Professional Documents
Culture Documents
Antibiotics 170308134011 PDF
Uploaded by
SeptaPratamaApt0 ratings0% found this document useful (0 votes)
15 views81 pagesOriginal Title
antibiotics-170308134011.pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
15 views81 pagesAntibiotics 170308134011 PDF
Uploaded by
SeptaPratamaAptCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 81
That is capable of destroying or weakening certain
microorganisms, especially bacteria or fungi, that cause
infections or infectious diseases.
Antibiotics are usually produced by or synthesized from other
microorganisms, such as molds.
These are used to treat infections caused by bacteria.
Antibacterial agents or antibiotics fall into several major
categories.
Aminoglycosides
Carbapenes
Cephalosporin's
Erythromycins
Penicillin's (including various sub groups)
Sulfonamides
Tetracycline's
Fluoroquinolones
Metranidazole
Miscellaneous agents
These drugs containing amino sugars, are used primarily in
infections caused by gram negative enterobacteria and
suspected sepsis.
The toxic potential of these drugs limit their use.
MOA: These are bactericidal, they inhibit the bacterial
protein synthesis by binding the function of 30 S ribosomal
sub unit.
Their MOA is not fully known.
Major amino glycosides include:
AGENT HALF ADMINISTRATION COMMON DOSAGE
LIFE RANGE(A)
15MG/KG/DAY(once daily
Amikacin 2-3 hrs IV, IM dose)
3mg/ kg/day(standard)
Gentamycin 2 hrs IV, IM 6-7mg/kg/day(once daily)
Kanomycin 2-4 hrs Oral, IV 15mg/kg every 8-12hrs
50-100mg/kg/day(oral)
Neomycin 2-3hrs Oral, Topical 10-15mg/day (topical)
Netilmicin 2-7 hrs IV, IM 3-6mg/kg/day
Streptomycin 2-3 hrs IM 15mg/kg/day
3mg/ kg/day(standard)
Tobramycin 2-5 hrs IV, IM 6-7mg/kg/day(once daily)
Streptomycin :
It is active against both gram positive and gram negative
bacteria.
This drug has restricted its use to organisms that cause plague,
tularemia, gram positive streptococci and mycobacterium
tuberculosis.
Amikacin, kanomycin, gentamycin, tobramycin, neomycin
netilmicin are active against many gram negitive bacteria.
Gentamycin active against some staphylococcus strains. it is
more active than Tobramycin against Serratia organisims
Amikacin is broadest spectrum aminoglycoside with activity
against most aerobic gram negative bacilli as well as many
anaerobic gram negative strains that resist gentamycin and
tobramycin.
It is also active against M. tuberculosis and M. avium-
intracellulare.
Tobramycin may be more active against pseudomonas
aeruginosa than gentamycin.
Netilmicin may be active against gentamycin- resistant
organisms it appears to be less ototoxic than other
aminoglycosides.
Neomycin in addition to its activity against such gram negative
organisms as Escherichia coli and klebsiella pneumoniae, is
active against several gram positive organisms.
Therapeutic uses:
Streptomycin is used to treat plague, tularemia, acute
brucellosis(given in combination with tetracycline) and
tuberculosis( given in combination with other anti tubercular
agents).
Gentamycin, tobramycin, amikacin and netilmicin are used for
gram negitive bacillary infections( those caused by
enterobacter, serratia, klebsiella and p. aeruginosa),
Bacterial endocarditis caused by streptococcus viridians (given in
combination with pencillin), pneumonia (given in combination with
cephalosporin's or penicillin), meningitis, complicated uti,
osteomylelitis and peritonitis.
Neomycin is used for preoperative bowel sterilization; hepatic coma
and in topical form for skin and mucous membrane
infections(burns).
PRECAUTIONS & MONITERING EFFECTS:
Amino glycosides cause serious adverse effects to prevent or
minimize such problems blood drug concentrations, BUN and serum
creatinine levels should be monitored during the therapy.
A) OTOTOXICITY:
Amino glycosides causes vestibular or auditory damage.
Gentamycin and streptomycin can cause primarily vestibular
damage. (tinnitus, vertigo and ataxia)
Amikacin, kannamycin, and neomycin cause mainly auditory
damage. (hearing loss).
Tobramycin can result in both vestibular and auditory damage.
B) NEPHROTOXICITY:
Because amino glycosides accumulate in the proximal
convoluted tubule, mild renal dysfunction develops in up to
25% of patients receiving these drugs for several days.
Neomycin is the most nephrotoxic amino glycoside,
streptomycin is the least nephrotoxic.
Gentamycin and tobramycin are nephrotoxic to approximately
same degree.
Risk factors for increased nephrotoxic effects include:
Preexisting renal disease
Previous or prolonged amino glycoside therapy
Concurrent administration of another nephrotoxic drug.
NEUROMUSCULAR BLOCKADE:
This problem may arise in patients receiving high dose amino
glycoside therapy:
Risk factors for neuromuscular blockade include :
Concurrent administration of neuromuscular agents or an
anesthetic
Preexisting hypocalcaemia or myasthenia gravis.
Intraperitonial or rapid IV administration.
Hypersensitivity and local reactions are rare adverse effects of
amino glycosides.
These agents are ß Lactams that contain a fused ß lactam ring and a five
membered ring system that differs from penicillin's in being unsaturated and
containing a carbon atom instead of sulfur atom.
The class has a broader spectrum of activity than do most ß lactam .
Imipenem was first carbapenam compound introduced in United states
followed by Meropenam and most recently Ertapenam and Doripenam
came into existence.
Imipenam is combined by Cilastanin sodium as it is inhibited by the renal
dipeptidases.
Major carbapenems include:
Agent Elimination Half life ROA Dosage
route
Doripenam Renal 1 hr IV 500mg every 8 hrs
Imipenam Renal 1 hr IV 250 mg every 6 hrs
Ertapenam Renal 4 hrs IV, IM 1g/day
Meropenam Renal 1.5 hrs IV, IM 0.5-2g every 8 hrs
Mechanism of Action:
Carbapenems are bactericidal, inhibiting bacterial cell wall
synthesis.
Spectrum of activity:
These drugs have the broadest spectrum of all ß lactam
antibiotics.
The group is active against most gram positive cocci, gram
negative rods and anaerobes.
This class has good activity against many bacterial strains
that resist other antibiotics.
Ertapenam has narrower spectrum of activity than other
carbapenams.
It has little or no activity against P. aeruginosa and
Acinetobacter.
Therapeutic uses:
These are effective against urinary tract and lower respiratory
infections, intra abdominal and gynecological infections and
skin, soft tissue and joint infections.
Precautions and monitoring effects:
Carbapenems may cause nausea, vomiting, diarrhea and
pseudomembraneous colitis.
Seizures, dizziness and hypotension may develop; seizures
appear less frequently with meropenam or ertapenem.
Patients who are allergic to penicillin or cephalosporin's may
suffer cross- sensitivity reactions during carbapenams therapy.
These agents are known as ß lactam antibiotics because
their chemical structure consists of ß lactam ring adjoined
to a thiazolidine ring.
Cephalosporin's generally are classified in major groups
based on mainly on their spectrum activity.
Mechanism of action:
These are bactericidal they inhibit bacterial cell wall
synthesis, reducing cell wall stability and thus causing
membrane lysis.
Spectrum of activity:
First generation: These cephalosporin's are active against most
gram positive cocci (except enterococci) as well as enteric aerobic
gram negative bacilli.
Second generation: Cephalosporin's are active against the
organisms covered by first generation cephalosporin's and have
extended gram negative coverage, including ß lactamse producing
strains of Haemophilus influenzae.
Third generation: Cephalosporin's have wider activity against
more gram negative bacteria, for example Enterobacter, citrobacter,
serratia, providencia, neisseria and haemophilus
Fourth generation cephalosporin's include cefepime and
ceftaroline.
These shows evidence of greater activity versus gram positive
cocci, enterobacteriaceae and pseudomonas than third
generation.
It has poor activity against anaerobes, stenonotrophonomas and
pseudomonas species.
First generation cephalosporin's:
Agent Elimination Half life ROA Dosage
route
Cefadroxil Renal 1-5 hrs Oral 1-2G/DAY
Cefazolin Renal 1.4-2.2 hrs IV 250mg-1g/day
Cefalexin Renal 0.9-1.3 hrs Oral 250-500mg every
6hrs
Cephapirin Renal 0.6-0.8 hrs IV, IM 500mg-2gm every
4-6 hrs
cephradine Renal 1.3 hrs Oral , IV 250-500mg every
6hrs
Second generation Cephalosporins:
Agent Elimination Half life ROA Dosage
route
Cefaclor Renal 0.8 hr Oral 250-500MG
Cefmetazol Renal 72 mins IV 2g every 6- 12 hrs
e
Cefotetan Renal 2.8-4.6hrs IV, IM 1-2g every 12 hrs
Cefoxitin Renal 0.8 hrs IV 1-2g every 6-8 hrs
Cefprozil Renal 78 mins Oral 250-500 mg every
12-24 hrs
Cefuroxime Renal 1.5-2.2 hrs IV, IM 750mg-1.5g every
8hrs
Third generation:
Agent Elimination Half life ROA Dosage
route
Cefixime Renal 3-4 hrs Oral 400mg/day
Cefdinir Renal 1.7-1.8hrs Oral 300mg every 12
hrs
Cefditoren Renal 1.6hrs Oral 400mg every 12
hrs
Cefoperazo Renal 1.6-2.4hrs IV 2-4g every 12 hrs
ne
Cefotaxime Renal 1.5hrs IV 1-2g every 6-8 hrs
Cefpodoxim Renal 2.5hrs Oral 100-400mg every
e 12 hrs
Ceftazidime Renal 1.8hrs IV,IM 1-2g every 8-12
hrs
Ceftibuten Renal 2.5hrs Oral 400mg/day
Ceftizoxime Renal 1.7hrs IV 1-2g every 8-12
hrs
Fourth generation:
Agent Elimination Half life ROA Dosage
route
Cefepime Renal 2-2.3hrs IV,IM 1-2g every
8-12hrs
Ceftaroline Renal 2.6hrs IV 600mg every
12hrs
First Generation: these are commonly administered to
treat serious Klebsiella infections and gram positive
and some gram negative infections in patients with
mild penicillin allergy.ono
Second generation: these are valuable in treatment of
UTI resulting from E.coli organisms acute otitis media,
sinusitis and gonococcus diseases.
Cefaclor (ceclor): it is useful in otitis media and
sinusitis in the patients who are allergic to ampicillin
and amoxicillin.
Cefuroxime(Zinacef): it is commonly administered for
outpatient community acquired pneumonia.
Third generation : these can penetrate into cerebrospinal
fluid and thus are valuable in treatment of meningitis caused
by meningococci, pneumococci, H. influenza etc.,
These are also used to treat sepsis and fever.
Fourth generation agent cefepime is approved for treatment
of UTI’s, skin infections, pneumonia.
Precautions and monitoring
Because all cephalosporin's are eliminated renally doses must
be adjusted for patients with renal impairment.
Other adverse effects include nausea, vomiting, diarrhea,
nephrotoxicity.
Cephalosporin's may cause false positive glycosuria results on
test using the copper reduction method's
Ceftriaxome is now contraindicated in new borns in
concomitant with calcium containing solutions due to the risk
of precipitation in lungs and kidneys.
MOA: these may be bactericidal or bacteriostatic they bind
to the 50S ribosomal subunit , inhibiting bacterial protein
synthesis.
Spectrum Of Activity: these are active against many gram
positive organisms including streptococci ,
corynaebacterium, neisseria species as well as some strains
of mycoplasma, legionella and treponema.
Therapeutic uses:
These are drugs used for treatment of mycoplasma
pneumoniae, campylobacter infections, legionnaries
disease, chlamidial infections and diphtheria.
In patients with penicillin allergies erythromycins are most
commonly used especially in treatment of pneumococcal
pneumonia, s.aureus infections, syphilis and gonorrhea.
These may be given prophylactic ally before dental procedures
to prevent bacterial endocarditis.
Precautions & monitoring parameters:
Gastrointestinal distress(GI) (nausea, vomiting, diarrhea,
epigastric discomfort) may occur with all erythromycin forms
and are most common adverse effect.
Allergic reactions may present as skin eruptions, fever and
eosinophilia.
Cholestatic hepatitis may arise in patients treated for 1 week or
longer with erythromycin estolate , symptoms usually disappear
within few days as drug therapy ends.
IM injections for more than 100mg produce severe pain
persisting for hours.
Transient hearing impairment may develop with high dose
erythromycin therapy.
Agent Elimination route Half life ROA DOSAGE
AZITHROMYCIN HEPATIC 68HRS ORAL 250mg/day
Clarithromycin Renal 3-7 hrs Oral 250-500mg every
12 hrs
Erythromycin Heaptic 1.2-3.6hrs Oral 250-500mg every 6
based estolate, hrs
ethyl succinate
and stereate
Erythromycin IV 0.5-2.0g every 6
gluceptate and hrs
lactobionate
I. Natural penicillin's:
Among most important antibiotics natural penicillin's are
preferred drugs in treatment of many infectious diseases.
Available agents:
Penicillin G: sodium and potassium salts are administered
orally, intravenously and intramuscularly,
Penicillin V: it is a soluble drug form administered orally.
Penicillin G procaine and Penicillin G benzthine are
repository drug forms and administered IM.
MOA:
Penicillin's are bactericidal, they inhibit bacterial cell wall
synthesis in a manner similar to cephalosporin's.
Spectrum of activity:
Natural penicillin's are highly active against gram positive
cocci and some gram negative cocci.
Penicillin G is 5 to 10 times more active than penicillin V
against gram negative organisms and some aerobic organisms.
As natural penicillin are already hydrolyzed by penicillinases
they ineffective against S. aureus and other organisms that
resist penicillin
Therapeutic uses:
Penicillin G is preferred agent for all the infections
caused by penicillin susceptible s. pneumoniae organisms
including:
Pneumonia
Arthritis
Meningitis
Peritonitis
Pericarditis
Osteomyelitis
Mastoiditis
Penicillin's G and V are highly effective against other
streptococcal infections such as pharyngitis, otitis media
Sinusitis and bacteremia.
Penicillin G preferred agent in gonococcal infections, syphilis,
anthrax, actinomycosis, gas gangrene and listeria infections.
Penicillin V is most useful in skin, soft tissue and mild
respiratory infections.
Penicillin G procaine is effective against syphilis and
uncomplicated gonorrhea.
Penicillin G and V are used prophylactic ally to prevent
streptococcal infections, rheumatic fever and neonatal
opthalmia.
Precautions and monitoring:
Hypersensitivity reactions:
The rash may be urticarial, vesicular, bullous, scarlantiform or
maculopapular.
Anaphylaxis is a life-threatening reaction that most commonly
occurs with parenteral administration. Signs and symptoms
include severe hypotension, bronchoconstriction, nausea,
vomiting, abdominal pain and extreme weakness.
Other manifestations of hypersensitivity reactions include
fever, eosinophilia, angioedema and serum sickness.
Other adverse effects of natural penicillin's include GI distress,
bone marrow suppression (impaired platelet aggregation,
agranulocytosis).
With high dose therapy seizures may occur particularly in
patients with renal impairment.
Agent Elimination Half-life ROA Dosage
route
Penicillin G Renal 0.5hrs Oral, IV, IM 200,000-
500,000U
every 6-8 hrs
Penicillin V Renal 1 hr Oral 500mg-2g per
day
Penicillin G Renal 24-60hrs IM 300,000-
Procaine 600,000u/day
Penicillin G Renal 24-60hrs IM 300,000-
benzathine 600,000u/day
Penicillinase resistant penicillin's:
These penicillin's are not hydrolyzed and the agents include
methicillin, nafcillin and isoxazolyl penicillin's- dicloxacillin and
oxacillin.
MOA: same as natural penicillin's.
Spectrum of activity:
Because these penicillin's resist pencillinases these are active against
staphylococci.
Therapeutic uses:
These are used in staphylococcal infections resulting from organisms
that resist natural penicillins.
These agents are less potent than natural penicillin's .
Nafcillin is excreted through liver and thus may be useful in
treating staphylococcal infections in patients with renal
impairment.
Oxacillin and dicloxacillin are most valuable in long term
therapy of serious staphylococcal infections (endocarditis,
osteomyelitis) and in treatment of staphylococcal infections of
skin and soft tissues.
Precautions and monitoring effects:
Like natural penicillins hypersenitivity reactions including
Methicillin may cause nephrotoxicity and interstitial nephritis.
Oxacillin may be hepatotoxic.
Agent Elimination Half- ROA Dosage
route life
Dicloxacillin Renal 0.5- Oral 500mg-1g/day
9.5hr
Methicillin Renal 0.5-1hr IV,IM 1-2g every 4-
6hrs
Nafcillin Hepatic 0.5hrs Oral, 0.25-2g every
IV,IM 4-6hrs
Oxacillin Renal 0.5hrs Oral, 500mg-2g
IV,IM every 4-6hrs
Aminopenicillins :this group includes the semi synthetic
agents ampicillin and amoxicillin. Because of their wider
antibacterial spectrum these drugs are also known as broad
spectrum penicillin's.
MOA: same as natural penicillin's
Spectrum of activity:
These has a spectrum that is similar to but broader than that
of natural and penicillinase resistant penicillins.
Aminopenicliins are ineffective against most staphylococcal
organisms.
Therapeutic uses:
These are used to treat gonococcal infections, upper respiratory
infections, uncomplicated urinary tract infections and otitis
media.
For the infections resulting from penicillin resistant organisms
ampicillin may be given in combination with salbactum.
Amoxicillin is less effective than ampicillin in shigellosis
Amoxicillin is more effective against S.aureus and klebsiella
infections when administered in combination with clavulanic
acid.
Precautions and monitoring:
Hypersensitivity reactions may occur.
Diarrhea is most common with ampicillin.
Ampicillin and amoxicillin cause generalized erythomatous,
maculopapular rash.
Agent Elimination Half-life ROA Dosage
route
Amoxicillin Renal 0.8-1.4hr Oral 250-500mg
every 8 hrs
Amoxicillin/ Renal 1hr Oral 250-500mg
clavulanic acid every 8 hrs
Ampicillin Renal 0.8-1.5hrs Oral, 250-2g every
IV,IM 4-6hrs
Ampicillin / Renal 1-1.8hrs IV,IM 1.5-3g every 6
salbactum hrs
Extended spectrum penicillin:
These agents have widest antibacterial spectrum similar to that of
aminopenicillins but also are effective against klebsiella and
enterobacter species.
These are called as antipseudomonal penicillin's this group
includes the carboxypenicillins(tircacillin) and ureidopencillins
(pipercillin).
MOA: same as natural penicillin's
Spectrum of activity:
These drugs have spectrum similar to that of aminopenicillins but
also are effective against klebsiella and enterobacter species.
Tircacillin is active against P. aeruginosa combined with
clavulanic acid(timentin).
Pipercillin is more active than tircacillin against Pseudomonas
organisms.
Pipercillin and tazobactum it is a β-lactamase inhibitor that
expands the spectrum of activity to include staphylococci,
haemophylus, bacterioids.
Generally tazobactam does not enhance activity against
pseudomonas.
Therapeutic uses:
These are mainly used to treat serious infections caused by
gram negative organisms (sepsis, pneumonia, infections in
abdomen, bone and soft tissues).
Tazobactum/pipercillin is effective in treatment of nocosomal
pneumonia.
Precautions and monitoring:
Hypersensitivity reactions may occur.
Tircacillin may cause hypokalemia.
High dose content of tircacillin may pose a danger to patients
with heart failure.
All inhibit platelet aggregation which may result in bleeding.
Agent Elimination Half-life ROA Dosage
route
Pipercillin Renal 0.8-1.4hrs IV,IM 1.0-1.5mg/kg
every 6-12 hrs
Pipercillin/t Renal 0.7-1.2hrs IV 3.3g every 6hrs
azobactum
Ticarcillin/ Renal 1-1.5hrs IV 3.1g every 4-
clavulanic 6hrs
acid
Sulfonamides
Derivatives of sulfanilamide, these agents were the first drugs
to prevent and cure human bacterial infections successfully.
Sulfonamides remain drug of choice for certain infections.
The major sulfonamides are sulfadiazine, sulfamethoxazole,
sulfisoxazole and sulfamethizole.
MOA: sulfonamides are bacteriostatic, they suppress bacterial
growth by triggering a mechanism that blocks folic acid
synthesis, there by forcing bacteria to synthesize their own
folic acid.
Spectrum of activity:
Sulfonamides are broad spectrum agents with activity against
many gram positive organisms (s. pyogenes, s.pneumoniae)
and certain gram negative organisms (H. influenzae, E.coli).
They are also effective against certain strains of Chlamydia
trachomatis, nocardia, actinomyces and Bacillus anthracis.
Therapeutic uses:
Sulfonamides most often are used to treat urinary tract
infections caused by E.coli including acute and chronic cystitis
and chronic upper respiratory tract infections.
These agents are also used in nocardiasis, trachoma,
conjunctivitis and dermatitis.
Sulfadiazine may be administered in combination with
pyrimethamine to treat toxoplasmosis.
Sulfamethoxazole may be given in combination with
trymethoprim to treat pneumonia, enteritis, sepsis, UTI,
respiratory infections and gonococcal urethritis.
Sulfisoxazole is sometimes used in combination with
erythromycin ethylsuccinate to treat acute otitis media caused
by H. influenzae organisms.
Prophylactic sulfonamide therapy has been used
successfully to prevent streptococcal infections and
rheumatic fever recurrences.
Precautions and monitoring effects:
Sulfonamides may cause blood dyscrasias(hemolytic
anemia- particularly in patients with G6PD deficiency,
a plastic anemia, thrombocytopenia, agranulocytosis
and eosinophilia).
Hypersensitivity reactions include mostly in skin and
mucous membranes.
Manifestations include various types of skin rashes, exfoliate
dermatitis and photosensitivity.
Crystalluria and hematuria may occur possibly leading to UTI
obstruction, sulfonamides should be used cautionly in patients
with renal impairment.
AIDS patients have increased frequency of cutaneous
hypersensitivity reactions to sulfamethoxyzole.
Agent Elimination Half-life ROA Dosage
route
Sulfacytine Renal 4-4.5hrs Oral 250mg every
6hrs
Sulfadiazine Renal 6hrs Oral, IV 2-4g/day
Sulfamethoxazole Hepatic 9-11hrs Oral 1-3g/day
Sulfisoxazole Renal 3-7hrs Oral, IV 2-8g/day
Sulfamethizole Renal Oral 0.5-1g every
6-8hrs
Tetracycline's
These broad spectrum agents are effective against certain
bacterial strains that resist other antibiotics.
These drugs are preferred only in few situations.
The major drugs are democlocycline(declomycin),
doxycycline (vibramycin), minocycline (minocin), and
oxytetracyclin (terramycin).
MOA: these are bacteriostatic they inhibit bacterial protein
synthesis by binding to 30 S ribosomal subunits.
Spectrum of activity:
These are active against gram positive and gram negative
organisms spirochetes, rickettsial species and certain
protozoa.
Therapeutic uses:
These are agents of choice in rickettsial (rocky mountain
spotted fever), chlamidial and mycoplasmal infections,
amebiasis and bacillary infections.
Tetracycline's are useful alternatives of penicillin's in
treatment of anthrax, syphilis, gonorrhea, Lyme disease and
H.influenzae respiratory infections.
Oral or topical tetracycline's may be administered as a
treatment of acne.
Doxycycline is highly effective in prophylaxis of traveler’s
diarrhea.
Demeclocycline is used commonly as an adjunctive agent to
treat the syndrome of inappropriate antidiuretic hormone
secretion (SIADH).
GI distress is common in adverse effects of tetracyclines. This
problem can be minimized by administering the drug with
food or temporarily reducing the dose.
Phototoxic reactions may develop with exposure to sunlight.
This reaction is common with demoxycycline and
doxycycline.
Tetracycline's may cause hepatotoxicity particularly in
pregnant women.
Renally impaired patients may experience increased BUN
levels.
Tetracycline's may induce permanent tooth discoloration, tooth
enamel effects and retarded bone growth in infants and
children.
IV tetracyclines are irritating and may cause phlebitis.
Agent Eliminatio Half-life ROA Dosage
n route
Demeclocyclin Renal 10-17hrs Oral 300mg-1g/day
e
Doxycycline Hepatic 14-25hrs Oral,IV 100-200mg
every 12 hrs
Minocycline Heptic 12-15hrs Oral, IV 100-200mg
every 12 hrs
Oxytetracycline Renal 6-12 hrs Oral, 200-500mg
IM every 6hrs
Fluoroquinolines
These agents include ciprofloxacin, norfloxicin, ofloxicin,
moxifloxicin, levofloxicin and gemifloxicin.
MOA: these inhibit DNA gyrase.
Spectrum of activity: these are highly active against enteric
gram negative bacilli, salmonella, shigella, campylobacter,
haemophilus and neisseria.
Ciprofloxacin has an activity against P. aeruginosa and
some anaerobes.
It has moderate activity against M.tuberculosis
Gram positive organisms are less susceptible than gram
negative but usually are sensitive.
Therapeutic uses:
Norfloxicin is indicated for the oral treatment of UTI,
uncomplicated gonococcal infections and prostatitis.
Ciprofloxacin, ofloxicin and levofloxicin are available orally
and intravenously.
Ciprofloxacin is approved in use of UTI, LRTI, sinusitis,
bone, joint and skin structure infections, typhoid fever,
urethral and cervical gonococcal infections and diarrhea.
Ofloxicin approved for use in LRTI, uncomplicated
gonococcal and chlamydial cervicitis and urethritis,
prostatitis and UTI.
Levofloxicin is approved for treatment for UTI,
gemifloxicin, moxifloxicin and levofloxicin are also used in
lower respiratory tract infections and available orally.
Moxifloxicin is approved for treatment of complicated intra
abdominal infections but should not be used for UTI’s.
Precautions and monitoring:
Occasional adverse effects include nausea, dyspepsia,
headache, dizziness, insomnia, photosensitivity.
Infrequent adverse effects include rash, urticaria, leucopenia
and elevated liver enzymes, crystalluria occurs with high doses
at alkaline PH.
Agent Eliminatio Half-life ROA Dosage
n route
Ciprofloxicin Renal 5-6hrs IV 200-600mg
every 12hrs
Gemifloxicin Fecal 4-12hrs Oral 320mg once
daily
Levofloxicin Renal 8hrs IV, Oral 250-500mg
every 24hrs
Moxiflyg/doxi Hepatic 12hrs Oral 400mg
Miscellaneous agents
1. Aztreonam:
• This agent was the first commercially available monobactam.
• It resembles the amino glycosides in its efficacy against
many gram negative organisms but does not cause
nephrotoxicity or ototoxicity.
• MOA: Aztreonam is bactericidal, it inhibits bacterial cell
wall synthesis.
• Spectrum of activity: This drug is active against many gram
negative organisms, including Enterobacter
Therapeutic uses:
It is used for UTI infections, septicemia, skin infections, lower
respiratory infections.
Precautions and monitoring:
It sometimes causes, nausea, vomiting and diarrhea.
This drug may include skin rash.
Agent Elimination Half- ROA Dosage
route life
Aztreonam Renal 1.7hrs Oral, IV 50-100mg/kg/day
Chloram phenicol:
It is a nitrobenzene derivative, this drug has broad activity
against rickettsia as well as many gram negative organisms.
It is also effective against many ampicillin-resistant strains of
H. inluenzae.
MOA: it is bacterial bacteriostatic, sometimes it may be
bactericidal against a few bacterial strains.
Spectrum of activity: it is active against rickettsia and wide
range of bacteria, including H. influenza, salmonella typhi,
neisseria meningitis.
Therapeutic uses:
It can be used only to suppress infections that cannot be
treated effectively with other antibiotics.
It is used for typhoid, meningococcal infections in
cephalosporin allergic patients and anaerobic infections.
Rickettesial infections in pregnant patients, tetracycline
allergic patients and renally impaired patients.
Precautions and monitoring:
It can cause bone marrow suppression with resulting
pancytopenia rarely the drug leads to a plastic anemia.
Hypersensitivity reactions may occur.
This drug therapy may leads to grey baby syndrome.
Clindamycin
This agent has essentially replaced lincomycin, the drug from
which it is derived.
MOA: it is bacteriostatic. It binds to ribosomal subunit.
Spectrum of activity: this agent is active against most gram
positive and many anaerobic agents.
Therapeutic uses: it is used for abdominal and female
genitourinary tract infections.
Precautions and monitoring effects:
Clindamycin may cause rash, nausea, vomiting, diarrhea,
fever, abdominal pain and bloody stools. Blood dyscrasias
may occur.
Agent Elimination Half-life ROA Dosage
route
Clindamycin Hepatic 2-4hrs Oral, 300-900mg
IV,IM every 6-8hrs
Dapsone:
A member of sulfone class this drug is primary agent in
treatment of all forms of leprosy.
MOA: it is bateriostatic for mycobacterium leprae, its
mechanism is resembles the sulfonamides.
Spectrum of activity: this drug is active against M.leprae.
It also has same activity against Pneumocystis.carinil organisms
and malarial parasite plasmodium.
Therapeutic uses:
It is a drug of choice for treating leprosy.
This agent is also used in dermatitis herpetiformis (skin disorder).
Precautions and monitoring:
Hemolytic anemia may occur with daily doses> 200mg.
Nausea, vomiting and anorexia may develop.
Adverse CNS effects include headache, dizziness, nervousness, lethargy
and psychosis.
Other adverse effects includes skin rash, peripheral neuropathy, blurred
vision, hepatitis etc.,
Agent Elimination Half-life ROA Dosage
route
Dapsone Hepatic 28hrs Oral 50-100mg/day
Clofazimine:
It is a phenazine dye with antimicrobial and anti inflammatory
activity.
MOA: it appears to bind preferentially to mycobacterial DNA,
inhibiting replication and growth.
It is bactericidal against M.leprae.
It is active against various mycobacteria, M.leprae,
M.tuberculosis.
Clofazimine is used to treat leprosy and variety of
mycobacterium infections.
Pigmentation may occur in 75%to 100% patients within few
weeks.. This skin discoloration may lead to severe
depression(suicide).
Urine sweat and other body fluids may be discolored.
Agent Elimination Half-life ROA Dosage
route
Clofazimine Hepatic 70 days Oral 50-100mg/day
Rifaximin :
It is semi synthetic antibiotic structurally related to rifamycin.
MOA: it inhibits bacterial RNA synthesis by binding to the
β subunit of bacterial DNA dependent RNA polymerase.
This is non systematically absorbed drug has activity against
both enterotoxigenic strains of E.coli.
Therapeutic uses: it is used in treatment of travelers diarrhea
and noninvasive strains of E.coli and prophylaxis of hepatic
encephalopathy.
High resistant rates have been reported after 5 days of
treatment.
Precautions and monitoring:
Because of its limited systemic absorption adverse effects are
few but include constipation vomiting and headache.
Agent Eliminati Half-life ROA Dosage
on route
Rifaximin Fecal 6hrs Oral 200mg
t.i.d
Trimethroprim:
A substituted pyrimidine trimetroprim is most commonly
combined with sulfamethaxazole in preparation called co-
trimoxazole.
MOA: it inhibits the dihydrofoliate reductase thus blocking
bacterial synthesis of folic acid.
Spectrum of activity:
It is active against most gram negative and gram positive
organisms
Trimethroprim-sulfamethaxazole are active against a variety of
Organisms like S. pneumoniae, N. meningitis and
cornybacterium diptheriae.
Therapeutic uses:
It may be used alone or in combination with
sulfamethaxazole to treat UTI, klebsiella and enterobacter
organisms.
The combination therapy is effective for gonococcal urethritis,
chronic bronchitis and salmonella infections.
Precautions and Monitoring:
Most adverse effects involve the skin like rash, pruritis and
exfoliate dermatitis.
The combination therapy causes blood dyscrasias.
Adverse GI effects nausea, vomiting and epigastric distress.
Patients with AIDS may suffer with fever, rash, malaise and
pancytopenia.
Agent Elimination Half-life ROA Dosage
route
Trimethoprim Renal 8-15hrs Oral 100-
200mg/day
Metronidazole:
It is used in treatment of amebiasis, giardiasis and
trichomoniasis.
MOA: it is a synthetic compound with amebicidal and
trichomonacidal action. its mechanism of action involves
disruption of helical structure of DNA.
Spectrum of activity& therapeutic uses:
This is prefered drug in amebic dysentary, giardiasis and
trichomoniasis.
These are also active against all anaerobic cocci and gram
negative anaerobic bacilli.
Precautions and monitoring:
The most common adverse effect of this drug is
nausea, epigastric distress.
It is carcinogenic in mice and should not be used
unnecessarily.
Headache, vomiting, metallic taste and stomatitis have
been reported.
Agent Elimination Half-life ROA Dosage
route
Metronidazol Hepatic 1-1.6hrs Oral, IV 250-500mg every 6-
e 8hrs
You might also like
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Cover Kebijakan MutuDocument1 pageCover Kebijakan MutuSeptaPratamaAptNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- PHARMACOLOGY-introDocument18 pagesPHARMACOLOGY-introSeptaPratamaAptNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Principle of Drug ActionDocument15 pagesPrinciple of Drug ActionSeptaPratamaAptNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- PlagiarismDocument33 pagesPlagiarismMahrukh BaigNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Drug AntagonismDocument9 pagesDrug AntagonismSeptaPratamaAptNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Biaya Kuliah PMB 2020Document1 pageBiaya Kuliah PMB 2020SeptaPratamaAptNo ratings yet
- Stok Opname 28 Feb (Gudang) - 1Document144 pagesStok Opname 28 Feb (Gudang) - 1SeptaPratamaAptNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Infographic Antimicrobial Resistance 20140430 PDFDocument1 pageInfographic Antimicrobial Resistance 20140430 PDFMarkus AbiogNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Stok Opname 28 Feb (Gudang) - 1Document144 pagesStok Opname 28 Feb (Gudang) - 1SeptaPratamaAptNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Eligible Study Programmes by Partners Final1701191426Document130 pagesEligible Study Programmes by Partners Final1701191426Eko Bayu AjiNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Beta LactamDocument14 pagesBeta LactamSeptaPratamaAptNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Antimicrobial Stewardship PDFDocument37 pagesAntimicrobial Stewardship PDFSeptaPratamaAptNo ratings yet
- Drug Dose Adjustment in Chronic Renal Diseases: Medicine UpdateDocument7 pagesDrug Dose Adjustment in Chronic Renal Diseases: Medicine UpdateSeptaPratamaAptNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Antimicrobial StewardshipDocument37 pagesAntimicrobial StewardshipSeptaPratamaAptNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Ang 2 PDFDocument12 pagesAng 2 PDFSeptaPratamaAptNo ratings yet
- Invoice Septa UnajaDocument1 pageInvoice Septa UnajaSeptaPratamaAptNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- I Don't KnowDocument1 pageI Don't KnowSeptaPratamaAptNo ratings yet
- E1304amcp - 11.15.13 Final JMCP VersionDocument22 pagesE1304amcp - 11.15.13 Final JMCP VersionSeptaPratamaAptNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Probiotics For Prevention of Necrotizing Enterocolitis in Preterm Infants - AlFaleh, K - 2014 - Cochrane Library PDFDocument19 pagesProbiotics For Prevention of Necrotizing Enterocolitis in Preterm Infants - AlFaleh, K - 2014 - Cochrane Library PDFSeptaPratamaAptNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- E1304amcp - 11.15.13 Final JMCP VersionDocument22 pagesE1304amcp - 11.15.13 Final JMCP VersionSeptaPratamaAptNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Drug-Induced Nephrotoxicity: Cynthia A. Naughton, Pharmd, BCPS, North Dakota State University College of PharmacyDocument8 pagesDrug-Induced Nephrotoxicity: Cynthia A. Naughton, Pharmd, BCPS, North Dakota State University College of PharmacyAbdur Rachman Ba'abdullahNo ratings yet
- Order Obat 2Document4 pagesOrder Obat 2SeptaPratamaAptNo ratings yet
- 3rd LabDocument47 pages3rd LabUmair GulzarNo ratings yet
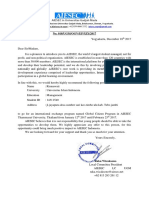
- No. 018/UGM/OGV/EP/XIX/2017: AIESEC in Universitas Gadjah MadaDocument2 pagesNo. 018/UGM/OGV/EP/XIX/2017: AIESEC in Universitas Gadjah MadaSeptaPratamaAptNo ratings yet
- Itinerary Visit ParisDocument1 pageItinerary Visit ParisSeptaPratamaAptNo ratings yet
- SSM Application SummaryDocument61 pagesSSM Application SummarySeptaPratamaAptNo ratings yet
- 1 s2.0 S0378427416329381 MainDocument1 page1 s2.0 S0378427416329381 MainSeptaPratamaAptNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- WHO - Indoor Air PollutionDocument484 pagesWHO - Indoor Air PollutionCosmo Deus100% (2)
- Denah ApotekDocument1 pageDenah ApotekSeptaPratamaAptNo ratings yet
- Cervical Changes During Menstrual Cycle (Photos)Document9 pagesCervical Changes During Menstrual Cycle (Photos)divyanshu kumarNo ratings yet
- Dysfunctional Uterine Bleeding (DUB)Document1 pageDysfunctional Uterine Bleeding (DUB)Bheru LalNo ratings yet
- Untitled Form - Google Forms00Document3 pagesUntitled Form - Google Forms00Ericka Rivera SantosNo ratings yet
- JAR Part 66 Examination Mod 03Document126 pagesJAR Part 66 Examination Mod 03Shreyas PingeNo ratings yet
- Rifle Threat Performance Matrix: SeriesDocument1 pageRifle Threat Performance Matrix: SeriesKuhnNo ratings yet
- BrainPOP Nutrition Quiz242342Document1 pageBrainPOP Nutrition Quiz242342MathableNo ratings yet
- Ideal Discharge Elderly PatientDocument3 pagesIdeal Discharge Elderly PatientFelicia Risca RyandiniNo ratings yet
- Non-Binary or Genderqueer GendersDocument9 pagesNon-Binary or Genderqueer GendersJuan SerranoNo ratings yet
- JOHARI Window WorksheetDocument2 pagesJOHARI Window WorksheetAnonymous j9lsM2RBaINo ratings yet
- Sample Quantitative Descriptive Paper 1Document20 pagesSample Quantitative Descriptive Paper 1oishimontrevanNo ratings yet
- MPSI OverviewDocument15 pagesMPSI OverviewZaqee AlvaNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Project Report On MKT Segmentation of Lux SoapDocument25 pagesProject Report On MKT Segmentation of Lux Soapsonu sahNo ratings yet
- Big Elephants Are Useful Mnemonics & IdiomsDocument144 pagesBig Elephants Are Useful Mnemonics & IdiomsNachoAndrésLlorente100% (1)
- Differential Partitioning of Betacyanins and Betaxanthins Employing Aqueous Two Phase ExtractionDocument8 pagesDifferential Partitioning of Betacyanins and Betaxanthins Employing Aqueous Two Phase ExtractionPaul Jefferson Flores HurtadoNo ratings yet
- BATES CH 6 The Thorax and LungsDocument2 pagesBATES CH 6 The Thorax and LungsAngelica Mae Dela CruzNo ratings yet
- Culturally Safe Classroom Context PDFDocument2 pagesCulturally Safe Classroom Context PDFdcleveland1706No ratings yet
- Stress Relieving, Normalising and Annealing: Datasheet For Non-Heat-TreatersDocument2 pagesStress Relieving, Normalising and Annealing: Datasheet For Non-Heat-TreatersGani PateelNo ratings yet
- Ott OTT Ecolog 1000 Water Level LoggerDocument3 pagesOtt OTT Ecolog 1000 Water Level LoggerNedimZ1No ratings yet
- Sialoree BotoxDocument5 pagesSialoree BotoxJocul DivinNo ratings yet
- Mrunal Handout 12 CSP20Document84 pagesMrunal Handout 12 CSP20SREEKANTHNo ratings yet
- Gut Health Elimination Diet Meal Plan FINALDocument9 pagesGut Health Elimination Diet Meal Plan FINALKimmy BathamNo ratings yet
- Biography of Murray (1893-1988) : PersonologyDocument6 pagesBiography of Murray (1893-1988) : PersonologyMing100% (1)
- Anatomy and Physiology Chapter 2Document28 pagesAnatomy and Physiology Chapter 2Marshalee FrancisNo ratings yet
- Easy Rasam Recipe Made Without Rasam PowderDocument6 pagesEasy Rasam Recipe Made Without Rasam PowderPrantik Adhar SamantaNo ratings yet
- Senior Cohousing - Sherry Cummings, Nancy P. KropfDocument86 pagesSenior Cohousing - Sherry Cummings, Nancy P. KropfAnastasia JoannaNo ratings yet
- UntitledDocument18 pagesUntitledSpace HRNo ratings yet
- Dirty Dozen List of Endocrine DisruptorsDocument4 pagesDirty Dozen List of Endocrine DisruptorsMariuszNo ratings yet
- SPKT Thiet Ke Co Khi 1Document33 pagesSPKT Thiet Ke Co Khi 1Chiến PhanNo ratings yet
- SpectraSensors TDL Analyzers in RefineriesDocument8 pagesSpectraSensors TDL Analyzers in Refineries1977specopsNo ratings yet
- Labor EstimateDocument26 pagesLabor EstimateAngelica CabreraNo ratings yet