Professional Documents
Culture Documents
Tribo EC Journal
Tribo EC Journal
Uploaded by
Erni RismiyantiCopyright:
Available Formats
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Medical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manual DownloadDocument7 pagesMedical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manual DownloadSteven Dubose100% (24)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Science 5 DLP 1 - Human Reproductive SystemDocument12 pagesScience 5 DLP 1 - Human Reproductive SystemMark Cua89% (35)
- Komi Classification of Bile Duct CystsDocument3 pagesKomi Classification of Bile Duct Cystsmero1983No ratings yet
- Cuneyt Alper MD, Charles Bluestone MD, Margaretha Casselbrant, Joseph Dohar MD, Ellen Mandel MD - Advanced Therapy of Otitis Media (2003, PMPH Usa)Document576 pagesCuneyt Alper MD, Charles Bluestone MD, Margaretha Casselbrant, Joseph Dohar MD, Ellen Mandel MD - Advanced Therapy of Otitis Media (2003, PMPH Usa)Carmen-BadeaNo ratings yet
- Common Problems: in Newborn InfantDocument94 pagesCommon Problems: in Newborn InfantAhmad JustNo ratings yet
- Is Smoking An Effective Way To Take KratomDocument3 pagesIs Smoking An Effective Way To Take KratomZackNo ratings yet
- Identification of Exudates in Inflammation PDFDocument5 pagesIdentification of Exudates in Inflammation PDFlourdes kusumadiNo ratings yet
- Medication Exercise Treatment Hygiene Outpatient DietDocument6 pagesMedication Exercise Treatment Hygiene Outpatient DietCarla Tongson MaravillaNo ratings yet
- (Anatomy) Chapter 12 - Lymphatic SystemDocument71 pages(Anatomy) Chapter 12 - Lymphatic SystemJezreel Mian A. LacsonNo ratings yet
- Protocol Update Dec 2019Document13 pagesProtocol Update Dec 2019Aarzu ChoudharyNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 42Document16 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 42sarasjunkNo ratings yet
- Cap 22Document47 pagesCap 22Andreea AronNo ratings yet
- MalnutritionDocument71 pagesMalnutritionnasibdin100% (2)
- Neurologic Reflexes Assessment in Magnesium Sulfate AdministrationDocument30 pagesNeurologic Reflexes Assessment in Magnesium Sulfate AdministrationMaria Pina Barbado PonceNo ratings yet
- Body System 2º EnriqueDocument9 pagesBody System 2º EnriqueRUIZ CANO EnriqueNo ratings yet
- Person Gordon'S Approach: Before Hospitalization During Hospitalization PsychologicalDocument2 pagesPerson Gordon'S Approach: Before Hospitalization During Hospitalization Psychologicalpearlannesanford1995No ratings yet
- Concept MapDocument4 pagesConcept MapDud AccNo ratings yet
- Wallgren 1948Document7 pagesWallgren 1948Dyah Farida InliNo ratings yet
- TMS Special Edition 17 0821webDocument52 pagesTMS Special Edition 17 0821webalinaNo ratings yet
- 1 s2.0 S1365182X2032236XDocument1 page1 s2.0 S1365182X2032236XHưng Nguyễn KiềuNo ratings yet
- Making Occlusion 2Document7 pagesMaking Occlusion 2Ali QawasNo ratings yet
- Competency Appraisal Midterm ExaminationsDocument9 pagesCompetency Appraisal Midterm ExaminationsRellie Castro100% (1)
- Chapter 26 Management of Patients With Dysrhythmias and Conduction ProblemsDocument22 pagesChapter 26 Management of Patients With Dysrhythmias and Conduction ProblemsAbel C. Idusma Jr.No ratings yet
- Urological Infections 2010.PDF EditDocument112 pagesUrological Infections 2010.PDF EditMuhammad Bilal Bin AmirNo ratings yet
- Hoeltke Chapter2 RevisedDocument44 pagesHoeltke Chapter2 RevisedKarby LeeNo ratings yet
- Prevention of Foot Ulcer 2020Document22 pagesPrevention of Foot Ulcer 2020Devi SiswaniNo ratings yet
- Bacillus Clausii Is A RodDocument9 pagesBacillus Clausii Is A RodGrax DeeNo ratings yet
- Good Will HuntingDocument4 pagesGood Will HuntingMary MoralesNo ratings yet
- Questions Bio PostDocument16 pagesQuestions Bio PostJanlie GautaneNo ratings yet
- Laboratorio Clinico Toledo: Patient Number Birthdate SexDocument1 pageLaboratorio Clinico Toledo: Patient Number Birthdate SexMirle BonetNo ratings yet
Tribo EC Journal
Tribo EC Journal
Uploaded by
Erni RismiyantiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tribo EC Journal
Tribo EC Journal
Uploaded by
Erni RismiyantiCopyright:
Available Formats
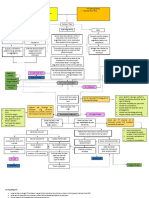
EXFOLIATIVE CHEILITIS: REPORT OF TWO CASES
PRESENTING A MARKED CLINICAL IMPROVEMENT
AFTER ORAL OLANZAPINE
Tribó MJ*, Martinez Escala ME*, Ros-Montalban S**, Ros-Cucurell E**, Pujol RM*, Bulbena A**
Departments of Dermatology and Pathology*. Department of Psychiatry**. Hospital del Mar. IMAS. Barcelona. SPAIN
Introduction
The concept of exfoliative cheilitis (EC) defines a heterogeneous spectrum of chronic inflammatory processes characterized by a persisting crusting and desquamation of the
lips. It is a disorder presenting a female predominance and often develops before the age of 30 years. The etiology of EC is unknown, but a possible factitious origin has been
postulated. In the dermatological French literature this condition has been described as "le tic des lèvres", in which recurrent manipulation of the lips may lead to inflammatory
changes or to exacerbate pre-existing lesions. Histopathological features are often non-specific (epithelial hyperplasia and a mild inflammatory infiltrate surface). EC should be
differentiated from other disorders causing persistent cheilitis such as Candidal lip infections, atopic cheilitis, actinic cheilitis, and glandular cheilitis. Historically, the use of
dopamine receptor antagonists, such as aloperidol and pimozide, had been useful in the treatment of tics. The apparition of atypical antipsychotics, for instance olanzapine and
risperidone, has permitted us optimized the risk and benefit balance. We report two additional cases of exfoliative cheilitis showing a marked improvement was noted after
treatment with oral olanzapine.
Clinical cases
A 61-year-old woman was referred to our Department for evaluation of referred for one A 18-year-old man presented a two month's history of persistent dryness and desquamation
year's history of angular cheilitis refractory to emollients and topical corticosteroids. Past of the lips. He has been treated with petroleum jelly and topical corticosteroids without
medical history disclosed an anxiety disorder causing motor automatisms treated with improvement. He dropped out school last year because of stress. The diagnosis of
antidepressant and anxiolytics. Physical examination revealed a thick yellowish brown anxiety disorder with obsessive traits and motor rituals was established. Physical
crusting on the lips extending to the vermillion border (Fig 1a, 1b). A complete haematological, examination revealed a yellow brown crusting of the lips with whitish patches on the
biochemical and immunological survey disclosed no abnormalities. Patch testing with the mucous side (Fig 4). A bacteriological culture from the crusts isolated Candida albicans
European standard series was also negative. A punch biopsy specimen from the lower and P. aeruginosa. Treatment with oral fluconazole and ciprofloxacin were prescribed
lip disclosed (Fig 2) an epithelial and glandular hyperplasia with a mild perivascular but no clinical improvement was noted. A completed haematological, biochemical and
inflammatory infiltrate in the upper submucosa. No epithelial dysplasia was present. The immunological survey disclosed no abnormalities. Patch test results were also negative.
diagnosis of EC was established and treatment with oral olanzapine (5mg/day), alprazolam The clinical diagnosis of EC was established. Oral olanzapine (2.5 mg/day) was prescribed.
(1mg/day) and lipoic acid (200 mg/day) were prescribed. A marked clinical improvement A marked and persistent clinical improvement of the lesions was observed after three
(80%) was noted after four months of treatment (Fig 3). months.
Fig 4. Physical examination
revealed a yellow brown
crusting of the lips with
Fig 1a and 1b. A thick yellowish brown crusting on the lips extending to the whitish patches on the
vermillion border. mucous side.
Fig 2. An
epithelial and
glandular
hyperplasia
with a mild
perivascular
inflammatory Fig 5. A marked clinical
infiltrate in improvement after three
the upper Fig 3. Patient one improvement after four months of oral olanzapine
submucosa. months of treatment with olanzapine. treatment.
Conclusions
• EC seems to include a heterogeneous group of disorders: factitious cheilitis, cheilitis secondary to an impulsivity disorder and probably several inflammatory disorders
causing persisting lip desquamation (irritative cheilitis, allergic contact cheilitis, infectious disorders, etc).
• In some cases of exfoliative cheilitis underlying psychiatric disturbances may be detected.
• We reported two cases of persistent EC refractory to topical treatments in two patients with an underlying psychiatric disorder who recognized a possible self-inflicted cause
for the lesions.
• In both patients a marked clinical improvement was noted after treatment with oral olanzapine. No significant side-effect was noted.
• Oral olanzapine, an effective drug usually prescribed for the obsessive-impulsive disorder, may be an additional useful therapeutic option for patients with exfoliative cheilitis.
References
1. Aydin E, Gokoglu O, Ozcurumez G, Aydin H. Factitious cheilitis: a case report. J Med Case Report 2008;2:29-32.
2. Daley TD, Gupta AK. Exfoliative cheilitis. J Oral Pathol Med 1995;24.117-9.
3. Reade PC, Sim R. Exfoliative cheilitis - a factitious disorder? Int J Oral Maxillofac Surg 1986;15:313-7.
4. Taniguchi S, Kono T. Exfoliative cheilitis: A Case Report and Review of the Literature. Dermatology 1998;196(2):253-5.
Institut Municipal
d’Assistència Sanitària
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5820)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1093)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (845)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Medical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manual DownloadDocument7 pagesMedical Nutrition Therapy A Case Study Approach 5th Edition Nelms Solutions Manual DownloadSteven Dubose100% (24)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Science 5 DLP 1 - Human Reproductive SystemDocument12 pagesScience 5 DLP 1 - Human Reproductive SystemMark Cua89% (35)
- Komi Classification of Bile Duct CystsDocument3 pagesKomi Classification of Bile Duct Cystsmero1983No ratings yet
- Cuneyt Alper MD, Charles Bluestone MD, Margaretha Casselbrant, Joseph Dohar MD, Ellen Mandel MD - Advanced Therapy of Otitis Media (2003, PMPH Usa)Document576 pagesCuneyt Alper MD, Charles Bluestone MD, Margaretha Casselbrant, Joseph Dohar MD, Ellen Mandel MD - Advanced Therapy of Otitis Media (2003, PMPH Usa)Carmen-BadeaNo ratings yet
- Common Problems: in Newborn InfantDocument94 pagesCommon Problems: in Newborn InfantAhmad JustNo ratings yet
- Is Smoking An Effective Way To Take KratomDocument3 pagesIs Smoking An Effective Way To Take KratomZackNo ratings yet
- Identification of Exudates in Inflammation PDFDocument5 pagesIdentification of Exudates in Inflammation PDFlourdes kusumadiNo ratings yet
- Medication Exercise Treatment Hygiene Outpatient DietDocument6 pagesMedication Exercise Treatment Hygiene Outpatient DietCarla Tongson MaravillaNo ratings yet
- (Anatomy) Chapter 12 - Lymphatic SystemDocument71 pages(Anatomy) Chapter 12 - Lymphatic SystemJezreel Mian A. LacsonNo ratings yet
- Protocol Update Dec 2019Document13 pagesProtocol Update Dec 2019Aarzu ChoudharyNo ratings yet
- Medical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 42Document16 pagesMedical-Surgical Nursing Assessment and Management of Clinical Problems 9e Chapter 42sarasjunkNo ratings yet
- Cap 22Document47 pagesCap 22Andreea AronNo ratings yet
- MalnutritionDocument71 pagesMalnutritionnasibdin100% (2)
- Neurologic Reflexes Assessment in Magnesium Sulfate AdministrationDocument30 pagesNeurologic Reflexes Assessment in Magnesium Sulfate AdministrationMaria Pina Barbado PonceNo ratings yet
- Body System 2º EnriqueDocument9 pagesBody System 2º EnriqueRUIZ CANO EnriqueNo ratings yet
- Person Gordon'S Approach: Before Hospitalization During Hospitalization PsychologicalDocument2 pagesPerson Gordon'S Approach: Before Hospitalization During Hospitalization Psychologicalpearlannesanford1995No ratings yet
- Concept MapDocument4 pagesConcept MapDud AccNo ratings yet
- Wallgren 1948Document7 pagesWallgren 1948Dyah Farida InliNo ratings yet
- TMS Special Edition 17 0821webDocument52 pagesTMS Special Edition 17 0821webalinaNo ratings yet
- 1 s2.0 S1365182X2032236XDocument1 page1 s2.0 S1365182X2032236XHưng Nguyễn KiềuNo ratings yet
- Making Occlusion 2Document7 pagesMaking Occlusion 2Ali QawasNo ratings yet
- Competency Appraisal Midterm ExaminationsDocument9 pagesCompetency Appraisal Midterm ExaminationsRellie Castro100% (1)
- Chapter 26 Management of Patients With Dysrhythmias and Conduction ProblemsDocument22 pagesChapter 26 Management of Patients With Dysrhythmias and Conduction ProblemsAbel C. Idusma Jr.No ratings yet
- Urological Infections 2010.PDF EditDocument112 pagesUrological Infections 2010.PDF EditMuhammad Bilal Bin AmirNo ratings yet
- Hoeltke Chapter2 RevisedDocument44 pagesHoeltke Chapter2 RevisedKarby LeeNo ratings yet
- Prevention of Foot Ulcer 2020Document22 pagesPrevention of Foot Ulcer 2020Devi SiswaniNo ratings yet
- Bacillus Clausii Is A RodDocument9 pagesBacillus Clausii Is A RodGrax DeeNo ratings yet
- Good Will HuntingDocument4 pagesGood Will HuntingMary MoralesNo ratings yet
- Questions Bio PostDocument16 pagesQuestions Bio PostJanlie GautaneNo ratings yet
- Laboratorio Clinico Toledo: Patient Number Birthdate SexDocument1 pageLaboratorio Clinico Toledo: Patient Number Birthdate SexMirle BonetNo ratings yet