Professional Documents
Culture Documents
Pyelonephritis PDF
Pyelonephritis PDF
Uploaded by
Anonymous nd5HDUUNzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pyelonephritis PDF
Pyelonephritis PDF
Uploaded by
Anonymous nd5HDUUNzCopyright:
Available Formats
Article renal
Pyelonephritis
William V. Raszka, Jr,
Objectives After completing this article, readers should be able to:
MD,* Omar Khan, MD†
1. Describe the epidemiology of urinary tract infections and pyelonephritis in children.
2. Discuss the risk factors for the development of pyelonephritis.
Author Disclosure 3. Compare and contrast methods to diagnose urinary tract infection and pyelonephritis
Drs Raszka and Khan in children.
did not disclose any 4. Describe the management of pyelonephritis.
financial relationships 5. Explain the long-term complications of pyelonephritis.
relevant to this
article.
Introduction
The frequency of urinary tract infections (UTIs) is second only to that of respiratory tract
infections in the pediatric population. UTIs often are separated into infections of the lower
urinary tract that involve the bladder and urethra and those of the upper tract that involve
the kidneys, renal pelvis, and ureters. Infections of the upper tract are designated pyelo-
nephritis. A complicated UTI, whether of the upper or lower tract, usually is associated
with an underlying condition that increases the likelihood of a therapeutic failure.
Underlying conditions include abnormal anatomy, urologic dysfunction, the presence of
an indwelling catheter, or isolation of a multiresistant organism.
Epidemiology
Although the prevalence of UTI has been studied in a variety of patient populations, there
are fewer data regarding the prevalence of pyelonephritis due, in part, to the difficulty in
distinguishing upper from lower tract disease. The prevalence of UTI is influenced by
factors such as age, sex, population sample, urine collection method, testing methodolo-
gies, diagnostic criteria, and culture. Age and sex are the most important factors. In
newborns, the prevalence of UTI in preterm infants (2.9%) exceeds that of term infants
(0.7%). UTI is more common in preschool-age children (1% to 3%) than in school-age
children (0.7% to 2.3%). During adolescence, both sexually active girls and homosexual
boys are at increased risk for developing UTI.
Sex has an enormous impact on the prevalence of UTI. In a retrospective population-
based study, the cumulative incidence rate during the first 6 years of life was 6.6% for girls
and 1.8% for boys. In the first 3 postnatal months, UTI is more common in boys and five
to ten times more common in uncircumcised boys than in circumcised boys. Thereafter,
girls are far more likely to develop symptomatic UTI. The prevalence rate of UTI is 1% to
3% in girls 1 to 5 years old and 1% in school-age children. The prevalence rate in school-age
boys is 0.03%.
Although risk factors for the development of pyelonephritis have not been described
well, risk factors for the development of UTI include a previous history of UTI, siblings
who have a history of UTI, female sex (presumably because of the short female urethra), an
indwelling urinary catheter, an intact prepuce in boys, and structural abnormalities of the
kidneys and lower urinary tract. Up to 50% of infants may have an underlying structural or
physiologic abnormality of the urinary tract detected at the time of their first UTI.
Vesicoureteral reflux is the most common and important risk factor for the development of
pyelonephritis.
*Associate Professor of Pediatrics and Director, Infectious Disease Service, Department of Pediatrics, University of Vermont
College of Medicine, Burlington, Vt.
†
Department of Family Medicine, Fletcher Allen Health Care, Burlington, Vt.
364 Pediatrics in Review Vol.26 No.10 October 2005
renal pyelonephritis
Although many Enterobacteriaceae and other organ- icantly greater risk for the development of a bladder
isms may cause UTI in children, Escherichia coli is the infection.
most common pathogen. E coli can be isolated in approx- The most important risk factor for the development of
imately 90% of patients at the time of their initial UTI pyelonephritis in children is vesicoureteral reflux (VUR).
and in more than two thirds of patients who have VUR is detected in approximately 10% to 45% of young
recurrent UTI. Other organisms commonly found in children who have symptomatic UTI. Although there is
patients who have community-acquired UTI include some debate about how reflux damages the renal paren-
Enterobacter, Proteus, and Klebsiella sp. Streptococcus chyma, refluxed infected urine from the bladder increases
agalactiae may cause pyelonephritis in neonates. En- the risk of pyelonephritis and, in young children, renal
terococcus sp may cause up to 5% of UTIs and often is complications such as scarring.
associated with more complex genitourinary tract ab-
normalities. Coagulase-negative staphylococci and Clinical Findings
Lactobacillus sp are rare causes of cystitis or pyelone- The clinical manifestations of pyelonephritis are highly
phritis. variable. Older children may present with fever, chills,
nausea, and flank pain in addition to typical signs of lower
Pathophysiology tract disease such as dysuria, urgency, and increased
In almost all children outside the immediate newborn urinary frequency. Clinical findings include suprapubic
period, pyelonephritis develops after fecal flora colonize and costovertebral (CVA) tenderness. Flank pain, fever,
the urethra and ascend into the bladder and kidneys. The and vomiting occur more commonly in patients who
interval between colonization, infection, and disease is have pyelonephritis than in those who have lower tract
not known. Children can present
with pyelonephritis without pre-
Fever
ceding symptoms typical of lower
tract infection.
Several virulence factors have
been identified in organisms that
and irritability are the most
cause pyelonephritis. A small common presenting findings in infants who
number of E coli O serotypes are
responsible for approximately
have pyelonephritis.
80% of cases of pyelonephritis,
60% of cystitis, and 30% of asymp-
tomatic bacteriuria but are found in only 30% of fecal disease, but these finding are neither specific nor sensitive
flora. The most important virulence factors, particularly for pyelonephritis. As many as 25% of children who have
in patients whose urinary tracts are normal, govern ad- no classic signs or symptoms of pyelonephritis are ulti-
herence or attachment to host mucosal cells. Adhesins, mately confirmed to have upper tract disease; up to 50%
molecules mediating attachment, are on the surfaces of of children who have flank pain have no other evidence of
bacteria or bacterial appendages. Three major adhesins pyelonephritis.
associated with strains of E coli causing UTI are PAP, Fever and irritability are the most common presenting
AFA, and SFA. PAP is the best known and most closely findings in infants who have pyelonephritis. Other find-
associated with pyelonephritis. This molecule is located ings include poor feeding, lethargy, and in toddlers,
on the P pili or fimbriae and recognizes P blood group abdominal pain. Traditionally, pyelonephritis is sus-
determinants found on cells lining the urinary tract. pected in any infant or child who has fever, emesis, flank
Operons that control expression of PAP, AFA, and SFA pain, or CVA tenderness on physical examination and a
molecules are found in most E coli isolated from patients positive urine culture.
who have pyelonephritis.
Host defenses against the development of UTI relate Diagnosis
primarily to anatomic and physiologic considerations. UTI should be considered in any child 2 months to 2
The ability to empty the bladder of urine regularly and years of age or younger who has unexplained fever.
completely is the most important host defense mecha- Approximately 5% to 7% of febrile infants younger than
nism against infection. Patients who do not completely 8 weeks of age have a UTI compared with approximately
empty the bladder, regardless of the reason, are at signif- 5% of febrile children younger than 1 year of age and 2%
Pediatrics in Review Vol.26 No.10 October 2005 365
renal pyelonephritis
Sensitivity and Specificity
Table. icant hematuria, usually is diagnostic of pyelonephritis.
Some laboratories perform an “enhanced urinalysis,”
Ranges for Components of the which involves examining a drop of urine on a hemocy-
Urinalysis in the Diagnosis of tometer. The presence of more than 10 white blood cells
suggests a UTI.
Urinary Tract Infection Many gram-negative organisms reduce nitrates to ni-
Sensitivity Specificity trites in the urine. A positive nitrite test is an insensitive
(%) (%) but relatively specific test for UTI (Table). The presence
Test (range) (range) of bacteria in a spun urine sample is neither specific nor
Leukocyte esterase 70 to 95 65 to 90 sensitive enough to use clinically. Although laboratories
White blood cells on 30 to 100 45 to 100 rarely perform routine Gram stains on urine, a positive
microscopy Gram stain result on an unspun urine specimen is diag-
Nitrite 15 to 80 90 to 100 nostic of UTI.
Bacteria on microscopy 15 to 100 10 to 100 Many children who have radiographically confirmed
pyelonephritis have elevated peripheral white blood cell
counts or nonspecific markers of inflammation such as an
increased erythrocyte sedimentation rate or C-reactive
of all febrile children younger than 5 years of age. Pa- protein value, but these laboratory tests are neither sen-
tients usually are diagnosed following examination of sitive nor specific enough to confirm or exclude pyelone-
their urine. The purpose of the urinalysis is to identify phritis.
those children at greater or lesser risk of having a UTI. The diagnosis of UTI is confirmed by the growth of a
Culture of an appropriately obtained urine specimen is significant number of bacteria in a properly obtained
the laboratory test that establishes or excludes the pres- urine specimen. Based on studies of healthy women more
ence of UTI. than 50 years ago, growth of more than 105 organisms/
Urine can be collected by bag technique, mid-stream mL of voided midstream urine is indicative of UTI.
clean catch, urethral catheterization, or suprapubic aspi- Specimens that grow fewer than 104 organisms are un-
ration. Although many physicians continue to rely on likely to represent UTI. In the appropriate clinical set-
bagged urine specimens, UTI should not be diagnosed ting, growth of 104 and 105 organisms may represent
by a bagged specimen because of its low specificity and UTI. Any growth of gram-negative bacteria in urine
poor positive predictive value. A negative culture from an obtained by suprapubic aspiration indicates a UTI. For
appropriately obtained bagged specimen, however, may children in whom urine is obtained by transurethral
be useful in some situations to exclude UTI. For a child 2 catheterization, some have proposed that more than
months to 2 years of age, urine for culture should be 50,000 colonies/mL of urine be used as the criterion for
obtained by suprapubic aspiration or transurethral cath- diagnosing the infection. Urine cultures do not distin-
eterization. Both of these methods are simple and easy to guish between lower and upper urinary tract infection
perform and give reliable results. In older children, mid- Approximately 10% to 20% of adult women who have
stream clean catch of spontaneously voided urine after pyelonephritis have concomitant bacteremia. In chil-
appropriate cleansing of the urinary meatus is acceptable. dren, the prevalence of bacteremia in patients younger
A clean urine specimen can be used to assess for than 2 months of age diagnosed as having a UTI is 22.7%
evidence of inflammation or bacteria. The leukocyte and in patients between the ages of 2 months and 36
esterase test identifies an enzyme produced by white months of age is 3.0%. Infants and children whose urine
blood cells. A positive leukocyte esterase test usually and blood cultures are positive are assumed to have
corresponds to at least 5 white blood cells per high- pyelonephritis.
power field, with a sensitivity of 70% to 95% (Table). Imaging studies are needed infrequently to confirm a
Direct visualization of the unspun urine gives informa- diagnosis of pyelonephritis. Computed tomography
tion about the number and characteristics of white blood scans are more sensitive than ultrasonography at detect-
cells. More than 5 white blood cells per high-power field ing changes consistent with pyelonephritis, but they
represents pyuria. Similar to the leukocyte esterase test, require the use of intravenous contrast. DMSA renal
the presence of white blood cells in the urine is a sensitive scintography is the imaging study of choice to confirm or
but nonspecific test for UTI. The exception is the finding exclude the diagnosis of pyelonephritis as well as to
of white blood cell casts, which, in the absence of signif- detect renal scarring. Its routine use, however, is limited
366 Pediatrics in Review Vol.26 No.10 October 2005
renal pyelonephritis
to situations such as the challenging patient who has a antibiotics had no advantage over oral antibiotics regard-
neurogenic bladder or significant genitourinary abnor- ing time to defervescence, renal scarring, duration of
malities. hospitalization, and time to urine sterilization.
Many oral agents can be used for the empiric therapy
Treatment of pyelonephritis in patients well enough to take oral
Various antimicrobial agents are useful for the treatment medications. Amoxicillin, however, is no longer an ac-
of UTI. Antimicrobial selection and route of administra- ceptable choice because approximately 40% of E coli
tion are guided by local microbial resistance patterns and strains elaborate a penicillinase. TMP-SMX has been a
the ability of the patient to take and retain oral agents. standard first-line oral agent for some time and may be
Many commonly used antibiotics are concentrated in the more effective than beta-lactams at treating UTIs. How-
urine and are useful in treating lower tract disease. Renal ever, E coli resistance to TMP-SMX is becoming more
parenchymal antibiotic levels, however, more closely re- common. TMP-SMX should not be used for empiric
semble bloodstream levels. The consequence is that ni- therapy of pyelonephritis if local resistance to the drug
trofurantoin, which achieves negligible levels in the in E coli exceeds 10% to 20%. Alternatives to TMP-
blood but is concentrated in the urine, is a good drug for SMX include first-, second-, and third-generation oral
the treatment or prophylaxis of lower UTI but not for cephalosporins, penicillin/beta-lactamase inhibitor
pyelonephritis. combinations, and for the child older than 12 months of
Children who are suspected of having pyelonephritis age, ciprofloxacin. Because of concerns about adverse
are started empirically on antibiotics effective against the effects of ciprofloxacin in young children, when it ap-
usual pathogens for their clinical condition. Children pears to be the best drug, the potential benefits and
problems associated with it
should be discussed with the par-
For
ents.
For patients who have a con-
patients who have a confirmed UTI, firmed UTI, antimicrobial suscep-
tibility testing results should
antimicrobial susceptibility testing results guide therapy. Whenever possi-
should guide therapy. ble, amoxicillin or TMP-SMX
should be used. Although few
randomized trials comparing
treatment regimens for pyelone-
deemed toxic or ill enough to require hospitalization phritis in children have been performed, the available
usually are started on intravenous antibiotics. Ampicillin evidence suggests that 10 to 14 days of antimicrobial
and gentamicin have been used empirically for decades to therapy is adequate for uncomplicated pyelonephritis.
treat pyelonephritis. Gentamicin is effective against most After completion of 10 to 14 days of antibiotics for their
aerobic gram-negative bacilli; ampicillin is the drug of initial UTI, children ages 2 months to 2 years should be
choice for enterococci. Alternatives to this regimen in- continued on prophylactic antibiotics until imaging
clude most first-, second-, or third-generation cephalo- studies are completed and VUR is excluded.
sporins, trimethoprim-sulfamethoxazole (TMP-SMX), Follow-up urine culture after 24 hours of therapy is
and penicillin/beta-lactamase inhibitor combination not indicated because it rarely is positive. Almost 90% of
drugs. Parenteral antibiotics most often are continued infants who have febrile UTIs and presumed pyelone-
until the patient is afebrile for 24 hours. phritis were afebrile within 48 hours of initiation of
For children who are presumed to have pyelonephritis antibiotics. Those who remained febrile for more than
and who appear ill or are vomiting but are not ill enough 48 hours did not have any different laboratory or clinical
to require hospitalization, an intramuscular dose of findings from those who became afebrile in fewer than
ceftriaxone or gentamicin can be administered followed 48 hours. Most important, there was not a higher rate of
by oral antibiotics. For children older than 1 month of complications in those who failed to respond in 48 hours.
age who are suspected of having pyelonephritis, do not However, many clinicians re-evaluate children who have
appear toxic, and can take oral agents, oral antimicrobial not become afebrile within 48 hours with another urine
agents can be started. At least one study has shown that culture or an imaging study, looking for evidence of
in children older than 2 months of age, intravenous urinary tract obstruction.
Pediatrics in Review Vol.26 No.10 October 2005 367
renal pyelonephritis
ferred choice for all boys of any age at the time of their
first UTI. Radionuclide cystography often is performed
in girls and for follow-up VCUGs.
Unfortunately, it is uncertain whether the identifica-
tion and treatment of children who have primary VUR
confer clinically important benefits. In randomized, con-
trolled trials, no treatment or treatment of VUR with
long-term antibiotics, surgery, or a combination of anti-
biotic prophylaxis and surgery seemed to have similar
results. Natural history studies suggest that long-term
medical management is as effective as surgical therapy for
those who have primary VUR. Currently, children who
have VUR are placed on long-term prophylactic antibi-
otics such as daily nitrofurantoin, trimethoprim, or
TMP-SMX. Children who have VUR and recurrent UTI
with progressive renal damage despite prophylactic anti-
biotics or those who have severe reflux often are consid-
ered for surgical correction of the VUR.
Complications
Patients who have pyelonephritis may develop bactere-
mia. The likelihood of developing bacteremia depends
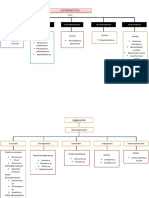
Figure. Fluoroscopic VCUG showing grade III reflux.
on the age of the child. Children younger than 2 months
of age are the most likely to have bacteremia at the time
Prevention of presentation. No laboratory test or physical findings
The goal of medical management of patients who have can distinguish between patients who have bacteremia
pyelonephritis not only is to eradicate the infection but to and those who do not. Children who have bacteremia
identify those patients at risk for subsequent infection have similar clinical courses as those who do not, whether
and renal scarring. The American Academy of Pediatrics treated with oral or intravenous antibiotics.
(AAP) recommends that children younger than age 2 Long-term complications of pyelonephritis include
years diagnosed with their first UTI be evaluated for recurrence, renal scarring, and hypertension. Approxi-
evidence of urologic abnormalities. Many clinicians also mately 18% of boys who have a UTI before age 1 year
evaluate older children who have febrile UTIs or pyelo- develop recurrent infections compared with 32% when
nephritis. Although one study suggested that the results the initial infection happened after the first postnatal
of ultrasonography had no impact on the management of year. Most recurrences occur within the first year of
a select group of children who had an initial UTI, the infection. Similar to boys, girls who have their first UTI
AAP recommends that renal ultrasonography be used to at a later age have a higher recurrence rate than those
define the anatomy of the urinary tract because the test is diagnosed in the first year (40% versus 26%). Each prior
noninvasive, involves no radiation, and can define renal infection increases the risk of a recurrence by as much as
anatomy readily (eg, obstruction, major scarring, cysts, 25%.
or renal dysplasia). Children who have pyelonephritis may develop renal
Children who have UTI diagnosed in the first 2 years scarring. For most children who have UTI in whom renal
after birth should be evaluated with voiding cystoure- scars are found, the scars are visible on the first set of
thrography (VCUG). Both fluoroscopic or contrast imaging studies. These original scars remain unchanged
VCUG and radionuclide cystography are good at detect- irrespective of the child’s future clinical course. Infants
ing reflux and duplicated systems. Fluoroscopic VCUG and young children are more prone to scarring than are
can provide enough information to grade reflux (Figure) children older than age 5 years and adults, although the
according to an international scale that calculates the reason is unclear. Children treated for UTI who have
height of the reflux and the associated anatomic changes evidence of VUR are significantly more likely to develop
to the kidney and identifies bladder and urethral abnor- scars than are children who do not have VUR. Almost all
malities better than radionuclide studies. It is the pre- new scars in children who have VUR occur before the age
368 Pediatrics in Review Vol.26 No.10 October 2005
renal pyelonephritis
of 6 years and almost always in association with new Chon CH, Lai FC, Shortliffe LM. Pediatric urinary tract infections.
UTIs. More severe reflux is associated with a greater risk Pediatr Clin North Am. 2001;48:1441–1459
Edelmann CM Jr, Ogwo JE, Fine BP, Martinez AB. The prevalence
of scarring. A long-term follow-up study of children who
of bacteriuria in full-term and premature newborn infants. J Pe-
had grade III or IV reflux managed either medically or diatr. 1973;82:125–132
surgically found that the incidence of new scar formation Herr SM, Wald ER, Pitetti RD, Choi SS. Enhanced urinalysis
over a 5-year period was 20% in children younger than improves identification of febrile infants ages 60 days and
age 2 years, 10% in children between 2 and 4 years, and younger at low risk for serious bacterial illness. Pediatrics. 2001;
108:866 – 871
5% in children older than age 4 years at the time of
Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH,
enrollment. Only two children developed new scars more Wald ER. Imaging studies after a first febrile urinary tract
than 5 years after enrollment. infection in young children. N Engl J Med. 2003;348:195–202
Early detection of pyelonephritis is critical to preser- Keren R, Chan E. A meta-analysis of randomized, controlled trials
vation of renal function. In a recent study of United comparing short- and long-course antibiotic therapy for urinary
tract infections in children. Pediatrics. 2002;109:e70. Available
States children who were identified as having UTI early
at: http://pediatrics.aappublications.org/cgi/content/full/
in life, only one child had renal scarring on entry. Other 109/5/e70
United States investigators also have found a low inci- Kraus SJ. Genitourinary imaging in children. Pediatr Clin North
dence of renal scarring in children who had presumed Am. 2001;48:1381–1424
pyelonephritis identified early in life. This contrasts with Le Bouguenec C, Lalioui L, du Merle L, et al. Characterization of
AfaE adhesins produced by extraintestinal and intestinal human
older studies, which demonstrated a high incidence of
Escherichia coli isolates: PCR assays for detection of Afa adhesins
scarring. that do or do not recognize Dr blood group antigens. J Clin
Long-term follow-up studies have linked renal scar- Microbiol. 2001;39:1738 –1745
ring with hypertension, decreased glomerular filtration, Olbing H, Smellie JM, Jodal U, Lax H. New renal scars in children
and end-stage renal disease. Unfortunately, the exact with severe VUR: a 10-year study of randomized treatment.
Pediatr Nephrol. 2003;11:1128 –1131
mechanism of risk of eventually developing hypertension
Pitetti RD, Choi S. Utility of blood cultures in febrile children with
by patients who have scars is not known. Moreover, it is UTI. Am J Emerg Med. 2002;20:271–274
unclear why some children who have extensive scars Ronald A. The etiology of urinary tract infection: traditional and
never develop hypertension. Currently, the best evidence emerging pathogens. Am J Med. 2002;113(suppl 1A):14S–19S
suggests that children who have pyelonephritis and renal Wheeler DM, Vimalachandra D, Hodson EM, Roy LP, Smith GH,
Craig JC. Interventions for primary vesicoureteric reflux.
scarring be followed carefully over time.
Cochrane Database Syst Rev. 2004:CD001532
Wiswell T. The prepuce, urinary tract infections, and the conse-
Conclusion quences. Pediatrics. 2000;105:860 – 862
Pyelonephritis in the pediatric patient is a serious illness.
Although some aspects of the management of this disease
are still open to debate, there is broad agreement that Multimedia Links
AAP Guidelines on the diagnosis, treatment, and evaluation of the
prompt recognition and treatment are essential to pre-
initial urinary tract infection in febrile infants and young chil-
vent long-term sequelae. dren. Available at: http://www.aap.org/policy/ac9830.htm
The NIH/NIDDK Web site on pyelonephritis. Available at: http://
www.niddk.nih.gov/health/kidney/summary/pyelonep/
Suggested Reading pyelonep.htm
American Academy of Pediatrics. Committee on Quality Improve- MEDLINEplus medical encyclopedia on pyelonephritis. Available
ment. Subcommittee on Urinary Tract Infection. Practice pa- at: http://www.nlm.nih.gov/medlineplus/ency/article/000522.
rameter: the diagnosis, treatment, and evaluation of the initial htm
urinary tract infection in febrile infants and young children. The Atlas of Renal Pathology. Available at: http://ajkd.
Pediatrics. 1999;103:843– 852 wbsaunders.com/atlas/35/2/atlas35_2.htm
Pediatrics in Review Vol.26 No.10 October 2005 369
renal pyelonephritis
PIR Quiz
Quiz also available online at www.pedsinreview.org.
9. Which of the following findings or conditions increases the risk of developing a urinary tract infection
(UTI)?
A. Acidification of the urine.
B. Dilution of the urine.
C. High specific gravity.
D. Incomplete bladder emptying.
E. Large bladder capacity.
10. An 18-month-old boy presents with fever for 3 days. Urine is obtained by catheterization. Which of the
following findings in the urine confirms the diagnosis of UTI?
A. Positive Gram stain of unspun urine.
B. Positive leukocyte esterase test.
C. Positive nitrite test.
D. Presence of bacteria in spun urine.
E. Presence of 10 white blood cells in unspun urine.
11. A 15-month-old girl who has recurrent UTIs presents with fever and irritability. Analysis of her urine
shows more than 50 white blood cells per high-power field. Which of the following oral medications is
least likely to be effective for the empiric treatment of her presumed UTI?
A. Amoxicillin.
B. Cefuroxime.
C. Cephalexin.
D. Ciprofloxacin.
E. Trimethoprim-sulfamethoxazole.
12. A 20-month-old patient is diagnosed as having her first UTI. After 24 hours of antibiotics, she is afebrile.
Renal ultrasonography findings are normal. Which of the following tests should be performed on this girl?
A. DMSA renal scintography.
B. Immediate repeat urine culture.
C. Intravenous pyelography.
D. Repeat renal ultrasonography in 6 weeks.
E. Voiding cystourethrography.
370 Pediatrics in Review Vol.26 No.10 October 2005
You might also like
- Gemstones ManualDocument44 pagesGemstones ManualMickShazan100% (4)
- Abdominal Pain During PregnancyDocument58 pagesAbdominal Pain During PregnancyLuminita OpranNo ratings yet
- 1993 92 723 Larry J. Baraff: Capillary Refill: Is It A Useful Clinical Sign?Document4 pages1993 92 723 Larry J. Baraff: Capillary Refill: Is It A Useful Clinical Sign?Citty'Q' HuwalidNo ratings yet
- Aortic Valve StenosisDocument4 pagesAortic Valve StenosisYrag NoznipNo ratings yet
- Kernicterus, (Bilirubin Encephalopathy) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandKernicterus, (Bilirubin Encephalopathy) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- NR March2014Document44 pagesNR March2014Susana Jacqueline Echeverria Muñoz100% (1)
- Final Exam-Law On Obligations and ContractsDocument6 pagesFinal Exam-Law On Obligations and ContractsKat Miranda78% (9)
- Approach To Febrile ChildDocument52 pagesApproach To Febrile ChildwoldemariamNo ratings yet
- Treatment of Acute PharyngitisDocument4 pagesTreatment of Acute PharyngitisZafira Ananda RaishaNo ratings yet
- How Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Document14 pagesHow Do I Diagnose The Cause of A Cough of Less Than 3 Weeks' Duration?Sudhir TyagiNo ratings yet
- Peripheral Artery DiseaseDocument8 pagesPeripheral Artery DiseasemainehoonaNo ratings yet
- Preventive Pediatrics Part 3Document5 pagesPreventive Pediatrics Part 3mkct111No ratings yet
- Headway Test Unit 5ADocument3 pagesHeadway Test Unit 5Akaro2511personalNo ratings yet
- Class Modifier Module For 5eDocument16 pagesClass Modifier Module For 5eAnita BotosNo ratings yet
- Heart FailureDocument11 pagesHeart FailureYusnida RahmawatiNo ratings yet
- Atopic Dermatitis: Education GapDocument16 pagesAtopic Dermatitis: Education GapAncuta CalimentNo ratings yet
- Lineage Holder of LiuhebafaDocument5 pagesLineage Holder of Liuhebafaapi-381186363% (8)
- Importance of Prenatal Check Ups and The Tests They Need To Undergo Before BirthDocument56 pagesImportance of Prenatal Check Ups and The Tests They Need To Undergo Before BirthAl YsSa Ricafort MillabasNo ratings yet
- Urinary Tract Infection in Children - Classification, Diagnosis and TreatmentFrom EverandUrinary Tract Infection in Children - Classification, Diagnosis and TreatmentNo ratings yet
- CPG Pcap 2012 PDFDocument54 pagesCPG Pcap 2012 PDFroshmae67% (3)
- Case 9: 2-Week-Old With Lethargy - CrimsonDocument7 pagesCase 9: 2-Week-Old With Lethargy - Crimsonalwaysbeclosing52No ratings yet
- Case Study: Chapter 10 Pediatric DisordersDocument6 pagesCase Study: Chapter 10 Pediatric DisordersRica AvendañoNo ratings yet
- Chapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingDocument3 pagesChapter II - Anemia and Hypovolemic Shock Secondary To An Upper Gastrointestinal BleedingKn VelasquezNo ratings yet
- Ven. Mahasi Sayadaw - A Discourse On VipassanaDocument28 pagesVen. Mahasi Sayadaw - A Discourse On VipassanaiguanamusNo ratings yet
- Chapter Vi Multidisciplinary and Sectoral Collaboration Lesson 1Document13 pagesChapter Vi Multidisciplinary and Sectoral Collaboration Lesson 1Sophia Kaye Aguinaldo100% (1)
- Nursing Care The Mechanical VentilatedDocument11 pagesNursing Care The Mechanical VentilatedIchal faisNo ratings yet
- Pyelonephritis: Urinary Tract Infection Vesicoureteric RefluxDocument12 pagesPyelonephritis: Urinary Tract Infection Vesicoureteric Reflux3ling3No ratings yet
- PyelonephritisDocument7 pagesPyelonephritisKokila AbelNo ratings yet
- Inflamatory Bowel Disease: Dr. Samir IsmailDocument82 pagesInflamatory Bowel Disease: Dr. Samir IsmailGhadeer EbraheemNo ratings yet
- 2.11 SEPTIC ABORTION AND SEPTIC SHOCK. M. Botes PDFDocument4 pages2.11 SEPTIC ABORTION AND SEPTIC SHOCK. M. Botes PDFteteh_thikeuNo ratings yet
- Agis Mira Dewi, S.kedDocument35 pagesAgis Mira Dewi, S.kedAgiish EMdeNo ratings yet
- Obstetric HistoryDocument38 pagesObstetric HistoryHannah LeianNo ratings yet
- 1 Typhoid FeverDocument14 pages1 Typhoid FeverWildan YogaNo ratings yet
- Abdominal Mass Differential PresentationDocument42 pagesAbdominal Mass Differential Presentationdeb haartNo ratings yet
- Bronchiolitis Clinical Practice GuidelineDocument21 pagesBronchiolitis Clinical Practice GuidelineJuwita PratiwiNo ratings yet
- HPV Case StudyDocument2 pagesHPV Case StudyEileen Aquino MacapagalNo ratings yet
- Tubo Ovarian AbscessesDocument8 pagesTubo Ovarian AbscessesHanif Prasetyo KusumoNo ratings yet
- Benign Febril Convulsion PDFDocument18 pagesBenign Febril Convulsion PDFAESTHETIC PHOTONo ratings yet
- IM Clinics History 2Document4 pagesIM Clinics History 2LucyellowOttemoesoeNo ratings yet
- PyelonephritisDocument17 pagesPyelonephritisapi-339668544100% (1)
- What Are Febrile Convulsions?Document16 pagesWhat Are Febrile Convulsions?Redgina CalimlimNo ratings yet
- PERITONITISDocument27 pagesPERITONITISTiffany Adrias100% (1)
- Newborn Screening Summary 2010Document42 pagesNewborn Screening Summary 2010Ana Cristina Montillano100% (3)
- Session13 - Endometrial CaDocument27 pagesSession13 - Endometrial CaCHALIE MEQUNo ratings yet
- Necrotizing Enterocolitis ProtocolDocument3 pagesNecrotizing Enterocolitis Protocoleddy riachyNo ratings yet
- Renal Concept MapDocument8 pagesRenal Concept MapXtine CajiNo ratings yet
- Endometriosis: Li Qi LingDocument67 pagesEndometriosis: Li Qi LingwaheedaNo ratings yet
- Clinical Practice Guideline For CataractDocument27 pagesClinical Practice Guideline For CataractNaufal FarisatriantoNo ratings yet
- Iron Deficiency Anemia Among Pregnant Women in Nablus District Prevalence Knowledge Attitude and Practices PDFDocument72 pagesIron Deficiency Anemia Among Pregnant Women in Nablus District Prevalence Knowledge Attitude and Practices PDFEArl CopinaNo ratings yet
- Reye SyndromeDocument10 pagesReye SyndromeDanil KhairulNo ratings yet
- Headache in PregnancyDocument34 pagesHeadache in PregnancybagusNo ratings yet
- Current Medical Treatment On BPHDocument33 pagesCurrent Medical Treatment On BPHDeviruchi GamingNo ratings yet
- Pediatrics MALNUTRITION - Dra. Garcia's Lecture: Primum Non NocereDocument8 pagesPediatrics MALNUTRITION - Dra. Garcia's Lecture: Primum Non NocerekrishNo ratings yet
- Normal Vaginal Delivery After One Lower Segment Caesarean Section Can Be Safe Option For Many Women But Not Right Choice For AllDocument6 pagesNormal Vaginal Delivery After One Lower Segment Caesarean Section Can Be Safe Option For Many Women But Not Right Choice For AllRussel Cauton de JesusNo ratings yet
- Creamer Et Al-2016-British Journal of DermatologyDocument34 pagesCreamer Et Al-2016-British Journal of DermatologyAtika Indah SariNo ratings yet
- Acute Poststreptococcal Glomerulonephritis An UpdateDocument6 pagesAcute Poststreptococcal Glomerulonephritis An UpdateJuan Antonio Herrera LealNo ratings yet
- Kenya ARV Guidelines 2018Document230 pagesKenya ARV Guidelines 2018Felix Wafula MusibiNo ratings yet
- VP Shunt UrgencyDocument7 pagesVP Shunt UrgencyAollia GoodmaanNo ratings yet
- Guidelines GonoDocument6 pagesGuidelines GonoFen NavarreteNo ratings yet
- Φ PathophysiologyDocument4 pagesΦ PathophysiologyMariah AshooriyanNo ratings yet
- CPC-Patho Version 6Document20 pagesCPC-Patho Version 6Bea SamonteNo ratings yet
- History Taking PediatricDocument27 pagesHistory Taking PediatricIvan DanusaputraNo ratings yet
- Session12-Uterine LeiomyomasDocument26 pagesSession12-Uterine LeiomyomasCHALIE MEQUNo ratings yet
- The Normal Anthropometric Measurements For HealthyDocument43 pagesThe Normal Anthropometric Measurements For HealthyAli Mohamed BurhanNo ratings yet
- A Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutFrom EverandA Study of the Lack of Hiv/Aids Awareness Among African American Women: a Leadership Perspective: Awareness That All Cultures Should Know AboutRating: 5 out of 5 stars5/5 (1)
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- What Is Research: DefinitionDocument4 pagesWhat Is Research: DefinitionAfif Al FatihNo ratings yet
- Daftar PustakaDocument16 pagesDaftar PustakaAfif Al FatihNo ratings yet
- YeaaaahDocument1 pageYeaaaahAfif Al FatihNo ratings yet
- Yeaaaah 23456789Document1 pageYeaaaah 23456789Afif Al FatihNo ratings yet
- Immunodeficiency: Principles of ImmunologyDocument16 pagesImmunodeficiency: Principles of ImmunologyAfif Al FatihNo ratings yet
- Activities and IntentsDocument47 pagesActivities and IntentsAfif Al FatihNo ratings yet
- Clinical EndocrinologyDocument52 pagesClinical EndocrinologyAfif Al FatihNo ratings yet
- Absen Cwek PaiDocument2 pagesAbsen Cwek PaiAfif Al FatihNo ratings yet
- Nelson Mandela Long Walk To Freedom MCQs Class 10 English Chapter 2Document17 pagesNelson Mandela Long Walk To Freedom MCQs Class 10 English Chapter 2kausalyaparida22No ratings yet
- Huling Hiling Ni Hermano HusengDocument3 pagesHuling Hiling Ni Hermano HusengEzekiel VilaNo ratings yet
- S 17 RBZDocument0 pagesS 17 RBZMike WrightNo ratings yet
- Feminism and A Female Trinity in Denise Boucher S Les F Es Ont SoifDocument10 pagesFeminism and A Female Trinity in Denise Boucher S Les F Es Ont SoifBridget LeonardNo ratings yet
- Pengaruh Pemberian Ischemic Compression Dan Contract Relax Stretching Terhadap Intensitas Nyeri Myofascial Trigger Point Syndrome Ototupper TrapeziusDocument9 pagesPengaruh Pemberian Ischemic Compression Dan Contract Relax Stretching Terhadap Intensitas Nyeri Myofascial Trigger Point Syndrome Ototupper TrapeziusDian DianaNo ratings yet
- MAD Art of Caricatures by Tom Richmond Do WordDocument192 pagesMAD Art of Caricatures by Tom Richmond Do WordJjaz Animações ZíporaNo ratings yet
- Competency Assessment Results Summary: Form A/C24/0108Document2 pagesCompetency Assessment Results Summary: Form A/C24/0108Ict GothongNo ratings yet
- Dok For SocialstudiesDocument4 pagesDok For Socialstudiesapi-242128584No ratings yet
- Problems of Interpretation in TheDocument18 pagesProblems of Interpretation in TheAnonymous lVC1HGpHP3No ratings yet
- SBP 05Document306 pagesSBP 05Galih FidiantoNo ratings yet
- Mastering Conversation British English StudentDocument4 pagesMastering Conversation British English StudentDariiaNo ratings yet
- Asistio Vs AguirreDocument11 pagesAsistio Vs AguirreDaley CatugdaNo ratings yet
- Chytidiomycoya: Blastocladiales Neocallimasticales Monoblepbaridales Chytridiales SpizellomycetalesDocument7 pagesChytidiomycoya: Blastocladiales Neocallimasticales Monoblepbaridales Chytridiales Spizellomycetalesratih purwaningrum13No ratings yet
- Your English Pal ESL Lesson Plan Music Student v4 ExteDocument4 pagesYour English Pal ESL Lesson Plan Music Student v4 ExteAdriana RoberttiNo ratings yet
- Quran General Knowledge PART 1Document4 pagesQuran General Knowledge PART 1maniNo ratings yet
- EE101 - Quiz #1Document16 pagesEE101 - Quiz #1Rick AlvientoNo ratings yet
- Factors of Causes of Deviation in TafsirDocument14 pagesFactors of Causes of Deviation in Tafsirfatkhul mubinNo ratings yet
- Ayers: 1. Humphrey Eyre/HeyerDocument10 pagesAyers: 1. Humphrey Eyre/HeyerJeff MartinNo ratings yet
- Moving Into Apartment Bed BugsDocument2 pagesMoving Into Apartment Bed Bugsstovedebtor26No ratings yet
- Govind Sharma 2Document85 pagesGovind Sharma 2Daefnate KhanNo ratings yet
- Digital Death (Missing Bits)Document48 pagesDigital Death (Missing Bits)Stacey Pitsillides100% (1)
- Multiple SclerosisDocument14 pagesMultiple SclerosisMioara HorbaniucNo ratings yet
- Portfolio Adv11Document4 pagesPortfolio Adv11Johana GarciaNo ratings yet