Professional Documents
Culture Documents
1692-Article Text-4776-1-10-20180308 PDF
Uploaded by
irene aureliaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1692-Article Text-4776-1-10-20180308 PDF
Uploaded by
irene aureliaCopyright:
Available Formats
Paediatrica Indonesiana
p-ISSN 0030-9311; e-ISSN 2338-476X; Vol.58, No.1(2018). p. 53-8; doi: http://dx.doi.org/10.14238/pi58.1.2018.53-8
Original Article
Prescribing antibiotics to pediatric dengue patients:
increasing risk of bacterial resistance
Dhanunjaya Sandopa1, Sree Keerthi Nethi1, Sai Charitha Sreeram1,
Narasimha Kumar Godlaveti Vijay2, Vyshnavi Biradavolu1, Jagadeesh Vijay Kakimani1
I
Abstract n the field of medicine, the battle between
Background Use of antibiotics to treat self-limiting viral infections bacteria and mankind can be explained in three
like dengue fever (DF) without any co-morbid conditions in pediat- phases: the pre-antibiotic era, the antibiotic
ric patients is common practice in India, and a major contribution
of the inappropriate use of antibiotics in the country. era, and the post-antibiotic era. The period
Objective To provide an analysis of diagnosis, grading, and prescrib- before the introduction of sulfa drugs and penicillin
ing of antibiotics in pediatric inpatients with DF in a tertiary care is considered to be the ‘pre-antibiotic era’. Bacteria
teaching hospital in India.
Methods Data from case sheets of all pediatric inpatients (n=370)
dominated mankind and bacterial infections were
diagnosed with DF without co-morbid conditions were collected the leading cause of death.1 Discovery of penicillin
with regards to diagnosis, grading, presence, and appropriateness by Sir Alexander Fleming in 1928 laid the foundation
of antibiotic usage according to the 2009 WHO Guidelines, the and hope of controlling bacterial infections. Since
National Vector Borne Disease Control Program (NVBDCP) of India
Guidelines, and the Hospital Infection Society (HIS) Guidelines. that time, the ‘antibiotic era’ has seen the discovery
Results Platelet count determination (50% of the cases) was the of many antibiotics, which has transformed modern
major diagnostic method for dengue. Inappropriate grading of DF medicine and saved millions of lives. 2 These
was seen in 20% of patients. Almost 75% of the 370 dengue cases
were prescribed antibiotics for the expressed purpose of avoiding
discoveries gave hope that mankind would rein over
hospital-acquired infections. A single antibiotic was given in 225 bacterial infections forever. However, the foremost
prescriptions (60.81%), 2 antibiotics in 33 (8.91 %) cases, and 3 driving force for discovering newer antibiotics was the
antibiotics in 9 (2.43%) cases. development of resistance to the existing antibiotics.
Conclusions Prescribing one or more antibiotics to treat self-
limiting viral infections is considered as inappropriate and may lead Eventually, the antibiotic pipeline began to dry
to the development of multidrug resistance. Furthermore, excess use up, because the pharmaceutical industry considers
of antibiotics in infancy may induce imbalances in gut and micro-
biota, called dysbiosis, and increases the probability of occurrence
of diseases such as obesity, diabetes, and asthma in later life. These
findings can inform the development of antibiotic stewardship in
the treatment of dengue. [Paediatr Indones. 2018;58:53-8; doi: From the Department of Clinical Pharmacology, Sri Padmavathi School
http://dx.doi.org/10.14238/pi58.1.2018.53-8]. of Pharmacy, Tirupathi, Andhrapradesh 1, and the Department of
Pharmacology, Siddha Central Research Institute, Chennai, Tamilnadu2,
India.
Keywords: antibiotics; bacterial resistance;
dengue; inappropriate use Reprint requests to: Mr. Dhanunjaya Sandopa, Assistant Professor,
Department of Clinical Pharmacology, Sri Padmavathi School of Pharmacy,
Tirupathi, Andhrapradesh, India 517503. Tel. +91-9177392747; Fax.
0877 – 2237732; Email: dhanuspsp@gmail.com.
Paediatr Indones, Vol. 58, No. 1, January 2018 • 53
Dhanunjaya Sandopa1 et al.: Prescribing antibiotics to pediatric dengue: increasing risk of bacterial resistance
investment in antibiotic study to be unprofitable, is increasing the condition of resistance, due to
fearing a possible lack of returns. This approach of the improper diagnosis, lack of understanding of the
pharmaceutical industry is due to the short period of potential dangers of inappropriate use, costs, and
antibiotic usage compared to other drugs used to treat outcomes of therapy. 4 During our hospital visit
metabolic, cardiovascular, and central nervous system as per the curriculum of Pharm. D. course in the
disorders. Hence, bacterial resistance to antibiotics is pediatric ward, we observed the use of antibiotics
inevitable, as newer antibiotics may be outdated in a to treat diseases which are generally self-limiting,
short span of time.2 to avoid hospital-acquired infections in Sri Ven-
In response to antibiotics, bacteria change in kateswara Ramnarayana Ruia Government General
ways that reduce or eliminate drug effectiveness. Hospital (SVRRGGH), Tirupathi. Hence, we aimed
These changes are due to the evolution of antibiotic to evaluate the extent of inappropriate prescrib-
resistance genes by spontaneous mutations and ing of antibiotics in treating dengue fever (DF) in
furthered by natural selection of resistant strains pediatric patients.
over sensitive ones. 3 Once a strain develops
resistance, the once-effective antibiotic will no
longer inhibit the bacteria. If this continues, Methods
mankind will eventually face a cataclysmic
condition. In view of this, the US Centers for Disease This cross-sectional, observational study was carried
Control and Prevention (CDC) declared in 2013 that out for 6 months (July to December 2016) in the
the human race is now in the ‘post-antibiotic era’. inpatient Department of Pediatrics, SVRRGGH,
Moreover, the World Health Organization (WHO) Tirupathi, India. The minimum required sample
warned of a dreadful antibiotic resistance crisis.2 size (n=370) used was based on the pilot study that
This situation is comparable to the pre-antibiotic was performed in the early weeks of July 2016 on 50
era, in that irrational use of antibiotics has led to patients.
the emergence of resistant strains and infections The study was approved by the Institutional
which are not yet recognized and the re-emergence Review Board, Sri Padmavathi School of Pharmacy,
of virulent forms of previous infections.1 Resistance Tiruchanoor, Tirupathi, India. All patients admitted
development is an evolutionary process, with to the pediatric inpatient ward of SVRRGGH with
unpredictable times. Resistance requires constant dengue fever during the study period were included
exposure of bacteria to the antibiotic. Hence, the in the study, except for those with other infections
rational or irrational use of antibiotics drives the and co-morbid conditions.
evolution of bacterial resistance. As such, the A specially designed pro forma was used for
greater the exposure of bacteria to antibiotics, the collecting data, including patient demographics,
faster the evolution of resistance.3 past medical history, family and surgical history,
Dengue and chikungunya are the third and traveling and transfusion history, signs and
fourth most common monsoon diseases in India. symptoms, diagnosis, and medications presently
They are mosquito-borne (Aedes aegypti) viral prescribed for each patient. The data were
diseases associated with urban environments. obtained from patient case profiles after obtaining
Dengue manifests as sudden onset of fever and parental informed consent. All prescriptions were
severe headache; it occasionally produces shock analyzed for the appropriate diagnosis, grading,
and hemorrhage leading to death. Chikungunya and presence of antibiotics, according to the 2009
is characterized by pain usually lasting 3-7 days WHO Guidelines5 and National Vector Borne Disease
and, in some cases, results in persistent arthritis. Control Programme (NVBDCP) Guidelines of India.6
These diseases share common symptoms of a typi- In addition, the presence of appropriate antibiotics
cal bacterial infection, and mislead health workers for hospital-acquired infection was also assessed
to use antibiotics unnecessarily. In addition, illicit based on Hospital Infection Society (HIS) Guidelines
prescribing of antibiotics by medical practitioners of India.7-9
54 • Paediatr Indones, Vol. 58, No. 1, January 2018
Dhanunjaya Sandopa1 et al.: Prescribing antibiotics to pediatric dengue: increasing risk of bacterial resistance
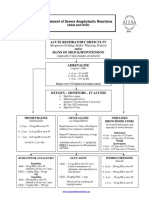
Results 9 (2.43%) cases, at a time (Figure 1). Triple therapy
antibiotics included cefotaxime in all prescriptions
In this study, we observed more DF cases (Table with cefixime, azithromycin, amoxyclav, doxycycline,
1) in children between the age group 5-10 years and ceftriaxone in different combinations. Antibiotics
(52.97%), followed by 0-4 years (37.29%) and 11-15 given as dual therapy were ceftriaxone with doxycycline,
years (9.23%). cefotaxime, or amoxyclav, and cefotaxime with
Out of 370 cases, 181 (48.91%) cases were doxycycline, cefixime, or metronidazole.
diagnosed based on platelet count, followed by NS1 Among the antibiotics prescribed, cefotaxime
antigen (36.75%), IgM (12.7%) and IgG (1.62%) and ceftriaxone were most commonly used (97 cases;
antibodies, while only 4.4% of cases were diagnosed 30.50% for each drug), followed by doxycycline
solely based on symptoms (Table 2). (17.92%), amoxyclav (10.06%), cefixime (3.77%),
In this study, 315 (85.13%) cases were appro amikacin (2.83%), azithromycin (2.51%), as well as
priately graded and 72 cases (19.45%) were inappro ciprofloxacin and metronidazole (0.94%) (Table 4).
priately graded (Table 3). Of the 315 appropriately-
graded cases, mild dengue was observed in 132 cases
(41.9%), moderate dengue in 176 cases (55.87%),
and severe dengue in 7 cases (2.22%). Among the
moderate and severe cases, DHF prevalence was
49.45% (183 subjects) in which DHF1 contributed to
the highest percentage (48.63%; 89 cases), followed
by DHF 2 (47.54%), and DHF 3 (3.82%).
Of 370 confirmed dengue cases, 267 (74.6%)
cases were prescribed antibiotics. A single antibiotic
was prescribed to 225 cases (60.81% of all cases), 2
antibiotics to 33 (8.91%) cases, and 3 antibiotics to
Figure 1. Distribution of antibiotics
Table 1. Age distribution of dengue fever patients
Age group No. of cases (N=370) Table 4. Antibiotic prescribing pattern
0-4 years 138 Antibiotic No. of prescription (N=267)
5-10 years 196 Cefotaxime, n(%) 96 (35.9)
11-15 years 36 Ceftriaxone, n(%) 96 (35.9)
Doxycycline, n(%) 37 (13.8)
Table 2. Diagnostic parameters used to diagnose dengue Amoxyclav, n(%) 23 (8.6)
fever Cefixime, n(%) 7 (2.6)
Parameters No. of cases (N=370) Amikacin, n(%) 4 (1.5)
PLT, n (%) 181 (48.91) Azithromycin, n(%) 2 (0.75)
NS1AG, n (%) 136 (36.75) Ciprofloxacin, n(%) 1 (0.38)
IgM, n (%) 47 (12.7) Metronidazole, n(%) 1 (0.38)
IgG, n (%) 6 (1.62)
Table 3. Appropriateness in grading dengue fever
Discussion
Grading No. of cases (N=370)
Inappropriate, n (%) 72 (19.45)
In this study we found that dengue was more
Appropriate, n (%) 315 (85.13)
prevalent in the age group of 5-10 years. This may
Paediatr Indones, Vol. 58, No. 1, January 2018 • 55
Dhanunjaya Sandopa1 et al.: Prescribing antibiotics to pediatric dengue: increasing risk of bacterial resistance
be because of children playing in unsanitary places assessment of complications. As manifestations of
or field areas where there is risk of being bitten by DF vary by grades, different treatment approaches
mosquitoes. There is no existing scientific reason for are required, as mentioned in the WHO Guidelines.
high prevalence of dengue in children, but the rate Mild dengue does not require therapy with IV fluids,
of mortality in pediatrics is high due to secondary while moderate and severe dengue requires IV fluid
infections, developing immunity, and exposure maintenance. Moderate dengue can be managed
to virulent strains, while most children remain with IV fluids at a rate of 2 to 3 mL/kg/hr, with
asymptomatic.10 reassessment of CBC to increase the rate up to 5 to
The most common monsoon diseases in 10 mL/kg/hr for 2 hours. In severe dengue, hemo-
India are malaria, diarrhea, dengue, chikungunya, dynamic status of the patient requires assessment,
typhoid, viral fevers, and cholera. They all share for the basis of the physician to decide between a
some common symptoms and present challenges bolus of 20 mL/kg in 15 minutes or maintenance
for the physician. Antibiotics are of no use in with IV fluids at a rate of 5 to 10 mL/kg/hr over
management of dengue and chikungunya, as they 1 hour. Otherwise, DF may be fatal after entering
are viral, infections. According to the WHO Clinical into the phases like shock and coma.5,6
Guidelines 5 and the 2014 NVBDCP Guidelines, 6 In our observation, 75% of the cases were
no drug of choice for dengue exists, as drugs that prescribed with antibiotics, under the guise of avoiding
directly act against dengue virus are still in the hospital-acquired infections. However, antibiotics
pipeline.11 Hence, therapy is solely based on the are not necessary to treat dengue, according to the
management of symptoms. Accurate diagnosis of guidelines. Empiric antibiotics are being prescribed
dengue can be confirmed based on serum positivity for suspected infections to avoid hospital-acquired
for NS1 antigen, IgM, and IgG antibodies. The infections. However, this empiric use of antibiotics
NS1 antigen can be determined by ELISA, which for treating nosocomial infections should be according
is highly sensitive, specific,12 and helpful in the to the HIS guidelines. In addition, antibiotics like
early diagnosis of acute infection. In our study, amikacin, doxycycline, and amoxyclav should not
we observed that platelet count determination be used without performing susceptibility tests, while
had been used in most (50%) of the cases to ceftriaxone and cefixime cannot be used prior to
diagnose dengue infection. This approach is not performing hypersensitivity tests.13-16 Azithromycin,
appropriate because thrombocytopenia occurs due ceftriaxone, and metronidazole can only be used
to destruction of platelets, mediated by antiplatelet- for the prophylaxis of endocarditis and sexually
antibodies observed from the 3rd day to the 7th day transmitted diseases (STDs).17,18 In addition, usage
of illness. Moreover, platelet count may also fall of amoxyclav in dengue can further increase the risk
in other infections like HIV, HHV-6, ehrlichiosis, of bleeding.14
Rickettisia, malaria, hepatitis-C, cytomegalovirus, The prescribing of antibiotics is an art requiring
Epstein-Barr syndrome, Helicobacter pylori, and skill in using the appropriate antibiotic for the
E. coli. Hence, platelet count is not an ideal diagnos particular infection. Inappropriate usage of more
tic parameter to diagnose dengue fever. However, it than one antibiotic increases the chances of
can be considered for prognosis of the disease. These developing multidrug resistance, which is a serious
implementations can make the physician clear and issue to be considered. Though there are many
confident regarding usage of antibiotics and further policies describing the appropriate indications
allows him to follow strict regimen recommended by for use of antibiotics, these drugs are often used
WHO and HIS of India and thus reduce the need for inappropriately. Furthermore, if this scenario
antibiotic use and cost burden on the patient. continues, the list of organisms developing resistance
Once the dengue diagnosis has been con- will increase. More powerful and costlier antibiotics
firmed, grading plays a major role in the success must be prescribed for simple infections, which
of the treatment. Inappropriate grading may result may have many adverse effects and can present an
in failure of therapy, and the need for advanced economic burden to patients.
56 • Paediatr Indones, Vol. 58, No. 1, January 2018
Dhanunjaya Sandopa1 et al.: Prescribing antibiotics to pediatric dengue: increasing risk of bacterial resistance
In conclusion, prescribing one or more antibio guidelines for clinical management of dengue fever. 2014 Dec;
tics to treat self-limiting viral infections is considered [cited 2016 March 17] Available from: https://www.scribd.
as inappropriate, and leads to the development of com/document/347257604/Dengue-National-Guidelines-
multidrug resistance. Furthermore, excess use of 2014-Compressed.
antibiotics in infancy may induce imbalances in gut 7. Hospital Infection Society guidelines. Nosocomial Infection
and microbiota, called dysbiosis, and increase the – Prevention and Management. 1-10; [cited 2016 March 15].
probability of diseases such as obesity, diabetes, and Available from: http://www.apiindia.org/pdf/pg_med_2008/
asthma in later life.19 These findings can be used to Chapter-08.pdf.
improve antibiotic stewardship in the treatment of 8. World Health Organization. Prevention of hospital-acquired
dengue. infections: a practical guide. Malta: WHO; 2002. p.1-64.
9. Mohammed M, Mohammed A, Mirza M, Ghori A. Noso
Acknowledgments comial infections: an overview. Int Res J Pharm. 2014;5:7-
12.
The authors are grateful to all who have contributed to the 10. Murray NE, Quam MB, Wilder-Smith A. Epidemiology of
success of this study. We especially acknowledge the Department dengue: past, present and future prospects. Clin Epidemiol.
of Pediatrics, Sri Venkateswara Ramnarayana Ruia Government 2013;5:299-309
General Hospital (SVRRGGH), Tirupathi, India for assistance in 11. Ghazala Z, Anuradha HV, Shivamurthy MC. Pattern of
procuring data. It has been a privilege and wonderful experience management and outcome of dengue fever in pediatric in-
to be part of this esteemed institution and we owe our sincere patients in a tertiary care hospital: a prospective observational
thanks to our Principal, Dr. D. Ranganayakulu, Sri Padmavathi study. International Journal of Basic & Clinical Pharmacology.
School of Pharmacy (SPSP), Tirupathi. We would also like to 2014; 3:534-8. DOI: http://dx.doi.org/10.5455/2319-2003.
express our profound gratitude to Mrs. P. Sulochana, BA, LLB, ijbcp20140623.
Chairperson, SPSP, Tirupathi who provided the facilities to 12. Bisordi I, Rocco IM, Suzuki A, Katz G, Silveira VR, Maeda
execute this work. AY, et al. Evaluation of dengue NS1 antigen detection for
diagnosis in public health laboratories, São Paulo State, 2009.
Rev Inst Med Trop São Paulo. 2011;53:315-20.
Conflict of Interest 13. HL Sharma, KK Sharma. Penicillins, cephalosporins and
other b-lactam antibiotics. In: Kothari Divyesh A, editors.
None declared. Principles of pharmacology. 2nd ed. New Delhi: Paras Medical
Publisher; 2103. p. 722-8.
14. Sharma HL, Sharma KK. Aminoglycosides. In: Kothari
References Divyesh A, editor. Principles of pharmacology. 2nd ed. New
Delhi: Paras medical publisher; 2103. p. 738.
1. Yoneyama H, Katsumata R. Antibiotic resistance in bacteria 15. Harvey RA. Protein synthesis inhibitors. In: Clark MA,
and its future for novel antibiotic development. Biosci editor. Pharmacology. 6th ed. New Delhi: Lippincott's
Biotechnol Biochem. 2006;70:1060-75.C. Illustrated Reviews Series; 2012. p. 395-404.
2. Ventola CL. The antibiotic resistance crisis: part 1: causes 16. Sharma HL, Sharma KK. Broad spectrum antibiotics:
and threats. P T. 2015;40:277-83. tetracyclines and chloramphenicol. In: Kothari Divyesh A,
3. Read AF, Woods RJ. Antibiotic resistance management. Evol editor. Principles of pharmacology. 2nd ed. New Delhi: Paras
Med Public Health. 2014;2014:147. medical publisher; 2103. p. 748-50.
4. Eandi M, Zara GP, Della Pepa C. Application of pharma 17. Sharma HL, Sharma KK. Macrolides, ketolides, lin
coeconomics to the use of antibiotics. Clin Microbiol Infect. cosamides, oxazolidones and other antibacterial drugs.
2000;6:90-2. In: Kothari Divyesh A, editor. Principles of pharmacology.
5. World Health Organization. Dengue: guidelines for diagnosis, 2nd edition. New Delhi: Paras medical publisher; 2103. p.
treatment, prevention and control. Geneva: World Health 741-3.
Organization; 2009. p.1-147. 18. Sharma HL, Sharma KK. Antiamoebic and other antipro
6. National vector borne disease control programme. National tozoal drugs. In: Kothari Divyesh A, editor. Principles of
Paediatr Indones, Vol. 58, No. 1, January 2018 • 57
Dhanunjaya Sandopa1 et al.: Prescribing antibiotics to pediatric dengue: increasing risk of bacterial resistance
pharmacology. 2nd ed. New Delhi: Paras Medical Publisher; 19. Vangay P, Ward T, Gerber JS, Knights D. Antibiotics, pediatric
2103. p. 819-21. dysbiosis, and disease. Cell Host Microbe. 2015;17:553-64.
58 • Paediatr Indones, Vol. 58, No. 1, January 2018
You might also like
- 9.insulin Treatment in ChildDocument21 pages9.insulin Treatment in Childirene aureliaNo ratings yet
- 1240-Article Text-2900-1-10-20170201 PDFDocument7 pages1240-Article Text-2900-1-10-20170201 PDFirene aureliaNo ratings yet
- Vitamin D Status in Egyptian Children With Allergic RhinitisDocument5 pagesVitamin D Status in Egyptian Children With Allergic Rhinitisirene aureliaNo ratings yet
- AnaphylacticDocument1 pageAnaphylacticirene aureliaNo ratings yet
- Can 2018Document4 pagesCan 2018Ayiek WicaksonoNo ratings yet
- Heart Murmurs in Healthy Newborn Babies 28.0.011Document3 pagesHeart Murmurs in Healthy Newborn Babies 28.0.011constantinNo ratings yet
- Who His HWF Amr 2018.1 EngDocument28 pagesWho His HWF Amr 2018.1 EngMaulina ManurungNo ratings yet
- Walsh 2018Document3 pagesWalsh 2018irene aureliaNo ratings yet
- Transport of Sick NB PDFDocument25 pagesTransport of Sick NB PDFirene aurelia100% (1)
- Bedolla Barajas2018Document7 pagesBedolla Barajas2018irene aureliaNo ratings yet
- Vitamin D Status in Egyptian Children With Allergic RhinitisDocument5 pagesVitamin D Status in Egyptian Children With Allergic Rhinitisirene aureliaNo ratings yet
- Peters2018 PDFDocument10 pagesPeters2018 PDFirene aureliaNo ratings yet
- 9.insulin Treatment in ChildDocument21 pages9.insulin Treatment in Childirene aureliaNo ratings yet
- 13.sick Day Management in CHDocument12 pages13.sick Day Management in CHirene aureliaNo ratings yet
- Association Between Caesarean Delivery and Isolated Doses of Formula Feeding in Cow Milk AllergyDocument6 pagesAssociation Between Caesarean Delivery and Isolated Doses of Formula Feeding in Cow Milk Allergyirene aureliaNo ratings yet
- 150327 Neonatal Sepsis 김세현 PDFDocument30 pages150327 Neonatal Sepsis 김세현 PDFirene aureliaNo ratings yet
- Multisite NIRS Application Precourse Arend BosDocument39 pagesMultisite NIRS Application Precourse Arend Bosirene aureliaNo ratings yet
- Rina Ramayani Komplikasi SN KONIKA XVIIDocument26 pagesRina Ramayani Komplikasi SN KONIKA XVIIirene aureliaNo ratings yet
- Peters2018 PDFDocument10 pagesPeters2018 PDFirene aureliaNo ratings yet
- Neonatal Transport - Diane CoadDocument28 pagesNeonatal Transport - Diane Coadirene aureliaNo ratings yet
- Transport of Sick NB PDFDocument25 pagesTransport of Sick NB PDFirene aurelia100% (1)
- Initial Assessment On PresentationDocument2 pagesInitial Assessment On PresentationAnggita Dewi RahmasariNo ratings yet
- Rtc-Scent 2012 05 Octaplex ProtocolDocument1 pageRtc-Scent 2012 05 Octaplex Protocolirene aureliaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Medical Certificate For Cause of DeathDocument1 pageMedical Certificate For Cause of DeathTikaNo ratings yet
- School Health ProgramDocument28 pagesSchool Health ProgramSubhash BishnoiNo ratings yet
- A Clinicians Pearls Myths in Rheumatology 2Nd Edition John H Stone Full ChapterDocument67 pagesA Clinicians Pearls Myths in Rheumatology 2Nd Edition John H Stone Full Chapterclarence.terry830100% (6)
- Precautions With Diabetic Patients Undergoing SurgeryDocument6 pagesPrecautions With Diabetic Patients Undergoing SurgeryErvin Kyle OsmeñaNo ratings yet
- Deg-Nala Disease: HistoryDocument3 pagesDeg-Nala Disease: Historysafi ullahNo ratings yet
- April 29 8:30AM - Dental Residencies by Mark KodayDocument23 pagesApril 29 8:30AM - Dental Residencies by Mark Kodayjordyn1990No ratings yet
- Nephrotic SyndromeDocument66 pagesNephrotic SyndromeNicole ChanNo ratings yet
- Physical Education - Ppt. Lesson 2Document24 pagesPhysical Education - Ppt. Lesson 2toni tesoro100% (1)
- Albendazole-Related Loa Loa EncephalopathyDocument2 pagesAlbendazole-Related Loa Loa EncephalopathyLucchéri Ndong AkomezogheNo ratings yet
- Speaking Sub-Test Overview: Roleplay StructureDocument23 pagesSpeaking Sub-Test Overview: Roleplay Structureelite9491100% (2)
- PharmacoinformaticsDocument25 pagesPharmacoinformaticsDaxesh Patel100% (2)
- Drug-Study-Po (1) EwesdfdsfdsfsddsfdsfdsDocument14 pagesDrug-Study-Po (1) EwesdfdsfdsfsddsfdsfdsIbrahim RegachoNo ratings yet
- Activity Design Mrsia 2018 Final BudgetDocument3 pagesActivity Design Mrsia 2018 Final BudgetRJay Mon MarcosNo ratings yet
- Ryans World Squad GoalsDocument1 pageRyans World Squad GoalsMelindaNo ratings yet
- A Comparative Study To Assess The Knowledge On Blood Donation Among Students ofDocument10 pagesA Comparative Study To Assess The Knowledge On Blood Donation Among Students ofGaoudam NatarajanNo ratings yet
- Transient Tachypnea of NewbornDocument4 pagesTransient Tachypnea of NewbornloraineNo ratings yet
- Certificate of EligibilityDocument6 pagesCertificate of EligibilitySweet SimyunnNo ratings yet
- 3) Measurement of Mortality and MorbidityDocument21 pages3) Measurement of Mortality and Morbidityjaish8904100% (1)
- American Board of Family Medicine: 2020 Questions & AnswersDocument112 pagesAmerican Board of Family Medicine: 2020 Questions & AnswersthanaaNo ratings yet
- QPD - Post-Discharge Follow-Up Phone Call Script SampleDocument3 pagesQPD - Post-Discharge Follow-Up Phone Call Script Samplejphinazee218No ratings yet
- 4.10.17final Clinical Trials Talk.4.10.2017 - 300526 - 284 - 30426 - v1Document67 pages4.10.17final Clinical Trials Talk.4.10.2017 - 300526 - 284 - 30426 - v1Mohammed HammedNo ratings yet
- 500 سؤال PDFDocument121 pages500 سؤال PDFAmir Atta100% (2)
- Jornal Materniti Blues-1Document10 pagesJornal Materniti Blues-1Izmi NasutionNo ratings yet
- Evaluation of Continuous Arch and Segmented Arch Leveling Techniques in Adult Patients-A Clinical Study PDFDocument6 pagesEvaluation of Continuous Arch and Segmented Arch Leveling Techniques in Adult Patients-A Clinical Study PDFDiana Paola FontechaNo ratings yet
- International Rescue Committee: Kenya ProgramDocument3 pagesInternational Rescue Committee: Kenya ProgramstevewanjiNo ratings yet
- Approach To The Child With Acute Diarrhea in Resource-Limited Countries - UpToDateDocument17 pagesApproach To The Child With Acute Diarrhea in Resource-Limited Countries - UpToDateNedelcu MirunaNo ratings yet
- Manulife CoverMe FollowMe Health Comp Chart Jan 2018 ENGLISHDocument2 pagesManulife CoverMe FollowMe Health Comp Chart Jan 2018 ENGLISHMamacintNo ratings yet
- Early Diagnosis & Prompt Treatment of Acute Abdominal Pain: Kiki Lukman The College of Surgeons of IndonesiaDocument69 pagesEarly Diagnosis & Prompt Treatment of Acute Abdominal Pain: Kiki Lukman The College of Surgeons of IndonesiaRani Silmi ZulafaNo ratings yet
- Abid Hussain: ARAR Group of Companies, Lahore - Assistant ManagerDocument2 pagesAbid Hussain: ARAR Group of Companies, Lahore - Assistant ManagerAbid HussainNo ratings yet
- EDITORIAL Successful Treatment Strategy of Turkey Against Covid19 Outbreak-12345 PDFDocument2 pagesEDITORIAL Successful Treatment Strategy of Turkey Against Covid19 Outbreak-12345 PDFMohaymin AljabryNo ratings yet