Professional Documents
Culture Documents
Gene Therapy For High-Grade Glioma
Uploaded by
Arh SetiawanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gene Therapy For High-Grade Glioma
Uploaded by
Arh SetiawanCopyright:
Available Formats
[Cell Adhesion & Migration 2:3, 186-191; July/August/September 2008]; ©2008 Landes Bioscience
Special Focus: Glioma Therapy
Gene therapy for high-grade glioma
Current approaches and future directions
Atsushi Natsume and Jun Yoshida*
Department of Neurosurgery; Nagoya University School of Medicine; Nagoya Japan
Key words: glioma, gene therapy, suicide gene, cytokine gene, oncolytic viruses
The treatment of high-grade gliomas remains difficult despite Suicide Gene Therapy
recent advances in surgery, radiotherapy and chemotherapy. True
advances may emerge from the increasing understanding in molec- The suicide gene therapy strategy involves the activation of
ular biology and discovery of novel mechanisms for the delivery prodrugs in tumor cells after transfecting the cells with a gene to
of tumoricidal agents. In an attempt to overcome this formidable induce the expression of an activating enzyme. The most extensively
neoplasm, molecular approaches using gene therapy have been investigated model of this strategy is the herpes simplex virus-
investigated clinically since 1992. The clinical trials have mainly thymidine kinase (HSV-tk) gene system used along with the systemic
been classified into three approaches: suicide gene therapy, immune administration of ganciclovir (GCV) (Fig. 1). This well-studied
gene therapy and oncolytic viral therapy. In this article, we review system was first reported by Moolten in 1986.3 In brief, HSV-tk,
these approaches, which have been studied in previous and ongoing unlike human-tk, monophosphorylates the nucleoside analog GCV;
clinical trials. the monophosphorylated GCV is then converted to triphosphate
GCV in the host cells. The triphosphate form is incorporated into
Introduction the DNA and it consequently blocks DNA replication and inhibits
Gliomas are the most common primary tumors of the central cell division. Preclinical studies using the HSV-tk/GCV system have
nervous system, accounting for 30% of adult primary brain tumors. reported inspiring results in various cancer models, including brain
The treatment of brain tumors remains difficult despite recent tumors. In one of these studies, the experimental brain tumors disap-
advances in surgery, radiotherapy and chemotherapy. Currently, no peared completely in 11 of 14 animals following transduction with
optimal treatment option is available for glioblastoma multiforme, the HSV-tk-expressing retrovirus and administration of GCV.2 As
and the patients typically survive for less than a year.1 The poor indicated in Table 1, most clinical studies have utilized a retroviral
prognosis is partially because of the inability to deliver chemo- vector, but the therapeutic effect was limited.4 In a randomized phase
therapeutic agents across the blood-brain barrier (BBB) and the low III clinical trial, which was completed in the year 2000, patients
tumor response to radiation. Therefore, novel and more effective were randomized to receive either surgical resection followed by
strategies are warranted and true advances may emerge from the radiotherapy with or without HSV-tk/GCV gene therapy.5 There
increasing understanding in molecular biology and discovery of novel was no difference between both the treatment arms in terms of
mechanisms for the delivery of tumoricidal agents. In an attempt median survival, which was the primary endpoint; this result was
to overcome this formidable neoplasm, molecular approaches using probably due to low transduction efficiency of the retroviral vectors.
gene therapy have been investigated clinically since 1992.2 The Eventually, they indicated the need to develop better techniques
clinical trials have mainly studied three approaches: (1) suicide gene for the delivery and distribution of therapeutic genes to achieve
therapy, (2) cytokine gene therapy and (3) oncolytic viral therapy effectiveness.
(Table 1; www.wiley.co.uk/genetherapy/clinical/). In this article, we Adenoviral vectors with better transduction efficiency and poten-
review these approaches, which have been studied in previous and tial to infect proliferating and non-proliferating cells may prove more
ongoing clinical trials. effective. A recent dose-escalating phase I trial reported the safety of
an adenoviral vector. In this trial, 10 of 11 patients survived 52 weeks
from the time of diagnosis, with an average survival of 112.3 weeks;6
this is more than twice the expected survival with conventional treat-
ments, and at the time of publication, one patient had survived for
*Correspondence to: Jun Yoshida; 65 Tsurumai-cho; Showa, Nagoya 466-8550 248 weeks from the time of diagnosis. However, further studies in
Japan; Tel.: +81.52.744.2353; Fax: +81.52.744.2360; Email: nsoffice@med. this area are warranted.
nagoya-u.ac.jp Suicide gene therapy via the introduction of apoptosis-inducing
Submitted: 02/25/08; Accepted: 05/13/08 genes is another promising strategy. The tumor protein TP53
Previously published online as a Cell Adhesion & Migration E-publication:
performs numerous functions, including regulation of progres-
http://www.landesbioscience.com/journals/celladhesion/article/6278 sion via the cell cycle, DNA repair after damage and induction of
186 Cell Adhesion & Migration 2008; Vol. 2 Issue 3
Gene therapy for gliomas
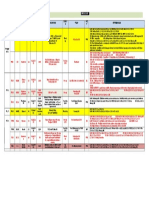
Table 1 Clinical gene therapy trials for glioma
Phase Gene(s) Gene type(s) Vector Principal investigator, Institution, Country
I HSV‑TK Suicide Retrovirus John C. Van Gilder Univ. of Iowa USA
I HSV‑TK Suicide Adenovirus E. Antonio Chiocca The Ohio State University USA
I HSV‑TK Suicide Retrovirus Economou Beatson Oncology Centre UK
I HSV‑TK Suicide Retrovirus Griffith R. Harsh Massachusetts General Hospital USA
I HSV‑TK Suicide Retrovirus F. W. Floeth Heinrich‑Heine‑University Germany
I HSV‑TK Suicide Adenovirus Frank Lieberman Mt. Sinai Medical USA
I/II HSV‑TK Suicide Retrovirus L. Mariani Oncology Clinical Research Switzerland
Novartis Pharma Basel
I/II HSV‑TK Suicide Retrovirus Rolf W. Seiler Univ. Canton Hospital Switzerland
I/II HSV‑TK Suicide Lipofection J. Voges University of Koln Germany
I/II HSV‑TK Suicide Retrovirus Jose Maria Izquierdo Universidad Autonoma de Madrid Spain
I/II HSV‑TK LacZ Suicide Marker Adenovirus Seppo Yla‑Herttuala Univ. of Kuopio Finland
I/II HSV‑TK Suicide Retrovirus David Klatzmann CERVI, Hopital Pitie‑Salpetriere France
I/II HSV‑TK Suicide Retrovirus Nanno Harrie Mulder Academic Hospital Groningen The Netherlands
II HSV‑TK Suicide Retrovirus Bernard Maria Univ. of Florida USA
III HSV‑TK Suicide Retrovirus Nikolai Rainov Martin‑Luther Universitat Germany
III HSV‑TK Suicide Retrovirus Bernard Maria Univ. of Florida USA
I IL‑2 Cytokine Nanno Harrie Mulder Academic Hospital Groningen The Netherlands
I IL‑2 Cytokine Retrovirus Robert E. Sobol Sidney Kimmel Cancer Center USA
I IFNbeta Cytokine Lipofection Jun Yoshida Nagoya University Japan
I IL‑4 Cytokine Retrovirus Ian Pollack University of Pittsburgh USA
I GM‑CSF Cytokine Naked/Plasmid DNA William T. Curry, Jr. Massachusetts General Hospital USA
I IFNb Cytokine Adenovirus Stephen L. Eck Univ. of Pennsylvania USA
I/II IL‑12 Cytokine Semliki forest virus
I No transgene Oncolytic virus Herpes simplex virus Roy Rampling Beatson Oncology Centre UK
I No transgene Oncolytic virus Poliovirus Darrell D. Bigner Duke University USA
I No Transgene Oncolytic virus Herpes simplex virus William T. Curry Massachusetts General Hospital USA
I/II No transgene Oncolytic virus Herpes simplex virus James Markert Univ. of Alabama USA
I/II No transgene Oncolytic virus Adenovirus Frederick F. Lang The University of Texas USA
M.D. Anderson Cancer Center
II No transgene Oncolytic virus Herpes simplex virus Roy Rampling Beatson Oncology Centre UK
III No transgene Oncolytic virus Herpes simplex virus Gareth Cruickshank Queen Elizabeth Hospital UK
I Antisense IGF‑1 Antisense Lipofection Joseph Ilan Case Western Reserve University USA
I CMV pp65‑LAMP Antigen RNA transfer John H. Sampson Duke University USA
I MGMT Cell protection/ Retrovirus Lars Martin Wagner Cincinnati Children’s Hospital USA
Drug resistance Medical Center
I MGMT Cell protection/ Retrovirus Hans Peter Kiem Fred Hutchinson Cancer Research USA
Drug resistance Center and University of Washington
I TGFb Growth factor Naked/Plasmid DNA Keith L. Black Maxine Dunitz Neurosurgical Institute USA
I p53 Tumor suppressor Adenovirus Frederick F. Lang University of Texas USA
MD Anderson Medical Center
I IL‑13 a 2‑specific Receptor Naked/Plasmid DNA Michael Jensen City of Hope National USA
scFvFc‑z T Medical Center
cell receptor
Source, www.wiley.co.uk/genetherapy/clinical/ (September, 2007). HSV‑tk, herpes simplex virus‑thymidine kinase; IL, interleukin; IFN, interferon; GM‑CSF, granulocyte‑macrophage colony stimulating factor; MGMT,
O6‑methylguanine deoxyribonucleic acid methyltransferase; TGF, transforming growth factor.
apoptosis. p53 mutations have been reported in 30–60% of malig- with recurrent glioma; their protocol involved intratumoral injection
nant gliomas.7 The replacement of the wild-type p53 gene function of p53-expressing adenoviral vector followed by tumor resection.8
may reduce tumor growth or induce apoptosis. In 2003, a group of It was demonstrated that exogenous p53 activated downstream
researchers at the MD Anderson Medical Center performed a phase I effectors and induced apoptosis, and clinical toxicity was minimal.
clinical trial of adenovirus-mediated p53 gene therapy in 15 patients However, the transfected cells were on an average only 5 mm away
www.landesbioscience.com Cell Adhesion & Migration 187
Gene therapy for gliomas
Figure 1. HSV-tk/GCV Suicide gene therapy. In tumor cells transduced with the HSV-tk gene, HSV-tk monophosphorylates the nucleoside analog GCV that
is administered systemically. The monophosphorylated GCV is then converted to triphosphate GCV in the host cells. The triphosphate form is incorporated
into the DNA, and it consequently blocks DNA replication and induced apoptosis (A). The toxic triphosphate is eventually transported to neighboring cells,
and provides “bystander effects” (B) leading to apoptosis (C).
from the injection site. A more widespread distribution of a vector glioma cells induced a cytocidal but not a cytostatic response even in
should be achieved to gain maximum therapeutic benefit. The IFN-resistant human glioma cell lines, probably by inducing apop-
currently known limitations of adenoviral vectors are as follows: tosis.17 In vivo experiments using nude mice implanted with human
(1) the immunogenicity of the vector may limit the efficacy of this glioma cells intracranially or subcutaneously revealed that the local
strategy,9,10 and (2) the cell entry of an adenovirus depends on the administration of cationic liposomes containing the human IFNβ
coxsackie-adenovirus receptor (CAR) that is scarcely expressed in gene induced apparent tumor growth reduction, prolonged survival
malignant gliomas.11 Several attempts have been made to resolve this and natural killer (NK) cell activation.18,19 In addition, a similar
issue by engineering adenoviruses with tropism for glioma-specific growth-inhibitory effect was also observed in a syngeneic intracranial
receptors.12 mouse glioma model treated with the liposome-mediated murine
IFNβ gene. This gene therapy system induced specific cytotoxic
Immune Gene Therapy T-cell immunity against mouse glioma and the NK cells.20,21 Based
The central nervous system in mammals is often regarded as on these observations, a phase I clinical trial of IFNβ gene therapy
immunologically privileged and may have a disadvantage with regard was performed in five patients with recurrent malignant glioma.22
to augmenting the immune response. It is generally believed that This was a two-stage trial in which the initial treatment comprised
brain tumors have low immunogenicity and suppress the immune tumor removal and injection of liposomes containing the human
response. However, recent advances in the understanding of cytokine IFNβ gene into the margin of the resulting defect and subsequent
action and gene delivery techniques have revived the interest in delivery of subsequent injections via an implanted catheter. The
the concept of immune gene therapy using a variety of cytokine clinical toxicity was found to be minimal. At ten weeks after treat-
genes that increase tumor immunogenicity and/or activate the host ment initiation, two patients showed more than 50% reduction
immune response. To achieve regression of infiltrative intracranial while others had stable disease. The median survival was longer in the
neoplasms that form multiple foci, two approaches have been treated subjects than in the matched historical control from our insti-
employed: (1) administration of tumor vaccines using genetically tution. After the gene therapy, significant changes were observed in
engineered cells that express cytokines such as interleukin (IL)-2 and histology and gene expression related to immunoresponse, apoptosis
IL-4 and (2) intratumoral secretion in situ by transfecting tumor and neovascularization23 (Fig. 2). This study provides the foundation
cells with cytokine genes. With regard to the former, previous reports for a phase II trial of IFNβ gene therapy. Very recently, Chiocca et al.
have suggested that peripheral tumor vaccination can definitely reported a phase I clinical trial (a dose-escalating cohort) of stereot-
initiate a systemic immune response against intracranial tumors.13,14 actic injection of an IFNβ-expressing adenoviral vector in 11 patients
However, large amounts of tumor tissues or autologous tumor cell with malignant glioma. Direct injection of the vector into the tumor
lines are required to generate gene-modified tumor vaccines of a and the surrounding normal brain areas after surgical tumor removal
clinical grade; this may limit the feasibility of whole tumor vacci- was feasible. A reproducible increase in tumor cell apoptosis was
nation strategies. With regard to the latter, IL-4 expression in situ observed after the treatment.24
was reported to induce an inflammatory response, leading to tumor
Oncolytic Viral (Gene) Therapy
regression,15,16 while severe CNS toxicity caused by brain edema
has been documented when IL-2 or interferon-gamma (IFN)γ was While gene therapy strategies typically employ replication-
secreted intracranially by tumor cells. IFNβ is another potential incompetent viruses as the gene delivery tool, oncolytic viral therapy
cytokine that exerts pleiotropic biological effects.17 Although identi- utilizes replication-competent viruses to infect and lyse the cells with
fied for and named due to its ability to interfere with viral replication or without employing gene transfer (Fig. 3). Numerous viruses have
in treated cells, IFNβ also has immunomodulatory and antiprolifera- been proposed and investigated for their therapeutic application as
tive effects. In 2000, our group at Nagoya University, Japan, started oncolytic agents. Three human pathogenic viruses—herpes simplex
using the cytokine gene therapy: the IFNβ gene was delivered via virus (HSV), adenovirus and poliovirus—have been extensively
cationic liposomes based on the following preclinical and experi- studied and demonstrated to have clinical potential.
mental studies. In vitro experiments demonstrated that the cationic HSV is an enveloped double-strand DNA virus with natural
liposome-mediated human IFNβ gene transfer to cultured human neurotropism and the ability to replicate in dividing and nondividing
188 Cell Adhesion & Migration 2008; Vol. 2 Issue 3
Gene therapy for gliomas
cells. Martuza et al. developed a conditionally repli-
cating HSV, G207; this virus exhibits mutations in both
copies of the neurovirulence gene γ134.5 and disrupts
the gene encoding ribonucleotide reductase. Preclinical
studies have demonstrated that G207 decreased the growth
of experimental glioma and that it was well tolerated in
nonhuman primates.25 In 2000, a dose-escalated phase
I clinical trial was published, and it was the first report
on the use of a replication-competent HSV mutant in
a human brain tumor trial.26 Twenty-one patients with
recurrent malignant glioma were enrolled in the study,
and no dose-limiting toxicities (DLTs) were observed.
Of the 21 patients, eight demonstrated reduced tumor
enhancement volumes, and two patients were long-term
survivors. Another HSV mutant 1716 exhibited deletion
only in the γ134.5 genes. The phase I trial for recurrent
glioma has been completed. No DLTs were encountered in
the nine patients enrolled in the trial, and viral replication
was demonstrated in tumor; the amount of recovered virus
exceeded the input dose in some patients, and this result
further confirmed the validity of the principle.27 In a phase
II clinical trial of this mutant HSV, a response was noted
in 2 of 12 patients.28 Both G207 and 1716 are currently
under further clinical investigation.
Adenoviruses are nonenveloped DNA viruses capable
of infecting both the dividing and nondividing cells.
Bischoff et al. developed a conditionally replicative adeno-
virus, ONYX-015.29-31 ONYX-015 contains a deletion
in the viral protein E1B-55K, which normally binds to
and inactivates the host cell p53 protein. Therefore, it is
assumed that cells with functional p53 cannot support viral Figure 2. Mechanisms of liposome-mediated IFNβ gene therapy. Histology and cDNA
expression microarray analyses revealed significant inductions in apoptosis (A) and
replication in the absence of this protein, whereas tumor antitumor immunoresponse (B), and inhibition of neovascularization (C).
cells with a nonfunctional p53 can support viral replication.
Preclinical studies in human malignant glioma xenografts
demonstrated cell lysis and impaired tumor growth in response to reached.33 Of the 12 patients who received the highest doses of the
ONYX-015, but the response was independent of the p53 status.32 virus, three survived until the end of the study and were available for
Although the exact mechanism is not completely understood and follow-up for more than 19 months.
may not be related to p53, ONYX-015 is only the third oncolytic Poliovirus is a nonenveloped RNA virus with natural neurot-
virus to be tested in human clinical trials for malignant glioma ropism. The cellular receptor responsible for viral entry, CD155 is
(following G207 and 1716). In the initial phase I clinical trial of ectopically upregulated in malignant glioma,34-36 and the virulence
intratumoral delivery, none of the 24 patients with glioma exhibited of poliovirus can be manipulated in a cell-type specific manner
a significant response, with 96% experiencing disease progression. at the level of translation control.34,37 Viral protein translation is
This was a dose-escalated study wherein no patient demonstrated mediated by the internal ribosome entry site (IRES) element in the
any serious adverse events and the maximum tolerated dose was not 5' nontranslated region of the viral genome. The IRES function
Figure 3. Oncolytic therapy. Oncolytic viral therapy utilizes replication-competent viruses which ideally can infect and replicate in tumor cells (A). The viruses
specifically lyse tumor cells (B) and sequentially infect neighboring cells (C).
www.landesbioscience.com Cell Adhesion & Migration 189
Gene therapy for gliomas
depends on cell-specific constraints that can be exploited to drive the 4. Ram Z, Culver KW, Oshiro EM, Viola JJ, DeVroom HL, Otto E, Long Z, Chiang Y,
McGarrity GJ, Muul LM, Katz D, Blaese RM, Oldfield EH. Therapy of malignant brain
poliovirus gene expression and cytotoxicity, preferably in malignant tumors by intratumoral implantation of retroviral vector-producing cells. Nat Med 1997;
cells.38,39 These findings led to the development of a recombinant 3:1354-61.
poliovirus for the treatment of malignant gliomas. By exchanging the 5. Rainov NG. A phase III clinical evaluation of herpes simplex virus type 1 thymidine kinase
and ganciclovir gene therapy as an adjuvant to surgical resection and radiation in adults with
IRES element of the poliovirus with that of human rhinovirus type previously untreated glioblastoma multiforme. Hum Gene Ther 2000; 11:2389-401.
2 (HRV2), Gromeier et al. created a recombinant virus (PV-RIPO) 6. Germano IM, Fable J, Gultekin SH, Silvers A. Adenovirus/herpes simplex-thymidine
kinase/ganciclovir complex: preliminary results of a phase I trial in patients with recurrent
with a greatly diminished viral propagation in normal neuronal cells malignant gliomas. J Neuro-Oncol 2003; 65:279-89.
while retaining excellent lytic growth in malignant glioma cells.34 7. Ware ML, Berger MS, Binder DK. Molecular biology of glioma tumorigenesis. Histol
Preclinical studies of PV-RIPO provide principle data for a planned Histopathol 2003; 18:207-16.
8. Lang FF, Bruner JM, Fuller GN, Aldape K, Prados MD, Chang S, Berger MS, McDermott MW,
phase I clinical trial. When delivered directly into the spinal cord, Kunwar SM, Junck LR, Chandler W, Zwiebel JA, Kaplan RS, Yung WK. Phase I trial of
PV-RIPO significantly attenuated the in vitro growth of neuronal adenovirus-mediated p53 gene therapy for recurrent glioma: biological and clinical results.
cells and failed to cause poliomyelitis in both mice transgenic for the J Clin Oncol 2003; 21:2508-18.
9. Morral N, O’Neal W, Zhou H, Langston C, Beaudet A. Immune responses to reporter pro-
CD155 receptor35 and cynomolgus monkeys.34 On the other hand, teins and high viral dose limit duration of expression with adenoviral vectors: comparison
eight different glioma cell lines tested in vitro were highly susceptible of E2a wild type and E2a deleted vectors. Hum Gene Ther 1997; 8:1275-86.
to PV-RIPO infection, and the intratumoral injection into HTB-14 10. Tripathy SK, Black HB, Goldwasser E, Leiden JM. Immune responses to transgene-encoded
proteins limit the stability of gene expression after injection of replication-defective adeno-
astrocytic intracerebral tumors resulted in complete regression in 18 virus vectors. Nat Med 1996; 2:545-50.
of 25 mice. A phase I clinical trial of PV-RIPO is currently underway 11. Asaoka K, Tada M, Sawamura Y, Ikeda J, Abe H. Dependence of efficient adenoviral gene
delivery in malignant glioma cells on the expression levels of the Coxsackievirus and adeno-
for application in recurrent malignant glioma. virus receptor. J Neurosurg 2000; 92:1002-8.
12. Shinoura N, Sakurai S, Asai A, Kirino T, Hamada H. Transduction of a fiber-mutant
Future Directions adenovirus for the HSVtk gene highly augments the cytopathic effect towards gliomas. Jpn
J Cancer Res 2000; 91:1028-34.
Each of the strategies described herein have their own distinct 13. Sobol RE, Fakhrai H, Shawler D, Gjerset R, Dorigo O, Carson C, Khaleghi T, Koziol J,
advantages and limitations inherent to the technology employed. Shiftan TA, Royston I. Interleukin-2 gene therapy in a patient with glioblastoma. Gene
Ther 1995; 2:164-7.
Despite the relatively rapid advancement in our scientific under- 14. Okada H, Giezeman-Smits KM,Tahara H, Attanucci J, Fellows WK, Lotze MT, Chambers WH,
standing and technological capabilities, all the major molecular Bozik ME. Effective cytokine gene therapy against an intracranial glioma using a retrovirally
approaches currently being investigated are significantly deficient in transduced IL-4 plus HSVtk tumor vaccine. Gene Ther 1999; 6:219-26.
15. Yu JS, Wei MX, Chiocca EA, Martuza RL, Tepper RI. Treatment of glioma by engineered
one or more of the following categories. interleukin 4-secreting cells. Cancer Res 1993; 53:3125-8.
(1) Delivery—the ability to reach the tumor efficiently and spread 16. Wei MX, Tamiya T, Hurford RK Jr, Boviatsis EJ, Tepper RI, Chiocca EA. Enhancement of
throughout the entire population of malignant cells. interleukin-4-mediated tumor regression in athymic mice by in situ retroviral gene transfer.
Hum Gene Ther 1995; 6:437-43.
(2) Effectiveness—the ability to control or eradicate malignant cells. 17. Borden EC, Lindner D, Dreicer R, Hussein M, Peereboom D. Second-generation interfer-
i.e., to halt the growth or induce regression of malignant gliomas. ons for cancer: clinical targets. Semin Cancer Biol 2000; 10:125-44.
(3) Adverse Events (Safety)—the ability to target tumor cells 18. Yagi K, Hayashi Y, Ishida N, Ohbayashi M, Ohishi N, Mizuno M, Yoshida J. Interferon-
beta endogenously produced by intratumoral injection of cationic liposome-encapsulated
without causing significant toxicity to the surrounding normal gene: cytocidal effect on glioma transplanted into nude mouse brain. Biochemistry and
brain. molecular biology international 1994; 32:167-71.
With increase in our understanding of molecular biology and 19. Mizuno M, Yoshida J. Effect of human interferon beta gene transfer upon human glioma,
transplanted into nude mouse brain, involves induced natural killer cells. Cancer Immunol
technical advances, a strategy that is not limited by these factors may Immunother 1998; 47:227-32.
become a tenable goal. 20. Natsume A, Mizuno M, Ryuke Y, Yoshida J. Antitumor effect and cellular immunity activa-
tion by murine interferon-beta gene transfer against intracerebral glioma in mouse. Gene
A rational combination of therapeutic strategies with different Ther 1999; 6:1626-33.
modes of action has the potential to deliver synergistic benefit by 21. Natsume A, Tsujimura K, Mizuno M, Takahashi T, Yoshida J. IFNbeta gene therapy induces
using one agent to sensitize treatment by the other. The oncolytic systemic antitumor immunity against malignant glioma. J Neuro-oncol 2000; 47:117-24.
22. Yoshida J, Mizuno M, Fujii M, Kajita Y, Nakahara N, Hatano M, Saito R, Nobayashi M,
viruses G207 and ONYX-015 have been studied in the context of Wakabayashi T. Human gene therapy for malignant gliomas (glioblastoma multiforme and
glioma therapy combined with radiotherapy. Other interesting molec- anaplastic astrocytoma) by in vivo transduction with human interferon beta gene using
ular therapeutic approaches include anti-angiogenic molecules such as cationic liposomes. Hum Gene Ther 2004; 15:77-86.
23. Wakabayashi T, Natsume A, Hashizume Y, Fujii M, Mizuno M, Yoshida J. A phase I clinical
endostatin; anti-receptor antibodies for EGFR, VEGF and PDGFR; trial of interferon-beta gene therapy for high-grade glioma: novel findings from gene expres-
and inhibitors of downstream signaling such as mTOR inhibitors. sion profiling and autopsy. J Gene Med 2008.
These approaches have provided encouraging results in glioma 24. Chiocca EA, Smith KM, McKinney B, Palmer CA, Rosenfeld S, Lillehei K, Hamilton A,
Demasters BK, Judy K, Kirn D. A Phase I Trial of Ad.hIFNbeta Gene Therapy for Glioma.
models. Although preclinical data are intriguingly promising, all these Mol Ther 2008.
approaches are yet to demonstrate a significant benefit in a phase II or 25. Hunter WD, Martuza RL, Feigenbaum F, Todo T, Mineta T, Yazaki T, Toda M, Newsome JT,
Platenberg RC, Manz HJ, Rabkin SD. Attenuated, replication-competent herpes simplex
III clinical trial. In the near future, malignant gliomas will probably be virus type 1 mutant G207: safety evaluation of intracerebral injection in nonhuman pri-
treated through synergistic effects of a multipronged attack. mates. J Virol 1999; 73:6319-26.
26. Markert JM, Medlock MD, Rabkin SD, Gillespie GY, Todo T, Hunter WD, Palmer CA,
References Feigenbaum F, Tornatore C, Tufaro F, Martuza RL. Conditionally replicating herpes simplex
1. Fine HA, Dear KB, Loeffler JS, Black PM, Canellos GP. Meta-analysis of radiation therapy virus mutant, G207 for the treatment of malignant glioma: results of a phase I trial. Gene
with and without adjuvant chemotherapy for malignant gliomas in adults. Cancer 1993; Ther 2000; 7:867-74.
71:2585-97.
27. Rampling R, Cruickshank G, Papanastassiou V, Nicoll J, Hadley D, Brennan D, Petty R,
2. Culver KW, Ram Z, Wallbridge S, Ishii H, Oldfield EH, Blaese RM. In vivo gene transfer MacLean A, Harland J, McKie E, Mabbs R, Brown M. Toxicity evaluation of replication-
with retroviral vector-producer cells for treatment of experimental brain tumors. Science competent herpes simplex virus (ICP 34.5 null mutant 1716) in patients with recurrent
(New York, NY) 1992; 256:1550-2. malignant glioma. Gene Ther 2000; 7:859-66.
3. Moolten FL. Tumor chemosensitivity conferred by inserted herpes thymidine kinase genes:
paradigm for a prospective cancer control strategy. Cancer Res 1986; 46:5276-81.
190 Cell Adhesion & Migration 2008; Vol. 2 Issue 3
Gene therapy for gliomas
28. Papanastassiou V, Rampling R, Fraser M, Petty R, Hadley D, Nicoll J, Harland J, Mabbs R,
Brown M. The potential for efficacy of the modified (ICP 34.5(-)) herpes simplex virus
HSV1716 following intratumoural injection into human malignant glioma: a proof of
principle study. Gene Ther 2002; 9:398-406.
29. Bischoff JR, Kirn DH, Williams A, Heise C, Horn S, Muna M, Ng L, Nye JA, Sampson-
Johannes A, Fattaey A, McCormick F. An adenovirus mutant that replicates selectively in
p53-deficient human tumor cells. Science (New York, NY) 1996; 274:373-6.
30. Rainov NG, Ren H. Oncolytic viruses for treatment of malignant brain tumours. Acta
neurochirurgica 2003; 88:113-23.
31. Vecil GG, Lang FF. Clinical trials of adenoviruses in brain tumors: a review of Ad-p53 and
oncolytic adenoviruses. J Neuro-oncol 2003; 65:237-46.
32. Geoerger B, Grill J, Opolon P, Morizet J, Aubert G, Lecluse Y, van Beusechem VW,
Gerritsen WR, Kirn DH, Vassal G. Potentiation of radiation therapy by the oncolytic
adenovirus dl1520 (ONYX-015) in human malignant glioma xenografts. Brit J Cancer
2003; 89:577-84.
33. Chiocca EA, Abbed KM, Tatter S, Louis DN, Hochberg FH, Barker F, Kracher J, Grossman SA,
Fisher JD, Carson K, Rosenblum M, Mikkelsen T, Olson J, Markert J, Rosenfeld S,
Nabors LB, Brem S, Phuphanich S, Freeman S, Kaplan R, Zwiebel J. A phase I open-label,
dose-escalation, multi-institutional trial of injection with an E1B-Attenuated adenovirus,
ONYX-015, into the peritumoral region of recurrent malignant gliomas, in the adjuvant
setting. Mol Ther 2004; 10:958-66.
34. Gromeier M, Lachmann S, Rosenfeld MR, Gutin PH, Wimmer E. Intergeneric poliovirus
recombinants for the treatment of malignant glioma. P Natl Acad Sci-Biol 2000; 97:
6803-8.
35. Merrill MK, Bernhardt G, Sampson JH, Wikstrand CJ, Bigner DD, Gromeier M.
Poliovirus receptor CD155-targeted oncolysis of glioma. Neuro-Oncol 2004; 6:208-17.
36. Sloan KE, Stewart JK, Treloar AF, Matthews RT, Jay DG. CD155/PVR enhances glioma
cell dispersal by regulating adhesion signaling and focal adhesion dynamics. Cancer Res
2005; 65:10930-7.
37. Gromeier M, Alexander L, Wimmer E. Internal ribosomal entry site substitution elimi-
nates neurovirulence in intergeneric poliovirus recombinants. P Natl Acad Sci-Biol 1996;
93:2370-5.
38. Merrill MK, Gromeier M. The double-stranded RNA binding protein 76:NF45 heterodi-
mer inhibits translation initiation at the rhinovirus type 2 internal ribosome entry site.
J Virol 2006; 80:6936-42.
39. Song Y, Friebe P, Tzima E, Junemann C, Bartenschlager R, Niepmann M. The hepatitis
C virus RNA 3'-untranslated region strongly enhances translation directed by the internal
ribosome entry site. J Virol 2006; 80:11579-88.
www.landesbioscience.com Cell Adhesion & Migration 191
You might also like
- Asher - Bacteria, Inc.Document48 pagesAsher - Bacteria, Inc.Iyemhetep100% (1)
- Fulbright Certificate of HealthDocument8 pagesFulbright Certificate of HealthLinda Klimavicius100% (1)
- CHAPTER XI - Gene TherapyDocument4 pagesCHAPTER XI - Gene TherapyKeannoNo ratings yet
- The Anti Vaccine MovementDocument13 pagesThe Anti Vaccine MovementMariangeles PontorieroNo ratings yet
- Venom Antivenom and ImmunityDocument80 pagesVenom Antivenom and ImmunityAris DedovićNo ratings yet
- PHA Individual Health Profile & Assessment Form As of Oct.09, 2017Document8 pagesPHA Individual Health Profile & Assessment Form As of Oct.09, 2017Eden VblagasyNo ratings yet
- Preventive Veterinary MedicineDocument48 pagesPreventive Veterinary MedicineBorja Bueno Garcia100% (3)
- Rabies, Malaria, Tetanus PSBIM Review 2014Document52 pagesRabies, Malaria, Tetanus PSBIM Review 2014Argyll Lorenzo BongosiaNo ratings yet
- Nutri Quiz2Document6 pagesNutri Quiz2Rosa Lynn YaunNo ratings yet
- HandbookOfNatureCureVol1-Fielder, DR John LDocument85 pagesHandbookOfNatureCureVol1-Fielder, DR John LStewie532No ratings yet
- Gene Therapy For CancerDocument7 pagesGene Therapy For Canceresraa elsharkawyNo ratings yet
- Practice Test Pediatric Nursing 100 ItemsDocument17 pagesPractice Test Pediatric Nursing 100 ItemsKarla FralalaNo ratings yet
- Communicable Diseases ReviewerDocument13 pagesCommunicable Diseases ReviewerMarivic Salcedo McCreaNo ratings yet
- Pathway Cancer MedicationDocument10 pagesPathway Cancer MedicationWaode RahmahNo ratings yet
- Gene Transfer and CancerDocument3 pagesGene Transfer and CancerIsabel Sofia Corredor MendezNo ratings yet
- Introduction To Gene Therapy: 1.1 Genes As DrugsDocument7 pagesIntroduction To Gene Therapy: 1.1 Genes As DrugsJason LingNo ratings yet
- 1st StudyDocument14 pages1st StudyWeeaboo Franz VlogsNo ratings yet
- Assignment No. 1: Gene TherapyDocument5 pagesAssignment No. 1: Gene Therapykhadija tariqNo ratings yet
- Cam4 6 207Document13 pagesCam4 6 207marconijrrNo ratings yet
- Define Gene Therapy.: 3. Explain The Ethical Considerations in Germ Line Gene TherapyDocument5 pagesDefine Gene Therapy.: 3. Explain The Ethical Considerations in Germ Line Gene TherapyJake AlarconNo ratings yet
- Cancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T CellDocument10 pagesCancer - 2004 - Li - Treatment Outcome and Pattern of Failure in 77 Patients With Sinonasal Natural Killer T Cell or T Cell2512505993No ratings yet
- Gene TherapyDocument3 pagesGene TherapyGleeson Jay NiedoNo ratings yet
- Approach: Genes Cells Biological Tissues Disease MutatedDocument9 pagesApproach: Genes Cells Biological Tissues Disease MutatedrajnikhatkarNo ratings yet
- Gene Therapy Clinical Trials Worldwide To 2017 An UpdateDocument16 pagesGene Therapy Clinical Trials Worldwide To 2017 An UpdateLeonardo Sandi SalazarNo ratings yet
- 10 1056@NEJMoa1900574 PDFDocument9 pages10 1056@NEJMoa1900574 PDFGhadah AlyousifNo ratings yet
- Ruxolitinib For Glucocorticoid-Refractory Acute Graft-versus-Host DiseaseDocument11 pagesRuxolitinib For Glucocorticoid-Refractory Acute Graft-versus-Host DiseasemrboredguyNo ratings yet
- Cancer Immunotherapy Beyond Checkpoint BlockadeDocument16 pagesCancer Immunotherapy Beyond Checkpoint Blockaderaxi bacumabNo ratings yet
- KLP 1Document15 pagesKLP 1Arig Al Fath OdeNo ratings yet
- BMJ 2021 068956.fullDocument14 pagesBMJ 2021 068956.fullAnna JuniedNo ratings yet
- The Future of Immune Checkpoint Therapy: Padmanee Sharma and James P. AllisonDocument6 pagesThe Future of Immune Checkpoint Therapy: Padmanee Sharma and James P. Allisonlos mejores icfesNo ratings yet
- BTE101 Lecture18.1 MedBiotechApp GeneTherapy MHU SummerSemester2021 BRACU FinalDocument42 pagesBTE101 Lecture18.1 MedBiotechApp GeneTherapy MHU SummerSemester2021 BRACU FinalM.H. RafidNo ratings yet
- Gene Therapy For Cancer Treatment 1Document33 pagesGene Therapy For Cancer Treatment 1Shambhoo SwarajNo ratings yet
- Ublituximab Versus Teriflunomide in Relapsing Multiple SclerosisDocument11 pagesUblituximab Versus Teriflunomide in Relapsing Multiple SclerosisLee Foo WengNo ratings yet
- Gene Therapy Is The InsertionDocument8 pagesGene Therapy Is The InsertionxulkifalNo ratings yet
- Recurrent Glioblastoma Treated With Recombinant Poliovirus: Original ArticleDocument12 pagesRecurrent Glioblastoma Treated With Recombinant Poliovirus: Original ArticleTrinanda ChoirunissaNo ratings yet
- Vaccine HistoryDocument35 pagesVaccine HistoryEhed AymazNo ratings yet
- Terapi GenDocument81 pagesTerapi Genyudha fahmiNo ratings yet
- Actualización de Inmunoterapia en CáncerDocument13 pagesActualización de Inmunoterapia en CáncerAli BelloNo ratings yet
- Jco 2015 64 8931Document10 pagesJco 2015 64 8931Kamila MuyasarahNo ratings yet
- Immuno TherapyDocument20 pagesImmuno TherapyAttis PhrygiaNo ratings yet
- A Novel Oncolytic Viral Therapy and Imaging Technique For Gastric Cancer Using A Genetically Engineered Vaccinia Virus Carrying The Human Sodium Iodide SymporterDocument7 pagesA Novel Oncolytic Viral Therapy and Imaging Technique For Gastric Cancer Using A Genetically Engineered Vaccinia Virus Carrying The Human Sodium Iodide SymporterkNo ratings yet
- Gene Theraphy Module14Document24 pagesGene Theraphy Module14Anime HubNo ratings yet
- Gene Therapy For Cancer Treatment Past Present FutureDocument10 pagesGene Therapy For Cancer Treatment Past Present FuturefrancoismullierNo ratings yet
- Car T LymphomaDocument14 pagesCar T LymphomaMuneer KhalamNo ratings yet
- Ibru Benda Rituxi For Mantle Cell Lymphoma NEJMDocument13 pagesIbru Benda Rituxi For Mantle Cell Lymphoma NEJMMiriam AguilarNo ratings yet
- Green-Tsui2013 Article ImpactOfAnesthesiaForCancerSurDocument22 pagesGreen-Tsui2013 Article ImpactOfAnesthesiaForCancerSurNataNo ratings yet
- Biomedicines: Gene Therapy Used in Cancer TreatmentDocument14 pagesBiomedicines: Gene Therapy Used in Cancer TreatmentParagRoyNo ratings yet
- Ipilimumab For Patients With Relapse After Allogeneic TransplantationDocument11 pagesIpilimumab For Patients With Relapse After Allogeneic TransplantationMhmd KorosNo ratings yet
- Selle2015 PDFDocument12 pagesSelle2015 PDFatikha apriliaNo ratings yet
- Gene TherapyDocument20 pagesGene Therapyrohitmohan1234mnbNo ratings yet
- Successful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolDocument2 pagesSuccessful Management of Granulocytic Sarcoma With Co - 2016 - Pediatric HematolHawin NurdianaNo ratings yet
- Fonc 11 693386Document9 pagesFonc 11 693386Luana FerreiraNo ratings yet
- Biology ProjectDocument18 pagesBiology Project39 Aditiya DuttaNo ratings yet
- Retroviral Gene Therapy in Germany With A View On Previous Experience and Future PerspectivesDocument19 pagesRetroviral Gene Therapy in Germany With A View On Previous Experience and Future PerspectivesCarlos Meza HernandezNo ratings yet
- Viral Oncolytic Immune TherapyDocument8 pagesViral Oncolytic Immune TherapyKingNo ratings yet
- Hematolrep 03 E2 v2Document3 pagesHematolrep 03 E2 v2772450336No ratings yet
- Mrna 3Document8 pagesMrna 3api-675909478No ratings yet
- Module 12 - The Aspect of Gene TherapyDocument4 pagesModule 12 - The Aspect of Gene TherapyMark Daniel DeTorres GolisaoNo ratings yet
- Identification and Validation of Expressed HLA-binding Breast Cancer Neoepitopes For Potential Use in Individualized Cancer TherapyDocument12 pagesIdentification and Validation of Expressed HLA-binding Breast Cancer Neoepitopes For Potential Use in Individualized Cancer TherapydianaNo ratings yet
- Caac 21599Document8 pagesCaac 21599Kezia TindasNo ratings yet
- Gene TherapyDocument18 pagesGene TherapyAgnimitra ChoudhuryNo ratings yet
- Alderton 2012Document1 pageAlderton 2012NicoNo ratings yet
- BevazicumabDocument10 pagesBevazicumabmanuel barrientosNo ratings yet
- Neural Stem Cell RXDocument7 pagesNeural Stem Cell RXdupuytrenNo ratings yet
- PHASE 2 STUDY OF PEVONEDISTAT - AZACITIDINE VERSUS AZACITID - 2020 - HematologyDocument2 pagesPHASE 2 STUDY OF PEVONEDISTAT - AZACITIDINE VERSUS AZACITID - 2020 - HematologyFrankenstein MelancholyNo ratings yet
- HER2 PivotalTrialDocument10 pagesHER2 PivotalTrialapi-26302710No ratings yet
- Metastatic MelanomaDocument8 pagesMetastatic MelanomashokoNo ratings yet
- Imunoterapie EndocrinologieDocument17 pagesImunoterapie EndocrinologieClaudia IrimieNo ratings yet
- Fimmu 10 01205Document16 pagesFimmu 10 01205Vostie1811No ratings yet
- Infections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumFrom EverandInfections in Cancer Chemotherapy: A Symposium Held at the Institute Jules Bordet, Brussels, BelgiumNo ratings yet
- Bedah Saraf: Senin, 08 Agustus 2020Document2 pagesBedah Saraf: Senin, 08 Agustus 2020Arh SetiawanNo ratings yet
- B.ANAK 1-7 Nov 2019 Edit 10.31Document4 pagesB.ANAK 1-7 Nov 2019 Edit 10.31Arh SetiawanNo ratings yet
- Preop BS 10-17Document1 pagePreop BS 10-17Arh SetiawanNo ratings yet
- Uro 13-6-19-1Document1 pageUro 13-6-19-1Arh SetiawanNo ratings yet
- Bedah Saraf: Jumat, 23 Oktober 2020Document2 pagesBedah Saraf: Jumat, 23 Oktober 2020Arh SetiawanNo ratings yet
- Bedah Saraf: Senin, 08 Agustus 2020Document2 pagesBedah Saraf: Senin, 08 Agustus 2020Arh SetiawanNo ratings yet
- Preop BS 10-17Document1 pagePreop BS 10-17Arh SetiawanNo ratings yet
- Maping UrologiDocument2 pagesMaping UrologiArh SetiawanNo ratings yet
- OK 4 (DR - FE) OK 4 (DR - FE) OK 4 (DR - HS) OK 4 (Dr. FE) OK 4 (DR - HS) OK 4 (DR - FE)Document1 pageOK 4 (DR - FE) OK 4 (DR - FE) OK 4 (DR - HS) OK 4 (Dr. FE) OK 4 (DR - HS) OK 4 (DR - FE)Arh SetiawanNo ratings yet
- Ymj 56 139 PDFDocument7 pagesYmj 56 139 PDFArh SetiawanNo ratings yet
- 19052018Document3 pages19052018Arh SetiawanNo ratings yet
- Journal of Pediatric SurgeryDocument14 pagesJournal of Pediatric SurgeryArh SetiawanNo ratings yet
- Raynauds Disease.1Document14 pagesRaynauds Disease.1Pierre LaPaditeNo ratings yet
- Platelet-Rich Plasma: Support For Its Use in Wound Healing: ReviewDocument9 pagesPlatelet-Rich Plasma: Support For Its Use in Wound Healing: ReviewArh SetiawanNo ratings yet
- Platelet-Rich Plasma: Support For Its Use in Wound Healing: ReviewDocument9 pagesPlatelet-Rich Plasma: Support For Its Use in Wound Healing: ReviewArh SetiawanNo ratings yet
- Penatalaksanaan Pasien Cedera KepalaDocument21 pagesPenatalaksanaan Pasien Cedera KepalaA170riNo ratings yet
- Young 2016Document14 pagesYoung 2016Arh SetiawanNo ratings yet
- Penatalaksanaan Pasien Cedera KepalaDocument21 pagesPenatalaksanaan Pasien Cedera KepalaA170riNo ratings yet
- Penatalaksanaan Pasien Cedera KepalaDocument21 pagesPenatalaksanaan Pasien Cedera KepalaA170riNo ratings yet
- Young 2016Document14 pagesYoung 2016Arh SetiawanNo ratings yet
- Expended Program For Immunization (EPI)Document10 pagesExpended Program For Immunization (EPI)el_japonNo ratings yet
- Drug StudyDocument2 pagesDrug StudyKrysNo ratings yet
- Measles OutbreakDocument2 pagesMeasles OutbreakIdylah_Kionisa_9369No ratings yet
- Cis 2018 PDFDocument3 pagesCis 2018 PDFTara Oliveros Dela CruzNo ratings yet
- Emvolio Pilot Strategy DocumentDocument34 pagesEmvolio Pilot Strategy DocumentPrabir Kumar ChatterjeeNo ratings yet
- No Vaccination No EnrollmentDocument32 pagesNo Vaccination No EnrollmentRutchie Cabahug-AguhobNo ratings yet
- Louis PasteurDocument2 pagesLouis PasteurAlia Dzafrina100% (5)
- Air Borne DiseasesDocument3 pagesAir Borne DiseasesMuhammad Anwar GulNo ratings yet
- CV - Pramod JogDocument1 pageCV - Pramod JogMuthu KumarNo ratings yet
- Imt Request LetterDocument11 pagesImt Request LetterCHERYL CABRERANo ratings yet
- MOV - 1.2 Attendance Sheet For Social Mobilization-1Document2 pagesMOV - 1.2 Attendance Sheet For Social Mobilization-1PHO KALINGANo ratings yet
- Kidd Blood Group System (2Document4 pagesKidd Blood Group System (2RSH1987100% (1)
- MTB Second Edition Step 3 ErrataDocument9 pagesMTB Second Edition Step 3 ErrataDaniel I. SullivanNo ratings yet
- Echo - Medical Supplies and Equipment For Primary Health CareDocument192 pagesEcho - Medical Supplies and Equipment For Primary Health CareKing Solomon CatralNo ratings yet
- Laporan Vaksin 01112021 OkeDocument1,077 pagesLaporan Vaksin 01112021 OkeThewie ApydNo ratings yet
- Tropical Diseases An Unsolved ChallengeDocument9 pagesTropical Diseases An Unsolved ChallengeYet Barreda BasbasNo ratings yet
- Cryptococcal Antigen Latex Agglutination Test JOSEPHDocument14 pagesCryptococcal Antigen Latex Agglutination Test JOSEPHchocoholic potchiNo ratings yet
- Vaccine Storage Handling Guidelines enDocument24 pagesVaccine Storage Handling Guidelines enalexanderNo ratings yet
- Science - 31 October 2014Document182 pagesScience - 31 October 2014Martín LopezNo ratings yet