Professional Documents
Culture Documents
Burns Guidelines Quick Reference Chart PDF
Burns Guidelines Quick Reference Chart PDF
Uploaded by
Lidya NazirOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Burns Guidelines Quick Reference Chart PDF
Burns Guidelines Quick Reference Chart PDF
Uploaded by
Lidya NazirCopyright:
Available Formats
Women’s and Children’s Hospital
Paediatric Burn Guidelines
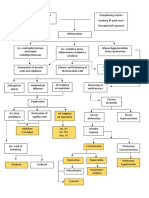
Assessment and treatment of major paediatric burns >10% TBSA
First aid Fluid requirements
First aid >> Stop the burning process. ‘Cool the burn’ with cool tap water for 20 minutes. Do not use ice. Fluid Hartmann’s solution (Parkland Formula) Examples
If cool tap water has not been applied it is still effective up to 3 hours post burn. resuscitation 4mls x % of burn x body weight (kg) 4x40%x12kgs=1920mls
>> Remove clothing, jewellery and anything constricting. = quantity over 24 hours
>> Once cooled, cover burn area with cling wrap and warm the patient. Elevate limbs. Give 50% of the fluid in the first 8 hours 960mls in 8 hours
>> Chemical burns – Wash copiously with water until ‘burning’ sensation settles. Give 50% of the fluid in the next 16 hours 960mls in 16 hours
Primary survey The periods of time are calculated from the time of the burn injury.
Children should have daily maintenance in addition to the fluid resuscitation.
Airway >> Stabilze cervical spine.
Examples
>> Check airway patency.
>> Observe for signs of inhalation injury. 5% Glucose + 0.45% Normal Saline
@ 4mls/kg/Hr for the first 10kg 12kg
Breathing >> Humidified oxygen should be commenced. If breathing is compromised, consider early
endotracheal intubation. 2mls/kg/Hr for between 10–20kg 4mls per kg for the first 10kg = 40mls
1mls/kg/Hr for greater than 20kg 2mls/kg for between 10–20kg = 4mls
Circulation >> Check pulses and blood pressure. Consider IV access.
>> Circumferential deep dermal to full thickness burns may cause a tourniquet effect. Escharotomies 44mls/hour
may be required. Elevate the affected area. Check distal pulses and capillary return and contact Monitor urine >> Burns >15% may require a urethral catheter.
WCH Burns Service. output >> Urine output should be 0.5 to 1ml/kg/hr.
Disability >> Assess conscious state. >> If urine output becomes excessive (>2ml/kg/hr) reduce fluid resuscitation rate.
>> Observe urine colour, if the urine is red or brown consult WCH Burns Service.
Exposure/ >> Estimate percent of total body surface area burned (%TBSA). Monitor temperature,
Environment avoid hypothermia. Secondary survey
Brief history >> Allergies, past medical history, tetanus status, medications and last meal. Other injuries >> Check for any other injuries, i.e. cervical or spinal injuries, loss of consciousness, lacerations etc.
Lund and Browder chart Insert >> Insert nasogastric tube in any patient with burns >15%, or any patient that is unresponsive or any
nasogastric tube patient preparing for air transport.
Area 0–1 1–4 5–9 10–14 15 Adult Superficial Deep Total Analgesia >> Ensure that respiratory rate, sedation and oxygen saturation are monitored during morphine administration.
year year year year year %
>> Initial morphine: Prepare a syringe with 10mg of morphine to a total of 10mls = 1mg/ml.
Head 19 17 13 11 9 7 >> Titrate to comfort in five minutely doses.
Neck 2 2 2 2 2 2 >> <12 months of age call WCH on call Anaesthetist on 8161 7000, pager 3643.
10–20kg use 0.5ml 20–30kg use 1ml 30–40kg use 1.5ml >40kg use 2ml bolus
Ant. trunk 13 13 13 13 13 13
>> When comfortable start morphine infusion at 0.5mg/kg in 50mls normal saline. Run up to 4ml/Hr with
Post. trunk 13 13 13 13 13 13 boluses available every 30 minutes.
R. buttock 2.5 2.5 2.5 2.5 2.5 2.5 Medications >> Tetanus toxoid should be given if patient is not currently covered.
L. buttock 2.5 2.5 2.5 2.5 2.5 2.5 Burn history Obtain:
Genitalia 1 1 1 1 1 1 >> Time of injury.
R. upper arm 4 4 4 4 4 4 >> Mechanism of injury e.g. scald, contact, flame.
>> Location of the event e.g. confined space (risk of inhalation injury).
L. upper arm 4 4 4 4 4 4
>> Any associated injuries.
R. lower arm 3 3 3 3 3 3
Wound care >> Obtain advice from WCH Burns Service.
L. lower arm 3 3 3 3 3 3 >> Wash burns with soapy water, cover with cling wrap.
R. hand 2 2 2 2 2 2 >> Apply White Soft Parafin to the face.
L. hand 2 2 2 2 2 2 Referral criteria
R. thigh 6 7 8.5 9 9.5 10 >> Burns greater than 5–7% Total Body >> Full thickness burns. >> Circumferential burns.
L. thigh 6 7 8.5 9 9.5 10 Surface Area (TBSA). >> Electrical burns >> Burn Injury in patients with
>> Burns to face, hands, feet, genitalia, >> Chemical burns. pre-existing medical disorders.
R. leg 5 5 5.5 6 6.5 7
perineum, major joints. >> Inhalation burns. >> Burns with associated trauma.
L. leg 5 5 5.5 6 6.5 7 >> Suspicious burns.
R. foot 3.5 3.5 3.5 3.5 3.5 3.5
L. foot 3.5 3.5 3.5 3.5 3.5 3.5
For more information Considerable care has been taken to ensure that the information included in these
guidelines is accurate. These guidelines are intended as an aid only and should not
Women’s and Children’s Hospital, Burns Service replace clinical judgment. Any loss or damage incurred as a consequence of using
Total
Telephone: (08) 8161 7000 and page the burns registrar. these guidelines is not the responsibility of the Women’s and Children’s Hospital.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5814)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- 1000 Microbiology MCQs With Key PDFDocument49 pages1000 Microbiology MCQs With Key PDFSaktai Diyami100% (2)
- An Introduction To Genetic Analysis (11th)Document897 pagesAn Introduction To Genetic Analysis (11th)Luigi Ruocco100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Calcium Gluconate Drug StudyDocument1 pageCalcium Gluconate Drug StudyKrissy Java79% (14)
- Home Health Services Coverage and Limitations Handbook - AdoptionDocument104 pagesHome Health Services Coverage and Limitations Handbook - AdoptionRad EkkawiNo ratings yet
- TellmeGen Interpretation ManualDocument22 pagesTellmeGen Interpretation Manualhello goodbyeNo ratings yet
- Admission HospitalDocument7 pagesAdmission HospitalYuhuuNo ratings yet
- Get Rid of Lipomas Naturally With These 3 Home Remedies!Document10 pagesGet Rid of Lipomas Naturally With These 3 Home Remedies!XICMENNo ratings yet
- Copd PathoDocument1 pageCopd PathoRey AngeloNo ratings yet
- ANC and BFDocument29 pagesANC and BFRose Anne Tusi BotinNo ratings yet
- Trends and Changes in PediatricsDocument30 pagesTrends and Changes in PediatricsJaya PrabhaNo ratings yet
- Big Data in Evaluating Drug Efficacy and SafetyDocument28 pagesBig Data in Evaluating Drug Efficacy and SafetyVerena NatasiaNo ratings yet
- GastrotomyDocument23 pagesGastrotomyMr. AlphaNo ratings yet
- Agc332 Exam June 2019Document3 pagesAgc332 Exam June 2019Solomon MbeweNo ratings yet
- PDFsam PsiatriaDocument58 pagesPDFsam PsiatriaEquipo CuatroNo ratings yet
- The Effect of Covid-19 in KabaddiDocument25 pagesThe Effect of Covid-19 in KabaddiShadman RafidNo ratings yet
- GHB FactsDocument1 pageGHB FactsTristan HallmanNo ratings yet
- Medical Terminology and AnatomyDocument16 pagesMedical Terminology and AnatomysureshdassNo ratings yet
- Termpaper DPTDocument80 pagesTermpaper DPTAsha jiluNo ratings yet
- Eff Pleura & PneuDocument77 pagesEff Pleura & PneurianiNo ratings yet
- 366-Article Text-1782-1-10-20230930Document6 pages366-Article Text-1782-1-10-20230930Elang kurniati Elang kurniatiNo ratings yet
- January 2014 (IAL) MS - Unit 1 Edexcel Biology PDFDocument22 pagesJanuary 2014 (IAL) MS - Unit 1 Edexcel Biology PDFsimplesaiedNo ratings yet
- Uses of Tissue Culture Techniques in Plant ProtectionDocument14 pagesUses of Tissue Culture Techniques in Plant Protectionabinaya100% (1)
- The Pomegranate. Fruit of Paradise. Stover. 2007Document5 pagesThe Pomegranate. Fruit of Paradise. Stover. 2007Salma elfaNo ratings yet
- EcgDocument433 pagesEcgihtisham1No ratings yet
- Healthy Smiles Implant Patient Surgery Information and Consent FormDocument3 pagesHealthy Smiles Implant Patient Surgery Information and Consent FormAnup Lal RajbahakNo ratings yet
- BELLO DOCsDocument98 pagesBELLO DOCsPia Loraine BacongNo ratings yet
- CriteriaDocument2 pagesCriteriarh 077No ratings yet
- Tracheostomy: ENT Department DMC & Hospital Ludhiana PunjabDocument46 pagesTracheostomy: ENT Department DMC & Hospital Ludhiana PunjabVikrant MittalNo ratings yet
- Prep Test Odev-1Document13 pagesPrep Test Odev-1Ayşe Hanım ukNo ratings yet
- Prof. Eman Rushdy Sulphonylurea A Golden Therapy For DiabetesDocument51 pagesProf. Eman Rushdy Sulphonylurea A Golden Therapy For Diabetestorr123No ratings yet