Professional Documents
Culture Documents
Diuretic Agents: Drug Group Urine Body Nacl Nahco K CL PH
Uploaded by
Justin Victor AngOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diuretic Agents: Drug Group Urine Body Nacl Nahco K CL PH
Uploaded by
Justin Victor AngCopyright:
Available Formats
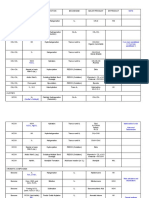
DIURETIC o Carbonic anhydrase, the enzyme required to reabsorb
HCO3 is the target of carbonic anhydrase inhibitor
AGENTS diuretic drugs
ELECTROLYTE CHANGES PRODUCED BY DIURETIC DRUGS o Active secretion and reabsorption of weak acids and
URINE BODY bases
Drug group Cl- Weak acid transport occur in the straight S2
NaCl NaHCO3 K+ 2 pH segment
Carbonic anhydrase Weak bases are transported in the S1 and S2
acidosis segments
inhibitors
Loop diuretics alkalosis o Uric acid transport
2. Thick Ascending Limb of the Loop of Henle (TAL)
Thiazides , alkalosis
o Reabsorption of sodium (20-30%), potassium and chloride
Potassium-sparing
, acidosis carried out by a single carrier (cotransporter) [target
diuretics
of loop diuretics]
Arrows under URINE indicate change in amount of salt or ion o Major site of calcium and magnesium reabsorption
excreted o Potassium is pumped into the cell from both luminal and
Arrows under BODY indicate change in concentration of basal sides, an escape route must be provided, this
chloride ion in blood occurs into the lumen via a potassium channel; since
the potassium diffusing back is not accompanied by an
anion, a net positive charge is set up in the lumen,
this positive potential drives the reabsorption of
calcium and magnesium
o
3. Distal convoluted tubule (DCT)
o Actively pumps sodium and chloride out of the lumen of
the nephron
o Responsible for the reabsorption of 5-8% of sodium via
a contransporter (target of thiazide diuretics)
o Calcium is reabsorbed under the control of parathyroid
hormone (PTH)
o Removal of the reabsorbed calcium back into the blood
requires the sodium-calcium exchange process
4. Cortical Collecting Tubules (CCT)
o The principal cells are the major sites of sodium,
potassium and water transport
o The intercalated cells are the primary sites of H+
secretion
o Last tubular site for sodium reabsorption (2-5%) via
Figure 15-2. Tubule transport systems and sites of action of channels (not a transporter) [controlled by
diuretics. Circles with arrows denote known ion cotransporters aldosterone]
that are targets of the diuretics indicated by the numerals. o Reabsorption is accompanied by equivalent loss of K+ or
Question marks denote preliminary or incompletely documented H+ ion
suggestions for the location of certain drug effects o The aldosterone receptor and sodium channels are the
RENAL TRANSPORT MECHANISM sites of K-sparing diuretic action
1. Proximal convoluted tubule o Primary site of acidification of urine
(PCT) o Reabsorption of water in the collecting tubule is under
o Isosmotic reabsorption the control of ADH
of amino acids, glucose,
and numerous cation
o Major site for sodium
chloride (60-70%)
reabsorption in exchange
for H+ ion
o Major site for
bicarbonate reabsorption
o Bicarbonate is not
absorbed through luminal
membrane, it is
converted to CO2 via
carbonic acid to permit
reabsorption and
regenerated within the
tubular cell
o Furosemide (prototype), Bumetanide, and Torsemide
Sulfonamide derivatives
o Ethacrynic acid
Phenoxy acid derivative
Acts by the same mechanism
Uricosuric drug
o Inhibit the cotransport of sodium, potassium and
chloride
o Short-acting (diuresis over a 4-hour period)
o Rapidly absorbed
o Excreted by glomerular filtration and tubular secretion
o Loop diuretic reduce the reabsorption of both Na and Cl
by inhibiting the Na/K/Cl transporter
o Diminish the normal lumen-positive potential across the
tubule and cause an increase in Mg and Ca excretion
(chronic use has been associated with Mg wasting and
severe hypomagnesemia)
o Increase of calcium excretion can be useful in acute
management of hypercalcemia
o Loop agents appear to have direct effects on blood flow
through several vascular beds
o Reduction in secretion if simultaneously administered
with NSAIDs or Probenacid
B. EFFECTS
o Full dose produces massive sodium chloride diuresis
o Diluting ability of the nephron is reduced (site of
significant dilution of urine)
o Calcium excretion is increased due to the inhibition of
the Na+/K+/2Cl-transporter
o Potassium wasting and proton excretion hypokalemic
CARBONIC ANHYDRASE INHIBITORS alkalosis
A. PROTOTYPES AND MECHANISM OF ACTION o Non-steroidal anti-inflammatory drugs (NSAIDS)
o Acetozolamide is the prototype decreases the efficacy
o Sulfonamide derivatives o Pulmonary vasodilating effect
o Forerunners of modern diuretics C. CLINICAL USES
o Inhibition of carbonic anhydrase in the brush border o Treatment of edematous states (heart failure, acute
and intracellular carbonic anhydrase in the PCT causing pulmonary edema, ascites)
NaHCO3 diuresis and a reduction in total body HCO3 o Used in HPN if response to thiazides is inadequate
stores o Treatment of hypercalcemia (induced by malignancy)
o Inhibition of carbonic anhydrase also occurs in other managed by parenteral volume and electrolyte
tissues of the body as well as in the kidneys supplementation
o Well absorbed orally o Hyperkalemia
o Latency = 30 min o Acute renal failure can increase urine flow and
peak effect in 2 hrs. and persists for 12 hrs. enhance K excretion, can help flush large pigment load
after a single dose and intratubular casts, ameliorate intratubular
o Excreted through the S2 segment of the proximal tubule obstruction
by tubular secretion o Anion overdose toxic ingestion of bromide, fluoride,
o At maximal safely administered dosage, 85% inhibition iodide
of proximal bicarbonate reabsorption or 45% inhibition D. TOXICITY
of whole kidney HCO3 reabsorption (Acute HCO3 wasting o Can induce hypokalemic metabolic alkalosis
condition) o Potassium wasting maybe severe
o CA inhibition causes significant HCO3 losses and o Can cause hypovolemia and cardiovascular complications
hyperchloremic metabolic acidosis o Ototoxicity and sulfonamide allergy
B. EFFECTS o Hypomagnesemia
o Major renal effect is bicarbonate diuresis (eg. sodium o Hyperruricemia
bicarbonate is excreted) o Allergic and other reactions
body bicarbonate is depleted and results to skin rashes
metabolic acidosis eosinophilia
o Bicarbonate depletion results to slowing of its severe dehydration
excretion hyponatremia
o Self-limiting diuresis in 2-3 days
o Contraindication
o As increased sodium is presented to the CCT some of the
Cirrhosis
excess sodium is reabsorbed and potassium is secreted,
Borderline renal failure
resulting in a significant potassium “wasting”
Heart failure
o Inhibitory effect occurs throughout the body
o Useful reduction in IOP in the eye which is not self-
limiting Used for the treatment of glaucoma THIAZIDE DIURETICS
o In the CNS, acidosis can result to hyperventilation A. PROTOTYPE
which can protect against high altitude sickness (acute o Hydrochlorothiazide
mountain sickness) Used as diuretic if the edema is o Sulfonamide derivative
accompanied by metabolic alkalosis o Active by the oral route
o Urinary alkalinization (excretion of uric acid, o 6-12 hours duration of action
cystine, other weak acids can be enhance by increasing o Inhibit sodium chloride transport in the early segment
urine pH) of the DCT
o Metabolic alkalosis o Produces moderate sodium and chloride diuresis
o Adjuvants for the treatment of epilepsy, hypokalemic o Secreted by the organic acid secretory system in the
periodic paralysis, to increase urinary phosphate proximal tubule
excretion during hyperphosphatemia o Competes with the secretion of uric acid [can elevate
C. TOXICITIES levels of uric acid]
o Drowsiness and paresthesias occur after oral intake o Hypokalemic metabolic alkalosis may occur
o Alkalinization of the urine may cause precipitation of o Few sulfonamide derivatives lack the typical thiazide
calcium salts and formation of renal stones ring in their structure but have effects similar to
o Renal potassium wasting thiazides therefore are considered thiazide-like
o Patients with renal impairment may develop - Prototype drug
Hydrochlorothiazide
encephalopathy due to ammonia reabsorption - Sulfonamide derivative
o Hypersensivity reactions - Not very lipid soluble and
Fever rashes must given in large doses
BM suppression - Slowly absorbed and longer
Chlorothiazide
Interstitial nephritis duration of action
o Contraindications - Only thiazide available as
Decrease urinary excretion of NH4 and may parenteral administration
contribute to hyperammonemia and hepatic B. EFFECTS
encephalopathy in patients with cirrhosis o Reduction in the transport of sodium into the tubular
cell reduces intracellular sodium and promotes sodium-
LOOP DIURETICS calcium exchange reabsorption of calcium urine
A. PROTOTYPES AND MECHANISM OF ACTION calcium content is decreased
o Opposite of loop diuretics
o Rarely cause hypercalcemia but may unmask hypercalcemia 1° Conn’s syndrome
due to other causes (hyperparathyroidism, carcinoma, ectopic production
sarcoidosis) 2° heart failure
o Reduce BP (initially, reflects reduction in blood Cirrhosis
volume) nephrotic syndrome
o Reduce vascular resistance (continued use) [effect is D. TOXICITY
modest but significant and maximal at doses lower than 1. Hyperkalemia
the maximal diuretic dosage] 2. Hyperchloremic metabolic acidosis (inhibition of H
o Synergistic effect with loop diuretic producing marked secretion)
diuresis 3. Gynecosmastia, impotence, BPH (Spironolactone)
o Actions of thiazides can be inhibited by NSAIDs [endocrine abnormalities]
C. CLINICAL USES 4. Acute renal failure (Triamterene combined with
1. Hypertension and CHF [used for chronic therapy of mild Indomethacin)
edematous conditions (mild heart failure)] 5. Kidney stones (Triamterene)
2. Nephrolithiasis due to Idiopathic hypercalciuria [stone slightly soluble, may precipitate in the urine
formation can be reduced because of reduction in urine o Contraindications
calcium concentration] i. Chronic renal insufficiency
3. Nephrogenic Diabetes Insipidus ii. Liver disease
D. TOXICITY iii. Fatal hyperkalemia with concomitant use of beta
1. Massive sodium diuresis with hyponatremia can be an blockers and ACE inhibitors
early dangerous effect
2. Potassium wasting and metabolic alkalosis OSMOTIC DIURETICS
3. Diabetic patients may have significant hyperglycemia A. PROTOTYPE AND MECHANISM OF ACTION
4. Serum uric acid (hyperuricemia) and lipid levels may o Mannitol is the prototype
increase (hyperlipidemia) o Glycerin, Isosorbide, Urea (these are rarely used)
5. Sulfonamide allergy o Freely filtered at the glomerulus but poorly reabsorbed
6. Impaired carbohydrates tolerance in the tubules remains in the lumen and “holds” water
7. Allergic and other reactions by virtue of osmotic effect
skin rashes, photosensitivity, hemolytic anemia, o Given intravenously
thrombocytopenia, acute pancreatitis, acute o Sodium excretion is increased because the rate of urine
pulmonary edema, weakness, fatigability, flow is accelerated
paresthesias, impotence o Major location of action is at the PCT, where the bulk
o Contraindications: of isoosmotic reabsorption normally takes place
i. Cirrhosis to avoid K depletion and hepatic o Reabsorbtion of water is also reduced in the ascending
encephalopathy limb of the loop of Henle and collecting tubule
ii. Renal failure (renal insufficiency may be B. EFFECTS
intensified) o Increased urine volume
iii. Digitalis toxicity may manifest as a result of o Increased excretion of most filtered solutes unless
diuretic-induced K depletion they are actively reabsorbed
o Increased sodium excretion
because of accelerated urine flow in the tubules
and sodium transporters cannot handle the volume
POTASSIUM-SPARING DIURETICS rapidly enough
A. PROTOTYPES AND MECHANISM OF ACTION o Reduce brain volume and intracranial pressure
o Prevent K secretion by antagonizing the effects of (neurologic conditions) by osmotically extracting water
aldosterone at the cortical collecting tubule from the tissue
o Inhibition may occur by o With similar effect in the eye (acute glaucoma)
i. Direct antagonism at the level of cytoplasmic
mineralocorticoid receptors (Spirolactones)
ii. Suppression of renin or angiotensin II generation C. CLINICAL USES
(ACE inhibitors) o Used to maintain high urine flow
iii. Direct inhibition of Na transport through ion i. When renal blood flow is reduced
channels in the luminal membrane (Triamterene, ii. Solute overload (eg. severe hemolysis,
Amiloride) rhabdomyolysis)
o Combine and block intracellular aldosterone receptor iii. Reduce IOP in acute glaucoma
reduce expression of genes controlling synthesis iv. Reduce intracranial pressure in neurologic
of sodium ion channels and Na+/K+ ATPase conditions
o Actions can be inhibited by NSAIDs [dependent on renal D. TOXICITIES
o Extracellular volume expansion causing hyponatremia and
prostaglandin production]
pulmonary edema in patients with heart failure
- Synthetic steroids that acts as a
prior to diuresis because mannitol is rapidly
competitive antagonist to
distributed in extracellular compartment and
aldosterone [bind to aldosterone
extracts water from cells
receptors and reduce intracellular
o Headache, nausea and vomiting
formation of active metabolites of
SPIRONOLACTONE o Dehydration leading to hypernatremia
aldosterone]
o hyperkalemia as water is extracted from cells
- Inactivation occurs in the liver
- Slow onset of action with full
therapeutic effect achieved after ANTIDIURETIC HORMONE AGONISTS
several days A. PROTOTYPES AND MECHANISM OF ACTION
A spironolactone analog with greater o Antidiuretic hormone (ADH) [Vasopressin] and
EPLERENONE Desmopressin
selectivity for aldosterone receptor
- Extensively metabolized in the Prototypes
liver ADH agonists
- Major route of elimination is via Peptides
the kidneys Given IV
TRIAMTERENE
- Short half-life, given more Used in the treatment of central diabetes
frequently insipidus
- Direct inhibitor of Na influx in Renal action is mediated by V2 receptors and V1a
the cortical collecting tubule receptors
- Excreted unchanged in the urine - Nonpeptide ADH receptor antagonist
- A pyrazine carbonyl-guanidine (vaptan) approved for use
derivative - Orally active
AMILORIDE
- 50% oral absorption CONIVAPTAN - Inhibit effects of ADH in the
- Direct inhibitor of Na influx in collecting tubule
the cortical collecting tubule - Pharmacologic antagonist at V1a and V2
B. EFFECTS receptors
o Increase sodium clearance and decrease potassium and - A tetracycline antimicrobial drug
hydrogen excretion - Orally active
o May cause hyperkalemic metabolic acidosis - Inhibit effects of ADH in the
C. CLINICAL USE collecting tubule
o Treatment of potassium wasting caused by chronic DEMECLOCYCLINE - Reduce the formation of cAMP in
therapy with loop and thiazide diuretics (combination response to ADH
in a single pill) - Interfere with the actions of cAMP in
o Treatment of hyperaldosteronism (mineralocorticoid the collecting tubule cells
excess) - Mechanism is unknown
- Orally active
- Has anti-ADH effects but is never used
as an ADH antagonist
- Inhibit effects of ADH in the
collecting tubule
LITHIUM
- Reduce the formation of cAMP in
response to ADH
- Interfere with the actions of cAMP in
the collecting tubule cells
- Mechanism is unknown
B. EFFECTS AND CLINICAL USES
o Treatment of Syndrome of Inappropriate ADH secretion
(SIADH)
Condition where peptides are produced by certain
tumors
Can cause water retention and dangerous
hyponatremia
Lithium carbonate gives unpredictable response
Demeclocycline yields more predictable resulst and
less toxic
Conivaptan given via IV, not suitable for chronic
use in outpatients
o Pituitary diabetes insipidus
ADH and Desmopressin are useful
Not useful for nephrogenic diabetes insipidus
C. TOXICITIES
o Nephrogenic diabetes insipidus
If serum sodium is not monitored ADH antagonists
may cause severe hypernatremia and Nephrogenic DI
Patients with psychiatric disorder and treated
with Lithium can develop Nephrogenic DI (can be
treated with thiazide diuretic or amiloride)
o Renal failure
Caused by Lithium and Demeclocycline
Lithium can cause chronic interstitial nephritis
o Demeclocycline causes bone and teeth abnormalities in
children younger than 12 years old and those with liver
disease
CLINICAL PHARMACOLOGY OF DIURETIC AGENTS
1. Heart failure
EDEMATOUS 2. Hepatic
STATES cirrhosis
3. Kidney diseases
4. Idiopathic edema
1. Hypertension
NONEDEMATOUS 2. Nephrolithiasis
STATES 3. Hypercalcemia
4. Diabetes
insipidus
You might also like
- Carbonates in Continental Settings: Facies, Environments, and ProcessesFrom EverandCarbonates in Continental Settings: Facies, Environments, and ProcessesNo ratings yet
- Diuretics IDocument17 pagesDiuretics Iأمجد محمدNo ratings yet
- Applied Renal PhysiologyDocument18 pagesApplied Renal PhysiologyDamián ContrerasNo ratings yet
- 18 Diuretics (Notes) AtfDocument19 pages18 Diuretics (Notes) AtfSeerat ShabirNo ratings yet
- Acute Tubular Renal AcidosisDocument10 pagesAcute Tubular Renal AcidosisBarda GulanNo ratings yet
- Tubular Reabsorption and Secretion: by Dr. Rukhsana AnwarDocument49 pagesTubular Reabsorption and Secretion: by Dr. Rukhsana AnwarZia PhotostateNo ratings yet
- Nephrology B (Javate) : Electrolytes Sodium (Na) Potassium (K) CalciumDocument9 pagesNephrology B (Javate) : Electrolytes Sodium (Na) Potassium (K) CalciumShekinah MalimbanNo ratings yet
- L5 - 6 - Renal Reabsorbation and SecretationDocument21 pagesL5 - 6 - Renal Reabsorbation and SecretationBryn MasvaureNo ratings yet
- Physio 2Document6 pagesPhysio 2Mohammad AlomariNo ratings yet
- L4 Regional Transport 2023Document4 pagesL4 Regional Transport 2023bgj9cddvxhNo ratings yet
- Tubular Function (Distal Tubule)Document26 pagesTubular Function (Distal Tubule)Hakimah K. SuhaimiNo ratings yet
- Physiological Ion ChlorideDocument15 pagesPhysiological Ion ChlorideMohammad Arafat Siddiqui100% (2)
- SHS.108.Lect-10 Tubular ReabsorptionDocument61 pagesSHS.108.Lect-10 Tubular ReabsorptionAzlan YasirNo ratings yet
- Renal Physiology The Collecting DuctDocument3 pagesRenal Physiology The Collecting DuctSahnusha SryenNo ratings yet
- Classification of DiureticDocument3 pagesClassification of DiureticJanice Malafu De GuiaNo ratings yet
- Manejo Tubular de SolutosDocument4 pagesManejo Tubular de SolutosAnghelussNo ratings yet
- Ion Exchange PDFDocument14 pagesIon Exchange PDFKomma RameshNo ratings yet
- Acid Base Balance in The KidneyDocument5 pagesAcid Base Balance in The KidneyTala IyadNo ratings yet
- Ion Exchange ChromatographyDocument35 pagesIon Exchange Chromatographysantosh100% (1)
- Ion Exchange ResinDocument18 pagesIon Exchange ResinIvana Cortés MárquezNo ratings yet
- Cicm Part 1 StudyDocument6 pagesCicm Part 1 StudyReesha CornelioNo ratings yet
- Lecture ObjectivesCopy 6Document2 pagesLecture ObjectivesCopy 6mickeyNo ratings yet
- 6-Drugs Acting On The Renal System - 2Document65 pages6-Drugs Acting On The Renal System - 2Hamid Hussain HamidNo ratings yet
- DCT and Collecting DuctDocument29 pagesDCT and Collecting DuctayeshaNo ratings yet
- Tubular Reabsorption and SecretionDocument21 pagesTubular Reabsorption and SecretionAhmad KhanNo ratings yet
- Tubular Secretion by The Renal Tubules: Prof./ Ibrahim Mohamady IbrahimDocument20 pagesTubular Secretion by The Renal Tubules: Prof./ Ibrahim Mohamady IbrahimOsama MohamedNo ratings yet
- Removal of Heavy Metals From Drinking Water Supplies Through The Ion Exchange Membrane BioreactorDocument3 pagesRemoval of Heavy Metals From Drinking Water Supplies Through The Ion Exchange Membrane BioreactorYesid Tapiero MartínezNo ratings yet
- Applications For Ion Exchange: Figure 10-9Document50 pagesApplications For Ion Exchange: Figure 10-9nermeen ahmedNo ratings yet
- Renal Physiology BY Dr. Olasupo. S. AdeniyiDocument6 pagesRenal Physiology BY Dr. Olasupo. S. AdeniyiUloko ChristopherNo ratings yet
- Distal Tubule Balance and Tubuloglomerular Feedback-Group 2Document42 pagesDistal Tubule Balance and Tubuloglomerular Feedback-Group 2Chuleha SethNo ratings yet
- Renal Pharmacology 2023Document116 pagesRenal Pharmacology 2023sami MesfinNo ratings yet
- Renal SystemDocument91 pagesRenal SystemKetheesaran LingamNo ratings yet
- Membrane Transport: Biochemistry of MetabolismDocument39 pagesMembrane Transport: Biochemistry of MetabolismJonny2010No ratings yet
- L5&6-Tubular Reabsorption& SecretionDocument38 pagesL5&6-Tubular Reabsorption& SecretionsairahhannahNo ratings yet
- c15 Diuretic AgentsDocument13 pagesc15 Diuretic AgentsmohammadNo ratings yet
- RenalDocument134 pagesRenalMaleehaNo ratings yet
- BicarbonateDocument5 pagesBicarbonateRace MendezNo ratings yet
- Lec 14 - Kidney PDFDocument16 pagesLec 14 - Kidney PDFrajeshNo ratings yet
- Pedia 3A Nephrology Dr. Javate ParbsDocument15 pagesPedia 3A Nephrology Dr. Javate ParbsVERGARA, DINSLEENo ratings yet
- Renal Tubular Acidosis: Moderator:Dr Nitin Joshi Presented By: Dr. Parth Nathwani MGM Medical College, MumbaiDocument71 pagesRenal Tubular Acidosis: Moderator:Dr Nitin Joshi Presented By: Dr. Parth Nathwani MGM Medical College, MumbaiariNo ratings yet
- GUS1-K6-Reabsorpsi & Sekresi TubulusDocument33 pagesGUS1-K6-Reabsorpsi & Sekresi TubulusMarieta RitongaNo ratings yet
- REN Revision LectureDocument43 pagesREN Revision Lecturegyamfi.rolandNo ratings yet
- Reabsorption of SodiumDocument19 pagesReabsorption of Sodiumpriya shettyNo ratings yet
- Tubular ReabsorptionDocument42 pagesTubular Reabsorptionmina mounirNo ratings yet
- Renal 2 MTC PDFDocument55 pagesRenal 2 MTC PDFDrbee10No ratings yet
- What Is Diuretic? Classify Diuretics? A Diuretic Is DefinedDocument3 pagesWhat Is Diuretic? Classify Diuretics? A Diuretic Is DefinedSujan Bose100% (1)
- PHS RenalDocument44 pagesPHS Renaltewogbadeomobuwajo005No ratings yet
- WATER TREATMENT - Anion Exchangers - Ion Exchange W. H. HöllDocument8 pagesWATER TREATMENT - Anion Exchangers - Ion Exchange W. H. HöllMichael OkaiNo ratings yet
- Electrolyte 1Document8 pagesElectrolyte 1Ylooner QuitsNo ratings yet
- Salivation: Done By: Fatima Ammash & Malak RizkDocument20 pagesSalivation: Done By: Fatima Ammash & Malak RizkAbeda AmmashNo ratings yet
- Principles of Ion ExchangeDocument5 pagesPrinciples of Ion ExchangeYsabelle JimeneaNo ratings yet
- Handling of Certain Important Solutes by The Renal TubulesDocument14 pagesHandling of Certain Important Solutes by The Renal TubulesOsama MohamedNo ratings yet
- Intestinal Ion Transport and The Pathophysiology of Diarrhea - PMCDocument22 pagesIntestinal Ion Transport and The Pathophysiology of Diarrhea - PMCtanatswa courtney matingoNo ratings yet
- SODIUMDocument4 pagesSODIUMNorhidayah NoordinNo ratings yet
- Anthony M. Wachinski - Environmental Ion Exchange - Principles and Design-Taylor & Francis, Chapman and Hall - CRC (2016) (1) (044-093)Document50 pagesAnthony M. Wachinski - Environmental Ion Exchange - Principles and Design-Taylor & Francis, Chapman and Hall - CRC (2016) (1) (044-093)HARDY EDDISONNo ratings yet
- Diuretics and Renal Hormones - McMaster Pathophysiology ReviewDocument4 pagesDiuretics and Renal Hormones - McMaster Pathophysiology ReviewSandra MedinaNo ratings yet
- Part 1 - US-Grade 4-BiochemistryDocument34 pagesPart 1 - US-Grade 4-BiochemistryFarah Bashar Al-RawachyNo ratings yet
- L3 +L4 Renal System 2023Document31 pagesL3 +L4 Renal System 2023mizare29gNo ratings yet
- Renal Tubular TransportDocument38 pagesRenal Tubular TransportAhmad KhanNo ratings yet
- 22 Ion Exchange Chromatography LatestDocument29 pages22 Ion Exchange Chromatography LatestsanjayjkhasiyaNo ratings yet
- AlcoholsDocument2 pagesAlcoholsJustin Victor AngNo ratings yet
- Informative Speech On Those ChoicesDocument2 pagesInformative Speech On Those ChoicesJustin Victor AngNo ratings yet
- Org Chem E8 Classification Tests For Organic HalidesDocument4 pagesOrg Chem E8 Classification Tests For Organic HalidesJustin Victor AngNo ratings yet
- Occupational Toxicology: Threshold Limit Values (TLVS) Environmental ToxicologyDocument7 pagesOccupational Toxicology: Threshold Limit Values (TLVS) Environmental ToxicologyJustin Victor AngNo ratings yet
- Cns and AlcoholsDocument6 pagesCns and AlcoholsJustin Victor AngNo ratings yet
- Qualitative Analysis of Hydrolysates - Paper ChromatographyDocument5 pagesQualitative Analysis of Hydrolysates - Paper ChromatographyJustin Victor AngNo ratings yet
- Solubility Classification Using Water 5Document1 pageSolubility Classification Using Water 5Justin Victor AngNo ratings yet
- Recrystallization: Justin G. Ang and Nadine T. CaragDocument3 pagesRecrystallization: Justin G. Ang and Nadine T. CaragJustin Victor AngNo ratings yet
- Solubility Classification Using Water 5Document1 pageSolubility Classification Using Water 5Justin Victor AngNo ratings yet
- Qualitative Color Reactions of AlbuminDocument6 pagesQualitative Color Reactions of AlbuminJustin Victor AngNo ratings yet
- 7 SolubilityDocument5 pages7 SolubilityJoeco Abay-abayNo ratings yet
- Urinalysis ReferencesDocument2 pagesUrinalysis ReferencesJustin Victor AngNo ratings yet
- DsadaDocument2 pagesDsadaJustin Victor AngNo ratings yet
- Observations:: Lab Report For Experiment #2: Purification of Acetanilide by RecrystallizationDocument2 pagesObservations:: Lab Report For Experiment #2: Purification of Acetanilide by RecrystallizationJV GamoNo ratings yet
- 7 SolubilityDocument5 pages7 SolubilityJoeco Abay-abayNo ratings yet
- Title: Bianca Andrea C. Acuña, Pamela Tristen G. Agbayani, Gian Searle S. AlkuinoDocument1 pageTitle: Bianca Andrea C. Acuña, Pamela Tristen G. Agbayani, Gian Searle S. AlkuinoJustin Victor AngNo ratings yet
- Classification Tests For Organic HalidesDocument3 pagesClassification Tests For Organic HalidesRhone Roque100% (6)
- Experiment 9 Chem Formal ReportDocument7 pagesExperiment 9 Chem Formal ReportJustin Victor AngNo ratings yet
- Separation and Identification of Amino Acids by Paper ChromatographyDocument4 pagesSeparation and Identification of Amino Acids by Paper ChromatographyJustin Victor AngNo ratings yet
- Catalyst Note: (PT, Ni, PD)Document8 pagesCatalyst Note: (PT, Ni, PD)Justin Victor AngNo ratings yet
- Title: Bianca Andrea C. Acuña, Pamela Tristen G. Agbayani, Gian Searle S. AlkuinoDocument1 pageTitle: Bianca Andrea C. Acuña, Pamela Tristen G. Agbayani, Gian Searle S. AlkuinoJustin Victor AngNo ratings yet
- Experiment 2: Resultant and Equilibrant ForcesDocument7 pagesExperiment 2: Resultant and Equilibrant ForcesJustin Victor AngNo ratings yet
- Experiment 2: Resultant and Equilibrant ForcesDocument7 pagesExperiment 2: Resultant and Equilibrant ForcesJustin Victor AngNo ratings yet
- Experiment 2: Resultant and Equilibrant ForcesDocument7 pagesExperiment 2: Resultant and Equilibrant ForcesJustin Victor AngNo ratings yet
- Math Model Qs by NRBDocument4 pagesMath Model Qs by NRBapi-3825027No ratings yet
- Assignment CHAP NO 1.... Computer Fundamentals by PK SinhaDocument7 pagesAssignment CHAP NO 1.... Computer Fundamentals by PK SinhaThreating King100% (2)
- Anatomy-Head and NeckDocument94 pagesAnatomy-Head and NeckXahid IqbalNo ratings yet
- BOSCH FLEXIDOME Multi 7000 - DatasheetDocument8 pagesBOSCH FLEXIDOME Multi 7000 - DatasheetMarlon Cruz CruzNo ratings yet
- Asus Prime b250m Plus RGDocument13 pagesAsus Prime b250m Plus RGRenattech SilvaNo ratings yet
- Front Axle, Tie Rod and Drag Link (A21) - 20: Parts ListDocument4 pagesFront Axle, Tie Rod and Drag Link (A21) - 20: Parts ListdgloshenNo ratings yet
- Introduction To NFFHT: Shyam Sunder Assistant Professor Mechanical EngineeringDocument44 pagesIntroduction To NFFHT: Shyam Sunder Assistant Professor Mechanical EngineeringTAPASVI BHATTNo ratings yet
- T 703Document4 pagesT 703Marcelo RojasNo ratings yet
- 1 IntroductionDocument25 pages1 IntroductionNida I. FarihahNo ratings yet
- Hot Vibrating Gases Under The Electron Spotlight: Gas MoleculesDocument2 pagesHot Vibrating Gases Under The Electron Spotlight: Gas MoleculesRonaldo PaxDeorumNo ratings yet
- Journal of Experimental Biology and Agricultural Sciences: Anitha KC, Rajeshwari YB, Prasanna SB and Shilpa Shree JDocument5 pagesJournal of Experimental Biology and Agricultural Sciences: Anitha KC, Rajeshwari YB, Prasanna SB and Shilpa Shree Jkristel amadaNo ratings yet
- Recruiting Test General KnowledgeDocument15 pagesRecruiting Test General KnowledgeRelando Bailey84% (174)
- Aiwa CX jn5 ETDocument78 pagesAiwa CX jn5 ETluzmarospiNo ratings yet
- A Framework For Developing and Evaluating Utility Substation Cyber Security - Schneider ElectricDocument10 pagesA Framework For Developing and Evaluating Utility Substation Cyber Security - Schneider ElectricHugh cabNo ratings yet
- PHontDawg Vol.2 2007Document8 pagesPHontDawg Vol.2 2007Tanczos AndrasNo ratings yet
- The Design of Hazard Analysis Critical Control Point (HACCP) Plan For Biscuit PlantDocument7 pagesThe Design of Hazard Analysis Critical Control Point (HACCP) Plan For Biscuit Plantttk_maniNo ratings yet
- Previews 2502414 PreDocument9 pagesPreviews 2502414 PreAlex Andre RojasNo ratings yet
- m1340008 Dark FutureDocument220 pagesm1340008 Dark Futurejkj1176100% (1)
- Export - Carpet IndustryDocument36 pagesExport - Carpet IndustryShruti MittalNo ratings yet
- LANCNC Display Mount Plate Installation v5Document10 pagesLANCNC Display Mount Plate Installation v5Maquina EspecialNo ratings yet
- The Relationship of Language Development and Nutritional Status of The Child in The Region South of The City of Kediri Region Public HealthDocument12 pagesThe Relationship of Language Development and Nutritional Status of The Child in The Region South of The City of Kediri Region Public Healthdoddyk kurniawanNo ratings yet
- Spare Parts: LKH Centrifugal PumpDocument20 pagesSpare Parts: LKH Centrifugal PumpService CTANo ratings yet
- Frequency Adverbs Worksheet - Basic 02 IntensiveDocument2 pagesFrequency Adverbs Worksheet - Basic 02 IntensiveMorelia AlfaroNo ratings yet
- Daftar PustakaDocument2 pagesDaftar PustakaJohny Iskandar Arsyad NstNo ratings yet
- Solving Poisson's Equation Using The FFTDocument9 pagesSolving Poisson's Equation Using The FFTJhon CerónNo ratings yet
- Off-Label Drug Use - 2020Document14 pagesOff-Label Drug Use - 2020Bigabwa BernardNo ratings yet
- Let's Study This TextDocument9 pagesLet's Study This TextAnara BhismaNo ratings yet
- Pharmaceutics Exam 3 - This SemesterDocument6 pagesPharmaceutics Exam 3 - This Semesterapi-3723612100% (1)
- Title: "The Effect of Flooding in The Tourism Industry in Dagupan City" Rationale and Background of The StudyDocument4 pagesTitle: "The Effect of Flooding in The Tourism Industry in Dagupan City" Rationale and Background of The StudyTaehyung KimNo ratings yet
- Draconomicon 2 Metallic Dragons PDF 73Document3 pagesDraconomicon 2 Metallic Dragons PDF 73gabiNo ratings yet