Professional Documents
Culture Documents
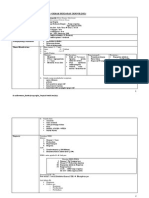
1 - Orthopaedic Diagnosis PDF
Uploaded by
arifamri920 ratings0% found this document useful (0 votes)
63 views25 pagesOriginal Title
1_Orthopaedic diagnosis.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
63 views25 pages1 - Orthopaedic Diagnosis PDF
Uploaded by
arifamri92Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 25
Section 1
General Orthopaedics
© ONAHAHNHH
ea
Nis
Orthopaedic diagnosis
Infection
Rheumatic disorders
Crystal deposition disorders
Osteoarthritis
Osteonecrosis and related disorders
Metabolic and endocrine disorders
Genetic disorders, skeletal dysplasias and malformations
Tumours
Neuromuscular disorders
Peripheral nerve injuries
Orthopaedic operations
133
167
201
229
255
1
Information consists of differences that make a difference.
Gregory Bateson
Orthopaedics is concerned with bones, joints, muscles,
tendons and nerves ~ the skeletal system and all that
makes it move. Conditions that affect these structures
fall into seven easily remembered pairs:
|. Congenital and developmental abnormalities
Infection and inflammation
Arthritis and rheumatic disorders
Metabolic and endocrine disorders
‘Tumours and lesions that mimic them
. Sensory disturbance and muscle weakness
Injury and mechanical derangement
Diagnosis in orthopaedics, as in all of medicine, is the
identification of disease. It begins from the very first
‘encounter with the patient and is gradually modified and
fine-tuned until we have a picture, not only of a patho-
logical process but also of the functional loss and the
disability that goes with it. Understanding evolves from
the systematic gathering of information from the history,
the physical examination, tissue and organ imaging and
special investigations. Systematic, but never mechani-
cal; behind the enquiring head there should also be what
D. H, Lawrence has called the intelligent heart, It must
never be forgotten that the patient is also a person, with
a mind and a personality, a job and hobbies, a family
and a home; all have a bearing upon ~ and are in turn
affected by ~ the disorder and its treatment.
HISTORY
Taking a history’ is a misnomer. The patient tells a
story; it is we the listeners who construct a history. The
story may be maddeningly disorganized; the history
has to be systematic. Carefully and patiently compiled,
it can be every bit as informative as examination or
laboratory tesis.
‘As we record it, certain key words will inevitably stand
out: injury, pain, stiffness, swelling, deformity, instabil-
ity, weakness, altered sensibility and loss of finetion. Each
symptom is pursued for more detail: we need to know
when it began, whether suddenly or gradually, sponta-
neously or after some specific event; how it has changed
or progressed; what makes i worse; what makes it better.
Orthopaedic diagnosi
While listening, we consider if the story fits some
pattern that we recognize ~ for we are already think-
ing of a diagnosis. Every piece of information should
be thought of as part of a larger picture which gradu-
ally unfolds in our understanding, ‘Disease reveals itself
in casual parentheses’, is the way Trotter described it.
‘SymProMs.
Pain
Pain is the most common symptom in orthopaedics. Itis
described in terms that range from the most boring and
bland to the impossibly dramatic and bizarre. The
metaphors used tell us more about the patient's psyche
than about the pathology; yet there are clearly differences,
between the throbbing pain of an abscess and the aching,
pain of chronic arthritis, between the ‘buming pain’ of
neuralgia and the ‘stabbing pain’ of a ruptured tendon.
Severity is even more subjective. High and low thresh-
olds undoubtedly exist, but to the patient pain is as bad
as it feels, and any system of pain grading’ must take
this into account. The main value of estimating severity
is in assessing the progress of the disorder or the response
to treatment. The following is a simple and useful system:
* Grade I (mild) Pain that can easily be ignored
* Grade I (moderate) Pain that cannot be ignored,
interferes with function and needs treatment from
time to time.
© Grade IM (severe) Pain that is present most of the
time, demanding constant attention.
* Grade IV (excruciating) Totally incapacitating pain.
Patients are often vague about the site of pain. Yet
its precise location is important, and in orthopaedics it
is particularly useful to ask the patient to point to
where it hurts; not merely to tell us, but actually to
point. But don't assume that the site of pain is always
the site of pathology; ‘referred’ pain and ‘autonomic’
pain can be very deceptive.
Referred pon Pain arising in or near the skin is usually
localized accurately. Pain arising in deep structures is
‘more diffuse and is sometimes of unexpected distribu-
tion; thus, hip disease may manifest with pain in the
‘knee (50 might an obturator hernia). This is not because
sensory nerves connect the two sites; it is due to inabil-
ity ofthe cerebral cortex to distinguish between sensory
You might also like
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- Status Kedokteran Keluarga DiareDocument18 pagesStatus Kedokteran Keluarga Diarearifamri92No ratings yet
- Refarat Gangguan Cemas MenyeluruhDocument27 pagesRefarat Gangguan Cemas Menyeluruharifamri92No ratings yet
- EKTIMADocument12 pagesEKTIMAarifamri92No ratings yet
- SPM GiziDocument2 pagesSPM Giziarifamri92No ratings yet
- PBL Module 2Document63 pagesPBL Module 2arifamri92No ratings yet
- Lapsus Kaki DiabetikDocument40 pagesLapsus Kaki Diabetikarifamri92No ratings yet
- Case 3:myopiaDocument24 pagesCase 3:myopiaarifamri92No ratings yet
- Lapsus Jiwa Non Psikotik Gang Anxietas DepresiDocument9 pagesLapsus Jiwa Non Psikotik Gang Anxietas Depresiarifamri92No ratings yet
- Module Opthalmology Corneal Ulcer: Group 7 Wulan-Fadzely-Arif Amri-Safuan Arif-Nadiah-Insyira-Fatimah-Andi AbsharinaDocument19 pagesModule Opthalmology Corneal Ulcer: Group 7 Wulan-Fadzely-Arif Amri-Safuan Arif-Nadiah-Insyira-Fatimah-Andi Absharinaarifamri92No ratings yet
- Modul 2: Dermatovenerology Case 3:vitiligoDocument15 pagesModul 2: Dermatovenerology Case 3:vitiligoarifamri92No ratings yet
- DBD AnakDocument3 pagesDBD Anakarifamri92No ratings yet