Professional Documents
Culture Documents
Folic Acid 2004 PDF
Uploaded by
naira9valentina9pareOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Folic Acid 2004 PDF
Uploaded by
naira9valentina9pareCopyright:
Available Formats
April 2005 䡠 Vol. 7 䡠 No.
4 ACMG practice guideline
Folic acid and neural tube defects
Helga V. Toriello, PhD, for the Professional Practice and Guidelines Committee
Key Words: folic acid supplementation, neural tube defects, prenatal diet, congenital anomalies
Major congenital anomalies occur in 2% to 3% of live births. nancies are unplanned, NTD prevention is best achieved by
Neural tube defects (NTDs), cleft lip and palate, and cardiac adequate daily folic acid intake throughout the reproductive
anomalies are some of the most common. NTDs are a group of years.
serious birth defects that affect the developing nervous system Women without a prior history of a NTD should ingest 400
and include anencephaly, spina bifida, and encephalocele. g (0.4 mg) of folic acid each day throughout their reproduc-
Birth records suggest that about 2500 babies with these birth tive years, either as a supplement, in a multivitamin, from
defects, or 1 to 2 per 1000, are born each year in the United foods fortified with folic acid, or a combination of these.13
States. Some affected pregnancies are spontaneously or elec- Available reports suggest that 400 g (0.4 mg) is sufficient to
tively aborted. Over 95% occur to women without a prior fam- cause a substantial reduction of NTDs (40%– 80%, dependent
ily history of this disorder. Neural tube defects occur within 1 on background NTD prevalence).8 While it is possible for
month of conception. Anencephaly and spina bifida are the women to increase their consumption of dietary folates by
most common NTDs and occur with about equal frequency, careful selection of foods, food folates are about half as bio-
whereas encephalocele is seen less frequently. In anencephaly, available as synthetic folic acid. Fortification of staple food
there is partial or complete absence of the skull bones usually products with synthetic folic acid is an effective and inexpen-
with a remnant of brain: it is almost always fatal before or sive approach to increasing overall folic acid intake without the
shortly after birth. Spina bifida with meningomyelocele results need for behavior change. Women are continuing to eat the
from failure of the vertebral arches to close over an open neural foods they have always eaten (unless they choose to follow
tube defect, exposing the spinal cord and nerves. Although certain low carbohydrate diets), but are now receiving the ben-
most cases of spina bifida are open, 10% to 15% are closed or efits of folic acid that has been added to these foods. In 1998,
covered by skin. Spina bifida is compatible with survival al- the Food and Drug Administration mandated the fortification
though in most cases individuals have moderate to severe dis- of enriched cereal grain flours with 140 g synthetic folic acid
abilities and, in some cases, may have mental retardation. With per 100 grams of grain. Studies show that after fortification,
encephalocele there is protrusion of the brain and/or its cov- prevalence of spina bifida decreased by 31%, and prevalence of
ering membranes through the skull, most often in the occipital anencephaly decreased by 16%.14 Although this is a step for-
region. ward, the actual amount added may not be sufficient to protect
Folic acid supplementation has been shown to reduce the against all folic acid-preventable NTDs. For women who have
incidence and recurrence of NTDs and possibly reduce the had a prior pregnancy with a NTD, following the report of the
occurrence of several other birth defects such as cardiac, oro- British MRC Vitamin Study,10 the Centers for Disease Control
facial, limb, and renal anomalies (see References1,2). For recommended supplementation with 4 mg of folate daily be-
women without a prior history of NTDs, 4 of 5 studies reported ginning at least one month before conception.15
decreases of 40% to 100% if folic acid was taken on a daily Although Vitamin B12 deficiency is rare in women and chil-
basis.3– 8 For women with a prior history of NTDs, all published dren, there is concern that folic acid dosages exceeding 1000 g
studies reported a similar reduction after folic acid supplemen- (1.0 mg) per day may hinder the diagnosis of this condition,
tation.9 –12 The dose of folic acid, either alone or part of a mul- thereby allowing any neurological symptoms to progress to
tivitamin preparation, varied between 400 to 5000 g (0.4 –5 irreversible deficits. For most women, the recommended
mg) per day and was taken at least 1 month before conception amounts of folic acid obtained from folic acid supplements
and throughout the first trimester. Because neural tube closure and food fortification are unlikely to exceed the 1000 g per
occurs within the first 28 days after conception, which is often day. Cumulative effects are unlikely since folic acid is highly
before the recognition of pregnancy, and because many preg- water soluble and is rapidly excreted.
Because the American College of Medical Genetics (ACMG)
Helga V. Toriello, PhD, Spectrum Health, Grand Rapids, Michigan. is committed to the prevention of congenital anomalies, we
American College of Medical Genetics, 9650 Rockville Pike, Bethesda, MD 20914-3998. support the following recommendations:
Approved by the ACMG Board of Directors October 26, 2004.
This statement supersedes the statements entitled “Folic Acid and Pregnancy” (1994) and (1) Women capable of becoming pregnant should take 400
“Folic Acid: Statement on Fortification and Supplementation” (1997). g (0.4 mg) of folic acid daily, in the form of a supple-
Go to www.geneticsinmedicine.org for a printable copy of this document. ment, multivitamin, and/or through fortified foods, in
See disclaimer at the end of this article addition to eating a healthy diet. This is particularly
Genetics IN Medicine 283
Toriello
important before conception and through the first tri- 6. Milunsky A, Jick H, Jick SS, Bruell CL, MacLaughlin DS, Rothman KJ, Willett W.
Multivitamin/folic acid supplementation in early pregnancy reduces the prevalence
mester of pregnancy. of neural tube defects. JAMA 1989;262:2847–2852.
(2) Women who have had a prior NTD-affected pregnancy, 7. Czeizel A, Dudas I. Prevention of first occurrence of neural tube defects by pericon-
who have a first-degree relative with a NTD, or who are ceptional vitamin supplementation. N Engl J Med 1992;327:1831–1835.
themselves affected should consult with their physicians 8. Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H et al. Prevention of neural-tube
defects with folic acid in China: China-U.S. Collaborative Project for Neural Tube
before becoming pregnant. They should obtain genetic Defect Prevention. N Engl J Med 1999;341:1485–1490.
counseling concerning their occurrence or recurrence 9. Laurence KM, James N, Miller MH, Tennant GB, Campbell H. Double-blind ran-
risks, pregnancy management, and the appropriate folic domized controlled trial of folate treatment before conception to prevent recurrence
acid intake for them. They may be advised to take 4000 of neural-tube defects. Br Med J 1981;282:1509 –1511.
10. Medical Research Council Vitamin Study Research Group. Prevention of neural
g (4.0 mg) of folic acid daily starting at least 1 month tube defects: results of the Medical Research Council Vitamin Study. Lancet 1991;
and preferably 3 months before conception. 338: 131–137.
(3) Because of a potential concern of masking timely detec- 11. Smithells RW, Nevin NC, Seller MJ, Sheppard S, Harris R, Read AP et al. Further
experience of vitamin supplementation for prevention of neural tube defect recur-
tion of B12 deficiency, the total daily intake of folic acid
rences. Lancet 1983;1:1027–1031.
should not exceed 1000 g (1.0 mg) unless prescribed 12. Vergel RG, Sanchez LR, Heredero BL, Rodriguez PL, Martinez AJ. Primary preven-
by a physician. Recent evidence, however, indicates that tion of neural tube defects with folic acid supplementation: Cuban experience. Pre-
fortification has not led to a major increase in masking nat Diagn 1990;10:149 –152.
13. Workshop on folate, B12, and choline. Sponsored by the Panel on Folate and other
of vitamin B12 deficiency.16
B vitamins of the Standing Committee on the Scientific Evaluation of Dietary Ref-
REFERENCES erence Intakes, Food and Nutrition Board, Institute of Medicine, Washington, D.C.,
March 3-4, 1997. Nutrition 1999;15:92–96.
1. Hall JG, Solehdin F. Folate and its various ramifications. Adv Pediatr 1998;45:1–35.
14. Williams LJ, Mai CT, Edmonds LD, Shaw GM, Kirby RS, Hobbs CA et al. Prevalence
2. McDonald SD, Ferguson S, Tam L, Lougheed J, Walker MC. The prevention of
of spina bifida and anencephaly during the transition of mandatory folic acid forti-
congenital anomalies with periconceptional folic acid supplementation. J Obstet
fication in the United States. Teratology 2002;66:33–39.
Gynaecol Can 2003;25:115–121.
3. Mulinare J, Cordero JF, Erickson JD, Berry RT. Periconceptional use of multivita- 15. Birth Defects and Genetic Diseases Branch, Division of Birth Defects and Develop-
mins and the occurrence of NTDs. JAMA 1988;260:3141–3145. mental Disabilities, National Center for Environmental Health and Injury Control,
4. Bower C, Stanley FJ. Dietary folate as a risk factor for NTDs: Evidence from a case CDC. Use of folic acid for prevention of spina bifida and other neural tube defects:
control study in Western Australia. Med J Aus 1989;150:613– 619. 1983–1991. Morb Mortal Wkly Rep 1991;40:513–516.
5. Mills JL, Rhoads GG, Simpson JL, Cunningham GC, Conley MR, Lassman MR et al. 16. Mills JL, Von Kohorn I, Conley MR, Zeller JA, Cox C, Williamson RE et al. Low
The absence of a relationship between the periconceptional use of vitamins and vitamin B-12 concentrations in patients without anemia: the effect of folic acid
NTDs. N Engl J Med 1989;321:430 – 435. fortification of grain. Am J Clin Nutr 2003;77:1474 –1477.
Disclaimer: This statement is designed primarily as an educational resource for medical geneticists and other health care providers
to help them provide quality medical genetic services. Adherence to this statement does not necessarily ensure a successful medical
outcome. This statement should not be considered inclusive of all proper procedures and tests or exclusive of other procedures and
tests that are reasonably directed to obtaining the same results. In determining the propriety of any specific procedure or test, the
geneticist should apply his or her own professional judgment to the specific clinical circumstances presented by the individual patient
or specimen. It may be prudent, however, to document in the patient’s record the rationale for any significant deviation from this
statement.
284 Genetics IN Medicine
You might also like
- Review FollicacidDocument10 pagesReview Follicacidجعفر محمد غالب A1 صباحيNo ratings yet
- Folic Acid Preeclampsia CebuDocument53 pagesFolic Acid Preeclampsia CebuVirginia AbalosNo ratings yet
- 2018 WaldDocument11 pages2018 WaldbryaneatscamerasNo ratings yet
- Commentary - A Brief History of Folic Acid in The Prevention of Neural Tube DefectsDocument3 pagesCommentary - A Brief History of Folic Acid in The Prevention of Neural Tube DefectsBryan LimNo ratings yet
- Folic Acid Supplementation: What Is New? Fetal, Obstetric, Long-Term Benefits and RisksDocument11 pagesFolic Acid Supplementation: What Is New? Fetal, Obstetric, Long-Term Benefits and Risksrendyprimananda840No ratings yet
- jcph616 PDFDocument11 pagesjcph616 PDFHarnila JaNo ratings yet
- Folic Acid Deficiency PaperDocument5 pagesFolic Acid Deficiency Paperapi-401073891No ratings yet
- 2018 GarrettDocument12 pages2018 GarrettbryaneatscamerasNo ratings yet
- 10 Facts Folic Acid Women Patients: Top About Your Should KnowDocument1 page10 Facts Folic Acid Women Patients: Top About Your Should Knowapi-2489399440% (1)
- Women's HealthDocument40 pagesWomen's HealthSarah UddinNo ratings yet
- Why Do I Need Folic Acid?Document7 pagesWhy Do I Need Folic Acid?MrVios FuryNo ratings yet
- Global Folate EpidemiologyDocument8 pagesGlobal Folate EpidemiologyDegefa HelamoNo ratings yet
- Folic Acid in PregnancyDocument3 pagesFolic Acid in PregnancybdianNo ratings yet
- Vitabiotics Clinical ReviewDocument8 pagesVitabiotics Clinical ReviewgumasheNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument6 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyMelda Amalia SikumbangNo ratings yet
- Acido FolicoDocument7 pagesAcido FolicoWiller Orlando Castellar LenguaNo ratings yet
- Neural Tube DefectsDocument2 pagesNeural Tube DefectsVijay SluNo ratings yet
- A Case Report of Myelomenigocele With Arnold Chiari Malformatin Ii-Highlighting The Importance of Anemia Mukth Bharath ProgrammeDocument3 pagesA Case Report of Myelomenigocele With Arnold Chiari Malformatin Ii-Highlighting The Importance of Anemia Mukth Bharath ProgrammeIJAR JOURNALNo ratings yet
- Folic Acid Supplementation and The Occurrence of Congenital Heart Defects, Orofacial Clefts, Multiple Births, and MiscarriageDocument5 pagesFolic Acid Supplementation and The Occurrence of Congenital Heart Defects, Orofacial Clefts, Multiple Births, and MiscarriageMarie GuajardoNo ratings yet
- Course Task #9Document1 pageCourse Task #9ANGEL MICAH DAVIDNo ratings yet
- Notes On Spinal DysraphismDocument3 pagesNotes On Spinal DysraphismMicaela GarciaNo ratings yet
- The Primary Prevention of Birth Defects: Multivitamins or Folic Acid?Document12 pagesThe Primary Prevention of Birth Defects: Multivitamins or Folic Acid?Nurul ArdaniNo ratings yet
- Epilepsy in Women (Continuun)Document23 pagesEpilepsy in Women (Continuun)Victor GuerreroNo ratings yet
- Folic Acid Supplementation For Pregnant Women and Those Planning Pregnancy: 2015 UpdateDocument6 pagesFolic Acid Supplementation For Pregnant Women and Those Planning Pregnancy: 2015 UpdateHarnila JaNo ratings yet
- Folic Acid To Reduce Neonatal Mortality From Neural Tube DisordersDocument12 pagesFolic Acid To Reduce Neonatal Mortality From Neural Tube DisordersNanda Rizky FathiyaNo ratings yet
- Folic AcidDocument7 pagesFolic AcidINDAH DWI MENTARINo ratings yet
- Vitamin A and PregnancyDocument3 pagesVitamin A and PregnancyIoana Influencers RebornNo ratings yet
- Folic Acid Awareness A Crucial Step Towards Preventing AnencephalyDocument2 pagesFolic Acid Awareness A Crucial Step Towards Preventing AnencephalyEditor IJTSRDNo ratings yet
- dfm450 FolateDocument10 pagesdfm450 Folateapi-437250421No ratings yet
- General EmbryologyDocument41 pagesGeneral EmbryologyRiya SinghNo ratings yet
- Folic Acid: Influence On The Outcome of Pregnancy: Theresa O Scholl and William G JohnsonDocument9 pagesFolic Acid: Influence On The Outcome of Pregnancy: Theresa O Scholl and William G JohnsonKeylLaNo ratings yet
- What Is Ferrous Sulphate and Folic AcidDocument2 pagesWhat Is Ferrous Sulphate and Folic AcidMilagros ConstantinoNo ratings yet
- Dos and Donts in PregnancyDocument9 pagesDos and Donts in PregnancyNadia UnitassiaNo ratings yet
- Peran Asam FolatDocument13 pagesPeran Asam FolatAmellia Fajriatii BambangNo ratings yet
- Asam Folat 3Document13 pagesAsam Folat 3singgit putri suwandhiNo ratings yet
- Lammer 2004Document7 pagesLammer 2004Flórian JeffersonNo ratings yet
- Periconceptional Multivitamin Intake During Early Pregnancy, Genetic Variation of Acetyl-N-Transferase 1 (NAT1), and Risk For Orofacial CleftsDocument7 pagesPericonceptional Multivitamin Intake During Early Pregnancy, Genetic Variation of Acetyl-N-Transferase 1 (NAT1), and Risk For Orofacial CleftsFlórian JeffersonNo ratings yet
- SpinaBifida ManagementDocument4 pagesSpinaBifida ManagementDimple GoyalNo ratings yet
- Summary of Paul Thomas & Jennifer Margulis's The Vaccine-Friendly PlanFrom EverandSummary of Paul Thomas & Jennifer Margulis's The Vaccine-Friendly PlanNo ratings yet
- FolicartDocument12 pagesFolicartDiana-Elena ComandasuNo ratings yet
- Am J Clin Nutr 2011 Verhoef 1 2Document2 pagesAm J Clin Nutr 2011 Verhoef 1 2Sugiyanto GunadiNo ratings yet
- Is Folic Acid Good For Everyone?: CommentaryDocument17 pagesIs Folic Acid Good For Everyone?: CommentaryKirubakaranNo ratings yet
- Continued Folic Acid Supplementation Throughout Pregnancy, May Cause Colorectal Cancer in The Future - Somayeh Zaminpira - Sorush NiknamianDocument4 pagesContinued Folic Acid Supplementation Throughout Pregnancy, May Cause Colorectal Cancer in The Future - Somayeh Zaminpira - Sorush NiknamianSomayeh ZaminpiraNo ratings yet
- 08 Lectura ZINCDocument11 pages08 Lectura ZINCGraciela Pérez FigueroaNo ratings yet
- Journal at Iba PaDocument5 pagesJournal at Iba PaMIkahell CaszxyNo ratings yet
- American Academy of Pediatrics Metabolic Disorders 2014 Practice TestDocument43 pagesAmerican Academy of Pediatrics Metabolic Disorders 2014 Practice TestPrabu KumarNo ratings yet
- Neuroprotective Effects of Prenatal Folic Acid Supplementation Why Timing MattersDocument2 pagesNeuroprotective Effects of Prenatal Folic Acid Supplementation Why Timing MattersRony WirantoNo ratings yet
- Folic Acid in Pregnancy: Ethics/EducationDocument3 pagesFolic Acid in Pregnancy: Ethics/EducationAjengNo ratings yet
- 231 445 1 SMDocument4 pages231 445 1 SMAnonymous zH3OueNo ratings yet
- Factors Affecting Development ReportDocument21 pagesFactors Affecting Development ReportCamille Mae AsuncionNo ratings yet
- Women and Birth: Emma Vosnacos, Deborah J. PinchonDocument7 pagesWomen and Birth: Emma Vosnacos, Deborah J. PinchonAji SadamNo ratings yet
- Folic Acid FinalDocument4 pagesFolic Acid FinalDouglasNo ratings yet
- Vitamin K in The NewbornDocument5 pagesVitamin K in The NewbornPamela_Harnden_8116No ratings yet
- Effect of Supplementation During Pregnancy With L-ArginineDocument8 pagesEffect of Supplementation During Pregnancy With L-ArgininePujianti LestarinaNo ratings yet
- Spina BifidaDocument2 pagesSpina Bifidasrust2792No ratings yet
- Cormack 2021 - Neonatal Refeeding Syndrome and Clinical Outcome in ELBW Secondary Cohort Analysis ProVIDe TrialDocument14 pagesCormack 2021 - Neonatal Refeeding Syndrome and Clinical Outcome in ELBW Secondary Cohort Analysis ProVIDe TrialKarla LapendaNo ratings yet
- Bpj18 Pregnancy Pages 42-49Document8 pagesBpj18 Pregnancy Pages 42-49Charla SyafefiNo ratings yet
- Final Editing AssignmentDocument5 pagesFinal Editing Assignmentbarsha subediNo ratings yet
- Nutrition and Micronutrients in PregnancyDocument18 pagesNutrition and Micronutrients in PregnancyMeseret Hamer ZewdieNo ratings yet
- Summary of High-Quality CPR Components For BLS Providers: Component Adults and Adolescents Children InfantsDocument1 pageSummary of High-Quality CPR Components For BLS Providers: Component Adults and Adolescents Children InfantsAlfonso Tuñoque Chavez0% (1)
- Analisis Tecnico Usando Inteligencia ArtificialDocument59 pagesAnalisis Tecnico Usando Inteligencia ArtificialAnonymous KeU4gphVL5No ratings yet
- Pie Diabético: de La Fisiopatología A La Clínica: March 2009Document14 pagesPie Diabético: de La Fisiopatología A La Clínica: March 2009naira9valentina9pareNo ratings yet
- Artículo - OLR PDFDocument6 pagesArtículo - OLR PDFnaira9valentina9pareNo ratings yet
- 1 s2.0 S120197122030285X PDFDocument3 pages1 s2.0 S120197122030285X PDFnaira9valentina9pareNo ratings yet
- Surgical TechniquesDocument8 pagesSurgical Techniquesnaira9valentina9pare100% (1)
- 267 873 1 SMDocument5 pages267 873 1 SMnaira9valentina9pareNo ratings yet
- Bases Moleculares de Enfermedad de HuntingtonDocument9 pagesBases Moleculares de Enfermedad de Huntingtonnaira9valentina9pareNo ratings yet
- Papel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos FrontalesDocument7 pagesPapel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos Frontalesnaira9valentina9pareNo ratings yet
- Papel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos FrontalesDocument7 pagesPapel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos Frontalesnaira9valentina9pareNo ratings yet
- Gnentic Regulation of Cerebellar DevelopmentDocument10 pagesGnentic Regulation of Cerebellar Developmentnaira9valentina9pareNo ratings yet
- Papel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos FrontalesDocument7 pagesPapel de Los Ganglios Basales en La Monitorización de Las Funciones de Los Lóbulos Frontalesnaira9valentina9pareNo ratings yet
- Untitled Document 22Document5 pagesUntitled Document 22api-609568172No ratings yet
- Geriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDocument9 pagesGeriatric Index of Comorbidity: Validation and Comparison With Other Measures of ComorbidityDesya EspriliaNo ratings yet
- Cqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyDocument3 pagesCqi Indicators As Per Nabh 5Th Edition: S. No. Standard Ref. Deptt. KPI Formula FrequencyNatasha Bhasin91% (11)
- Sepsis Bundle by DR - ZakiDocument3 pagesSepsis Bundle by DR - Zakizaki ansariNo ratings yet
- PolydactylyDocument16 pagesPolydactylyGupies100% (1)
- Fnac of Thyroid - 102717Document13 pagesFnac of Thyroid - 102717Lal RuattlingaNo ratings yet
- Ovitrelle Epar Medicine Overview - enDocument3 pagesOvitrelle Epar Medicine Overview - enPhysics with V SagarNo ratings yet
- Neoplasms - Primary and Secondary Neoplasms of The BrainDocument11 pagesNeoplasms - Primary and Secondary Neoplasms of The BrainHisabu MohammedNo ratings yet
- HCIA Study Guide 2023Document22 pagesHCIA Study Guide 2023consultasluisfloresdrNo ratings yet
- Effectiveness of TECAR Therapy and Therapeutic Exercise in The Treatment of Musculoskeletal Conditions A Review ArticleDocument4 pagesEffectiveness of TECAR Therapy and Therapeutic Exercise in The Treatment of Musculoskeletal Conditions A Review ArticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Different Faces of HIV in A Single Patient: Case StudyDocument3 pagesDifferent Faces of HIV in A Single Patient: Case StudyAdvanced Research PublicationsNo ratings yet
- Effects of SmokingDocument2 pagesEffects of SmokingHAHAHANo ratings yet
- Cardiac Murmurs in Children: FactfileDocument2 pagesCardiac Murmurs in Children: FactfileResya I. NoerNo ratings yet
- Evidence Based For Failed Back Syndrome: Salim M. Ghazi, MDDocument50 pagesEvidence Based For Failed Back Syndrome: Salim M. Ghazi, MDneareastspineNo ratings yet
- NCP StrokeDocument7 pagesNCP StrokeMonica Gagarin Cortez100% (1)
- Nurselabs PEDIA QuestionsDocument13 pagesNurselabs PEDIA QuestionsSteffi MurielNo ratings yet
- Investigations For PneumoniaDocument27 pagesInvestigations For PneumoniaRoshana Mallawaarachchi0% (1)
- Dental Update 2002. Trismus - Aetiology Differential Diagnosis and TreatmentDocument5 pagesDental Update 2002. Trismus - Aetiology Differential Diagnosis and TreatmentMNur AshraNo ratings yet
- DAFTAR PUSTAKA Referat Ca MammaeDocument5 pagesDAFTAR PUSTAKA Referat Ca MammaeAulia JanerNo ratings yet
- Glycogen Storage Disease, Type II (Pompe Disease) : BackgroundDocument7 pagesGlycogen Storage Disease, Type II (Pompe Disease) : Background201111000No ratings yet
- Parameatal Cyst :A Case ReportDocument3 pagesParameatal Cyst :A Case ReportDr.ankit AnandNo ratings yet
- Drugs of ChoiceDocument2 pagesDrugs of ChoiceGian Carla SoNo ratings yet
- Ent Osce 2008Document22 pagesEnt Osce 2008salamred100% (2)
- Drug Study Atropine SulfateDocument1 pageDrug Study Atropine Sulfateirhizzp75% (8)
- Controversies Practice Changers in Ob-GynDocument57 pagesControversies Practice Changers in Ob-GynVirginia AbalosNo ratings yet
- PTS - Soal Bahasa Inggris Kelas IXDocument6 pagesPTS - Soal Bahasa Inggris Kelas IXRini YusmayantiNo ratings yet
- Compulsive-Sexual-Behavior-Disorder-In-Obsessive-Compulsive-Disorder-Prevalence-And-Associated-Comorbidity - Content File PDFDocument8 pagesCompulsive-Sexual-Behavior-Disorder-In-Obsessive-Compulsive-Disorder-Prevalence-And-Associated-Comorbidity - Content File PDFAlexandra SadkowskaNo ratings yet
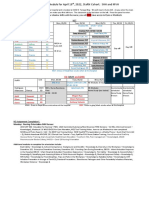
- Facility Week Plan April 18 2022 CohortDocument2 pagesFacility Week Plan April 18 2022 CohortElaine De VeraNo ratings yet
- Information Sheet 4.1-4: 1. Occupational Health and Safety IndicatorsDocument3 pagesInformation Sheet 4.1-4: 1. Occupational Health and Safety Indicatorsmark ian joverNo ratings yet
- Testing For Tuberculosis (TB) : Tuberculin Skin Test (TST)Document2 pagesTesting For Tuberculosis (TB) : Tuberculin Skin Test (TST)Aluh L DiniNo ratings yet