemiology and Natural HistoryDocument6 pagesHerniated Lumbar Intervertebral Disk: Epidemiology and Natural HistoryGeysel SuarezNo ratings yet
- Bydon 2019Document6 pagesBydon 2019julyanetorquatoNo ratings yet
- Baastrup's Disease: A Comprehensive Review of The Extant LiteratureDocument4 pagesBaastrup's Disease: A Comprehensive Review of The Extant LiteratureAlicja PopielNo ratings yet
- Lumbar Degenerative Disk Disease - StatPearls - NCBI BookshelfDocument6 pagesLumbar Degenerative Disk Disease - StatPearls - NCBI BookshelfAhmad SyahmiNo ratings yet
- HDL Management ConservatorDocument8 pagesHDL Management ConservatorCoLd AasdNo ratings yet
- Treatment of Lumbar Disc Herniation Evidence-Based PDFDocument6 pagesTreatment of Lumbar Disc Herniation Evidence-Based PDFAnastasya FannyNo ratings yet
- Whiplash Associated DisordersDocument12 pagesWhiplash Associated DisorderspuchioNo ratings yet
- Lumbar Disk HerniationDocument6 pagesLumbar Disk HerniationSyarifah Nadya ArfadNo ratings yet
- Chaptar 30 Degenerative Spine DiseaseDocument9 pagesChaptar 30 Degenerative Spine DiseaseAbraham SaldañaNo ratings yet
- 2019 Estado de La Unión. Revisión de Las Indicaciones y Técnicas de Fusión Lumbar para La Enfermedad Degenerativa de La ColumnaDocument14 pages2019 Estado de La Unión. Revisión de Las Indicaciones y Técnicas de Fusión Lumbar para La Enfermedad Degenerativa de La Columnajuan pabloNo ratings yet
- Genicular Nerve Ablation Zeitlinger2019Document7 pagesGenicular Nerve Ablation Zeitlinger2019drjorgewtorresNo ratings yet
- Vertebral Fractures: Clinical PracticeDocument9 pagesVertebral Fractures: Clinical PracticeIndraYudhiNo ratings yet
- Laminectomy With Fusion Versus Young LaminoplastyDocument6 pagesLaminectomy With Fusion Versus Young Laminoplasty7w7dzjhgbqNo ratings yet
- Management of Degenerative Lumbar Spinal Stenosis in The ElderlyDocument7 pagesManagement of Degenerative Lumbar Spinal Stenosis in The ElderlySandroNo ratings yet
- ScoliosisDocument8 pagesScoliosisLusian VissNo ratings yet
- Degenerative Lumbar Spinal Stenosis: Evaluation and ManagementDocument9 pagesDegenerative Lumbar Spinal Stenosis: Evaluation and ManagementVy Phạm Thị TrúcNo ratings yet
- A Longitudinal Study of Back Pain and RadiologicalDocument5 pagesA Longitudinal Study of Back Pain and RadiologicalSumanta KamilaNo ratings yet
- Conferences and Reviews: Cervical SpondylosisDocument9 pagesConferences and Reviews: Cervical SpondylosisPrasanna GallaNo ratings yet
- Management of Degenerative Cervical Disc DiseaseDocument8 pagesManagement of Degenerative Cervical Disc DiseasefromneptuneNo ratings yet
- Maus 2012Document29 pagesMaus 2012211097salNo ratings yet
- Neuroimaging of Spinal Canal StenosisDocument17 pagesNeuroimaging of Spinal Canal Stenosisrulitoss_41739No ratings yet
- 1 s2.0 S2255497115302111 MainDocument6 pages1 s2.0 S2255497115302111 MainkkkjaegiNo ratings yet
- Treatment of Central Cord Syndrome Without Associated Spinal InstabilityDocument5 pagesTreatment of Central Cord Syndrome Without Associated Spinal Instabilityfori:=1tondoNo ratings yet
- Cervical Radiculopathy: Sravisht Iyer Han Jo KimDocument8 pagesCervical Radiculopathy: Sravisht Iyer Han Jo KimMatias ChandiaNo ratings yet
- El Borno FusionDocument112 pagesEl Borno FusionneareastspineNo ratings yet
- Volume 08 04 Lumbar Instability From DDDDocument7 pagesVolume 08 04 Lumbar Instability From DDDcarrotbutterNo ratings yet
- Diare AnakDocument6 pagesDiare AnakVictoria HusadaniNo ratings yet
- HNPDocument7 pagesHNPDennyNo ratings yet
- Lumbar Degenerative Disease BackgroundDocument8 pagesLumbar Degenerative Disease BackgroundWilyanto YangNo ratings yet
- Original Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global OutcomeDocument6 pagesOriginal Paper: Lumbar Disk Herniations - Clinical Status, Diagnosis, Imaging, Surgical Treatment and Global Outcomeasep budiyantoNo ratings yet
- Degenerative Disc Disease by Dr. BBTDocument11 pagesDegenerative Disc Disease by Dr. BBTBhusan TamrakarNo ratings yet
- Ste I Ndler 1938Document8 pagesSte I Ndler 1938Roy Mtz PageNo ratings yet
- Ankylosing Spondylitis BMJ RevDocument5 pagesAnkylosing Spondylitis BMJ RevsamarqandiNo ratings yet
- Scaitic Treatment PDFDocument5 pagesScaitic Treatment PDFSebastiano SerraNo ratings yet
- A Retrospectie Study of Cranial Strain Patterns in Patients With Idiopathic Parkinson's DiseaseDocument6 pagesA Retrospectie Study of Cranial Strain Patterns in Patients With Idiopathic Parkinson's DiseaserafaelNo ratings yet
- IndianJClinAnaesth 9 3 374 378Document5 pagesIndianJClinAnaesth 9 3 374 378bhaskaracharya dontabhaktuniNo ratings yet
- Craniocervical Instability in Patients With Hypermobility Connective Disorders 2165 7939 1000299 PDFDocument3 pagesCraniocervical Instability in Patients With Hypermobility Connective Disorders 2165 7939 1000299 PDFATRAGENo ratings yet
- Rotator Cuff TendinopathyDocument7 pagesRotator Cuff TendinopathyMarcus Dos SantosNo ratings yet
- Volume: 03 Issue: 03 - May-Jun 2022Document4 pagesVolume: 03 Issue: 03 - May-Jun 2022Central Asian StudiesNo ratings yet
- Cervical Spondylotic Myelopathy: Aditya Iyer, MD, MS, Tej D. Azad, Ba, and Suzanne Tharin, MD, PHDDocument7 pagesCervical Spondylotic Myelopathy: Aditya Iyer, MD, MS, Tej D. Azad, Ba, and Suzanne Tharin, MD, PHDMây Trên TrờiNo ratings yet
- Adhesive Capsulitis: Use The Evidence To Integrate Your InterventionsDocument8 pagesAdhesive Capsulitis: Use The Evidence To Integrate Your InterventionsAndra DorobeicaNo ratings yet
- 1 s2.0 S1529943010003062 MainDocument7 pages1 s2.0 S1529943010003062 Main阮威勝No ratings yet
- Spontaneous Regression of A Large Lumbar Disc Extrusion: WWW - Jkns.or - KRDocument3 pagesSpontaneous Regression of A Large Lumbar Disc Extrusion: WWW - Jkns.or - KRAntonius YansenNo ratings yet
- The Treatment of Neck and Upper Back Pain With AcuDocument6 pagesThe Treatment of Neck and Upper Back Pain With AcuMohmmad Hossein NazariNo ratings yet
- Cervical RadiculopathyDocument7 pagesCervical Radiculopathyrhymescsf100% (1)
- Trauma of The Coccyx and CoccygodyniaDocument4 pagesTrauma of The Coccyx and CoccygodyniaTefera LeteboNo ratings yet
- Pathologic Basis of Lumbar Radicular Pain: BackgroundDocument8 pagesPathologic Basis of Lumbar Radicular Pain: BackgroundVizaNo ratings yet
- Spontaneous Regression of A Large Lumbar Disc Extrusion: WWW - Jkns.or - KRDocument3 pagesSpontaneous Regression of A Large Lumbar Disc Extrusion: WWW - Jkns.or - KRenglish-exactlyNo ratings yet
- Capsulitis Adhesiva PDFDocument14 pagesCapsulitis Adhesiva PDFErika LópezNo ratings yet
- Tendon InterventionDocument10 pagesTendon InterventionVerónica Téllez ArriagaNo ratings yet
- PLDD Lumbar Radicular Pain DR RadosDocument7 pagesPLDD Lumbar Radicular Pain DR RadosYAŞAR TÜRKNo ratings yet
- SpineMED White PaperDocument9 pagesSpineMED White PaperGhita DanielNo ratings yet
- Lumbar Spinal Stenosis: Devin K. Binder, M.D., PH.D, Meic H. Schmidt, M.D., and Philip R. Weinstein, M.DDocument10 pagesLumbar Spinal Stenosis: Devin K. Binder, M.D., PH.D, Meic H. Schmidt, M.D., and Philip R. Weinstein, M.DYerni DaeliNo ratings yet
- Durerea Vertebrogenă PUBMEDDocument4 pagesDurerea Vertebrogenă PUBMEDIulia MoldovanNo ratings yet
- South African Medical Journal Suid, Afrikaanse Tydskrif Vir GeneeskundeDocument3 pagesSouth African Medical Journal Suid, Afrikaanse Tydskrif Vir GeneeskundeniluhayusumbawatiNo ratings yet
- Management of Lumbar Spinal Stenosis 2016Document13 pagesManagement of Lumbar Spinal Stenosis 2016Bruno HazlebyNo ratings yet
- (10920684 - Neurosurgical Focus) Incidental Vertebral LesionsDocument9 pages(10920684 - Neurosurgical Focus) Incidental Vertebral LesionsRJ HSNo ratings yet
- Operative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesFrom EverandOperative Brachial Plexus Surgery: Clinical Evaluation and Management StrategiesAlexander Y. ShinNo ratings yet
- Carnegie Mellon Thesis RepositoryDocument4 pagesCarnegie Mellon Thesis Repositoryalisonreedphoenix100% (2)
- Boundary Value Analysis 2Document13 pagesBoundary Value Analysis 2Raheela NasimNo ratings yet
- CBC Heo (Wheel Loader) NC IIDocument58 pagesCBC Heo (Wheel Loader) NC IIJohn JamesNo ratings yet
- Total Physical Response (G4)Document3 pagesTotal Physical Response (G4)Aq Nadzrul LarhNo ratings yet
- Institutional Group Agencies For EducationDocument22 pagesInstitutional Group Agencies For EducationGlory Aroma100% (1)
- FMEA Minus The PainDocument7 pagesFMEA Minus The PainMUNISNo ratings yet
- Invisible CitiesDocument14 pagesInvisible Citiesvelveteeny0% (1)
- Inspección, Pruebas, Y Mantenimiento de Gabinetes de Ataque Rápido E HidrantesDocument3 pagesInspección, Pruebas, Y Mantenimiento de Gabinetes de Ataque Rápido E HidrantesVICTOR RALPH FLORES GUILLENNo ratings yet
- W.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueDocument2 pagesW.C. Hicks Appliances: Client Name SKU Item Name Delivery Price Total DueParth PatelNo ratings yet
- SIVACON 8PS - Planning With SIVACON 8PS Planning Manual, 11/2016, A5E01541101-04Document1 pageSIVACON 8PS - Planning With SIVACON 8PS Planning Manual, 11/2016, A5E01541101-04marcospmmNo ratings yet
- Imabalacat DocuDocument114 pagesImabalacat DocuJänrëýMåmårìlSälängsàngNo ratings yet
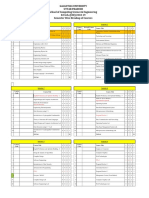
- Galgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesDocument2 pagesGalgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesRohit Singh BhatiNo ratings yet
- 18 Composition Rules For Photos That ShineDocument20 pages18 Composition Rules For Photos That Shinemahfuzkhan100% (1)
- Noise and DB Calculations: Smart EDGE ECE Review SpecialistDocument2 pagesNoise and DB Calculations: Smart EDGE ECE Review SpecialistLM BecinaNo ratings yet
- Grade 7 Nap MayDocument6 pagesGrade 7 Nap Mayesivaks2000No ratings yet
- Five Reasons Hazards Are Downplayed or Not ReportedDocument19 pagesFive Reasons Hazards Are Downplayed or Not ReportedMichael Kovach100% (1)
- (Sat) - 072023Document7 pages(Sat) - 072023DhananjayPatelNo ratings yet
- Data MiningDocument28 pagesData MiningGURUPADA PATINo ratings yet
- I. Learning Objectives / Learning Outcomes: Esson LANDocument3 pagesI. Learning Objectives / Learning Outcomes: Esson LANWilliams M. Gamarra ArateaNo ratings yet
- NAV SOLVING PROBLEM 3 (1-20) .PpsDocument37 pagesNAV SOLVING PROBLEM 3 (1-20) .Ppsmsk5in100% (1)
- Literature Review Template DownloadDocument4 pagesLiterature Review Template Downloadaflsigfek100% (1)
- Img 20150510 0001Document2 pagesImg 20150510 0001api-284663984No ratings yet
- Isi Rumen SBG Subtitusi HijauanDocument3 pagesIsi Rumen SBG Subtitusi HijauanBagas ImamsyahNo ratings yet
- SP-Chapter 14 PresentationDocument83 pagesSP-Chapter 14 PresentationLoiDa FloresNo ratings yet
- Victor 2Document30 pagesVictor 2EmmanuelNo ratings yet
- D25KS Sanvick PDFDocument4 pagesD25KS Sanvick PDFJiménez Manuel100% (1)
- Tutorial Chapter 5 - Power System ControlDocument2 pagesTutorial Chapter 5 - Power System ControlsahibNo ratings yet
- UNIT 5-8 PrintingDocument17 pagesUNIT 5-8 PrintingNOODNo ratings yet
- 2 Design of DOSAGE DESIGNDocument16 pages2 Design of DOSAGE DESIGNMarjo100% (1)
- PDFDocument3 pagesPDFAhmedraza123 NagdaNo ratings yet