Professional Documents
Culture Documents
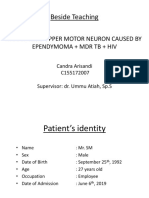
Multifocal Intradural Extramedullary Epe
Uploaded by
Bochand CoolCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Multifocal Intradural Extramedullary Epe
Uploaded by
Bochand CoolCopyright:
Available Formats
DOI: 10.3171/2010.9.
SPINE09963
Multifocal intradural extramedullary ependymoma
Case report
Eduardo Augusto Iunes, M.D.,1 João Norberto Stávale, M.D., Ph.D., 2
Rita de Cássia Caldas Pessoa, M.D., 3 Ricardo Ansai, M.D.,1 Franz Jooji Onishi, M.D.,1
Manoel Antonio de Paiva Neto, M.D., Ph.D.,1 Antônio de Pádua Bonatelli, M.D., Ph.D.,1
Sérgio Cavalheiro, M.D., Ph.D.,1 and Suzana M. Fleury Malheiros, M.D., Ph.D.1
Departments of 1Neurology and Neurosurgery, 2Pathology, and 3Radiology, Universidade Federal de São
Paulo, Brazil
In this paper, the authors present the case of a patient with multifocal intradural extramedullary ependymoma,
and they review 18 previously reported cases.
A 32-year-old man presented to the authors’ institution with a 1-month history of partial medullary syndrome.
Magnetic resonance imaging of the neuraxis revealed multifocal intradural extramedullary lesions at the bulbomed
ullary junction and C2–3, T5–11, L-2, L-4, L-5, and sacrum. Histological examination revealed a WHO Grade II
ependymoma.
The literature survey yielded 18 cases of ependymoma at the same location; none of them were multifocal at
presentation. The authors analyzed the epidemiological, clinical, and surgical features of all 19 cases reported to date,
including the present case.
Patients’ ages ranged from 24 to 69 years; 15 patients were women and 4 were men. The time elapsed from
symptom onset to diagnosis ranged from 1 month to 8 years. Pain (in 13 patients) and medullary syndrome (in 12)
were reported as the initial symptoms (information was not provided for 1 patient). Tumors were predominantly
located in the thoracic spine (11), but they also occurred in the cervicothoracic (3), cervical (2), and lumbar (2)
spine. The remaining tumor was multifocal. Solitary extramedullary tumors were found intraoperatively in 13 pa
tients; 3 were described as exophytic and 3 as extramedullary with some degree of medullary invasion. Histological
examination revealed 9 WHO Grade II tumors, 4 Grade III tumors, and 1 myxopapillary tumor. Data obtained for
the remaining cases proved inconclusive. The clinical condition improved in 11 patients, remained stable in 2, and
worsened (recurrence or progression) in 6. Of the 4 patients with Grade II tumors who presented with recurrence or
neuraxis spreading, 3 had meningeal infiltration or adhesion to the pia mater, which does not rule out the possibility
of neoplastic remnants in that area.
Intradural extramedullary ependymomas are rare, they predominate in women in the 5th decade of life, and pain
is the most frequent initial symptom. The extent of resection and the presence of meningeal infiltration seem to be key
determinants of prognosis. The present case is the first intradural extramedullary ependymoma (with the exception of
those occurring at the conus medullaris and terminal filum) with multiple lesions at presentation.
(DOI: 10.3171/2010.9.SPINE09963)
Key Words • ependymoma • extramedullary ependymoma •
intradural ependymoma • multifocal ependymoma
S
pinal cord tumors can be classified as extradural lary tumors and occur predominantly in adults. The re
(55%) or intradural (45%), the latter being either in ported cranial/spinal tumor ratio for ependymomas is
tramedullary (5%) or extramedullary (40%).22 Neuro 4:1, ranging from 3:1 to 20:1, depending on histological
fibromas, neuromas, and meningiomas account for roughly subtype.18,19,22 Intradural extramedullary ependymomas
60% of intradural extramedullary tumors and affect mainly are extremely rare except for those located at the termi
adults, whereas intramedullary tumors are more common nal filum or conus medullaris.20,22 An extensive literature
in children. Ependymomas and astrocytomas are the main survey yielded 18 such cases.3,5–7,9–14,17,21,23,24,27,29,31 The
histological diagnoses in the children.22 present study reports the 19th case and reviews all cases
Ependymomas are the most common intramedul described to date.
J Neurosurg: Spine / December 10, 2010 1
E. A. Iunes et al.
Fig. 1. Sagittal T2-weighted (A and C) and fat-suppressed, postcontrast T1-weighted (B and D) MR images of the cervicotho-
racic region demonstrating multiple intradural extramedullary lesions in the bulbomedullary junction, C2–3, and T6–11 with high
signal intensity on the T2-weighted images, cystic areas, and moderate and heterogeneous enhancement. Note the irregular and
thickened enhancement outlining the posterior surface of spinal cord.
Case Report
History and Examination. This 32-year-old man pre
sented with progressive paresthesia in the lower limbs,
gait disturbance, and urinary retention during the preced
ing month. Neurological examination showed hypesthe
sia at the T-9 level, lower-limb hyperreflexia, Romberg
sign, and calcaneal gait. Muscle strength was preserved.
Initial spinal MR imaging revealed multiple intradural
extramedullary lesions in the bulbomedullary junction
and C2–3, T5–11, L-2, L-4, L-5, and sacrum that were
predominantly isointense on T1-weighted images and
hyperintense on T2-weighted and FLAIR images, with
moderate contrast enhancement (Figs. 1 and 2). Cranial
MR imaging showed an interpeduncular nodular lesion
with mild contrast enhancement (Fig. 3).
Operation. A T7–9 laminectomy was performed at the
site of the major compression of the spinal cord according
to the MR imaging findings. A brownish intradural extra
medullary tumor compressing the spinal cord posteriorly
was immediately apparent after opening the dura. Under
microscopic assistance, no attachment of the tumor to the
dura or spinal cord was observed, but arachnoid infiltra
tion was noted. The tumor was soft. After internal debulk
ing of the lesion, a sharp dissection at the tumor–spinal
cord interface was performed, and the tumor was resected.
Because of the multifocal characteristic of the lesion and Fig. 2. Sagittal fat-suppressed postcontrast T2-weighted (left) and
T1-weighted (right) MR images of the lumbar spine demonstrating in-
arachnoidal infiltration, the aim of the surgery was spinal tradural and extramedullary entities appearing as cervicothoracic le-
cord decompression instead of total resection. The histo sions at the level of L-4 and L-5. Superficial enhancement is observed
logical examination revealed a WHO Grade II ependy in the conus medullaris.
2 J Neurosurg: Spine / December 10, 2010
Multifocal intradural extramedullary ependymoma
Fig. 3. Postcontrast FLAIR (left) and T1-weighted (right) MR imag-
es of the brain showing an interpeduncular nodular lesion hyperintense
on the FLAIR image and with mild contrast enhancement.
moma with hypercellular nodules showing a Ki 67 index
of 10% (Fig. 4).
Postoperative Course. Postoperatively, the patient de
veloped a transient motor deficit (strength 4/5 in the ilio
psoas, quadriceps, tibialis anterior, extensor hallucis lon Fig. 4. Photomicrographs showing a moderately cellular ependymo-
gus, and gastrocnemius muscles). He was able to stand on ma with a monomorphic nuclear morphology and a perivascular pseu-
his own and walk with assistance. The patient received ad dorosette (A), perivascular pseudorosette (B), increased cellularity and
juvant chemotherapy consisting of 4 cycles of carboplatin pleomorphic area with 1 mitosis (C), and ependymal rosette (D). H & E,
(175 mg/m2/week for 4 weeks), followed by a 2-week break, original magnification × 100 (A and B); × 400 (C and D).
without objective response.
Ten months after surgery, the patient presented with Patients’ ages ranged from 24 to 69 years, a range similar
progressive paraparesis. He underwent a partial resection to that described for intramedullary cases, with predomi
of the intradural extramedullary lesion between T-9 and nance in the 5th decade of life.20,22
T-10, which adhered to nerve roots without medullary in The initial symptoms were pain in 13 patients and
vasion. Histological examination again revealed a WHO medullary syndrome (with motor and/or sensory and/or
Grade II ependymoma. Regarding the intracranial lesion, sphincter control deficit) in 12 (data were not available for
it was never biopsied, but it was assumed to have the same 1 patient). Dorsalgia and radicular pain are the most fre
histology because of the similarity of the MR imaging quently reported clinical symptoms, regardless of com
characteristics. The tumor remained stable during follow- partment (intra- or extradural) or histological subtype.22
up. The patient underwent radiotherapy at 39.5 Gy (whole Intradural extramedullary ependymomas tend to follow
brain) and 36 Gy (neuraxis), but no objective response the same pattern, with pain being reported as the earliest
ensued. He refused further chemotherapy and 8 months symptom in the majority of cases described (13 [72.2%]
later developed a complete spinal cord syndrome and of 18 cases).
septic shock due to a urinary tract infection. The overall The time elapsed from symptom onset to diagnosis
survival was 105 weeks. ranged from 1 month to 8 years. The time interval from
the first clinical manifestation to diagnosis was less than
Discussion 1 year in most cases (12 [66.7%] of 18 cases). Diagno
sis was delayed in some patients because of the lack of
We found 17 publications reporting 18 patients with available MR imaging at the time. Among the patients
intradural extramedullary ependymoma (2 of them were reported on after the advent of MR imaging, only 2 were
reported in a single publication by Hentschel et al.13). Ta diagnosed later than 1 year. Graça et al.12 reported on a
ble 1 shows the demographic, clinical, and follow-up data 67-year-old woman who presented with foot numbness
of all patients, including the patient in the present report. that was initially diagnosed as peripheral neuropathy.
Of the 19 patients, 15 were women and 4 were men. The definitive tumor diagnosis was reached 2 years after
A higher incidence among women has been observed in the initial symptom. Katoh et al.14 reported on a 24-year-
earlier studies.9,12 In a review paper of intradural extra old woman presenting with sporadic dorsalgia. Magnetic
medullary ependymomas, Duffau et al.9 postulated that resonance imaging was performed 3 years later, on mani
a hormonal factor was involved. The higher prevalence festation of clinical features of medullary compression.
among females does not match epidemiological data on Magnetic resonance imaging is the gold standard
spinal tumors, which affect males and females at simi for diagnosing spinal tumors. Ependymomas usually en
lar rates, except for meningiomas, which are more com hance uniformly after Gd administration.16,28 Tumor loca
monly found among females, and intramedullary epen tion was distributed as follows: cervical in 2 patients, cer
dymomas, which are more prevalent among males.18,19,22 vicothoracic in 3, thoracic in 11, lumbar in 2, and multiple
J Neurosurg: Spine / December 10, 2010 3
E. A. Iunes et al.
TABLE 1: Summary of the cases reported*
Clinical Duration of
Authors & Year Age, Sex (yrs) Features Symptoms (wks) Site Intraop WHO Grade Clinical Course Follow-Up (wks)
Cooper et al., 1951 40, F pain, MS 156 T EM/TR I† disease free 106
Cheng et al., 1996 47, F MS 34 T exo/TR myxo disease free NR
González et al., 1971 43, F MS 416 T EM/TR II disease free NR
Katoh et al., 1995 24, F pain 156 CT EMA/TR III disease free 26
Li & Holtås, 1992 NR, F NR NR L EM NR disease free NR
Oliver et al., 1981 34, F pain, MS 260 T EM III disease free 13
Wagle et al., 1988 41, F pain 52 T EMA/TR II† disease free NR
Wolfla et al., 1997 69, F pain 26 T EM/TR II† disease free 27
Duffau et al., 2000 43, F pain, MS 52 T EM/TR II disease free 106
Robles et al., 2005 47, F MS subacute T EM/TR II recurrence 98
Payer et al., 1999 62, F pain 39 T EM/TR II disease free NR
Shuurmans et al., 2006 29, F pain, MS 17 C EMA/TR III recurrence & death 106
Fuentes Rodríguez et al., 2004 47, F pain 78 L EM/TR II disease free NR
Cerase et al., 2006 56, M pain, MS 8 T EM/TR III recurrence & death 57
Graça et al., 2006 67, F MS 104 T EM/TR II recurrence 56
Hentschel et al., 2004 37, M pain, MS 17 CT exo/TR II stable disease 6
51, F pain 52 CT exo/TR II stable disease 2
Benzagmout et al., 2008 31, M pain, MS 52 C EM/TR II† recurrence NR after relapse
present case 32, M MS 4 ML EM/PR II progression & death 105
* C = cervical; CT = cervicothoracic; EM = extramedullary; EMA = extramedullary with adhesion; exo = exophytic; L = lumbar; ML = multiple locations;
MS = medullary syndrome; myxo = myxopapillary; NR = not reported; PR = partial resection; T = thoracic; TR = total resection.
† These grades are probable grades.
in 1 patient (present case).3,5–7,9–14,17,21,23,24,27,29,31 In contrast sion might go undetected, particularly if partial resection
to intramedullary ependymomas that clearly tend to de is considered.
velop at the cervical medulla,19,20 the predominance of the Clinical improvement and local control occurred in 11
thoracic location was noteworthy in the present review. patients,6,7,9–11,14,17,21,23,29,31 5 of whom were followed up for
Three of 5 tumors with cervical involvement extended 13–106 weeks.7,9,14,21,31 Data on follow-up were not available
into the thoracic region (cervicothoracic tumors). This for 6 patients.6,10,11,17,23,29 Two patients remained stable, al
observation may suggest that they might actually be cer though the follow-up extended for only 2 and 6 weeks.13
vical intramedullary tumors (more prevalent) with extra Including the patient in the present case, recurrence or
medullary extension. The present case is the first of an progression occurred in 6 patients as follows:3,5,12,24,27 1
intradural extramedullary ependymoma (except for those patient developed distant spinal metastasis,24 2 had local
occurring in the conus medullaris and terminal filum) recurrence and distant spinal metastasis,5,12 1 had local re
with multiple lesions at presentation. This presentation currence and cerebellar metastasis,3 and 1 had spinal and
had been previously described in myxopapillary ependy intracranial metastases.27 The patient in the present case
momas.30 presented with multiple lesions at diagnosis. Three pa
Intraoperative reports described exophytic tumors tients, including the one in the present case, died of disease
in 3 cases (treated with total resection), extramedullary progression.5,27
tumors with some degree of medullary involvement in Histologically, 9 ependymomas were classified as
3 cases (treated with total resection), and 13 tumors de WHO Grade II, 1 was described as myxopapillary de
scribed as exclusively extramedullary (of which 10 were spite the thoracic location, 4 were anaplastic (Grade III),
treated with total resection and 1 with partial resection; 3 were “probable” Grade II tumors, and 1 was a probable
in 2 cases the extent of resection was not specified). In the Grade I ependymoma. The descriptions available were
present case, the tumor was exclusively extramedullary, not detailed for the last 4 cases.
but it infiltrated the arachnoid membrane. Graça et al.12 Higher-grade gliomas are more prevalent in the ce
reported a similar case of a Grade II tumor treated using rebral parenchyma, whereas lower-grade gliomas pre
gross-total resection. The tumor presented with a “pachy vail in the medulla.22 The present review showed a clear
meningitis” that might have been attributable to neoplas predominance of low-grade ependymomas. Histological
tic infiltration and contributed to the poor outcome as grade does not seem to be the major determinant of clini
observed in our patient. Finally, the true value of the sur cal outcome. Of the 6 cases with poor outcome,3,5,12,24,27
geon’s intraoperative observation should be emphasized, that is, those with recurrence or neuraxis spreading, only
since minimal medullary connections or arachnoid inva 2 had histological features of anaplastic ependymoma.5,27
4 J Neurosurg: Spine / December 10, 2010
Multifocal intradural extramedullary ependymoma
The 3 patients with WHO Grade II tumors with unfavor The thoracic location is the most common site for ex
able outcome warrant further evaluation. The patient re tramedullary ependymomas, unlike intramedullary ep
ported by Robles et al.24 underwent gross-total resection endymomas, which are mostly cervical. Multifocal pre
of an anterolateral tumor, yet the authors reported adhe sentation at diagnosis had not been previously described.
sion to the pia mater, which does not rule out the possibil The prognosis seems to be related to the extent of resec
ity of neoplastic remnants in that area. The local recur tion and the presence of meningeal infiltration.
rence was located in the posterior region, and histological
examination showed a Grade III ependymoma. Taking Disclosure
into account that the lesion was only partially resected, a
sampling error might be inferred (the pial portion might The authors report no conflict of interest concerning the mate
rials or methods used in this study or the findings specified in this
be a Grade III ependymoma). The patient reported on by paper.
Graça et al.12 presented with recurrence and spinal me Author contributions to the study and manuscript prepara
tastasis, but the tumor remained classified as a Grade II tion include the following. Conception and design: Malheiros.
tumor. An “important arachnoid inflammatory reaction” Acquisition of data: Iunes, Stávale, Pessoa. Analysis and interpreta
was also described, which might characterize a neoplastic tion of data: Iunes, Stávale, Pessoa, Neto. Drafting the article: Iunes,
infiltration and actually a partial resection, accounting for Neto, Malheiros. Critically revising the article: Neto, Malheiros.
the unfavorable outcome. The patient in the present case Reviewed final version of the manuscript and approved it for
submission: all authors. Administrative/technical/material support:
also had a WHO Grade II ependymoma. The pachymen Ansai, Onishi. Study supervision: Bonatelli, Cavalheiro, Neto, Mal
ingitis observed during surgery might in fact have been heiros.
tumoral infiltration that led to sampling errors. However,
the clinical feature of dissemination at presentation was References
irrefutable and may also have been associated with the
1. Anglade MP: Le gliome des fosses nasales. Étude clinique et
unfavorable outcome. The patient described by Benzag anatomo-pathologique. Presse Med 28:464, 1920
mout et al.3 also had a poor outcome with cerebellar 2. Bailey OT: Relation of glioma of the leptomeninges to neuro
metastasis and local recurrence. The tumor was initially glia nests: report of a case of astrocytoma of the leptomenin
classified as a “benign ependymoma,” and the authors did ges. Arch Path 21:584–600, 1936
not report on the follow-up after recurrence. 3. Benzagmout M, Boujraf S, Oulali N, Chbani L, Amarti A,
Two patients with WHO Grade III ependymomas Chakour K, et al: Intradural extramedullary ependymoma: is
with a favorable outcome were described by Katoh et al.14 there constantly a hormonal relationship? Surg Neurol 70:
and Oliver et al.21 However, the follow-up reported was 536–538, 2008
4. Browder J: Encephaloma or the so-called nasal glioma. Ann
short (only 26 and 13 weeks, respectively). Otol Rhinol Laryngol 38:395–403, 1929
The origin of intradural extramedullary ependy 5. Cerase A, Venturi C, Oliveri G, De Falco D, Miracco C: In
moma has been attributed to the presence of heterotopic tradural extramedullary spinal anaplastic ependymoma. Case
glial cells, since the earliest report by Cooper et al.7 This illustration. J Neurosurg Spine 5:476, 2006
observation implies the occurrence of invagination of the 6. Cheng CH, Lee TC, Huang HY, Lui CC: Extramedullary tho
neuraxis into the extramedullary space, evidenced by an racic myxopapillary ependymoma—a case report of a rare tu
encapsulated appearance (encapsulation by pia mater and mour. Ann Acad Med Singapore 25:869–872, 1996
7. Cooper IS, Craig WM, Kernohan JW: Tumors of the spinal
arachnoid membrane) and absence of medullary connec cord; primary extramedullary gliomas. Surg Gynecol Obstet
tion. These cells evolve to a tumor within the intradural 92:183–190, 1951
extramedullary space. The same hypothesis has been pro 8. Crook M: Congenital ganglio-neuroma of nose, report of a
posed to explain the origin of gliomas occurring outside case. J S Carolina Med Assoc 36:159–160, 1940
the neuraxis, including nasal and sacral gliomas.1,2,4,8,15,25,26 9. Duffau H, Gazzaz M, Kujas M, Fohanno D: Primary intradu
The presence of a medullary connection does not rule out ral extramedullary ependymoma: case report and review of
the hypothesis of an intramedullary tumor extending to the literature. Spine 25:1993–1995, 2000
the extramedullary compartment. Identification of exclu 10. Fuentes Rodríguez N, de la Paz Rivero M, Prince López JA,
Salas Rubio JH: Ependimoma intradural extramedular prima
sively extramedullary cases can be biased by subjective rio. Rev Cuba Med Mil 33, 2004 (http://scielo.sld.cu/scielo.
interpretation and by the resolution of surgical micro php?script=sci_arttext&pid=S0138-65572004000100009&ln
scopes, making it difficult to rule out medullary connec g=en&nrm=iso) [Accessed October 27, 2010]
tion. From a practical standpoint, however, all the cases 11. González Feria L, Fernández Martín F, Ginovés Sierra M,
reported appeared as intradural and extramedullary le Galera Davidson H: [Giant dorsal extramedullary ependymo
sions on the images, and the importance of these reports ma.] Arch Neurobiol (Madr) 34:325–332, 1971 (Spn)
may lie in considering ependymomas, although rare, as a 12. Graça J, Gültasli N, D’Haene N, Brotchi J, Salmon I, Balériaux
differential diagnosis of tumors at this location. D: Cystic extramedullary ependymoma. AJNR Am J Neuro
radiol 27:818–821, 2006
13. Hentschel SJ, McCutcheon IE, Ginsberg L, Weinberg JS: Ex
Conclusions ophytic ependymomas of the spinal cord. Acta Neurochir
Intradural extramedullary ependymomas are ex (Wien) 146:1047–1050, 2004
14. Katoh S, Ikata T, Inoue A, Takahashi M: Intradural extramedul
tremely rare and predominate in women in the 5th decade lary ependymoma. A case report. Spine 20:2036–2038, 1995
of life. Pain is the most frequent initial symptom, akin to 15. Kernohan JW, Fletcher-Kernohan EM: Ependymomas: a study
other tumors of the medullary canal. Magnetic resonance of 109 cases. Assoc Res Nerv Ment Dis 16:182–209, 1937
imaging of the entire neuraxis is essential to rule out in 16. Li MH, Holtås S: MR imaging of spinal intramedullary tu
tracranial ependymomas with metastasis to the neuraxis. mors. Acta Radiol 32:505–513, 1991
J Neurosurg: Spine / December 10, 2010 5
E. A. Iunes et al.
17. Li MH, Holtås S, Larsson EM: MR imaging of intradural ex 27. Schuurmans M, Vanneste JAN, Verstegen MJT, van Furth WR:
tramedullary tumors. Acta Radiol 33:207–212, 1992 Spinal extramedullary anaplastic ependymoma with spinal and
18. McCormick PC, Post KD, Stein BM: Intradural extramedullary intracranial metastases. J Neurooncol 79:57–59, 2006
tumors in adults. Neurosurg Clin N Am 1:591–608, 1990 28. Sun B, Wang C, Wang J, Liu A: MRI features of intramedul
19. McCormick PC, Stein BM: Intramedullary tumors in adults. lary spinal cord ependymomas. J Neuroimaging 13:346–351,
Neurosurg Clin N Am 1:609–630, 1990 2003
20. McCormick PC, Torres R, Post KD, Stein BM: Intramedul 29. Wagle WA, Jaufman B, Mincy JE: Intradural extramedullary
lary ependymoma of the spinal cord. J Neurosurg 72:523– ependymoma: MR-pathologic correlation. J Comput Assist
532, 1990 Tomogr 12:705–707, 1988
21. Oliver B, de Castro A, Sarmiento MA, Argüello C, Blaźquez 30. Woesler B, Moskopp D, Kuchelmeister K, Schul C, Wassmann
MG: [Dorsal extramedullary ependymoma (author’s transl).] H: Intracranial metastasis of a spinal myxopapillary ependy
Arch Neurobiol (Madr) 44:215–224, 1981 (Spn) moma. A case report. Neurosurg Rev 21:62–65, 1998
22. Parsa AT, Lee J, Parney IF, Weinstein P, McCormick PC, 31. Wolfla CE, Azzarelli B, Shah MV: Primary extramedullary
Ames C: Spinal cord and intradural-extraparenchymal spinal ependymoma of the thoracic spine. Case illustration. J Neu
tumors: current best care practices and strategies. J Neuroon rosurg 87:643, 1997
col 69:291–318, 2004
23. Payer M, Yonekawa Y, Imhof HG: Solitary thoracic intradu
ral extramedullary ependymoma. J Clin Neurosci 6:344–345,
1999 Manuscript submitted December 8, 2009.
24. Robles SG, Saldaña C, Boto GR, Martinez A, Zamarron AP, Accepted September 22, 2010.
Jorquera M, et al: Intradural extramedullary spinal ependy Please include this information when citing this paper: published
moma: a benign pathology? Spine 30:E251–E254, 2005 online December 10, 2010; DOI: 10.3171/2010.9.SPINE09963.
25. Rocher HL, Anglade M: Les fibrogliomes de la région nasale. Address correspondence to: Eduardo Augusto Iunes, M.D.,
Rev Chir 62:147–178, 1924 Department of Neurology and Neurosurgery, Universidade Federal
26. Roussy G, Cornil L: Les tumeurs méningées. Ann d’Anat de São Paulo, Rua Napoleão de Barros, 715/6th floor, São Paulo, SP,
Path 2:63–79, 1925 Brazil, 04024002. email: eaiunes@ig.com.br.
6 J Neurosurg: Spine / December 10, 2010
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Epilepsy Syndrome in Childhood HalDocument3 pagesEpilepsy Syndrome in Childhood HalBochand CoolNo ratings yet
- Rangkuman Judul Stase EpilepsiDocument2 pagesRangkuman Judul Stase EpilepsiBochand CoolNo ratings yet
- Rawon - Primer of Eeg HalDocument5 pagesRawon - Primer of Eeg HalBochand CoolNo ratings yet
- Brain Abscess: JUNE 2020Document38 pagesBrain Abscess: JUNE 2020Bochand CoolNo ratings yet
- NeuropatiDocument19 pagesNeuropatiBochand CoolNo ratings yet
- Sweeping PENJARINGAN TAHUN 2019Document3 pagesSweeping PENJARINGAN TAHUN 2019Bochand CoolNo ratings yet
- Case Infeksi FixDocument14 pagesCase Infeksi FixBochand CoolNo ratings yet
- Paraparesis Upper Motor Neuron Caused by EpendymomaDocument17 pagesParaparesis Upper Motor Neuron Caused by EpendymomaBochand CoolNo ratings yet
- Metlit Bab IIIDocument18 pagesMetlit Bab IIIBochand CoolNo ratings yet
- European Journal of Internal Medicine: Morohunfolu E. Akinnusi, Ranime Saliba, Jahan Porhomayon, Ali A. El-SolhDocument8 pagesEuropean Journal of Internal Medicine: Morohunfolu E. Akinnusi, Ranime Saliba, Jahan Porhomayon, Ali A. El-SolhBochand CoolNo ratings yet
- Surgical Treatment of Primary Intramedullary MSDocument9 pagesSurgical Treatment of Primary Intramedullary MSBochand CoolNo ratings yet
- Spinal Cord EpendyomasDocument3 pagesSpinal Cord EpendyomasBochand CoolNo ratings yet
- Van Esch 2016Document9 pagesVan Esch 2016Bochand CoolNo ratings yet
- Minocycline Prevents The Development of DepressionDocument7 pagesMinocycline Prevents The Development of DepressionBochand CoolNo ratings yet
- Paraparesis Upper Motor Neuron Caused by EpendymomaDocument16 pagesParaparesis Upper Motor Neuron Caused by EpendymomaBochand CoolNo ratings yet
- Antibiotic Could Protect Against Neurodegenerative Diseases During AgingDocument9 pagesAntibiotic Could Protect Against Neurodegenerative Diseases During AgingBochand CoolNo ratings yet
- BSTDocument1 pageBSTBochand CoolNo ratings yet
- Proposal T NHDocument6 pagesProposal T NHBochand CoolNo ratings yet
- Goila2009 The Diagnosis of Brain Death PDFDocument6 pagesGoila2009 The Diagnosis of Brain Death PDFBochand CoolNo ratings yet
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Higher Algebra - Hall & KnightDocument593 pagesHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Rehabilitation Team Approach: Amputee PatientDocument35 pagesRehabilitation Team Approach: Amputee Patientwww_wadtulesh27No ratings yet
- Differential Diagnostic by P'nutDocument141 pagesDifferential Diagnostic by P'nutRotate E100% (1)
- Conversion Disorder BrochureDocument2 pagesConversion Disorder BrochurerobktfNo ratings yet
- Penatalaksanaan Keperawatan Covid 19 Di Respiratory Ward AustraliaDocument22 pagesPenatalaksanaan Keperawatan Covid 19 Di Respiratory Ward AustraliaRadenroro Atih Utari RizkyNo ratings yet
- DCTMDDocument58 pagesDCTMDHanzara PanolNo ratings yet
- CBT For Tinnitus (20 Nov 2023)Document48 pagesCBT For Tinnitus (20 Nov 2023)agietz27No ratings yet
- Scientific Research For DiabtiesDocument18 pagesScientific Research For DiabtiesSubhana HashmiNo ratings yet
- AngioplastyDocument10 pagesAngioplastyВлада ХоружийNo ratings yet
- Hallucinations and Hearing VoicesDocument4 pagesHallucinations and Hearing VoicesCazacu ParascoviaNo ratings yet
- C Ovid 19 Treatment GuidelinesDocument274 pagesC Ovid 19 Treatment Guidelinesrenugadevi_dNo ratings yet
- CortisolDocument2 pagesCortisolkitu_alagappan4720No ratings yet
- Meningocele & Spina BifidaDocument20 pagesMeningocele & Spina BifidaAstrid SabirinNo ratings yet
- Management of Asthma: A Guide To The Essentials of Good Clinical PracticeDocument100 pagesManagement of Asthma: A Guide To The Essentials of Good Clinical Practicemalvika chawlaNo ratings yet
- 2012 NCCAOM Herbal Exam QuestionsDocument10 pages2012 NCCAOM Herbal Exam QuestionsElizabeth Durkee Neil100% (2)
- P LCR Parameter Platelet Large Cell Ratio Medical Laboratories PDFDocument3 pagesP LCR Parameter Platelet Large Cell Ratio Medical Laboratories PDFluxsura8217No ratings yet
- ATLS Chapter Review QuestionsDocument36 pagesATLS Chapter Review QuestionsKen Evans89% (57)
- Enhanced Recovery After Cesarean Delivery Role.2Document6 pagesEnhanced Recovery After Cesarean Delivery Role.2Kirin PorNo ratings yet
- Protein-Losing Enteropathy: Francisco A. SylvesterDocument10 pagesProtein-Losing Enteropathy: Francisco A. SylvesterNIKEN PUSPITASARINo ratings yet
- GoodPractice WL U02PresentingComplaint PDFDocument4 pagesGoodPractice WL U02PresentingComplaint PDFFlorina TrutescuNo ratings yet
- First Term QuizDocument22 pagesFirst Term QuizJaylord VerazonNo ratings yet
- Knowledge Regarding Prevention of Helminthic Disease Among School ChildrenDocument5 pagesKnowledge Regarding Prevention of Helminthic Disease Among School ChildrenIJAR JOURNALNo ratings yet
- Gambaran Dari: Acute Kidney Injury (Aki) : Dr. Hasan BasriDocument22 pagesGambaran Dari: Acute Kidney Injury (Aki) : Dr. Hasan BasriLiana Ika SuwandyNo ratings yet
- Antidepressant and Antipsychotic Side-Effects and Personalised Prescribing, A Systematic Review and Digital Tool Development. Lancet 2023Document17 pagesAntidepressant and Antipsychotic Side-Effects and Personalised Prescribing, A Systematic Review and Digital Tool Development. Lancet 2023tomil.hoNo ratings yet
- Week 06 - Antiparkinsonism AgentsDocument18 pagesWeek 06 - Antiparkinsonism AgentsDino MicaNo ratings yet
- Endemic and Sporadic GoiterDocument13 pagesEndemic and Sporadic GoiterBtwo SoelNo ratings yet
- Virus & Antiviral Drugs: Prof. Dr. Ishrat ImranDocument57 pagesVirus & Antiviral Drugs: Prof. Dr. Ishrat Imransomi shaikh100% (1)
- Diseases of The Hepatobiliary System in ChildrenDocument53 pagesDiseases of The Hepatobiliary System in ChildrenМарьяна РизничукNo ratings yet
- Iv InfusionDocument22 pagesIv Infusion1130119008 SARTIKA SARINo ratings yet
- Per-Pl 206Document266 pagesPer-Pl 206Wan YusufNo ratings yet
- Intro To EPDocument48 pagesIntro To EPusfcards100% (2)