Professional Documents
Culture Documents
Escherichia Coli Isolate Recovered From The Ear of A 4-Month-Old Child With Otitis Media
Uploaded by
justinOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Escherichia Coli Isolate Recovered From The Ear of A 4-Month-Old Child With Otitis Media
Uploaded by
justinCopyright:
Available Formats
In the last 15 years, varieties of plasmid-mediated β-lactamases have been identified in
Gram-negative bacteria, one of which includes the extended-spectrum β-lactamases (ESBL)
(Liebana et al., 2013). Among the β-lactamases, ESBL are known as enzymes that can hydrolyze
extended-spectrum (third genereation) cephalosporins (e.g., cefotaxime, ceftriaxone, ceftazidime,
and cefepime) and monobactams (e.g., aztreonam) but do not affect cephamycins (e.g., cefoxitin
and cefotetan) or carbapenems (e.g., meropenem or imipenem). Class A ESBLs mainly include
TEM, SHV, CTX-M, VEB, and GES enzymes (Coque et al., 2008; Pitout & Laupland, 2008;
Center of Disease Control and Prevention, 2010).
ESBL testing is performed for epidemiological purposes because ESBL-resistance genes
transmit rapidly. After the prevalence of ESBLs such as SHV-1 and TEM-1, the ESBL family of
cefotaxime β-lactamases (CTX) have increased in frequency around the world (Woerther, Burdet,
Chachaty, & Adremont, 2013; D’Andrea, Arena, Pallechi, & Rossolini, 2013). CTX-M β-
lactamases form a non-homogenous complex group of enzymes and can be divided into five
clusters according to amino acid sequence, with each genotype of CTX-M having different
hydrolysis reactions to β-lactam antibiotics. Unlike other ESBLs, CTX-M did not originate from
mutations of plasmid mediated enzymes but through the mobilization of chromosomal bla genes
of Kluyvera spp into mobile genetic elements, which greatly inhibited the action of cefotaxime
compared to ceftazidime (Cantón, 2008).
CTX-M genes have become the most common ESBL genes due to their mobilization and
dissemination mechanisms, namely insertion sequences (e.g., ISEcpl, IS26, and ISCR1), integrons,
transposons, and plasmids (Bush & Fisher, 2011; Coque, Baquero, & Cantón, 2008). CTX-M-1
was first reported in Munich, Germany from a cefotaxime-resistant but ceftazidime-susceptible
Escherichia coli isolate recovered from the ear of a 4-month-old child with otitis media.
Succeeding enzymes were grouped under the CTX-M family due to their preferential hydrolytic
activity against cefotaxime. CTX-M enzymes were initially detected in Enterobacteriaciae,
including Escherichia coli, Klebsiella pneumoniae and Salmonella spp. but have increased in
prevalence among non-Enterobacteriaciae Gram-negative bacilli such as Pseudomonas
aeruginosa and Stenotrophomonas maltophila (Cantón, González-Alba, & Galán, 2012).
According to a study conducted by Tacão, Correia, and Henriques (2012), cefotaxime-resistant
strains recovered were identified as Pseudomonas spp. (i.e., P. fluorescens & P. putida),
Enterobacteriaciae such as Escherichia coli and Enterobacter spp., and Aeromonas spp.
Bush, K., Fisher, J.F. (2011). Epidemiological expansion, structural studies, and clinical
challenges of new beta-lactamases from Gram-negative bacteria. Annu. Rev.
Microbiol. 65, 455–478
Cantón, R. (2008). Epidemiology and evolution of β-lactamases, in Evolutionary Biology of
Bacterial and Fungal Pathogens, Washington: ASM Press, 249–270.
Cantón, R., González-Alba, J. M., & Galán, J.C. (2012). CTX-M Enzymes: Origin and Diffusin.
Front Microbiol. 3, 110. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC3316993/#fn1
Center for Disease Control and Prevention (2010). Healthcare-associated Infections. Retrieved
from https://www.cdc.gov/hai/settings/lab/lab_esbl.html.
Coque T. M., Baquero F., Cantón R. (2008). Increasing prevalence of ESBL-producing
Enterobacteriaceae in Europe. Euro Surveill.
D’Andrea, M.M., Arena, F., Pallecchi, L., & Rossolini, G.M. (2013). CTX-M-type beta-
lactamases: a successful story of antibiotic resistance. Int J Med Microbiol. 303, 05–17.
Liebana, E., Carattoli, A., Coque, T.M., Hasman, H., Magiorakos, A., Mevius, D. et al. (2013).
Public health risks of enterobacterial isolates producing extended-spectrum β-lactamases or
AmpC g-lactamases in food and food- producing animals: An EU perspective of
epidemiology, analytical methods, risk factors, and control options. Food Safety, 56,
1030-1037.
Pitout, J. D. & Laupland, K. B. (2008). Extended-spectrum β-lactamase-producing
Enterobacteriaceae: an emerging public-health concern. Lancet Infect. 159–
16610.1016/S1473-3099(08)70041-0
Tacão, M., Correia, A., & Henriques, I. (2012). Resistance to Broad-Spectrum Antibiotics in
Aquatic Systems: Anthropogenic Activities Modulate the Dissemination of blaCTX-M-Like
Genes. Appl Environ Microbiol. 78(12), 4134-4140. Retrieved from https://www.ncbi.
nlm.nih.gov/pmc/articles/PMC3370516/
Woerther, P.L., Burdet, C., Chachaty, E., & Andremont, A. (2013). Trends in human fecal
carriage of extended-spectrum beta-lactamases in the community: toward the
globalization of CTX-M. Clin Microbiol. 26, 744-758.
You might also like
- Blee NuevoDocument11 pagesBlee Nuevomarivero23No ratings yet
- Neonatal Infections With Multidrugresistant ESBL-producing E. Cloacae and K. Pneumoniae in Neonatal Units of Two Different Hospitals in Antananarivo, MadagascarDocument10 pagesNeonatal Infections With Multidrugresistant ESBL-producing E. Cloacae and K. Pneumoniae in Neonatal Units of Two Different Hospitals in Antananarivo, MadagascarJulie Jubane TiuNo ratings yet
- Artigo blaCTX revista Acta UERJ-ZO 2024Document11 pagesArtigo blaCTX revista Acta UERJ-ZO 2024Raphael ConegundesNo ratings yet
- Babol Jbums v17n8p19 enDocument8 pagesBabol Jbums v17n8p19 enTendi SulaksoNo ratings yet
- E00489-12 FullDocument10 pagesE00489-12 FulldoruolaruNo ratings yet
- First Detection of Bla TEM, SHV and CTX-M AmongDocument7 pagesFirst Detection of Bla TEM, SHV and CTX-M AmongHamidou OuedraogoNo ratings yet
- E. coli Infection Antibiotic TreatmentDocument2 pagesE. coli Infection Antibiotic TreatmentClement ThompsonNo ratings yet
- Extended Spectrum Beta Lactamase Dan Beta Lactamase Ampisilin Kelas C Yang Diproduksi Escherichia Coli Dari Hewan MakananDocument14 pagesExtended Spectrum Beta Lactamase Dan Beta Lactamase Ampisilin Kelas C Yang Diproduksi Escherichia Coli Dari Hewan MakananAnonymous Gvten4DxNo ratings yet
- The Innate Immune System in Cystic Fibrosis Lung Disease: PerspectiveDocument5 pagesThe Innate Immune System in Cystic Fibrosis Lung Disease: PerspectiveLenny Maulida ValentinaNo ratings yet
- Escherichia coli β-Lactamases: What Really Matters: Priyanka Bajaj, Nambram S. Singh and Jugsharan S. VirdiDocument14 pagesEscherichia coli β-Lactamases: What Really Matters: Priyanka Bajaj, Nambram S. Singh and Jugsharan S. VirdiEma GuillotineNo ratings yet
- Foodsafetyfscj 5 122Document29 pagesFoodsafetyfscj 5 122Medical Laboratory ChannelNo ratings yet
- 10 Contribution of IncFII and Broad-Host IncA C and IncN Plasmids ToDocument4 pages10 Contribution of IncFII and Broad-Host IncA C and IncN Plasmids ToluismitlvNo ratings yet
- BRICEÑO-2012-Clinical Issues of RDocument28 pagesBRICEÑO-2012-Clinical Issues of Rduverney.gaviriaNo ratings yet
- tmpBF53 TMPDocument6 pagestmpBF53 TMPFrontiersNo ratings yet
- Current Trends in Antimicrobial Resistance of Escherichia ColiDocument31 pagesCurrent Trends in Antimicrobial Resistance of Escherichia ColiWilson rocha untojaNo ratings yet
- OriginalDocument24 pagesOriginalHenrique FerreiraNo ratings yet
- Virus Research: S. Pereira, C. Pereira, L. Santos, J. Klumpp, A. AlmeidaDocument10 pagesVirus Research: S. Pereira, C. Pereira, L. Santos, J. Klumpp, A. AlmeidaNi'matul MfNo ratings yet
- tmp72AD TMPDocument6 pagestmp72AD TMPFrontiersNo ratings yet
- Parasites That Heal: What Our Old Friends' Can Do For Us - Integrative Health EducationDocument3 pagesParasites That Heal: What Our Old Friends' Can Do For Us - Integrative Health EducationmayapetrovaNo ratings yet
- tmp6899 TMPDocument12 pagestmp6899 TMPFrontiersNo ratings yet
- Klebsiella pneumoniae Virulence Factors and Antimicrobial ResistanceDocument21 pagesKlebsiella pneumoniae Virulence Factors and Antimicrobial Resistancekiss4444f4No ratings yet
- New Insights About The EptA Protein and Its Correlation With The PMRC Gene in Polymyxin Resistance in Pseudomonas AeruginosaDocument6 pagesNew Insights About The EptA Protein and Its Correlation With The PMRC Gene in Polymyxin Resistance in Pseudomonas AeruginosaEdnésioNo ratings yet
- The Ecology Epidemiology Dan Virulence of EnterococcusDocument9 pagesThe Ecology Epidemiology Dan Virulence of EnterococcusFerdian Iwank IriyantoNo ratings yet
- Chapter One 1.0 Introduction/Literature Review 1.1 Background of StudyDocument62 pagesChapter One 1.0 Introduction/Literature Review 1.1 Background of StudySolomonNo ratings yet
- Wang 2016Document11 pagesWang 2016meNo ratings yet
- Ijerph 20 01900 v2Document11 pagesIjerph 20 01900 v2edisonballaNo ratings yet
- 1 Zarfel2013Document8 pages1 Zarfel2013luismitlvNo ratings yet
- 1 s2.0 S1214021X14600260 MainDocument10 pages1 s2.0 S1214021X14600260 MainSandu AlexandraNo ratings yet
- Effector ReviewDocument26 pagesEffector ReviewSumit MukherjeeNo ratings yet
- Anthrax Lethal Toxin Disrupts Intestinal Barrier Function and Causes Systemic Infections With Enteric Bacteria 2012Document10 pagesAnthrax Lethal Toxin Disrupts Intestinal Barrier Function and Causes Systemic Infections With Enteric Bacteria 2012fer123wizNo ratings yet
- Avian Pathogenic Escherichia Coli APEC An Update On The ControlDocument21 pagesAvian Pathogenic Escherichia Coli APEC An Update On The ControllokmenNo ratings yet
- Mycobacterium Tuberculosis: Aerosol Infection Causes Rapid Loss of Diversity in Gut MicrobiotaDocument9 pagesMycobacterium Tuberculosis: Aerosol Infection Causes Rapid Loss of Diversity in Gut MicrobiotaImha MikanersandsmashblastNo ratings yet
- Role of The Gut Microbiota in Defining Human HealthDocument15 pagesRole of The Gut Microbiota in Defining Human HealthVictor ResendizNo ratings yet
- C 1 The Contribution of Laboratory Animals To Medical Progress - Past, Present, and FutureDocument11 pagesC 1 The Contribution of Laboratory Animals To Medical Progress - Past, Present, and FuturenduthNo ratings yet
- Harada 2017Document12 pagesHarada 2017Natasha SiqueiraNo ratings yet
- Articulo OxforDocument16 pagesArticulo OxforbosueNo ratings yet
- E Coli 2016Document27 pagesE Coli 2016alanbecker_alNo ratings yet
- Yang 2021Document6 pagesYang 2021perencanaandinkesnaganrayaNo ratings yet
- Novel Bacteriophage Cocktail Reduces and Disperses Pseudomonas Biofilms - 2016Document15 pagesNovel Bacteriophage Cocktail Reduces and Disperses Pseudomonas Biofilms - 2016Max OhNo ratings yet
- The global prevalence and trend of human intestinal carriage of ESBL e. coliDocument8 pagesThe global prevalence and trend of human intestinal carriage of ESBL e. coliMiriam LeiNo ratings yet
- The Role of The Natural Environment in The Emergence ofDocument11 pagesThe Role of The Natural Environment in The Emergence ofPierrotNo ratings yet
- The Role of Microbiota in Respiratory Health and DiseasesDocument13 pagesThe Role of Microbiota in Respiratory Health and DiseasesannewidiatmoNo ratings yet
- Amebic Colitis: María Carolina Isea, Andrés Escudero-Sepulveda and Alfonso J. Rodriguez-MoralesDocument20 pagesAmebic Colitis: María Carolina Isea, Andrés Escudero-Sepulveda and Alfonso J. Rodriguez-MoralesNam ChannelNo ratings yet
- Emerging Bacterial Pathogens in Meat and PoultryDocument12 pagesEmerging Bacterial Pathogens in Meat and PoultryRadwan AjoNo ratings yet
- S AureusDocument8 pagesS AureusMario Andres Quezada AguiluzNo ratings yet
- High Rate of Fecal Carriage of Extended-Spectrum-Lactamase children SpainDocument3 pagesHigh Rate of Fecal Carriage of Extended-Spectrum-Lactamase children SpainMiriam LeiNo ratings yet
- Dibawakan Pada Musyawarah Wilayah Ketiga (MUSWIL) Khusus Lbukota Jakarta, Jakarta April Pencliti Puslitbang Farmasi TradisionalDocument7 pagesDibawakan Pada Musyawarah Wilayah Ketiga (MUSWIL) Khusus Lbukota Jakarta, Jakarta April Pencliti Puslitbang Farmasi TradisionalPusparasmi Mas Ayu SuprabhaNo ratings yet
- TanzaniaDocument13 pagesTanzaniaDESIRE OTSAGHE EKORENo ratings yet
- Antimicrob. Agents Chemother. 2001 Lenart 2198 203Document7 pagesAntimicrob. Agents Chemother. 2001 Lenart 2198 203uhuhsuNo ratings yet
- Mechanisms of Antimicrobial Resistance in ESKAPE PathogensDocument8 pagesMechanisms of Antimicrobial Resistance in ESKAPE PathogensCinthia MadeiraNo ratings yet
- Commensals, pathogens, and intestinal inflammation: An intriguing ménage à troisDocument4 pagesCommensals, pathogens, and intestinal inflammation: An intriguing ménage à troisshaznay delacruzNo ratings yet
- Typhoid Fever Cellular ModelDocument7 pagesTyphoid Fever Cellular ModelTio Prima SNo ratings yet
- Recent Insights Into The Vaginal MicrobiotaDocument12 pagesRecent Insights Into The Vaginal Microbiotaps piasNo ratings yet
- Antibiotic Resistance Mechanisms in Bacteria: Biochemical and Genetic AspectsDocument11 pagesAntibiotic Resistance Mechanisms in Bacteria: Biochemical and Genetic AspectsD Wisam NajmNo ratings yet
- Smoking and The Intestinal Microbiome: Ziv Savin Shaye Kivity Hagith Yonath Shoenfeld YehudaDocument8 pagesSmoking and The Intestinal Microbiome: Ziv Savin Shaye Kivity Hagith Yonath Shoenfeld YehudaVERONICA ANDREA AGAMEZ TAMARANo ratings yet
- Plasmid-Mediated Resistance - WikipediaDocument16 pagesPlasmid-Mediated Resistance - WikipediaUbaid AliNo ratings yet
- Manuscript v6Document13 pagesManuscript v6João Gabriel SonciniNo ratings yet
- Intestinal colonization with multidrug-resistant enterobacteriaceae in a healthy adult populationDocument8 pagesIntestinal colonization with multidrug-resistant enterobacteriaceae in a healthy adult populationOpenaccess Research paperNo ratings yet
- Pertussis Infection and VaccinesDocument173 pagesPertussis Infection and VaccinesbetsabevegaaNo ratings yet
- University of Michigan Medical School - ... Ral Region and Superficial Back ImagesDocument29 pagesUniversity of Michigan Medical School - ... Ral Region and Superficial Back ImagesjustinNo ratings yet
- University of Michigan Medical School - ... Eled Lumbar Spine, Hip and Knee ImagesDocument21 pagesUniversity of Michigan Medical School - ... Eled Lumbar Spine, Hip and Knee ImagesjustinNo ratings yet
- Chemistry NCA Part 2: Terms in This SetDocument10 pagesChemistry NCA Part 2: Terms in This SetjustinNo ratings yet
- University of Michigan Medical School - Labeled Overview of Upper Limb ImagesDocument23 pagesUniversity of Michigan Medical School - Labeled Overview of Upper Limb ImagesjustinNo ratings yet
- NCA LAB PracticeDocument26 pagesNCA LAB PracticejustinNo ratings yet
- Microbiology Nca-Cls: Terms in This SetDocument18 pagesMicrobiology Nca-Cls: Terms in This SetjustinNo ratings yet
- Chemistry NCA Q's Part 1Document14 pagesChemistry NCA Q's Part 1justinNo ratings yet
- Hemostasis - NCA-CLS Q'S: Terms in This SetDocument10 pagesHemostasis - NCA-CLS Q'S: Terms in This SetjustinNo ratings yet
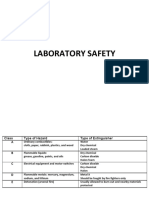
- Lab SafetyDocument5 pagesLab SafetyjustinNo ratings yet
- NCA Immuno PDFDocument19 pagesNCA Immuno PDFjustinNo ratings yet
- DDDDDDDDDDDocument7 pagesDDDDDDDDDDOlga BurduniucNo ratings yet
- ArbovirusDocument1 pageArbovirusjustinNo ratings yet
- Blood Bank Nca-Cls Q'S: Terms in This SetDocument18 pagesBlood Bank Nca-Cls Q'S: Terms in This SetjustinNo ratings yet
- NCA Immuno PDFDocument19 pagesNCA Immuno PDFjustinNo ratings yet
- Dipylidium Caninum Multiceps MulticepsDocument2 pagesDipylidium Caninum Multiceps MulticepsjustinNo ratings yet
- NCA Immuno PDFDocument19 pagesNCA Immuno PDFjustinNo ratings yet
- Lab SafetyDocument5 pagesLab SafetyjustinNo ratings yet
- NCA Immuno PDFDocument19 pagesNCA Immuno PDFjustinNo ratings yet
- ArbovirusDocument1 pageArbovirusjustinNo ratings yet
- Multiceps MulticepsDocument1 pageMulticeps MulticepsjustinNo ratings yet
- ArbovirusDocument1 pageArbovirusjustinNo ratings yet
- HelloDocument1 pageHellojustinNo ratings yet
- Lec 2 Part 2Document34 pagesLec 2 Part 2Ahmed JamalNo ratings yet
- Anti-Infective Agents and Triamsinolon Intravitreal (with cases reportDocument17 pagesAnti-Infective Agents and Triamsinolon Intravitreal (with cases reportMeironiWaimirNo ratings yet
- Beta-lactam antibiotics cell wall synthesis inhibitorsDocument29 pagesBeta-lactam antibiotics cell wall synthesis inhibitorsRen PastelNo ratings yet
- Generics menu card with pricesDocument4 pagesGenerics menu card with pricesChris NicodemusNo ratings yet
- Cefoperazone Sulbactam Injection DetailsDocument3 pagesCefoperazone Sulbactam Injection DetailsPharmaPackaging SolutionsNo ratings yet
- Cell Wall Synthesis Inhibitors - Part 1 AtfDocument4 pagesCell Wall Synthesis Inhibitors - Part 1 AtfJocelyn BelNo ratings yet
- Pure Antibiotic PowderDocument2 pagesPure Antibiotic PowderTitan BiotechNo ratings yet
- 2018 MMC AntibiogramDocument2 pages2018 MMC Antibiogramaman570570No ratings yet
- Book 2Document132 pagesBook 2siti fatimahNo ratings yet
- Cleanroom ClassificationDocument59 pagesCleanroom Classificationabbas aliNo ratings yet
- Beta Lactam AntibioticsDocument94 pagesBeta Lactam AntibioticsHely PatelNo ratings yet
- Drug Study - PiptazDocument1 pageDrug Study - PiptazMutya XDNo ratings yet
- Medication Card Case.2Document6 pagesMedication Card Case.2Jemina Rafanan RacadioNo ratings yet
- Allergic Cross-Reactivity of Select Antimicrobials: Figure: Penicillin Core StructureDocument2 pagesAllergic Cross-Reactivity of Select Antimicrobials: Figure: Penicillin Core StructureAhmad ShokryNo ratings yet
- List of AntibioticsDocument9 pagesList of Antibioticsdesi_mNo ratings yet
- Antimikroba Anti Jamur Antiparasit Antibiotik Antiviral Antimico-Bacterium Antimikosis Antihelmintik Antiamuba AntimalariaDocument22 pagesAntimikroba Anti Jamur Antiparasit Antibiotik Antiviral Antimico-Bacterium Antimikosis Antihelmintik Antiamuba AntimalariaHaris GaulNo ratings yet
- 191119-GCA3076-MS ANITA GAIKWAD-. Antimicrobial Susceptibility Test NEGDocument1 page191119-GCA3076-MS ANITA GAIKWAD-. Antimicrobial Susceptibility Test NEGMohan RadiyaNo ratings yet
- Antibiotic Moa Mor Indication Formulation/ Dose Typical Sensitivities Adverse Effects Interactions Other InfoDocument2 pagesAntibiotic Moa Mor Indication Formulation/ Dose Typical Sensitivities Adverse Effects Interactions Other Infokalli987No ratings yet
- ASTD PRODUCT LIST 2020Document2 pagesASTD PRODUCT LIST 2020midoNo ratings yet
- Antimicrobial AgentDocument46 pagesAntimicrobial Agentسامر الرفاعيNo ratings yet
- Bismillah Laporan Rs FixDocument48 pagesBismillah Laporan Rs FixDian AsriniNo ratings yet
- Cephalosporins in Animals - DosagesDocument7 pagesCephalosporins in Animals - DosagesSunilNo ratings yet
- 1 Classification of The AntibioticsDocument5 pages1 Classification of The AntibioticsRahma WatiNo ratings yet
- Culture Aerobic: Final Laboratory ReportDocument3 pagesCulture Aerobic: Final Laboratory Reportdr.diagnostics.labNo ratings yet
- Cell Wall Inhibitors - Pharmacology 3 - Frank SsengoobaDocument16 pagesCell Wall Inhibitors - Pharmacology 3 - Frank SsengoobaVhugala AudreyNo ratings yet
- Consum Ab Pacienti 2021Document399 pagesConsum Ab Pacienti 2021nicoletagenovevaNo ratings yet
- Daftar Dosis Dan Sediaan Obat AnakDocument5 pagesDaftar Dosis Dan Sediaan Obat AnakDaman Gregorius ManikNo ratings yet
- Antibiotic Approval TimelineDocument1 pageAntibiotic Approval TimelineMartin CuellarNo ratings yet
- Saldo Penerimaan & Pengeluaran07 - JANUARI - 2021Document32 pagesSaldo Penerimaan & Pengeluaran07 - JANUARI - 2021Desi Yuliana HarahapNo ratings yet
- CephalosporinDocument35 pagesCephalosporinGavin BirlaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (14)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (327)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)