Professional Documents
Culture Documents
Hemodynamic Support Table PDF
Hemodynamic Support Table PDF
Uploaded by
abdulOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hemodynamic Support Table PDF
Hemodynamic Support Table PDF
Uploaded by
abdulCopyright:
Available Formats
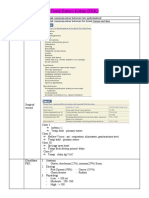
Recommendations: Hemodynamic Support and Adjunctive Therapy*
G. Fluid Therapy of Severe Sepsis
1. Crystalloids as the initial fluid of choice in the resuscitation of severe sepsis and septic shock
(grade 1B).
2. Against the use of hydroxyethyl starches for fluid resuscitation of severe sepsis and septic
shock (grade 1B).
3. Albumin in the fluid resuscitation of severe sepsis and septic shock when patients require
substantial amounts of crystalloids (grade 2C).
4. Initial fluid challenge in patients with sepsis-induced tissue hypoperfusion with suspicion of
hypovolemia to achieve a minimum of 30 mL/kg of crystalloids (a portion of this may be albumin
equivalent). More rapid administration and greater amounts of fluid
may be needed in some patients (grade 1C).
5. Fluid challenge technique be applied wherein fluid administration is continued as long as there
is hemodynamic improvement either based on dynamic (eg, change in pulse pressure, stroke
volume variation) or static (eg, arterial pressure, heart rate) variables (UG).
H. Vasopressors
1. Vasopressor therapy initially to target a mean arterial pressure (MAP) of 65 mm Hg (grade
1C).
2. Norepinephrine as the first choice vasopressor (grade 1B).
3. Epinephrine (added to and potentially substituted for norepinephrine) when an additional agent
is needed to maintain adequate blood pressure (grade 2B).
4. Vasopressin 0.03 units/minute can be added to norepinephrine (NE) with intent of either
raising MAP or decreasing NE dosage (UG).
5. Low dose vasopressin is not recommended as the single initial vasopressor for treatment of
sepsis-induced hypotension and vasopressin doses higher than 0.03-0.04 units/minute should be
reserved for salvage therapy (failure to achieve adequate MAP with other vasopressor agents)
(UG).
6. Dopamine as an alternative vasopressor agent to norepinephrine only in highly selected
patients (eg, patients with low risk of tachyarrhythmias and absolute or relative bradycardia)
(grade 2C).
7. Phenylephrine is not recommended in the treatment of septic shock except in circumstances
where (a) norepinephrine is associated with serious arrhythmias,
(b) cardiac output is known to be high and blood pressure persistently low or (c) as salvage
therapy when combined inotrope/vasopressor drugs and low dose vasopressin have failed to
achieve MAP target (grade 1C).
8. Low-dose dopamine should not be used for renal protection (grade 1A).
9. All patients requiring vasopressors have an arterial catheter placed as soon as practical if
resources are available (UG).
I. Inotropic Therapy
1. A trial of dobutamine infusion up to 20 micrograms/kg/min be administered or added to
vasopressor (if in use) in the presence of (a) myocardial dysfunction as suggested by elevated
cardiac filling pressures and low cardiac output, or (b) ongoing signs of
hypoperfusion, despite achieving adequate intravascular volume and adequate MAP (grade 1C).
2. Not using a strategy to increase cardiac index to predetermined supranormal levels (grade 1B).
J. Corticosteroids
1. Not using intravenous hydrocortisone to treat adult septic shock patients if adequate fluid
resuscitation and vasopressor therapy are able to restore hemodynamic stability (see goals for
Initial Resuscitation). In case this is not achievable, we suggest intravenous hydrocortisone alone
at a dose of 200 mg per day (grade 2C).
2. Not using the ACTH stimulation test to identify adults with septic shock who should receive
hydrocortisone (grade 2B).
3. In treated patients hydrocortisone tapered when vasopressors are no longer required (grade
2D).
4. Corticosteroids not be administered for the treatment of sepsis in the absence of shock (grade
1D).
5. When hydrocortisone is given, use continuous flow (grade 2D).
______
*Reprinted from Dellinger RP, Levy MM, Rhodes A, et al: Surviving Sepsis Campaign:
International guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med.
2013; 41:580-637
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pathology MCQDocument42 pagesPathology MCQJim Jose Antony100% (17)
- Outbreak Undead How To PlayDocument28 pagesOutbreak Undead How To PlayArdale PalilloNo ratings yet
- Fistul Entero Kutan (FEK)Document4 pagesFistul Entero Kutan (FEK)dewiswahyuNo ratings yet
- Neonate With AcrocyanosisDocument4 pagesNeonate With Acrocyanosisnurul noviarisaNo ratings yet
- Golden Hour CCM Arthur Van Zanten IC1Document3 pagesGolden Hour CCM Arthur Van Zanten IC1Sara NicholsNo ratings yet
- Multi Organ Dysfunction SyndromeDocument40 pagesMulti Organ Dysfunction SyndromeDr. Jayesh PatidarNo ratings yet
- Yusnimar, Penkes Ec SAE, Duty HannaDocument18 pagesYusnimar, Penkes Ec SAE, Duty HannaHanna GustinNo ratings yet
- Viarasilpa Et Al 2019 Venous Thromboembolism in Neurocritical Care PatientsDocument9 pagesViarasilpa Et Al 2019 Venous Thromboembolism in Neurocritical Care Patientsateia83No ratings yet
- UrosepsisDocument22 pagesUrosepsisWita Ferani KartikaNo ratings yet
- Anemia and Critical CareDocument77 pagesAnemia and Critical Carehunter_axl010% (1)
- DIPROSPAN Sterile Aqueous Suspension: DescriptionDocument6 pagesDIPROSPAN Sterile Aqueous Suspension: DescriptionAbet AtienzaNo ratings yet
- Anusuchi 9 (Payment Mechanism and Rates) UploadDocument61 pagesAnusuchi 9 (Payment Mechanism and Rates) UploadAmit OjhaNo ratings yet
- 11 - Management Post Operative Low Cardiac Output SyndromeDocument46 pages11 - Management Post Operative Low Cardiac Output SyndromeNat SNo ratings yet
- Peritonitis Update On Pathophysiology, Clinical Manifestations, and PDFDocument11 pagesPeritonitis Update On Pathophysiology, Clinical Manifestations, and PDFAnonymous InJS6aYZ100% (1)
- Hematologic Changes in SepsisDocument16 pagesHematologic Changes in SepsisnisaNo ratings yet
- Neonatal Sepsis: A Study of The Risk FactorsDocument42 pagesNeonatal Sepsis: A Study of The Risk FactorsNithin100% (3)
- Abbreviated PI ABBOTIC DraftDocument2 pagesAbbreviated PI ABBOTIC Draftadani 2372No ratings yet
- 10 Problem StatementDocument6 pages10 Problem StatementRicha Sharma100% (1)
- Critical Care PowerpointDocument63 pagesCritical Care PowerpointtikoNo ratings yet
- Guidelines For The Use of Blood Warming Devices AABBDocument42 pagesGuidelines For The Use of Blood Warming Devices AABBBrandonHuangNo ratings yet
- Shock AmbossDocument40 pagesShock AmbossAshraf AlbhlaNo ratings yet
- CH 14 Test BankDocument21 pagesCH 14 Test BankKrestine Molle100% (1)
- 1 s2.0 S2589555921000793 MainDocument10 pages1 s2.0 S2589555921000793 Mainelektifppra2022No ratings yet
- Sefril: (Cefradine)Document1 pageSefril: (Cefradine)Air Ticket & Visa SolutionNo ratings yet
- ScvO2 Pocket Card - 2017 PDFDocument3 pagesScvO2 Pocket Card - 2017 PDFghg sddNo ratings yet
- Hubungan Antara NLR Dan Aki Pada Pasien SepsisDocument4 pagesHubungan Antara NLR Dan Aki Pada Pasien Sepsisdwi widyaNo ratings yet
- Surfactant NeonatologyDocument19 pagesSurfactant NeonatologyMbabazi Theos100% (1)
- Use of Vasopressors and Inotropes - UpToDateDocument18 pagesUse of Vasopressors and Inotropes - UpToDateAlbertoMarteNo ratings yet
- JAUNDICE Internal Medicine PresentationDocument34 pagesJAUNDICE Internal Medicine PresentationNano BaddourNo ratings yet
- The Role of The Gut Microbiota in SepsisDocument9 pagesThe Role of The Gut Microbiota in SepsisSyahrul HamidNo ratings yet