Professional Documents
Culture Documents
Samson Ethics Notes
Uploaded by
Ashish Bamania0 ratings0% found this document useful (0 votes)
208 views14 pagessamson ethics notes
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentsamson ethics notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
208 views14 pagesSamson Ethics Notes
Uploaded by
Ashish Bamaniasamson ethics notes
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 14
5:08 pm @ 19% E>
samsonplab.co.uk
MEDICO-LEGAL MEDICINE AND ETHICS 2016
Commitment to Professionalism
[A doctor should demonstrate ethical practice and commitment to professionalism therefore you must be open and honest
With patients if things go wrong. If a patient under your eare has Suffered harm or distress, you must
ut matters right (if that is possible)
Offer an apology
Explain fully and promptly what has happened and the likely short-term and long-term effects.
You must respond promptly fully and honestly to complaints and offer an apology when appropriate
You should end a professional relationship with 2 patient only when the breakdown of trust between you and the patient
means you cannot provide good clinical care to the patient.
In providing clinical care you must
Prescribe drugs of treatment, including repeat prescriptions, only when you have adequate knowledge of the patient's
health, and are satis that the drugs or treatment serve the patient's needs
Provide effective treatments based on the best available evidence
You must listen to patients, take account oftheir views, and respond honesty to theie questions.
You must work in partnership with patients, sharing with them the information they will need to make decisions about
their care, including:
‘Their condition, its likely progression and the options for treatment, including associated risks and uncertainties
‘The progress of their care, and your role and responsibilities in the team
Wino ie responsible for each aspect of patient care, and how information is shared within teams and among those who
will be providing their care
You must give patients the information they want of need to knov in 2 way they can understand. You should make sure
that arrangements are made, wherever possible, to mest patients” language ang communication needs.
Prescription
Ensure that your prescribing ie appropriate and responsible and in the patent's best interests
Doctors are able to prescribe unlicensed medicine, but before doing so they must be satisfied that an alternative,
licensed medicine will not satisfy the patient's naeds. When prescribing offlicence, a doctor would need to take
responsiblity for oversecing the patient's care including monitering and any flloy-up treatment.
Good Medical Practice requires doctors to take account of the patient's views, support patients in caring for themselves,
and listen to patients, take account of their views, and respond honestly to thelr questions. However, GMC does not
‘expect doctors to compromise their clinical judgement in order to suit a patent's preferences.
[As long as a doctor genuinely feels that that they treatment they have recommended would be in their patient's best
clinical interests, they would not be acting against our guidance by refusing to prescribe an alternative treatment
Fequested by the patient. Doctors should only prescribe drugs to meet the identified needs of patients, and never simply
because patients demand them.
Maintaining trust in the profes
It wouldn't usually be appropriate for a doctor to raise the issue of their own personal beliefs in the course of a
consultation. If a doctor does find it necessary to explain their personal baliefs to patients (perhaps because - as in this
case study - it affects the treatment they provide), the doctor must be careful not to cause the patient distress
You must not ask for or accept - from patients colleagues o others - any inducement, gift or hospitality that may affect
lor be seen to affect the way You prescribe for, treat of refer patients or commission services for patients.
ov
II benefit to the patient
Whenever @ doctor provides or arranges treatment for a patient, they must do so on the basis of what would be of
fverall benefit to the patent. While the vast majonty of treatment dacsions will be medically indicated, the potential
benefits stretch beyond striciy medial interests to include, for example, peychological factors. This i= the case with
‘much cosmetic surgery - the doctor decides that the risks of surgery are cutweighed by the potential improvement in a
patient's mental health and general wellbeing that a positive outcame could achieve,
‘Autonomy and Privacy
Respact patient's autonomy and privacy
Doctors must be careful when using information about patients. It is important that the patiant has given consent for
the doctor to use their information in this way, whather or not the doctor believes thatthe patient can be identified from
the information,
8 pm @ 19% E>
samsonplab.co.uk
‘Autonomy and Privacy
Respect patient's autonomy and privacy’
Doctors must be careful when using information about patients. It is important that the patient has glven consent for
the doctor to use their information in this way, whether or not the doctor believes that the patient can be identified from
the information.
Even if the intended use is teaching, rather than something more easily accessible to the public, the doctor must take
care to ensure that the patient is not identifiable from the information.
Children and Young people (0-18 Years)
Doctors should ahvays actin the best interests of children and young people. This should be the guiding principle in all
Gecisions which may affect them, But identifying theic best interests ls not always easy. This is particularly the case in
relation to treatment that does not have proven health benefits or when competent young people refuse treatment that
's clearty in their mecical interests, There can also be a conflict between child protection and confidentiality, oth of
which are vitally important to the welfare of children and young people
[An assessment of best interests will include what is clinically indicated in a particular case. You should also consider:
the wiews of the child or young person, so far as they can exprass them, including any previously expressed preferences
the wiews of parents
the wiews of others close to the child or young person.
the cultura, religious or other beliefs and values of the child or parents
the wiews of other healthcare professionals involved in providing care to the child er young person, and of any other
professionals who have an interest in their welfare
lich choice, if there is more than one, wil least restrict the chil or young person's future options
You should talk directly and listen to children and young people who are able to take part in discussions about their
care. Young people who are able to understand what is being said and who can speak for themselves resent being
spoken about when they are present. But younger children might nat be able to understand what their illness or
Dropored treatment is likely to involve, even when explained in straightforward terms.
Both the GMC and the law permit doctors to undertake procedures that do not offer immediate or abvious therapeutic
benefits for children or young people, so long as they are in their best interests and performed with consent
To assess their bast Interests you should consider the raligious and cultural beliefs and values of the child or young
person and their parents as well as any social, psychological and emotional benefits. This may be relevant in
CGroumcision of male chilren for religious or cultural reasonels, of surgical correction of physical charactensics that do
rot endanger the chi’ lfe or heath
If providing treatment to children, you should be familiar with the detailed advice in 0-18 years: guidance for all
doctors, which includes the key points set out in this section of guidance. You should take particular care if you consider
providing cosmetic interventions for children or young people - you should make sure the environment for practice is
Appropriate to paediatric care, and work with multidistipinary teams that provide expertise in treating children and
young people where necessary
You must only provide interventions that are in the best interests of the child or young person. If a young person has
capacity to decide whether to undergo an intervention, you should stil encourage them to Involve their parents in
‘making their decsion.
[A parent can consent to an intervention for a child or young person who does not have the maturity and capacity to
‘make the decision, But you should involve the child in the decision ax much as possible. If you judge that the child does
rot want to have the cosmetic intervention, then you must not perform i
Assessing Best Interests
Doctors should always act in the best interests of children and young people - this should be the guiding principle in all
Gecisions that afect them. But in some situations, it can be difficult to Identiy what isin the chlés best interests.
This is particularly the case when considering interventions carried out for social, cultural or religious reasons, such as
ear-pinning or non therapeutic circumcision. While clnial factors play a significant rele in determining best interests,
{octors must also consider other factors, such as the views of the child and their parents
0-18 years: guidance for all doctors and our Cosmetic interventions guidance, states that children and young people
should be involved in decisions about their care and that doctors should listan to and respond to their concems. Far
cosmetic procedures such as pinnaplasty if a doctor considers that the chil doesn't want the procedure then they must
rot perform it
Divorce and Parental Responsibility
Divorce does not affect parental responsibilty. Parents are usually best placed to judge what is in their chil's best
Interests, at least until their children are mature encugh to make those decisions for themselves. However, it can be
challenging for dactors when parents da not agree on what's best for ther chil
0-18 years: guidance forall doctors provides advice on who has parental responsibil. Doctors should remember that
divorce or separation does not affect parental responsiblity. Everyone with parental responsibilty should be involved in
any important discussions about their chile's treatment, and given reasonable access to the medical records, as long as
this doesn't confct with the child's best interests. This wil usualy include both natural parents, and might include a
local authorty and others if, for example, 2 child isin care, It might be appropriate to involve others close to the chil
who regularly care for them, even if they dont legally have parental responsibilty
5:08 pm @ 19% m>
samsonplab.co.uk
Divorce and Parental Responsibility
Divorce does nat affect parental responsibility. Parents are usually best placed to judge what is in their chil's best
Inerasts, at least until their children are mature enough to make those decisions for themselves. However, it can be
challenging for dactors when parents do not agree on what's best for their chil
0-18 years: guidance for all doctors provides advice on who has parental responsibilty. Doctors should remember that
divorce or separation does not affect parental responsibilty. Everyone with parental responsiblity should be involved in
any important discussions about their child's treatment, and given reasonable access to the medical records, as long as
this doesnt conflict with the chil's best interests. This will usually include both natural parents, and might include a
local authority and others f, for example, 2 child is in care, It might be appropriate to Involve others close to the chil
wo regularly care for them, even if they don't legally have parental responsibilty.
der children and young people who understand what it entails should be consulted and asked to agree to their parents
being sven access to their madical records.
Work with other professionals
[A doctor should seek the views of other professionals
Wile it f= usually suffcient to have consent from just one parent, doctors should work with both parents where
possible, to try to informally resolve disputes that may occasionally arise about the child's treatment. Seeking the views
Of others whe are involved in the care of the child may help to achieve this, by giving a clearer picture of where a
chila’s best interests li,
Other members of a multi-dsciplinary team, or ather professionals who have an interest in the chlé's welfare, such as
teachers or socal workers, may be able to provide helpful input. I i is not possible to resolve a dispute about an
Important decision informally, it may be appropriate to seek legal advice about applying to the court for a determination
fon whether the treatment proposed isin the child's best interests.
Coping with Pressure
Obstacles of sharing information
All doctors know that our medical practice is affected in some way by our limits on time or other resources. Finding 2
way to make best use of those resources can be a challenge, particularly when doctors have to balance the needs of the
Individual patient with those of al the patients using a particular service
Where time pressures prevent them from spending as much time with patients as they'd tke, doctors should consider
what other means they could use to ensure that patients have all the information they want or need about thelr
Condition and any proposed investigation or treatment. Clear, up to date written information can be very helpful, as can
Getalls of good quality online or other reference sources.
Doctors don't practise in isolation, and they ray wish to explore what role other members of the healthcare team might
play in providing patients with advice and support
Effective Communication
Openness, trust and good communication
Everyone knows that doctors’ time is limited, but taking time to bulld trust and encourage patients to take an interest in
their own healthcare can save time later on. Honesty Is also crudal to a trusting doctor-patient partnership, and it iS
Important that doctors are honest about the limits of their knowledge. It's fine for doctors to discuss with patients any
policies and procedures that might restrict their practice, as this can help patients to understand their matives, building
trust and encouraging patients to comply with treatment.
Listen to patients
Doctors must listen carefully to what patients have to say, and what they're particularly concerned about, even if it
seems obvious straight away what the problem is. Many patients ~ particularly those with long-term conditions - are
‘experts in their condition, and how they experience living with it. I's a doctor's duty to encourage patients to use this
knowledge to enable the patient to make informed decisions about their care.
You must listen to patients, take account of their views, and respond honestly to their questions
You must give patients the information they want or need to know in @ way they can understand. You should make sure
that arrangements are made, wherever possible, to mest patient’ language and communeation needs,
Responding to patients’ questions is also very important. It doesn’t mean doctors have to take time to answer every
single question however irelevant it may be; f just means that they should respond, even i i's to assure them that i's
Effective communication between doctors and children and young people Is essential to the provision of good care. You
should find out what children, young people and their parents want and need to know, what issues are important to
5:08 pm @ 19% E>
samsonplab.co.uk
Effective communication between doctors and children and young poople is essential to the provision of good care. You
should find out what children, young people and their parents want and need to know, what issues are important to
them, and what opinions or fears they have about their health or treatment. In particular you shoul
Involve children and young people in discussions about thelr care
bbe honest and open with them and their parents, while respecting confidentiality
listen to and respect their views about their health, and respond to their concerns and preferences
explain things using language or ether forms of communication they can understand
Consider how you and they use non-verbal communication, and the surroundings in which you mest them
‘ve them opportunities to ask questions, and answer these honesty and to the Dest of your abllty
o all you can to make open and truthful discussion possible taking into account that this can be helped or hindered by
the involvement of parents or other people
dive them the same time and respect that you would gle to adult patients
Give information at an appropriate time and pace
Just lke adult patients, children and young people want and need information about their health and should be involved
in discussions about their care. However, itis important that they are net overburdened, and that information Is
provided in 2 manner appropriate to their understanding.
[At times, parents may want to protect their chiiren from upsetting or complex information. However, doctors have a
uty to be honest with all thelr patients, and this includes chlgren and young people, This can present a challenge if
they are asked to withhold information, but itis Important to bear in mind that the doctor's primary duty is to their
patient.
This does not mean that the views of parents should be disregarded: they are an integral part of assessing a child's best
Interests, Nonetheless, actors should not withhold information from a chilé or young person vino is capable of
Understanding it, unless they ask not to be told, ar unless providing the information would cause them serious harm,
‘The doctor needs to assess the child's capacity to understand the implications of his dlagnosis, before agrasing with the
parents! request not to inform him of the diagnose,
Refus
of Treatment
Doctors face a lificult dlemma when a young person with capacty refuses treatment that the doctor considers to be in
their best interests, This is particularly signifeant when the treatment is necessary to save the young person's life
Doctors should respect a young person's views about their health, as they would any other patient's, but this must be
balanced against the doctor's duty to actin their patent's best interests
‘The law in this area i complex, and differs across the UK. You should seek advice if you think treatment is in the best
Interests of a competent young person who refuses. Having said that, it Is usually preferable to try to resolve such
‘sues informally.
1 is essential that the young person, and their parents, have been provided with all the information they need to make
an informed decision. Often, other members from the multidisciplinary team may be better placed to provide this
Information to the young person,
Doctors may ask a counsellor with experience in working with young people to speak to to the child to try to Identify
his/her concerns, so that they can be appropriately addressed. By agreeing to Involve the child in reviewing his
treatment, the doctor is demonstrates respect for the child's views and ensures that he is involved in the decision-
‘making process.
You must provide a good standard of practice and care. If you assess, diagnose or treat patients, you must
‘Adequately assess the patient's condition, taking account of their history (including the symptoms and psycholoaical
spintual, social and cultural factors), their views and values. Where necessary, examine the patient.
You must treat patients as individuals and respect theic dignity and privacy
You must give patients the information they want of need to know in 2 way they can understand. You should make sure
that arrangements are made, wherever possible, to mest patients” language ang communication needs.
You must be satisfied that you have consent or other valié authority before you cafry out any examination or
Investigation, provide treatment or involve patients or volunteers in teaching or research
How you discuss a patient's clagnasis, prognosis and treatment options is often as important as the information itself
You should share information in @ way that the patient can understand and, whenever possible, ina place and at a time
when they are best able to understand and retain it.
You should check whether the patient needs any additional support to understand information, to communicate theit
Wishes, of to make a decision, You should bear in mind that some barriers to understanding and communication may
rot be’cbvious; for example, @ patient may have unspoken anxieties, or may be affected by pain or other underlying
problems.
5:08 pm @ 19%
samsonplab.co.uk
You must make sure, wherever practical, that arrangements are made to give the patient any necessary support. This
right incluce, for example: using an advocate or Interpreter; asking those close to the patent about te patient's
communication needs; oF giving the patient a wnten of audio recaré of the discussion and ary decisions that were
ade
Mental Capacity
You must work on the presumption that every adult pationt has the capacity to make dacisions about thelr care, and to
ecide whether to agree to, oF refuse, an examination, vestigation or treatment. You must oriy regard a patient as
lackng capacity once it is clear that, Raving been given all approprate help and support, they cannot understand
retan, use oF weigh up the infermation needed to make that decsion, er communicate their wishes.
You must not assume that 2 patient lacts capacity to make a cecision solely because of their age, disability,
appearance, behaviour, medial condition (including mental ess), their beliefs, their apparent. inabilty to
communicate, or the fact that they make a cecsion that you disagree with
[A patient's ability to make decisions may depend on the nature and seventy of their condition, or the dificulty or
complexity ofthe decision,
Ifa patient's capacity is affected in this way, you must [take] particular care to give the patient the time ané support
they need to maximise their ality to make decisions for themsalves, Far example, you will need to think carefuly about
the extra support needed by patients with dementia or learning disables.
You must take all reasonable steps to plan for foreseeable changas in a patient's capacity to make decisions. Ths means
that you should
iscuss treatment options in a place and at 2 time when the patient is best able to understand and retain the
Information
ask the patient if there is anytning that would help them remember information, oF make it easier to make a decision;
Such as bringing a relative, partner, fiend, carer or advocate to consultations, or having written oF audio information
‘bout their condition or the proposed investigation or treatment
Speck to those cles to the patent and to other healthcare staf about the best ways of communicating with the patient,
faking account of confidentiaity issues
Ifa patient is likely to have dfficuity retaining information, you should offer them 2 written record of your discussions,
Getaling what decisions were made and why.
You must assess a patiant's capacity to make a particiar decision at the time it needs to be made. You must not
assume that because a patient lacks capacity to make a decision on 2 particular occasion, they lack capacity to make
{ny decisions at al, or will not be able to make similar dessions in the future.
If your assessment is that the patient's capacity is borderine, you must be able to stow that tis more likely than not
that they lack capacity,
If your assessment leaves you in doubt about the patient's capacity to make a decision, you should seek advice from:
rursing staff or others involves in the patient's care, or those close to the patient, who may be aware of the patient's
Usual ablity to make decisions and their particular communication needs
colleagues with relevant specialist experience, such as psychiatrists, neurologists, or speech and language therapists
if yeu are still unsure about the patient's capacity to make a decision, you must sect legal advice with a view to asking
1 court to determine capacity
Maximising a patient's ability to make decisions
Doctors must werk on the presumption that every adult pationt has the capacity to make decisions about thei care, and
to decide whether to agree to, oF Fefuse, an examination, investigation of treatment.
[A pitient’s ablity to make decisions may cepend on a number of factors - the mature and severity of their medical
canciton, the complexity of the decision, even the consultng-reom envranment. For example, Shannon may be agitated
and upset by beirg at the doctor's surgery, as well as by feeling unwell.
Because of this, doctors must take all reascnable steps to maximise a patient's capacity to make a particular decision,
such as holding consultations at a time ard in a place where the fatient feels more comfortable; or using written
‘material and clagrame to help patients understand thelr diagnosis and treatment options
Consider the views of people close to the patient
‘An hicreasing number of patients with capacity issues may have someone with the legal power to make decsions on
their Behalf. But, even when this isnot the case, ts important - with the patient's consent, where possible - t involve
Carers in the discussion, whatever the level of the patlents learning disailty
Doctors must listen to carers, taking thelr views into account - bath when assessing the patients capacity and if they
have to make a best-intereste or Benefit decsion about treatment.
‘Treat patients as individuals and respect their dignity
1 important t2 involve the patient in the conversaton a= much as ie possibie, communicating with them in a
respectful way but also listening to what the carer has to say. A good technique is to ask the patient questions directly
Pad =
5:08 pm @ 19%€>
‘samsonplab.co.uk
‘Treat patients as individuals and respect their dignity
1 Is Important to involve the patent in the conversation 25 much as. pessibie, communicating with them in a
respactfel way but also listening to what the carer has to say. A good technique is to as the patent questions directly
‘while vorying the ancwors with ther oror
Patient focus
‘You must support patents in caring for themselves to empower them to improve and maintain ter neain. This may,
for examle include improve ard maintain ther health. This may, for example, includ:
Supporting patients to make lifestyle changes where approprats
‘Act immediately to put things right
themselves to the patient (or their relatvas) whether or not they were personaly responsible for the incident. Guidance
from the NHS Litgetion Authority confimms that en apolegy & not an edmissien of liaity ~ which is e concern thet
some doctors have about apolgising. GHC guidance (In Good Medical ractce) states that an apology shoud be offered,
But itis more important that the doctor explains fuly and promstly what's happened, and what are likly t2 be the
effects in bath the short ard long term.
treatment they provide or ararge.
Protect patients from risk of harm
If a doctor suspects that 2 colleague may not be it te practise, they must take steps immediatly to ensure that
patients are protected. THs will usually mean informing the doctor's employer and ~ for more serous cases - their
Feguater, the GNC. It may ‘ot be necessary tf laform the GNC about a” coctor ifthe complaint can be hardled
‘The doctor's employers are in a better positon to act quickly 10 assess a stuation and ensure patent protecten than a)
national body tke the GMC. However, if there isa possibilty thatthe doctors right to practise may need to be restrcted
Or removed, the GMC must be inforred as wel.
Work in partnership with patients
‘The Intomation tat 2 doctor wl give to a patient wil vary ‘om patant to paterE. Seme patients wil want to know
everything about possible side effects of treaimert, Fowever minor, and thers would be happy with the pare
sential,
Neverthsiess, doctors should tll patierts about likay site efacts, with an emphasis on anything that they may be
partculaly conceined about. Discussing isk can be a complicated mater. For some treatments Ik would be impractical
fo talk 2 patent thraugh every possible risk, Eut cot dcussing risk at all can sndermine a patients confdence in
If, ster discussion, @ patient still éoes not want to know in detall about their condition or the treatment, you should
consent to a proposed investigation or treatment. This is likely to inclide what the investigation or treatment aims to
chive and what it wll ivolve, for example: whether the procedure is imasive; what lvel of pain er discomfort chey
‘might experience, and what can be done to minimise it; anything thay shoule do to prepare forthe investigation oF
freatment and it involves any serious "sks,
[A balance must be stuck, ané doctors should discuss with patients any risks which are likely to oczur, and any that
‘may be of particular concern to them, and = where appropiate ~ refer them to ether soutces of tvormatin, such as the
leaflets accompanying prescription medicines
GGuicing 2 patient through the risks ard benefis of each avaliable cotion and emphasising wich option the dector
belles fo be best for them, and wy, wil enable patcnts to make informed cheices
Clear, accurate information about the rsks of any proposed investigation or treatrant, should be prasented in a way
patients san understand, can help them make informed decisions. (ne amount of information abovt Fick that You emould|
Share with patients wil depend on the individual patient and what they want or need to krow. Your discussions with
patients shoud focus en their Individual stuation and the rsk to them.
You must tall patians if an investigation or treatment might result in a sericus adverse outcome, even ifthe lkellhoed is
very small. You should alo tell patients about less serious de effecis or complications W Mey occur frequenty, and
‘exphin what the patient should do F they experience any of them,
Guidance on Personal beliefs
”
19%
5:08 pm,
‘samsonplab.co.uk
‘Guidance on Personal bellets
Al patients are enttied to treatmant and care to maet thelr clinical nesds.
‘he GMC publishes guidance relating to personal beliefs - both dectore' and patents. Ths aims te clanfy whether ard to
‘he guidance allows the night to say ro to @ particular procedure, but not to a particular patient er grcup of patents:
tat woule be gisermination
(GMC guidance does not require coctors with a conscientious objection to aborton ta refer patiants, even to anather GP,
provided that patents ae able to access alteraative care in good time. If patients don't have easy access to ether care
Eptione, dapanding on tre urgency, the GMC woulé expect doctors te ba propsrad to zet anda ter personal Bais In
crder to provide efactiva patient care.
Expressions of consent
Before accepting a patient's consent to treatment, the doctor who will Be proving the treatment must be satisfied that
tie patients consent Is vald. A signature on a form does rot, of Half conta that ths isthe case. Ifa patient Nas
‘consented to 2 planned investigation or treatment, but stil has questions or reseniators about &, the doctor proving |
{hat eeatment should make sure that thess concerns are propery adcreasea
The law requires that written cansent must be obtained for certain procedures, such as fertity treatment. It's also
Investigation o treatment is complex or if Invelves sigaificant risks "
Before accepting a patient's consent to treatment, the doctor who will Be proving the treatment must be satisfied that
te patients consent is valé. A signature on a form does rot, of Isai, contm that ths isthe case. Ifa patient nas
Consented to 2 planned investigation or traatment, but stil has questions or reseniators about &, the doctor roving
that teatment should make sure that these concerrs are propery aderessed
The law requires that written cansent must be obtained for certain procedures, such as fertity treatment. It's also
Investigation of treztment is complex or if Involves significant risks. "
Responsibility for seeking a patient's consent.
that seeking consent Is an end in tse, and semething that doctors co to patients. "Conseniung” is also frequently seen
In the GMC Consent guidance, tne GMC makes cles that ascussing consent shoula be an intagral part of tne:
consultation wth the patient. It's the responsibilty ef the doctor who is performing an invastigation or proving
{Peatmentto ensure thatthe patient has gven valié consent,
‘he coctor can delegate the responsiblity for seeking consent, as long as the person to whem they delegate is suitably
the treatment, and the risks attechet to it. However, i's the doctor doing the procedure that remains responsible for
‘Treat patients as individuals and respect thei
dignity
1k is important to involve the patient in the conversation as much as is possible, communiating wih them in 2
respectful way but aloo listening #o whet the carer has to sey. A.good tacinique ic to gok the petiant quastions cisely
while verifying the answers with their care.
\When treating patients with disabilities, there & a rek of what's known as ‘elagnoste overshadowing" «where
symptoms are interpreted as being part of the patient's current condition o” disability rather than another, new,
cancion,
“ha aim should be the minimum diversion from the norn, finding the least buréenseme way af providing the necessary
treatment that hest mects the epaciic needs of each incvidkal patient.
refusal of treaimert: ifthe patient does not have the capacity to consent, the patient then aso goes not have the
(pacty t retise, In tose circumstances, wnicn are undaval, @ cession must Oe mace basee on the patients best
Interests or overall benefit
IF anvone close to the patient wants to discuss their concerns shout the patiant's heath, you should make I clear to
tham that, whle itis not a breach of confdertaliy to listen to their concerns, you carn guarantee that you will not
thers, for example, IF it has influenced your assessment and treztment of the patient.
You srould not refuse to listen to a patient's partner, carers or ethers on the basis of confidentiality. Their views or the
Information they provide might Ee helpful in Your care of the patient You wil, theugh, need to consider whiner your
fatient would consider you listening to the conceme of others abou: your patient's health or care to De a breach of
‘ust, particularly If they have asted you nat te listen to partcular pecple.
Section 27 ofthe Data Protection Act givas patients the right to have access to thei personal infermation; but there are
”
19%
5:08 pm,
‘samsonplab.co.uk
Section 27 ofthe Data Protection Act gives patients the right to have access to ther personal infermation; but there are
some exceptions. For examele, you do rot Fave to supply a patient weh information about ancther person or that
antes another person az the source ofthe information, unl that other person consents of ft is reazonable in the
Informing the DVLA or the DVA
‘he Driver ané Vehicle and Licensing Agency (DVLA) and Oriver and Vehicle Agency (OVA) are legally responsible for
ceeidng if @ person is rieclaly unnt to erve. This means they need to Know Ifa anvirg licence noleer mas a conation|
or is undergoirg treatment that may row, oF inthe future, aft their safety as a criver
So thay have to know ifa criver has a condition that may now, oF in the future, affect their safety as a ceiver. While i
Is the driver themselves who is legally responsible for informing the DVLA or DVA if they have such a cendition, there
rive, and that they have a legal duty to inform the DVLA or DVA about the condition thamseives
You should se2k the advice of an experianced ealeague er the DVA ex DVA's medical sdvisar if you are not sure
whether a patient may be unfit to drve. You should keep under review any decision that they are fit, particularly F the
fate concltion or treatments change. The DVLA's publication For Medial Pracstioners = At a glance Guia to the
furrent Medica Standards of Fness to Drive includes information about 2 varoty of dsorders and conditions that can
‘he erwver Is gall responsible for informing the OVLA oF BVA about such a cundition or treatment. However, I a
patient has such @ condtion, you should explain to the patient
(@) that the condition may affect their ability to drive (ifthe patient is incapable of understanding this advice, for
example, secause of dementa, you should inform the OYLA or DVA immetdatei), and
{@) that they have a log city te inform the DVLA or BVA about the canton
1 2 patiere continues ta are when they may aot be ft ta doo, and it their doctor has mace every reasonable etter
to persuade them to stop then the doctor shoud contact the DVLA or OVA immadiately, teling the patent ‘st # thet is
possible
A confidential sexual
th services for the welfare of children and young peop!
CCilden and young pecple need to be able te access neath services confidentially and for those who do not want to
share ther personal health information witha parert or guardian, this means being able to access them alene.
what they wart. Ths ie partculary Imporant in the arsa of sexual health: eencem about confgentiliy ' the bicgest
eterrent nfen it comes to young people asking for sexual health advice. f young people dint fel able to seek advice
bout sexual haalth that presents a canger to ther heath, that af other young pecple and te health ofthe cemmunity
35.2 whole. Parents may hot be aware that their child = sexually actve, but ffs Geary In the childs best interests to
ave access to care and advee where necessary
0-18 years: guidance forall doctors recommends doctors think careilly about the effect the prasence of a chaperone |
‘an have! they can deter yeung people fram being frark and apan, and they may not be as likely to ask for help with
‘whet really woublng ther
The capacity to consent (Contraception)
‘As wth any patient, the doctor must decide whether the child er young person is compatant te mate decisens about
‘he doctor should make sure that the patient understands the implications of taking the pil ané of not taking the pil,
the risks and side-effects, other options for contraception, before he/she prascnbes it for her. If he/she fnds that the
ratient doas not have capacty to consent. she would not be in a postion to prescribe, although the doctor should stil
eop the consultation cenfidental
‘hough dector can try ta persuade the patient to speak to her parents, in the end the doctor could decide to prescribe
te pill wthout ther knowledge. This Iz because he/she judges that the patient understands the implications, and that
she is lkaly te continue to have sex whether or not ha/she prescribes the pil. That would rur the risk of unwanted
bregrancy and the doctor judges thatthe patient's best Intrests are served by prasenbing tre pl
Protecting children from abuse and neglect
sexual activity, the doctor must protect them by sharing relevant information with appropriate people or agencies,
USualy chicren’s seal services.
”
19%
5:08 pm
‘samsonplab.co.uk
Protecting chil
iren from abuse and neglect
0-18 years: guidance fer all doctors states that if a child er young person is invelved in abusive or seriously harmful
sexual activity, the doctor must protect them by sharing relevant information with appropriate people or agencies,
Usualy chidren's secial services.
Consider the potential adverse consequences, Docars must also consider the impact that sucr a dlscooure and its
‘As woh any disclosure, the doctor should tall the child or young person what they propose to asciese, to whom, and
\hy. The only exception to this if forming the chilé of the disclosure would undermine the purpese (for example if
they are likely to help an abuser evade the polce) or if would place them at increased risk of harm.
The coctors' frst concem must be the safety and welfare of chilren and yourg people. They must promptly inform an
propriate parton ar authonty of any rascanable conctrn tht 2 chid or young porcen iz st nck of shure, Whathar 9
Goctor decides to disclose or not, they should record thelr decision and the reasoning tehind it. Doctors will be abe to
reasonable belief, and through the appropriate cham.
0-18 Guidance for doctors
\When tresting aduts who care for, oF pose risks to, children and young people, the adult patient must be the doctor's
fret concer; but doctors must aed considar ang ac n ne best nterest ef chicren ane young peopl
|i may be appropriste to encouraze patients to consent to declosures you cansder necessary for thei protection, ard to
warn them of the risks of refusing to corsent: but you should usualy abide by a competent acult patient's refusal to
Consent to lecosure, even ther decision leaves tam, but nabady else, at rs of sercus harm,
You should do your best to provide patients with the information and support they naeé to make decsions in thelr own
Disclosure without consent
Clsclose may expose others to a isk of death or eeraus harm. Yeu should sil seek the patent's consent to csclasure if
practicable anc consider any reasons given for rerusal
Such a situation might arise, for example, when = disdosure would be Ikely to assist in te prevention, detection of
prosecution of serous crimeespacially crmes aganst the perstn. When victms of vislence refuse police assistance,
fisclasure may stil be justified If others remain at sk, for example, from someone whe Is prepared to use weapons, oF
and the public interest h maintaning confdentalty, or if sls net practicable or safe to seat the patients consent, you
should disclose information promptly to an apprepnate person or autfonty. You should inform the patient before
Aisclasing the information, if pracicable and sae, even f you intend to disclose without their consent.
Documents you mate (Inclucing dinical record) to formally fecord your werk must be clear, accurate and lable
‘elovant ciniea!fincings
the decisions made and actions agreed, and who Is making the decisions and agreeing the actions
the information given to patients
ny rugs prescribed or other investigation or treatment
who is making the record and when.
Conflicts of interest,
1. Any inducement gift or hospitality.
You must make sure that your conduct justifies your patent! trust in you and the publi’ trst inthe profession
You must not ask for or accept - from patiants, colleagues or others - any inducement, cit o* hosptalty that may affect
Good Meacal Pracice states that doctors must not ‘ask for er accept - trom patients, colleagues or others - any
Inducsment, git or hospitality that may affect or be seen to affec: the way you prescribe fr, treat or refer patients
ven if docter is certain that a lft or osoitality wil
rot afect nis or her aroiesslnal tidaement, if ti other necne's
”
5:08 pm © 19%€
‘samsonplab.co.uk
1. Any inducement gift or hospitality.
You must make sure that your conduct justifies your patent! trust in you and the publi’ trst inthe profession
You must not ask for or accept - from patiants, colleagues or others - any inducement, cit o° hosptalty that may affect
cr be seen to affect the way you prescribe for, treat of rafer patients or commission serices for patients
Good Metical Pracice states that doctors must not 'ask for ar accept - from patients, colleagues or others - any
inducement, ot or hospitality that may affect or be seen to affect the way you prescribe for, treat or refer patients
perception that if might do, then this could sil have’a negative Impact by undarmining those peosle's confidence In
‘er own doctors, and public vust Inthe profession
2, Relationships with former patients
Not al! personal relatinsnips aetwsen doctors and thelr former patents Involve an abuse of the professonal
relationship. It can be helpful for someone in the doctor's positon to consider what would happen if the relationship
broke up and 2 complaint were made about the doctor's cancuct.
A significant proportion of the complaints about doctors’ alleged appropriate relationships with patients come from the
patlat themsever afer the rlatanstip har ended, ftan actmoniousy, from the patents panner or ox parener
Docters should ask thenselves if they would be able to JUSUIY thelr actions If such @ complaint were to be made about
em,
Inappropriate relationships wth patients come from the patiantthemstlves after the relationship has ended, often
acrimaniously, oF from tre pation’s partner or ex partner ~ as happens inthe ease study. Doctors should ask
relationship locks to others, and whether t might damage wider public trust in the medical profession.
People must be able to dscase configential medica information about themselves, and otherwise confide in their doctor
without worrying that their doctor might rake sexual or emetional advances
Child protection
Docters play a crudal role in protecting children from abuse and neglect. You may be teld or notice things that teachers
and social workers, for example, may not. Yeu may have access to corvidertial information that causes you to have:
Cancer fer the safety or well-being of children,
Children, young people and parents may not want you to disclose ‘formation atout them if they think they wil be
denied hep, Hamed or meds to feel ashamed. They might hove hod bed experiences of fear contact withthe police oF
Socal senices. You should Felp them understand the importance and benefits of staring information. But you must not
Gelay sharing relevant information with an appropriate person or authonty if day would increase the isk to the chid oF
‘young person or to other chiren or young pecple
Confidentiality is important and information sharing should be preportionate to the rk of harm. You may share some
Imitad information, with consent f possible, to decide if there isa risk that would justify further lsclorures, A nk
right only Become apparent when 8 rumbar of pasple with nigging concame wil usually act ac 4 central co-ordination point ae they hold information about the patient's history and
current treatment and care, and have arranged or be aware of specalist investigations and referral.
Most pationts understand the importance of sharing information batween the various health professionals involved in
thar care, aut some patents are reluctant to agree to it. Ths Is the case wen Mrs Ford, who fas lst trust In her GP.
\Winere such a situation arses, the doctor mest balance the patient's wishes agains: the risk of faling to pass information
atout the patient’ trzatment and care en to thelr GP.
Responsibilities of an expert witness.
Expert witnesses. are essential to the judicial and tribunal systems and can help to resolve disputes by providing
specialst knowledge, Oocors can act ar expert witnesees in a wige range of cares ard itis important tat rose who
[Al dowors are expected t be honest and trustworthy at al times = Including when wailng feports and giving evidence ~
{rd to take reasonable steps to ensure that the information they provide i= nat incomplete or misleading, Doctors,
Including expert witnesses, must alo be clear about the limite t tae knowledge and competence,
If doctors are asked to cive evidence outside their area of expertise, they must either decline the invitation, oF they
must make t very clear that they are unable to cive ‘expert’ evidence on the aoint at issue,
Disclosure in Public interest
GHC guidance on confidentiality states that disclesures can be made in the public interest without a patient's consent ~
Ard, exceptionaly, where a patient hae withneld consent «if the disslosire wil assist in the prevention or detection of 2
hare is a genuine concern that advising doctors to repert knife wounds may put off victims of cime from seeking
treatment. Sut mat concern needs to be baanced against tne risks Inherent In serous crimes going unreperted. While
the fac thet a patiert has presented with a gunshot wound or an injury fram a krfe atack should always be reported =
ard quickly = Goctors need to make a judgement on the facts of each case about whether to share. cenfigental
Invormation
Patients rightly aesume that inférmation abaut them will be held in confidence by their dactore, but there are
cumstances where It sin the public interest to disclose certan information, even if patients object
The pice should be informed quickly whenever a pationt arives with an injury from an attack with a knife, blade or
ober srarp instrument. wren doing s, the doctor sheula aot gve the patients name.
Doctors must make a decision in the public interest about whether to dscose information about the patient, including
their ldentiy. Information likely to assst the pele m praventing. detecting and prosecuting serious crime, especially
crme against the parson, usually can be justfiad as being in the public Interest.
Responding to criticism in the press
Sometimes press stories may report inaccurate er misleading details about @ doctor's diagrosis or behaviour towards 2
peftasar patient. However distressing this may be forthe doctor invowad, If they decide to respond to the critlsm
they must be careful not to breach patient confidetilty by disclosing personal information abeut the patient, or
revealing an account of tair care. Even the simple Genial ar spec allegations caulé reveal mere personal Inrormauen
‘tout the patient than a basic denial woul,
Doctors have a duty to ensure that thelr conduct justifies oubic trust in the medical profession. That trust can be
Underminee by disputes betwesn patients and doctors conaucted in the media
However, if press reparts cause patients to be concerned about a particular doctor's - or their hospital's ~ practice, it
Giving general irformation about their normal pratice ar about normal hespital poly.
Assessing advance refusals of treatment
established in lav. A valié and applicable advance refusal of treatment has the same effect as a refusal of treatment by
‘Advance refusals may come in many forms, rancing trom 2 generaised verbal reusal noted in a patient's records to 2
Getaled ‘ving will type documert. It is for the dector arranging care to assass whether the refusal is valid and
Applicable tthe patent's partcular circumstances.
Pad
5:08 pm @ 19%
‘samsonplab.co.uk
Confidentiality: disclosing information about serious communicable diseases
CConfidentiaity is cortal to the trist between doctors and patients Patients neat to believe that what they tell their
decors will be kept ih canhdence, otherwise they might be urwiling Co shaie inormation which Is impertant for thelr
Gector to know in order to be able to provide safe arc effective treatment and care. That's importart fr the individual
Ditient ang for socieiy: we all Beneht f people who might nave serous communicable diseases are encouraged to seek
Bevice, testing and treatment
However, the right & confidentiality is not absdute, and there are circumstances in which @ docter may decide that
isclosng confidential Information 1s justified in the publc irterest. Dr Peters’ case stuiy examines three cliferent
1. HIV patient
|Aoctar needs to bance his duty of confidentiality te his patient, with the patent rik to other of his auch ax
partner from net being tod about his gifriend’s HIV status.
GHC guidarce on confidentiality states that doctors may disclose infermation to a known sewual contact ofa patient with
2 sericus communicable dsease if they are at sk of Infection (For example if theyre having unprotected sex) and the
patient cant be persuaded to tell them. This guidance apples, even f the sexual contac i nota patient.
2. Refusal to share information
Dectorssheuld usually respect 9 competent adult's refusal to share information
Ina stenaro where 2 doctor receives information that a patient of his is at sk ef serous harm and considers whether
the doctor to cleclose this information. "
GMC guidarce on confidentiality states that doctors should usually respect a competent adult patents’ refusal to consent
toinformaton buing shared, even I that leaves them, but novody eke, risk of harm.
Relatives, carers and partners
Family members, panners, cerers and anyone else dose to an incapacitated patient will often have sirong opinions
‘about she treatment and core they want thar loved one te have, They may algo eten have infermaton about what the
patient wou nave wanted, if may coule sl speak for themselves.
Problans can arse i there are differences o opinion, about what the patients wishes would have been. While trying to
‘manage such situations, & is moorant to start by establishing whether anyane has legal autherity to rake treatment
Gecisions on betalf ofthe patient, F they lose the capacity to do so,
Were, as stl often the case, there is no legal proxy, doctors must explain what they are asking those close to the
‘Views and values which wil then inform the decision aout treatment
Such discussions wil never be easy, but clanty about the role of family members and others in the decision-making
process may aveid ar reseve disagreements that can add to cstrass at an already aut te.
Conscientious objections to stopping a life-protonging treatment
Same docters may (or rsiginus or personal reatons) disagree in grincipo with patiors! eqht to rots We-peolonging|
treatment Ike Cinically assisted nutrition and hyératien. Some doctors may hold the view, that food and flies are not
\iite GMC guidance does not requre decors to act agains: tne bells, does stress tat they must net abandon such
patients, nor alow their care to suffer. The care of patients must always come fist, and doctors may, rarely, be
Fequired to sot aside thetr personal viens, util anather doctor can be found to taka over thelr rae,
‘Taking prompt action if patients are not receiving basic ca
service to provide basic care to mest their needs. Ths hes incuded cases where patients nave not had enough ty eat
ard era,
‘The GHC quidarce in Gaed macical practice is cls doctors must take prompt action, even if tient their patient and
wat reeds doing isit part of a coctor's rele. If decors see that a patient or eatierts are not geting the basic care
they neeg, they must immediatly fell someane who isn & postion to act straight away.
Work effectively as part of a team
‘Yeu must support coleagues who have problems with their performance or health. But you must put patient safety ast
atall tmes
&
a
5:09 pm ® w%e>
‘samsonplab co.uk
Resource end date
what needs doing isi't part of a doctor's role. If dactors see that a patient or patients are not getting the basic care
‘hay need, they must immadiataly tall someone wha is ina postion to act straght away.
Work effectively as part of a team
You must supper coleagues who have prublems with ther performance er heath. But yeu must put patient safety Fst
at all times,
Most patient care is delivered by teams made up of colleagues from a range of disciplines. In this case, as well as the
docto's and nurses, physiotherapists, occupational therapists, speech and language professionals are litely tbe
Involved inthe care of patents on a Stroke Un
GMC quidance in Good madical pratice is clear that doctors must work colaboratively with all their colleagues, ané
respedt thelr skils and corénbutions.
When to contact an external regulator
(GMC guidance, Raisvg and acting on concerns abour patient safety, states tat wherever possible, a ductor shoul! frst
raise their concarn with thelr manager of the arganisation where they work. Many concerns can’ often be quickly ané
‘ftectvely dealt wth ata local evel
‘The GMC guidance sets out the circumstances where you might need 1o escalate @ cincem elther to someone more
enior in the organisation, such az te Madial Director or Chef Executive or to contact an external regulator of other
organisauen,
Nursing and Midwifery Cauncl (NNC) er the Care Quality Commission (CQC). In this case, it might have bear
appropriate to cantac the CQC I the doctors felt Uey could false the Issue with the hospital because they belever
that the management or board were part of the pratiem,
1, having raise their concerns lacaly, they are not satisfed with the response, or if there is an immediate serious risk
1e patients, ther the CQC has te responsbilty to act oF intervene,
2026-07-24 10:25,
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Competition Ratios 2017 ST3 PDFDocument8 pagesCompetition Ratios 2017 ST3 PDFAshish BamaniaNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Person Specification 2017: Entry CriteriaDocument5 pagesPerson Specification 2017: Entry CriteriaAshish BamaniaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elective Placements Application GuideDocument6 pagesElective Placements Application GuideAshish BamaniaNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
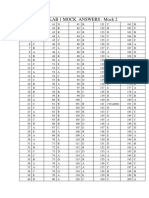
- Plab 1 Mock Answers: Mock 2: CyclizineDocument2 pagesPlab 1 Mock Answers: Mock 2: CyclizineAshish BamaniaNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Mock 4Document35 pagesMock 4Danish CsiNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)