Professional Documents
Culture Documents
Asthma
Asthma
Uploaded by
Ainil Maksura0 ratings0% found this document useful (0 votes)
10 views6 pagesAsma
Copyright
© © All Rights Reserved
Available Formats
PDF or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAsma
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views6 pagesAsthma
Asthma
Uploaded by
Ainil MaksuraAsma
Copyright:
© All Rights Reserved
Available Formats
Download as PDF or read online from Scribd
You are on page 1of 6
Asthma
‘Matthew C. Tews, DO
Key Points
+ Patients with severe asthme exaceibations may have
such severe restriction of aifiow that they do nat exhibit
wheezing on examination.
Beta? agonists are the mainstay of treatment for acute
asthma exacerbations
Comtiasteods should be ven to patients who do not
respond intl to beta? agonists and in these with
moderate to severe exacerbations.
INTRODUCTION
Asthmais a chronic disorder ofthe airways thatis astociated
with infammation, bronchial hyperreactivity, and intermit-
tent airflow obstruction. The most common chron disease
in childhood, itis also common in the adult population.
Presentations of acuteasthma account for more than 2 mil~
lion emergency department (ED) visits annually. The causes
are mulifactoria, but the pathophysiology is characterized
by the release of inflammatory cell mediators that lead 10
airway smooth muscle constriction, pulmonary vasculature
leakage, and mucous gland secretion.
‘Asthma is characteriaed by progressive shortness of
breath, variable airflow obstruction, and wheezing Symp-
toms fluctuate over time, and patients with worsening,
symptoms due to a trigger are considered to havean “exac~
erbation” and require prompt treatment to reverse the
airflow obstruction.
CLINICAL PRESENTATION
‘An acute asthma presentation is due to a decrease in expi-
ratory airflow and is characterized by progressive symp-
‘toms of shortness of breath, a nonproductive cough, and.
89
‘+ Peak expiratory flow rate and forced expiratory volume
in 1 second are objective measures ofthe severity of a
patient's asthma exacerbation and should be followed
sesally to measure improvement.
‘wheezing inal ung feds. Symptoms may develop over a
period of hours, days or weeks, but often there is an acute
worsening that prompts the patient to sek medical care.
‘The most common trigger of acute asthma is an upper
respiratory tact infection, but other factors may lead to
sudden worsening of symptoms (Table 21-1).
D> History
Obtaining a thorough history may not be possible in an
acute asthma exacerbation. A focused history should be
‘obtained in parallel with initiation of therapy to reverse
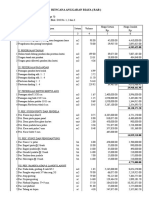
Table 21-1. Acute asthma triggers.
‘ewronmental alergers|
=
‘Gastoesophageal fluc disease
bac sme
‘Dccupatonel exposues
‘nhl initants
‘Stessindued
Envronmental changes (weather)
Ai pollutants
CHAPTER 21
Table 21-2. Risk factors for mortality in asthma.
Chon stead wage
Steanstesofshot acing bet agents per onth
History of intensive cae wit admissions
‘Previous intubations fo asthma
‘Cainguimonary comorbidities
ar uy use
law secineconomic status er imercityresdence
airflow obstruction, regardless of the trigger. Once the
patient has improved and is able to provide more history,
aan attempt should be made to characterize the triggering
event, rapidity of symptom onset, and the severity of the
exacerbation, which will help guide further treatment
and disposition. Characterization of the severity of the
patient’s underlying asthma may help predict mortality
(Table 21-2).
‘Attempting to define the patients underlying long-
‘termasthma control does not aid in the management of an
acute exacerbation, but will be important to understand
when prescribing outpatient therapeutic regimen and
‘follow-up. Patients should be asked about the frequency
and duration oftheir current asthma symptoms and recent
Deta-agonist usage.
Numerous medical conditions can present in a similar
fashion to asthma, including pulmonary embolism (PE),
‘pneumonia, congestive heart failure (CHE), acute myocar-
dial infarction (AMD, or chronic obstructive pulmonary
disease (COPD). The initial history should focus on dif-
ferentiating asthma from other life-threatening causes of
shortness of breath and wheezing.
D> Physical Examination
Patients may present with a wide spectrum of severity,
from an inerease in coughing to obvious respiratory dis-
tress with tachypnea and accessory muscle use. Mental
status should be assessed initially ecause alterations in
consciousness may affect the patient's ability to protect
their airway. A diminished level of consciousness is an
indicator of impending respiratory arrest. The neck
should be palpated for tracheal deviation and crepitus, as
might occur with spontaneous pacumothorex. The lung,
exam is variable and demonstrates prolonged expiration
with wheezing. However, the severity of the airflow
obstruction cannot be gauged by the loudness of the
wheezing. The patient who is audibly wheezing may still
have good air movement on auscultation, whereas the
Auiet sounding chest with little ait movement isa sign of
severe disease because there is not enough airflow to pro-
duce a wheeze. Percussion of the thorax reveals hyper-
resonance due to ait trapping, Evaluation of extremity
cedeme will help differentiate asthma from other causes of
difficulty breathing,
DIAGNOSTIC STUDIES
‘The use of diagnostic studies is limited in the evaluation of |
4 patient with an asthma exacerbation. However, certain
diagnostic modalities may be indicated, depending on the
clinical situation.
p> Laboratory
‘An arterial blood gas (ABG) may demonstrate an increased
CO, level, indicating ventilatory failure and need for
admision to the intensive care nit (ICU). However, the
patients clinical condition is more important than an ABG
to predict outcome or the need for intubation, Electrolytes
and rena function may be helpfili the paint as comor-
bidities that make metabolic derangements more ily. An
levated white blood cll count may ai in the diagnos of
‘concomitant pulmonary infection.
> Imaging
Hyperinflation ofthe lungs is seen in moderate to severe
-exacerbationsand may be reflected on the chest x-ray (CXR)
‘3 an increased anteror-posterior diameter and flattering
‘of the disphragm muscles ACXR should be considered in
patients not responding to treatment, those with fevers
{and those requiring hospitalization or intubation, About
15% ofthese patents have unsuspected pneumonia, CHE
‘pneumothorax, or peumomediastinam.
> Electrocardiogram
‘The electrocardiogram (ECG) is not routinely useful and
ofien demonstrates sinus tachycardia. In severe asthma
‘exacerbations, a right ventricular strain pattern that nor-
malizes with improvement of airflow may be seen,
Dysrhythmias and ischemia may occur in older patients
with coexistent heart disease,
PROCEDURES
> Peak Expiratory Flow Rate
Forced expiratory volume in I second (FEV 1) and peak expi-
ratory flow rate (PEFR) are objective measurements of the
degree of airway obstruction that can be performed at the
bedside (Figures 21-1 and 21-2). These aid the physician
‘monitoring the progression of treatment and determination
‘of patient disposition. Predicted values for FEVI and PEFR.
‘are based on the patients age, sex, and height and compared
‘with a standardized chart or by using the percent of the
patients personal best peak ow. PEFRs <25% predicted
indicate a life-threatening exacerbation and require aggressive
‘management. The severity of asthma can be determined by
the percentage PEFR and categorized as mild (>7096), moder
‘ate (40-G97), or severe (<40%6) and will suide further ther~
‘apy.PEER values at | hour fiom presentation and beyond are
useful to determine nced for hospitalization, Either FEVI ot
PEFR can be used in acite exacerbations,
ASTHMA
Fev meter,
The components of nebulizer treatment include the
mouthpiece, medication reservoir, O, tubing, and “accor
dion’ extension tube. The albuterol is placed within the
reservoir, and the components are fastened together. The
entension tube provides a reservoir of “trapped” O, and
nebulized albuterol that can be inhaled with each breath.
The O, tubing ishooked up to the green wall O, port and.
tured to 6 L/min because the yellow wall pot only deiv-
cs air (21% FiO, . The patient holds the nebulizer during
the treatment (Figuze 21-3). IF the patients unable to hold
thetreatment, «facemask is used instead.
The diagnosis of an asthma exacerbation in the ED is
relatively straightforward. Any patient who has a history
of asthma and presents with wheezing, cough, and dys-
pea likely has asthma as the underlying cause. However,
there are several situations in which wheezing may not be
asthma. Anaphylaxis may present with wheezing, but the
patient will often have urticaria and sometimes gastroin-
testinal symptoms. CHF may present with “cardiac
wheezing,” but the patient will often have “wet” lungs
sounds with rales in the bases, an enlarged heart on CXR,
peripheral edema, and jugular venous distention. CHE
Peak flow meter.
can have many underlying causes, but often these indi-
Viduals will have underlying heart disease and other
comorbidities. The presence of wheezing is common in
COPD, but unless the patient has a history of
a,-antitrypsin deficiency, this type of presentation is
found in patients with smoking history and who are
Handheld nebulizer treatment.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5810)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (843)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (346)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- DokumenterDocument3 pagesDokumenterAinil MaksuraNo ratings yet
- CvzainalDocument10 pagesCvzainalAinil MaksuraNo ratings yet
- PKM Polbung SirkumsisiDocument21 pagesPKM Polbung SirkumsisiAinil MaksuraNo ratings yet
- Transaksi Umum No Nama Program Jenis Pembayaran Nominal Satuan Kuantitas Keterangan Peruntukkan Total Transaksi (IDR)Document1 pageTransaksi Umum No Nama Program Jenis Pembayaran Nominal Satuan Kuantitas Keterangan Peruntukkan Total Transaksi (IDR)Ainil MaksuraNo ratings yet
- Sop PemulanganDocument4 pagesSop PemulanganAinil MaksuraNo ratings yet
- Penyuluhan DM-Ainil MaksuraDocument10 pagesPenyuluhan DM-Ainil MaksuraAinil MaksuraNo ratings yet
- 5 6212769944279450870Document2 pages5 6212769944279450870Ainil MaksuraNo ratings yet
- Soal Simple PhotograhicDocument5 pagesSoal Simple PhotograhicAinil MaksuraNo ratings yet
- 6204bc664dcef30a2cd91244 Alo1644477553187Document1 page6204bc664dcef30a2cd91244 Alo1644477553187Ainil MaksuraNo ratings yet
- 60604f4ba19294096ab2b0e4 Alo1644463706975Document1 page60604f4ba19294096ab2b0e4 Alo1644463706975Ainil MaksuraNo ratings yet
- 611096f29b5d380a4cedea1d Alo1640060971347Document1 page611096f29b5d380a4cedea1d Alo1640060971347Ainil MaksuraNo ratings yet
- Surat Selesai InternshipDocument1 pageSurat Selesai InternshipAinil MaksuraNo ratings yet
- 6110939d9b5d380a45edf64f Alo1628476348703Document1 page6110939d9b5d380a45edf64f Alo1628476348703Ainil MaksuraNo ratings yet
- RAB MarosDocument34 pagesRAB MarosAinil MaksuraNo ratings yet
- PKM JominDocument12 pagesPKM JominAinil MaksuraNo ratings yet
- 60557cd665112f099529e650 Alo1644463717034Document1 page60557cd665112f099529e650 Alo1644463717034Ainil MaksuraNo ratings yet
- Novel Perahu KertasDocument3 pagesNovel Perahu KertasAinil MaksuraNo ratings yet
- DisentriDocument21 pagesDisentriAinil Maksura100% (1)