Professional Documents
Culture Documents
Inborn Error of Metabolism Guide in Nutshell
Uploaded by
arjumandOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inborn Error of Metabolism Guide in Nutshell
Uploaded by
arjumandCopyright:
Available Formats
AIIMS- NICU protocols 2010
Approach to Inborn Errors of Metabolism Presenting in the Neonate
Suvasini Sharma, Pradeep Kumar, Ramesh Agarwal, Madhulika Kabra,
Ashok Deorari, Vinod Paul
Department of Pediatrics
All India Institute of Medical Sciences
Ansari Nagar, New Delhi –110029
Address for correspondence
Dr Ashok K Deorari
Professor
Department of Pediatrics
All India Institute of Medical Sciences
Ansari Nagar, New Delhi 110029
Email: ashokdeorari_56@hotmail.com
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Abstract
Inborn errors of metabolism (IEM) are an important cause of acute illness in newborns.
Presentation may mimic common neonatal conditions such as sepsis. Prompt detection
requires a high index of suspicion and the early measurement of biochemical markers
such as blood ammonia. Diagnosis is important not only for treatment but also for genetic
counselling. Guidelines for diagnosis and early management of IEM presenting in the
neonatal period are described.
Key words: Inborn errors of metabolism, encephalopathy, hyperammonemia
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Inborn errors of metabolism (IEM) are disorders in which there is a block at some point
in the normal metabolic pathway caused by a genetic defect of a specific enzyme. The
number of diseases in humans known to be attributable to inherited point defects in
metabolism now exceeds 500.1 While the diseases individually are rare, they collectively
account for a significant proportion of neonatal and childhood morbidity and mortality.
Diagnosis is important not only for treatment and prognostication but also for genetic
counselling and antenatal diagnosis in subsequent pregnancies.
Clinical Presentation:
Severe illness in the newborn, regardless of the underlying cause, tends to manifest with
non-specific findings, such as poor feeding, drowsiness, lethargy, hypotonia and failure
to thrive. IEM should be considered in the differential diagnosis of any sick neonate
along with common acquired causes such as sepsis, hypoxic-ischemic encephalopathy,
duct-dependant cardiac lesions, congenital adrenal hyperplasia and congenital infections.
Clinical pointers towards an underlying IEM include2:
• Deterioration after a period of apparent normalcy
• Parental consanguinity
• Family history of unexplained neonatal deaths
• Rapidly progressive encephalopathy and seizures of unexplained cause
• Severe metabolic acidosis
• Persistent vomiting
• Peculiar odor (urine, cerumen)
• Acute fatty liver or HELLP (hemolysis, elevated liver enzymes & low platelet
counts) during pregnancy: seen in women carrying fetuses with long-chain-3-
hydroxyacyl-coenzyme dehydrogenase deficiency (LCHADD).
Table 1 describes examination findings that may provide a clue to the underlying IEM.
Patterns of presentation include2,3:
1) Encephalopathy with or without metabolic acidosis: encephalopathy, seizures,
and tone abnormalities are predominant presenting features of organic acidemias,
urea cycle defects and congenital lactic acidosis. Isolated intractable seizures are
prominent in pyridoxine dependency, pyridoxal phopspahte dependency, folinic-
acid responsive seizures, and glucose transporter 1 defeciency. 4
2) Acute liver disease: This could manifest as-
• Jaundice alone- Gilbert syndrome, Criggler-Najjar syndrome
• Hepatic failure (jaundice, ascites, hypoglycemia, coagulopathy)-
Tyrosinemia, galactosemia, neonatal hemochromatosis, glycogen storage
disease type IV.
• Neonatal cholestasis: alpha-1 antitrypsin deficiency, Niemann-Pick
disease type C.
• Hypoglycemia: persistent and severe hypoglycemia may be an indicator of
an underlying IEM. Hypoglycemia is a feature of galactosemia, fatty acid
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
oxidation defects, organic acidemias, glycogen storage disorders and
disorders of gluconeogenesis.
3) Dysmorphic features: seen in peroxisomal disorders, pyruvate dehydrogenase
deficiency, congenital disorders of glycosylation (CDG), and lysosomal storage
diseases. Some IEMs may present with non-immune hydrops fetalis; these include
lysosomal storage disorders and CDG.
4) Cardiac disease: cardiomyopathy is a prominent feature in some IEM including
fatty acid oxidation defects, glycogen storage disease type II and mitochondrial
electron transport chain defects.
Investigations
Metabolic investigations should be initiated as soon as the possibility is considered. The
outcome of treatment of many IEM especially those associated with hyperammonemia is
directly related to the rapidity with which problems are detected and appropriate
management instituted.
First line investigations (metabolic screen):
The following tests should be obtained in ALL babies with suspected IEM.
1) Complete blood count: (neutropenia and thrombocytopenia seen in propionic and
methylmalonic academia)
2) Arterial blood gases and electrolytes
3) Blood glucose
4) Plasma ammonia (Normal values in newborn: 90-150 µg/dl or 64-107 µmol/L)
5) Arterial blood lactate (Normal values: 0.5-1.6 mmol/L)
6) Liver function tests
7) Urine ketones
8) Urine reducing substances.
9) Serum uric acid (low in molybdenum cofactor deficiency).
Figure 1 gives the algorithmic approach to a newborn with suspected IEM. Disease
category can be diagnosed based on blood ammonia, blood gas analysis and urine ketone
testing. Hyperammonemia without acidosis is caused by urea cycle defects. Metabolic
acidosis with or without hyperammonemia is a feature of organic acidemias and fatty
acid oxidation defects. Figure 2 explains the algorithmic approach to neonate with
persistent hypoglycemia and suspected underlying IEM. Table 2 explains the
categorization of IEM based on simple metabolic screening tests.
Second line investigations (ancillary and confirmatory tests)
These tests need to be performed in a targeted manner, based on presumptive diagnosis
reached after first line investigations:
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
1) Gas chromatography mass spectrometry (GCMS) of urine- for diagnosis of
organic acidemias.
2) Plasma amino acids and acyl carnitine profile: by tandem mass spectrometry
(TMS)- for diagnosis of organic acidemias, urea cycle defects, aminoacidopathies
and fatty acid oxidation defects.
3) High performance liquid chromatography (HPLC): for quantitative analysis of
amino acids in blood and urine; required for diagnosis of organic acidemias and
aminoacidopathies.
4) Lactate/pyruvate ratio- in cases with elevated lactate.
5) Urinary orotic acid- in cases with hyperammonemia for classification of urea
cycle defect.
6) Enzyme assay: This is required for definitive diagnosis, but not available for most
IEM’s. Available enzyme assays include: biotinidase assay- in cases with
suspected biotinidase deficiency (intractable seizures, seborrheic rash, alopecia);
and . GALT (galactose 1-phosphate uridyl transferase) assay- in cases with
suspected galactosemia (hypoglycemia, cataracts, reducing sugars in urine).
7) Neuroimaging: MRI may provide helpful pointers towards etiology while results
of definitive investigations are pending. Some IEM may be associated with
structural malformations e.g. Zellweger syndrome has diffuse cortical migration
and sulcation abnormalities. Agenesis of corpus callosum has been reported in
Menke’s disease, pyruvate decarboxylase deficiency and nonketotic
hyperglycinemia.5 Examples of other neuroimaging findings in IEM include:
• Maple syrup urine disease (MSUD): brainstem and cerebellar edema
• Propionic & methylmalonic acidemia: basal ganglia signal change
• Glutaric aciduria: frontotemporal atrophy, subdural hematomas
8) Magnetic resonance spectroscopy (MRS): may be helpful in selected disorders
E.g. lactate peak elevated in mitochondrial disorders, leucine peak elevated in
MSUD.
9) Urine for alpha-aminoadipic semialdehyde, - elevated in pyridoxine dependent
seizures. (test not available in India yet).4
10) Electroencephalography (EEG): some EEG abnormalities may be suggestive of
particular IEM; e.g. comb-like rhythm in MSUD, burst suppression in NKH and
holocarboxylase synthetase deficiency. 6
11) Plasma very long chain fatty acid (VLCFA) levels: elevated in peroxisomal
disorders.
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
12) Mutation analysis when available.
13) CSF aminoacid analysis: CSF Glycine levels elevated in NKH.
Precautions to be observed while collecting samples
1. Should be collected before specific treatment is started or feeds are stopped, as
may be falsely normal if the child is off feeds.
2. Samples for blood ammonia and lactate should be transported in ice and
immediately tested. Lactate sample should be arterial and should be collected
after 2 hrs fasting in a preheparinized syringe. Ammonia sample is to be collected
approximately after 2 hours of fasting in EDTA vacutainer. Avoid air mixing.
Sample should be free flowing.
3. Detailed history including drug details should be provided to the lab. (sodium
valproate therapy may increase ammonia levels).
Samples to be obtained in infant with suspected IEM when diagnosis is uncertain
and death seems inevitable (Metabolic autopsy)7,8
1. Blood: 5-10 ml; frozen at -200C; both heparinized (for chromosomal
studies) and EDTA (for DNA studies) samples to be taken
2. Urine: frozen at –20oC
3. CSF: store at –20oC
4. Skin biopsy: 3 X 2 mm full thickness in culture medium or saline with
glucose. Store at 4-80C. Do not freeze.
5. Liver and muscle biopsy: for histopathology, electron microscopy, and
enzyme studie.
6. Kidney and heart biopsy: as indicated.
7. Clinical photograph (in cases with dysmorphism)
8. Infantogram (in cases with skeletal abnormalities)
Treatment
In most cases, treatment needs to be instituted empirically without a specific diagnosis.
The metabolic screen helps to broadly categorize the patient’s IEM (e.g. urea cycle
defect, organic academia, congenital lactic acidosis etc), on the basis of which, empirical
treatment can be instituted.
Aims of treatment
1. To reduce the formation of toxic metabolites by decreasing substrate availability
(by stopping feeds and preventing endogenous catabolism)
2. To provide adequate calories
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
3. To enhance the excretion of toxic metabolites.
4. To institute co-factor therapy for specific disease and also empirically if diagnosis
not established.
5. Supportive care- treatment of seizures (avoid sodium valproate – may increase
ammonia levels), maintain euglycemia and normothermia, fluid, electrolyte &
acid-base balance, treatment of infection, mechanical ventilation if required.
Management of hyperammonemia9, 10
1) Discontinue all feeds. Provide adequate calories by intravenous glucose and
lipids. Maintain glucose infusion rate 8-10 mg/kg/min. Start intravenous lipid 0.5
g/kg/day (up to 3g/kg/day). After stabilization gradually add protein 0.25 g/kg till
1.5 g/kg/day.
2) Dialysis is the only means for rapid removal of ammonia, and hemodialysis is
more effective and faster than peritoneal dialysis, however peritoneal dialysis may
be more widely available and feasible. Exchange transfusion is not useful.
3) Alternative pathways for nitrogen excretion-:
Sodium benzoate (IV or oral)- loading dose 250 mg/kg then 250-400 mg/kg/day
in 4 divided doses. (Intravenous preparation not available in India).
Sodium phenylbutyrate (not available in India)-loading dose 250 mg/kg followed
by 250-500 mg/kg/day.
L-arginine (oral or IV)- 300 mg/kg/day (Intravenous preparation not available in
India)
L-carnitine (oral or IV)- 200 mg/kg/day
4) Supportive care: treatment of sepsis, seizures, ventilation. Avoid sodium
valproate.
Acute management of newborn with suspected organic acidemia11
1) The patient is kept nil per orally and intravenous glucose is provided.
2) Supportive care: hydration, treatment of sepsis, seizures, ventilation.
3) Carnitine: 100 mg/kg/day IV or oral.
4) Treat acidosis: Sodium bicarbonate 0.35-0.5mEq/kg/hr (max 1-2mEq/kg/hr)
5) Start Biotin 10 mg/day orally.
6) Start Vitamin B12 1-2 mg/day I/M (useful in B12 responsive forms of
methylmalonic acidemias)
7) Start Thiamine 300 mg/day (useful in thiamine-responsive variants of MSUD).
8) If hyperammonemia is present, treat as explained above.
Management of congenital lactic acidosis
1) Supportive care: hydration, treatment of sepsis, seizures, ventilation. Avoid
sodium valproate.
2) Treat acidosis: sodium bicarbonate 0.35-0.5mEq/kg/hr (max 1-2mEq/kg/hr)
3) Thiamine: up to 300 mg/day in 4 divided doses.
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
4) Riboflavin: 100 mg/day in 4 divided doses.
5) Add co-enzyme Q: 5-15 mg/kg/day
6) L-carnitine: 50-100 mg/kg orally.
7) Biotin 10 mg/day. (Biotin responsive Multiple carboxylase deficiency may
present with unexplained lactic acidosis)12
Treatment of newborn with refractory seizures with no obvious etiology (suspected
metabolic etiology)4, 13
1) If patient persists to have seizures despite 2 or 3 antiepileptic drugs in adequate
doses, consider trial of pyridoxine 100 mg intravenously. If intravenous
preparation not available, oral pyridoxine can be given (15 mg/kg/day).
2) If seizures persist despite pyridoxine, give trial of biotin 10 mg/day and folinic
acid 5mg twice daily (folinic acid responsive seizures). Trial of pyridoxal
phosphate 10 mg/kg/dose X 2 doses is also recommended, however this is not
available in India.
3) Rule out glucose transporter defect: measure CSF and blood glucose. In glucose
transporter defect, CSF glucose level is equal to or less than 1/3rd of the blood
glucose level. This disorder responds to the ketogenic diet.
Management of asymptomatic newborn with a history of sibling death with
suspected IEM:
1) After baseline metabolic screen, start oral dextrose feeds (10% dextrose).
2) After 24 hours, repeat screen. If normal, start breast feeds. Monitor sugar, blood
gases and urine ketones, blood ammonia 6 hourly.
3) Some authorities recommend starting medium chain triglycerides (MCT oil)
before starting breast feeds,3 however, this is not being followed in our center
(because of unpalatibility of MCT oil).
4) After 48 hours, repeat metabolic screen. Obtain samples for TMS and urine
organic acid tests.
5) The infant will need careful observation and follow-up for the first few months, as
IEM may present in different age groups in members of the same family.
Long term treatment of IEM
The following modalities are available:
1) Dietary treatment: This is the mainstay of treatment in phenylketonuria, maple syrup
urine disease, homocystinuria, galactosemia, and glycogen storage disease Type I & III.
Special diets for PKU and MSUD are commercially available in the west. These are not
available in India, but can be imported. These special diets are however very expensive,
and cannot be afforded by most Indian patients. Based on the amino acid content of some
common food products available in India, dietary exchanges are calculated and a low
phenylalanine diet for PKU and diet low in branched chain amino acids for MSUD are
being used in our center. However, there are no studies to document the efficacy of these
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
indigenous diets. Some disorders like urea cycle disorders and organic acidurias require
dietary modification (protein restriction) in addition to other modalities.1The ketogenic
diet is the treatment of choice for glucose transporter 1 defiency and pyruvate
dehydrogenase deficiency.
2) Enzyme replacement therapy (ERT): ERT is now commercially available for some
lysosomal storage disorders.15 However, these disorders do not manifest in the newborn
period, an exception being Pompe’s disease (Glycogen storage disorder Type II) which
may present in the newborn period and for which ERT is now available.
3) Cofactor replacement therapy: The catalytic properties of many enzymes depend on
the participation of non protein prosthetic groups, such as vitamins and minerals, as
obligatory cofactors. The following co-factors may be beneficial in certain IEM: 16
• Thiamine: mitochondrial disorders, thiamine responsive variants of
MSUD, PDH deficiency & complex I deficiency)
• Riboflavin: Glutaric aciduria Type I, Type II, mild variants of ETF, ETF-
DH, complex I deficiency
• Pyridoxine: 50% of cases of homocystinuria due to cystathionine β-
synthetase deficiency, pyridoxine dependency with seizures, xanthurenic
aciduria, primary hyperoxaluria type I, Hyperornithemia with gyrate
atrophy
• Cobalamin: Methylmalonic academia (cblA, cblB), Homocystinuria and
methylmalonic academia (cblC, cblD, cblF)
• Folinic acid: Hereditary orotic aciduria, Methionine synthase deficiency,
Cerebral folate transporter deficiency, hereditary folate malabsorption,
Kearns-Sayre syndrome
• Biotin: Biotinidase deficiency, holocarboxylase synthetase deficiency
Prevention
1) Genetic counselling and prenatal diagnosis: Most of the IEM are single gene
defects, inherited in an autosomal recessive manner, with a 25% recurrence risk.
Therefore when the diagnosis is known and confirmed in the index case, prenatal
diagnosis can be offered, wherever available for the subsequent pregnancies. The
samples required are chorionic villus tissue or amniotic fluid. Modalities
available are:17
• Substrate or metabolite detection: useful in phenylketonuria, peroxisomal
defects.
• Enzyme assay: useful in lysosomal storage disorders like Niemann-Pick
disease, Gaucher disease.
• DNA based (molecular) diagnosis: Detection of mutation in proband/
carrier parents is a prerequisite.
2) Neonatal screening: Tandem mass spectrometry is used in some countries for
neonatal screening for IEM. Disorders which can be detected by TMS include
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
aminoacidopathies ( phenylketonuria, MSUD, Homocystinuria, Citrullinemia,
Argininosuccinic aciduria, hepatorenal tyrosinemia), fatty acid oxidation defects,
organic acidemias (glutaric aciduria, propionic acidemia, methylmalonic
acidemia, isovaleric acidemia). The appropriate time for collection of samples is
between 1 and 3 days of life. The cost of this procedure is high, a potent dis-
inventive for resource poor countries like India. Also, the though the test is highly
sensitive, the specificity is relatively low; and there are difficulties in
interpretation of abnormal test results in apparently healthy infants.
Conclusion
IEM collectively represent an important cause of morbidity and death in the neonatal
period. The most important step in the diagnosis of IEM is clinical suspicion. Screening
investigations such as arterial blood gases, blood ammonia, lactate, sugar and urine
ketones help to categorize the possible IEM and guide immediate management.
Appropriate immediate treatment not only improves survival but also reduces the chances
of neurodevelopmental sequelae.
Do’s and Don’t’s
1) Don’t think of IEM as rare, exotic and untreatable disorders.
2) Think of IEM in sick newborns in parallel with other common conditions
such as sepsis. The signs and symptoms are usually non specific such as
lethargy, poor feeding and vomiting.
3) Observe the precautions as explained while collecting and storing samples
4) Even if the chances of survival appear bleak, every attempt must be made
to reach a diagnosis so that parents can be guided for future pregnancy.
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
References
1) Childs B, Valle D, Jimenez-Sanchez. The Inborn error and biochemical
variability. In: Scriver CR, Beaudet AL, Sly WS & Valle D (eds). The metabolic
and molecular basis of inherited disease, 8th ed, New York: McGraw-Hill, 2001:
155-166.
2) A Clinical guide to inherited metabolic diseases. JTR Clarke. 3rd Ed (2006),
Cambridge University Press, Cambridge.
3) Cataltepe SU, Levy HL. Inborn errors of metabolism. In: Cloherty JP, Eichenwald
EC, Stark AR eds. Manual of neonatal care. 6th Edition. Lippincott Williams &
Wilkins 2008; Philadelphia: 558-573.
4) Pearl PS. New treatment paradigms for neonatal metabolic epilepsises. J Inherit
Metab Dis 2009; 32: 204-213.
5) Blaser S, Feigenbaum A. A neuroimaging approach to inborn errors of
metabolism. Neuroimag Clin N Am 2004; 14: 307-329.
6) Nordli DR, De Vivo DC. Classification of infantile seizures: Implications for
identification and treatment of inborn errors of metabolism. J Child Neurol 2002;
17 (Suppl 3): 3S3-3S8.
7) Leonard JV, Morris AAM. Diagnosis and early management of inborn errors of
metabolism presenting around the time of birth. Acta Pediatrica 2006; 95: 6-14.
8) Christodoulou J, Wilcken B. Perimortem laboratory investigation of genetic
metabolic disorders. Semin Neonataol 2004; 9: 275-280.
9) Summar M. Current strategies for the management of neonatal urea cycle
disorders. J Pediatr 2001; 38: S30-S39.
10) Leonard JV, Morris AAM. Urea cycle disorders. Semin Neonatol 2002; 7: 27-35.
11) de Baulny HO, Saudubray JM. Branched-chain organic acidurias. Semin Neonatol
2002; 7: 65-74.
12) Saudubray JM, Nassogne MC, de Lonlay P, Touati G. Clinical approach to
inherited metabolic disorders in neonates: an overview. Semin Neonatol 2002; 7:
3-15.
13) Wolf NI, Bast T, Surtees S. Epilepsy in inborn errors of metabolism. Epileptic
Disord 2005; 7(2): 67-81.
14) Kabra M. Dietary management of Inborn errors of metabolism. Indian J Pediatr
2002; 69: 421-426.
15) Brady RO, Schiffmann R. Enzyme-replacement therapy for metabolic storage
disorders. Lancet Neurol 2004; 3: 752-756.
16) Saudubray JM, Sedel F, Walter JH. Clinical approach to treatable inborn
metabolic diseases: an introduction. J Inherit Metab Dis 2006; 29: 261-274.
17) Elias S, Simpson JL, Shulman LP. Techniques for prenatal diagnosis. In: Rimoin
DL, Connor JH, Pyeritz RE, Korf BR eds. Emery and Rimoin’s Principles and
practice of medical genetics. Churchill-Livingstone, London 2002: 802-825.
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Table 1: Clinical pointers towards specific IEM’s
Clinical finding Disorder
Coarse facies Lysosomal disorders
Cataract Galactosemia, Zellweger syndrome
Retinitis pigmentosa Mitochondrial disorders
Cherry red spot Lipidosis
Hepatomegaly Storage disorders, urea cycle defects
Renal enlargement Zellweger syndrome
Eczema/alopecia Biotinidase deficiency
Abnormal kinky hair Menke disease
Decreased pigmentation Phenylketonuria
Hiccups Nonketotic hyperglycinemia
Ophthalmoplegias MSUD, Nonketotic hyperglycinemia
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
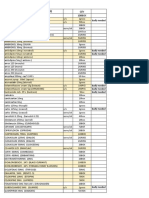
Table 2: Categorization of neonatal IEM using metabolic screening tests
Acidosis Ketosis Lactate Ammonia Diagnosis
- + - - Maple syrup urine
disease
+ +/- - +/- Organic aciduria
+ +/- + - Lactic acidosis
- - - + Urea cycle
- - - - Non-ketotic
hyperglycinemia , sulfite
oxidase deficiency,
peroxisomal,
Phenylketonuria,
galactosemia
Fig 1: Approach to newborn with suspected metabolic disorder
Suspected Metabolic Disorder
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Plasma NH3
High Normal
Blood pH & CO2 Blood pH & CO2
Normal Acidosis Normal
(PKU, NKH, Galactosemia,
Peroxisomal disorders,
Aminoacidopathies)
No ketosis No ketosis
Ketosis with or without
Lactic acidosis
Urea cycle defect FAOD Organic acidemias
Mitochondrial disorders
Plasma citrulline
↑↑↑ ↓↓↓
(>1000 µmol/L) 25-50µmol/L) (Undetectable)
ASA deficiency Urinary ASA Urinary orotic acid
(citrullinemia)
+ - + -
ASAL deficiency THAN OTC CPS/NAGS
(ASAuria) deficiency deficiency
(Abbreviations: FAOD: fatty acid oxidation defects, PKU: Phenylketonuria, NKH:
Nonketotic hyperglycinemia, ASA: Argininosuccinic acid, OTC: Ornithine
transcarbamoylase, CPS: carbamoyl phosphate synthetase I; NAGS: N-acetylglutamate
synthetase, THAN: transient hyperammonemia of newborn, ASAL: argininosuccinic acid
lyase)
Figure 2: Approach to newborn with persistent hypoglycemia and suspected IEM
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Hypoglycemia
Urine nonglucose reducing substances
Present Absent
Urine ketones
Positive Negative
Glycogen storage Fatty acid
Diseases Oxidative defects
Gluconeogenic defects Ketogenesis defects
Galactosemia Organic acidemias Hyperinsulinism
Appendix: Commercially available formulations used in IEM
Co-factor Trade name, formulation
Downloaded from www.newbornwhocc.org
AIIMS- NICU protocols 2010
Pyridoxine Tab Benadon (40mg) (Nicholas Piramal),
Inj Vitneurin (1 ampoule contains 50 mg
pyridoxine)
Hydroxycobalamin (Vitamin B12) Inj Trineurosol (1000mcg/ml)
(Tridoss Laboratories)
Thiamine Tab Benalgis (75 mg) (Franco India)
Riboflavin Tab Riboflavin (5 mg) (Shreya)
Biotin Tab Essvit (5mg, 10mg) (Ecopharma)
Carnitine Syrup L-Carnitor (5ml=500 mg), Tab L-
Carnitor (500 mg), Inj carnitor (1g/5ml)
(Elder)
Folinic acid Tab Leukorin (15 mg) (Samrath)
Sodium Benzoate Satchet 20g (Hesh Co.)
Arginine ARG-9 Satchet (3g) (Noveau Medicament)
Coenzyme Q Tab CoQ 30 mg, 50 mg. (Universal
Medicare)
Downloaded from www.newbornwhocc.org
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- IMPORTANT Renal ImagingDocument58 pagesIMPORTANT Renal ImagingarjumandNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- MRCPCH - Renal ImagingDocument28 pagesMRCPCH - Renal ImagingarjumandNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Test of Hearing and Pure Tone AudiometryDocument35 pagesTest of Hearing and Pure Tone AudiometryarjumandNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Asplenia ProtocolDocument5 pagesAsplenia ProtocolarjumandNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- MRCPCH - Important Skin DiseasesDocument42 pagesMRCPCH - Important Skin DiseasesarjumandNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- IMPORTANT Renal ImagingDocument58 pagesIMPORTANT Renal ImagingarjumandNo ratings yet
- Inborn Error of Metabolism - NotesDocument5 pagesInborn Error of Metabolism - NotesarjumandNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- List of Antidotes: No. Drugs AntidoteDocument3 pagesList of Antidotes: No. Drugs AntidotearjumandNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- MRCPCH - EnuresisDocument16 pagesMRCPCH - EnuresisarjumandNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Approach To ImmunodeficiencyDocument31 pagesApproach To ImmunodeficiencyarjumandNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Neonatal Neurological Emergencies - FINALDocument11 pagesNeonatal Neurological Emergencies - FINALarjumandNo ratings yet
- KETOGENIC DIET HELPS CONTROL SEIZURESDocument1 pageKETOGENIC DIET HELPS CONTROL SEIZURESarjumand100% (1)
- BMJ Pediatric Asthma in A NutshellDocument14 pagesBMJ Pediatric Asthma in A NutshellarjumandNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- INITIAL Laboratory Evaluation For Inborn Errors of Metabolism (UPTODATE)Document1 pageINITIAL Laboratory Evaluation For Inborn Errors of Metabolism (UPTODATE)arjumandNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- UPTODATE Lab Evaluation Persistent Neonatal HypoglycemiaDocument1 pageUPTODATE Lab Evaluation Persistent Neonatal HypoglycemiaarjumandNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- DR Shirin Surani Resident Year 1Document29 pagesDR Shirin Surani Resident Year 1arjumandNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Pediatric Influenza Clinical Practice Guidelines - Rev0117Document3 pagesPediatric Influenza Clinical Practice Guidelines - Rev0117arjumandNo ratings yet
- Neonatal GE EmergenciesDocument13 pagesNeonatal GE EmergenciesarjumandNo ratings yet
- Paediatric Rashes: Ali Faisal SaleemDocument51 pagesPaediatric Rashes: Ali Faisal Saleemarjumand100% (2)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- 13InsulinAgType1 PDFDocument1 page13InsulinAgType1 PDFZsákaiAntalNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Approach To AnemiaDocument24 pagesApproach To AnemiaarjumandNo ratings yet
- TOACSDocument18 pagesTOACSarjumandNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Bone Changes of Congenital HypothyroidismDocument1 pageBone Changes of Congenital HypothyroidismarjumandNo ratings yet
- Interpretation of Hepatitis B Serologic Test ResultsDocument1 pageInterpretation of Hepatitis B Serologic Test ResultsarjumandNo ratings yet
- PEDIATRIC RADIOLOGY QuestionsDocument35 pagesPEDIATRIC RADIOLOGY QuestionsarjumandNo ratings yet
- Zygoma Fixture in The Management of Advanced Atrophy of The Maxilla Technique and Long Term ResultsDocument17 pagesZygoma Fixture in The Management of Advanced Atrophy of The Maxilla Technique and Long Term ResultspedroNo ratings yet
- Managing Posterior Polar CataractDocument5 pagesManaging Posterior Polar CataractRajinder Kumar BassanNo ratings yet
- Contracted Endodontic AccessDocument48 pagesContracted Endodontic AccessSanket Pandey93% (27)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- The Clinical Assessment of Infants, Preschoolers and Their Families - IACAPAPDocument22 pagesThe Clinical Assessment of Infants, Preschoolers and Their Families - IACAPAPcpardilhãoNo ratings yet
- Records and Reports DocumentationDocument18 pagesRecords and Reports DocumentationJomarNo ratings yet
- Alternative Medicine Magazine December 2005Document140 pagesAlternative Medicine Magazine December 2005Irma Sari MuliadiNo ratings yet
- LeukemiaDocument44 pagesLeukemiaAnn Pauline GoducoNo ratings yet
- Towards A Culturally Centered Music Therapy PracticeDocument8 pagesTowards A Culturally Centered Music Therapy PracticeAnonymous RzMJ9cNo ratings yet
- Nasogastric Tube InsertionDocument17 pagesNasogastric Tube InsertionMichael Jude MedallaNo ratings yet
- Artigo 1Document4 pagesArtigo 1Everton PaesNo ratings yet
- The Effects of Two Vitamin D Regimens On Ulcerative Colitis Activity Index, Quality of Life and Oxidant/anti-Oxidant StatusDocument8 pagesThe Effects of Two Vitamin D Regimens On Ulcerative Colitis Activity Index, Quality of Life and Oxidant/anti-Oxidant StatusLeonardo AzevedoNo ratings yet
- Pediatric NeurologyDocument149 pagesPediatric Neurologyannyzhuk100% (2)
- Nursing Care Plan: Classwork Format Level I CCMC-CN Second Semester A.Y. 2020-2021Document6 pagesNursing Care Plan: Classwork Format Level I CCMC-CN Second Semester A.Y. 2020-2021Mary Ella Mae PilaNo ratings yet
- NPS Medicines ListDocument2 pagesNPS Medicines ListCin BinNo ratings yet
- How to Promote Wound HealingDocument7 pagesHow to Promote Wound HealingGabz GabbyNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Cross-Cultural Conference Presentation 02072018 StandardDocument33 pagesCross-Cultural Conference Presentation 02072018 Standardapi-298976119No ratings yet
- Orthotic Intervention For The Hand and Upper Extremity Splinting PrinciplesDocument61 pagesOrthotic Intervention For The Hand and Upper Extremity Splinting Principleskevin.smart540No ratings yet
- Lasa DrugsDocument4 pagesLasa Drugsvijay kumarNo ratings yet
- Beta Glucan Book PDFDocument51 pagesBeta Glucan Book PDFnvestgrrlNo ratings yet
- Foot phalanges anatomy and growthDocument9 pagesFoot phalanges anatomy and growthAfif MansorNo ratings yet
- OcdDocument9 pagesOcdapi-334485329No ratings yet
- SativexDocument9 pagesSativexkarenvilledaNo ratings yet
- Mga OorderinDocument7 pagesMga OorderinMary Ann Tobias VeraNo ratings yet
- (10920684 - Neurosurgical Focus) Novel Technique For Trialing Peripheral Nerve Stimulation - Ultrasonography-Guided StimuCath TrialDocument7 pages(10920684 - Neurosurgical Focus) Novel Technique For Trialing Peripheral Nerve Stimulation - Ultrasonography-Guided StimuCath TrialSebastiano SerraNo ratings yet
- CHEST Releases New Guidelines For Antithrombotic Therapy For VTE DiseaseDocument2 pagesCHEST Releases New Guidelines For Antithrombotic Therapy For VTE DiseaseИгорь БалдинNo ratings yet
- Food PoisoningDocument11 pagesFood PoisoningLeanne Teh100% (1)
- Bib OverviewDocument100 pagesBib OverviewMithun RajNo ratings yet
- SinnusitisDocument15 pagesSinnusitisAbigail BrillantesNo ratings yet
- Snake Bite SEODocument7 pagesSnake Bite SEOMitra Nabizadeh33% (3)
- Stretching - Inservice - Final Eddie PizzoDocument18 pagesStretching - Inservice - Final Eddie PizzoMatthew PuglieseNo ratings yet
- Is That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeFrom EverandIs That a Fact?: Frauds, Quacks, and the Real Science of Everyday LifeRating: 4.5 out of 5 stars4.5/5 (3)
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincFrom EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincRating: 3.5 out of 5 stars3.5/5 (137)
- The Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsFrom EverandThe Disappearing Spoon: And Other True Tales of Madness, Love, and the History of the World from the Periodic Table of the ElementsRating: 4 out of 5 stars4/5 (146)
- Science Goes Viral: Captivating Accounts of Science in Everyday LifeFrom EverandScience Goes Viral: Captivating Accounts of Science in Everyday LifeRating: 5 out of 5 stars5/5 (1)