Professional Documents
Culture Documents
Acute Kidney Injury: Annals of Internal Medicine
Acute Kidney Injury: Annals of Internal Medicine
Uploaded by
Charly ValderramaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Kidney Injury: Annals of Internal Medicine
Acute Kidney Injury: Annals of Internal Medicine
Uploaded by
Charly ValderramaCopyright:
Available Formats
Annals of Internal Medicine䊛
In the Clinic®
Acute Kidney Injury
A
cute kidney injury is a heterogeneous group
Screening and Prevention
of conditions characterized by a sudden de-
crease in glomerular filtration rate, mani-
fested by an increase in serum creatinine concentra-
tion or oliguria, and classified by stage and cause. Diagnosis
This type of injury occurs in approximately 20% of
hospitalized patients, with major complications in-
cluding volume overload, electrolyte disorders, ure- Treatment
mic complications, and drug toxicity. Management
includes specific treatments according to the under-
lying cause and supportive treatment to prevent and
manage complications. Kidney replacement therapy
is used when complications cannot be managed
with medical therapy alone. Despite advances in
care, the mortality rate in patients requiring kidney
replacement therapy remains approximately 50%.
CME/MOC activity available at Annals.org.
Physician Writers doi:10.7326/AITC201711070
Andrew S. Levey, MD
Matthew T. James, MD CME Objective: To review current evidence for screening, prevention, diagnosis, and
From Tufts Medical Center, treatment of acute kidney injury.
Boston, Massachusetts; and Funding Source: American College of Physicians.
the University of Calgary,
Calgary, Alberta. Disclosures: Dr. Levey, ACP Contributing Author, reports that he was a member of the KDIGO
Workgroup for the Clinical Practice Guideline on Acute Kidney Injury (published 2012). Dr.
James, ACP Contributing Author, reports grants from Amgen Canada outside the submitted
work. Disclosures can also be viewed at www.acponline.org/authors/icmje
/ConflictOfInterestForms.do?msNum=M17-2010.
Acknowledgment: The authors thank Sara Couture, BS, and Bryan Ma for assistance with
manuscript preparation.
With the assistance of additional physician writers, the editors of Annals of Internal Medi-
cine develop In the Clinic using MKSAP and other resources of the American College of
Physicians.
In the Clinic does not necessarily represent official ACP clinical policy. For ACP clinical
guidelines, please go to https://www.acponline.org/clinical_information/guidelines/.
© 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Acute kidney injury (AKI) is not a mately 50%. AKI may occur in pa-
single disease entity. It is a hetero- tients with or without underlying
geneous group of conditions char- chronic kidney disease (CKD). In-
acterized by a sudden decrease in complete recovery may lead to
glomerular filtration rate (GFR) fol- new onset or worsening of CKD.
lowed by an increase in serum cre- Evaluation and management of
1. Kellum JA, Lameire N, atinine concentration (SCC) or oli- AKI proceed in parallel rather than
Aspelin P. Kidney Disease: guria. AKI generally occurs in the sequentially. The goals are to ap-
Improving Global Out-
comes (KDIGO) Acute setting of acute or chronic illness. It ply specific treatments according
Kidney Injury Work Group.
KDIGO clinical practice affects approximately 20% of hos- to the underlying cause and pro-
guideline for acute kidney pitalized patients, of whom 10% vide supportive care to prevent
injury. Kidney Interna-
tional Supplement 1s. require kidney replacement ther- and treat complications. KRT is
2012;2:1-138. apy (KRT). Recent clinical guide- used when complications of kid-
2. Mehta R, Bagga A, Pati-
bandla R, Chakravarthi R. lines from Kidney Disease Improv- ney failure cannot be managed
Detection and manage-
ment of AKI in the devel- ing Global Outcomes (KDIGO) with medical therapy alone. The
oping world: The 18th define AKI as a subgroup of acute need for nephrologist consultation
Acute Disease Quality
Initiative (ADQI) Interna- kidney diseases and disorders or comanagement depends on
tional Consensus Confer- (AKD), and classify AKI according the stage, cause, and severity of
ence. Kidney International
Reports. 2017;2:515-8. to severity (stages) and cause, complications. This review focuses
3. Susantitaphong P, Cruz
DN, Cerda J, et al; Acute which influence prognosis and on general features of AKI in adults
Kidney Injury Advisory management (1). Major complica- in developed countries, not includ-
Group of the American
Society of Nephrology. tions include volume overload, ing pregnant women or kidney
World incidence of AKI: a electrolyte disorders, uremic com- transplant recipients. AKI is a more
meta-analysis. Clin J Am
Soc Nephrol. 2013;8: plications, and drug toxicity. De- serious problem in developing
1482-93. [PMID:
23744003] spite advances in prevention and countries due to risk factors re-
4. Wonnacott A, Meran S, treatment, the mortality in patients lated to underdevelopment and
Amphlett B, Talabani B,
Phillips A. Epidemiology requiring KRT remains approxi- lack of availability of KRT (2).
and outcomes in
community-acquired ver-
sus hospital-acquired AKI.
Clin J Am Soc Nephrol.
2014;9:1007-14. [PMID: Screening and Prevention
24677557]
5. Wang Y, Wang J, Su T, Which patients are at increased required dialysis. Rates were substantially higher
et al; ISN AKF 0by25 risk for AKI, and how should for patients with CKD. Decreased GFR and pro-
China Consortium.
Community-acquired clinicians identify them? teinuria were independent risk factors. Adjusted
acute kidney injury: a rate ratios were 2.5– 4.4 for patients with GFR
nationwide survey in AKI generally occurs in the set-
China. Am J Kidney Dis. >60 mL/min/1.73 m2 (CKD stages 1–2); 2.3– 8.2
2017;69:647-657. [PMID:
ting of acute and chronic illness, for GFR 45–59 mL/min/1.73 m2 (CKD stage 3a);
28117208] and is common among hospital- 5.6 –13 for GFR 30-44 mL/min/1.73 m2 (CKD
6. James MT, Hemmelgarn
BR, Wiebe N, et al; Alberta ized patients. stage 3b); and 13–19 for GFR 15–29 mL/min/
Kidney Disease Network.
1.73 m2 (CKD stage 4).
Glomerular filtration rate, A systematic review of large cohort studies, pri-
proteinuria, and the inci-
dence and consequences marily among hospitalized patients, con- The Box shows risk factors for AKI.
of acute kidney injury: a ducted between 2004 and 2012, showed sig-
cohort study. Lancet. Acute illness, complications of medi-
2010;376:2096-103. nificant heterogeneity in estimates among
[PMID: 21094997] studies, countries, and clinical settings, and
cations, and medical procedures are
7. Tsai TT, Patel UD, Chang
between adults and children (3). In studies of the most common. Older age and
TI, et al. Validated contem-
porary risk model of acute adults that identified AKI according to the preexisting CKD are the main sus-
kidney injury in patients
undergoing percutaneous KDIGO criteria and staging system, the pooled ceptibility factors. Risk prediction
coronary interventions: incidence rate of AKI was 21.6% (95% CI, instruments are available for some
insights from the National
Cardiovascular Data Regis- 19.3%–24.1%). Approximately 10% required high-risk settings, such as percuta-
try Cath-PCI Registry. J Am dialysis. The highest pooled AKI rate was ob- neous coronary intervention, cardiac
Heart Assoc. 2014;3:
e001380. [PMID: served in critical care settings (32%). In other surgery, liver surgery, and vascular
25516439] studies, among hospitalized patients approxi-
8. Allen DW, Ma B, Leung surgery (7–11).
KC, et al. Risk prediction
mately two thirds of AKI episodes were com-
models for contrast- munity-acquired—the remaining one third AKI is generally asymptomatic, so
induced acute kidney
injury accompanying
were hospital-acquired (4, 5). screening is usually required for
cardiac catheterization:
systematic review and In 1 population-based study (6), the rate of adults detection. The U.S. Preventive Ser-
meta-analysis. Can J Car-
diol. 2017;33:724-736.
with AKI but not CKD who required hospital ad- vices Task Force does not have
[PMID: 28545621] mission was 0.1% per year. Approximately 10% recommendations regarding
姝 2017 American College of Physicians ITC66 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
screening for AKI. KDIGO recom- drugs in patients with CKD, such
mends screening based on stratifi- as nonsteroidal anti-inflammatory Risk Factors for Acute Kidney
cation by risk according to expo- drugs (NSAIDs) and iodinated ra- Injury
sures and susceptibility. Because diocontrast media (contrast-
Exposures
there are few risk prediction instru- induced AKI) (15–17).
ments, we suggest the following Critical illness
approach guided by the clinical Risk for contrast-induced AKI Sepsis
setting. For outpatients with acute seems to be greater after arterial Circulatory shock
illness, measure SCC and calculate than venous administration of
Burns
estimated GFR (eGFR) and com- contrast media. For patients at
increased risk for this disorder, Trauma
pare to previous (“baseline”) val-
ues (12). Remeasure if SCC or KDIGO recommends using either Cardiac surgery (especially
eGFR are abnormal or worse than an iso-osmolal or a low-osmolal with cardiopulmonary bypass)
previous values. The urgency of medium (osmolality 2–3 times Major noncardiac surgery
repeated measurement depends that of plasma) rather than a
Nephrotoxic drugs
on the severity of illness and the high-osmolal contrast medium
(osmolality >4 times that of Iodinated radiocontrast
level of SCC and eGFR; hospital-
agents
ization should be considered. For plasma). IV volume expansion
hospitalized patients, SCC and with either an isotonic sodium chlo- Poisonous plants and animals
eGFR are generally measured on ride or a sodium bicarbonate solu- Susceptibility factors
admission and should be mea- tion should be done rather than no
Volume depletion
sured daily or every other day. For IV volume expansion. Several proto-
cols are available for intra-arterial Older age
patients with critical illness, SCC
and eGFR, as well as urine output, contrast administration, and these Female sex
should be measured at least daily. can be used for high-risk patients Black race
In our experience, accurate mea- receiving IV contrast administration Chronic kidney disease
surement of urine output is diffi- (18–22). Tailoring administration to
Other chronic diseases
cult, unless the patient is in an left ventricular filling pressure can
(heart, lung, liver)
intensive care unit (ICU). In all set- safely facilitate more volume expan-
tings, urinalysis should be done for sion and reduce the incidence of Diabetes mellitus
detection of AKD and CKD. contrast-induced AKI during cardiac Cancer
catheterization (23, 24). A recent Anemia
Increased SCC and oliguria may comparative effectiveness review From reference 1.
not occur for several hours after compares other strategies for pre-
the onset of an acute decline in venting this complication (25, 26).
GFR. Novel biomarkers are under
investigation to determine We also recommend volume ex-
whether they may enable earlier pansion with isotonic sodium chlo-
detection of decreased GFR and ride for other high-risk conditions,
complications of AKI (13, 14). such as cardiac surgery; hemolysis;
rhabdomyolysis; tumor lysis; and
Which measures are useful for
administration of cisplatinum, car-
preventing AKI, and when boplatin, ifosphamide, and am-
9. Wijeysundera DN, Kark-
outi K, Dupuis JY, et al.
should they be used? photericin B. Caution is warranted Derivation and validation
of a simplified predictive
We recommend general measures in patients with volume overload, index for renal replace-
to reduce exposures and suscepti- and IV fluids should be discontin- ment therapy after cardiac
surgery. JAMA. 2007;297:
bility when possible—for example, ued if symptoms of volume over- 1801-9. [PMID:
correcting volume depletion by load develop (see below).
17456822]
10. Wilson T, Quan S,
increasing oral salt and fluid intake Cheema K, et al. Risk
Monitoring therapeutic levels of prediction models for
or intravenous (IV) isotonic saline. acute kidney injury fol-
Other examples are avoiding di- nephrotoxic drugs, such as van- lowing major noncardiac
surgery: systematic re-
uretics and angiotensin-converting comycin, aminoglycosides, and view. Nephrol Dial Trans-
enzyme inhibitors (ACEIs) and calcineurin inhibitors, can reduce plant. 2016;31:231-40.
[PMID: 26705194]
angiotensin-receptor blockers risk for AKI. KDIGO suggests ad- 11. Borthwick E, Ferguson A.
(ARBs) during acute illness to pre- ditional measures to reduce the Perioperative acute kid-
ney injury: risk factors,
vent volume depletion and hypo- risk for nephrotoxicity of amino- recognition, manage-
ment, and outcomes.
tension, and avoiding nephrotoxic glycosides and amphotericin B. BMJ. 2010;341:c3365.
[PMID: 20603317]
7 November 2017 Annals of Internal Medicine In the Clinic ITC67 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Screening and Prevention... AKI generally occurs in the setting of
acute and chronic illness and is common among hospitalized patients.
Older age and CKD are the main susceptibility factors. Measurement of
SCC and eGFR and monitoring during hospitalization are essential to
detect AKI. Urine output should be monitored in patients with critical
illness. Urinalysis is helpful to detect AKD and CKD. General measures
to reduce risk include prevention and treatment of volume depletion
and avoidance of nephrotoxic drugs. IV isotonic fluids before, during,
and after intra-arterial administration of iodinated radiocontrast media
can reduce risk for contrast-induced AKI.
CLINICAL BOTTOM LINE
Diagnosis
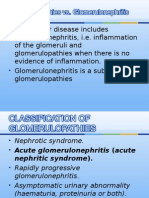
What criteria should clinicians tion based on severity (stages)
use to define and classify AKI? and cause (Figure 2). KDIGO
AKI is a heterogeneous group of definition and staging are
conditions, with a common defi- based on the Risk, Injury, Fail-
nition (Figure 1) and classifica- ure, Loss, End-Stage Renal Dis-
ease (RIFLE) and AKI Network
(AKIN) criteria and studies on
Figure 1. Relationships and definitions of kidney diseases and disorders. risk relationships. The rationale
for defining AKI separately from
other acute kidney diseases and
disorders was to provide a
more rigorous basis for re-
search studies, clinical practice
guidelines, and public health
efforts.
AKD AKI CKD
The KDIGO definition of AKI in-
cludes a change in SCC within
2–7 days and oliguria for 6 or
more hours. The stage is defined
by the peak rise in SCC com-
pared with previous values and
nadir in urine output and is re-
Variable AKI AKD CKD NKD*
Duration Within 7 d ≤3 mo >3 mo lated to risk for complications
Functional Increase in serum AKI GFR <60 GFR ≥60 and prognosis (Figure 2). eGFR
criteria creatinine clearance OR mL/min/1.73 m2 mL/min/1.73 m2 is preferred to SCC for assessing
by ≥50% within 7 d GFR <60
OR mL/min/1.73 m2
GFR in the steady state (i.e.,
Increase in serum OR when GFR is stable) because the
creatinine clearance Decrease in GFR by
by ≥0.3 mg/dL ≥35% times baseline
coefficients for age, sex, and race
within 2 d OR in the estimating equation take
OR Increase in serum into account variation in creati-
Oliguria for ≥6 h creatinine clearance by
≥50% times baseline nine generation by muscle, inde-
Structural Not defined Marker of kidney Marker of kidney No marker of pendent of GFR (12). A 1.5-, 2.0-,
criteria damage damage for >3 mo kidney damage and 3.0-fold increase in SCC dur-
(albuminuria, (albuminuria is most
hematuria, or pyuria common)
ing steady-state conditions re-
is most common) flect a 39%, 57%, and 74% de-
crease in eGFR, respectively.
AKI = acute kidney injury; AKD = acute kidney diseases and disorders; CKD = chronic kidney However, during AKI, SCC may
disease; GFR = glomerular filtration rate; NKD = no kidney disease. be in the nonsteady state, so
* Implies no functional or structural criteria according to the definitions for AKI, AKD, or CKD.
Clinical judgment required for individual patient decision making. changes in SCC and eGFR lag
姝 2017 American College of Physicians ITC68 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
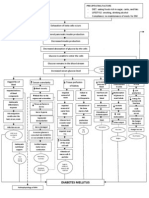
Figure 2. Overview of acute kidney injury.
At Risk Complications
Older age, comorbid conditions, CKD (decreased GFR, albuminuria) Volume overload
Electrolyte disorders
Stage 1 (hyperkalemia, metabolic acidosis,
Serum creatinine: 1.5–1.9 times baseline, or ≥0.3 mg/dL increase, or hyponatremia and hypernatremia,
KDIGO Staging and
urine output: <0.5 mL/kg/h for 6–12 h hypocalcemia and hypercalcemia,
Complications
hyperphosphatemia, hypermagnesemia)
Stage 2
Uremic complications
Serum creatinine: 2.0–2.9 times baseline, or urine output: <0.5 mL/kg/h for ≥12 h
(encephalopathy, pericarditis, pruritus, bleeding)
Stage 3 Drug toxicity
Initiation or renal replacement therapy, or serum creatinine: 3.0 times baseline, or
≥4.0 mg/dL, or urine output: <0.3 mL/kg/h for ≥24 h, or anuria for ≥12 h
Decreased Kidney Obstruction of the Urinary Parenchymal Kidney ATN
Perfusion Tract Diseases Other Than ATN
Causes
Causes Causes Causes Toxic ATN; ischemic ATN
Volume depletion; heart, Obstructive nephropathy Acute glomerulonephritis;
Causes, Clinical Setting and
lung, or liver disease; acute interstitial nephritis; Clinical Setting
Urinary Tract Findings
sepsis; increased intra- Clinical Setting pyelonephritis; thrombotic Circulatory shock; sepsis;
abdominal pressure; renal Urinary tract symptoms; microangiopathy; cast neph- drug exposure; transient
artery stenosis; NSAID history of urolithiasis, ropathy; infarction; hypotension; hemolysis;
toxicity genitourinary tract neoplasia, atheroembolism rhabdomyolysis; tumor lysis
or retroperitoneal disease
Clinical Setting Clinical Setting Urinary Tract Findings
Signs of volume depletion Urinary Tract Findings Systemic diseases; Urine not concentrated
or overload; SIRS; severe Hydronephrosis; relief with microangiopathic hemolysis urine; RTE cells; granular
hypertension urinary catheter casts
Urinary Tract Findings
Urinary Tract Findings Hematuria with RBC casts;
Concentrated urine; no pyuria with WBC casts; RTE
RTE cells or casts cells
Prevention Strategies Nephrologist
Intravenous fluid volume expansion, nephrotoxic medication avoidance, minimization Consultation and Comanagement
of radiocontrast media, hemodynamic monitoring and management Uncertainty about diagnosis
Management
Uncertainty about cause
Early-Stage Management Treatment of parenchymal diseases
Specific therapies and interventions that are dependent on the cause of acute kidney injury. Need for kidney replacement therapy
Intravenous fluid volume resuscitation, vasopressors, therapeutic drug level monitoring,
and adjustment of medication dosing Kidney Replacement Therapy
Volume overload, electrolyte disorders, uremic
Late-Stage Management complications (refractory to medical management)
Supportive care (maintenance of nutrition, electrolyte, and volume balance) and
assessment for complications requiring kidney replacement therapy
ATN = acute tubular necrosis; CKD = chronic kidney disease; GFR = glomerular filtration rate; NSAID = nonsteroidal anti-inflammatory drug;
RBC = red blood cell; RTE = renal tubular epithelial; SIRS = systemic inflammatory response syndrome; WBC = white blood cell.
12. Levey AS, Becker C, Inker
LA. Glomerular filtration
behind changes in GFR, and than 1 cause. Identifying causes rate and albuminuria for
detection and staging of
eGFR may be a less accurate esti- other than ATN is important be- acute and chronic kidney
mate of measured GFR. None- cause specific treatment of other disease in adults: a sys-
tematic review. JAMA.
theless, reporting eGFR in AKI causes can reverse the decline in 2015;313:837-46.
may be useful because changes GFR, whereas treatment for ATN [PMID: 25710660]
13. Kimmel M, Shi J, Latus J,
in eGFR show the direction and is supportive. The Box discusses et al. Association of renal
stress/damage and filtra-
estimate the magnitude of features that distinguish de- tion biomarkers with
changes in GFR. creased kidney perfusion from subsequent AKI during
hospitalization among
ATN. patients presenting to
The causes of AKI, which are cat- the emergency depart-
egorized according to underlying Complications of AKI result from ment. Clin J Am Soc
Nephrol. 2016;11:938-
pathophysiology, are decreased impaired excretory, endocrine, 46. [PMID: 27026519]
14. Perazella MA, Coca SG.
kidney perfusion, obstruction of and metabolic kidney functions. Traditional urinary bio-
the urinary tract, parenchymal Decreased GFR and tubular func- markers in the assess-
ment of hospital-
kidney diseases other than acute tion lead to retained water and acquired AKI. Clin J Am
tubular necrosis (ATN), and ATN solutes, manifested by volume Soc Nephrol. 2012;7:
167-74. [PMID:
(Figure 2). AKI often has more overload, hyperkalemia, high an- 22096038]
7 November 2017 Annals of Internal Medicine In the Clinic ITC69 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
ion gap metabolic acidosis, hy- were due to decreased kidney perfusion, 12%
Features Distinguishing ponatremia, hyperphosphatemia, were due to obstruction, 27% had “intrinsic
Decreased Kidney Perfusion hypermagnesemia, encephalop- kidney diseases” (parenchymal diseases, in-
From ATN athy, pericarditis, pruritus, and cluding ATN), and 12% were not classified (5).
Extracellular fluid volume depletion Causes of hospital-acquired AKI in patients
bleeding due to platelet dysfunc-
or circulatory disorders were described in patients admitted to general
tion. Deficiencies of erythropoie- medical or surgical services of an urban teach-
associated with volume
expansion are common in
tin and decreased synthesis of ing hospital. Of 380 episodes, 39% were due
decreased kidney perfusion, active vitamin D lead to anemia to decreased kidney perfusion, 2% to obstruc-
whereas recent exposure to and hypocalcemia. During recov- tion, 3% to parenchymal kidney diseases other
radiographic contrast or ery from AKI, persistent impair- than ATN, and 55% to causes associated with
nephrotoxic drugs or ATN; 3% were not classified (27).
ment in tubular function despite
hypotension is more prominent
in ATN. increasing GFR may give rise to
Decreased kidney perfusion de-
Decreased kidney perfusion excessive water and solute loss,
creases GFR and increases tubu-
improves rapidly after leading to volume depletion, hy-
lar reabsorption of sodium, chlo-
measures to increase kidney pernatremia, hypokalemia, non–
perfusion (e.g., intravenous ride, urea, and water, leading to
anion gap metabolic acidosis,
fluid in volume depletion), but urine concentration. Volume de-
no such response is observed
hypophosphatemia, hypomag- pletion as the cause of decreased
in ATN. nesemia, and hypercalcemia in kidney perfusion should be con-
Decreased kidney perfusion usually some cases. Drug toxicity is com- sidered in patients with a history
has concentrated urine and no mon because of altered pharma- of decreased oral intake, vomit-
RTE cells or granular casts in cokinetics and pharmacodynam-
urine; ATN usually has ing, diarrhea, increased ostomy
ics. Complications may occur in output, excessive sweating, per-
nonconcentrated urine, RTE
cells, and granular casts. other organ systems throughout cutaneous fluid drainage, bleed-
ATN = acute tubular necrosis; the course of disease; multiple ing, dizziness, light-headedness,
RTE = renal tubular epithelial. organ failure is associated with fainting, or recent weight loss,
the highest mortality. especially in the setting of dietary
What clinical manifestations
15. Huerta C, Castellsague J, should clinicians look for?
Varas-Lorenzo C, Garcı́a
Rodrı́guez LA. Nonsteroi- AKI is generally asymptomatic
dal anti-inflammatory Combined Diagnostic and
until the onset of kidney failure,
drugs and risk of ARF in Therapeutic Approach to AKI
the general population. emphasizing the importance of
Am J Kidney Dis. 2005; Assess volume status; administer
45:531-9. [PMID: monitoring SCC and eGFR and intravenous fluid if volume
15754275] urine output in patients at in- depleted or volume status is
16. Lapi F, Azoulay L, Yin H,
Nessim SJ, Suissa S. creased risk. However, clinical uncertain
Concurrent use of diuret-
ics, angiotensin convert-
manifestations are useful to de- Assess for indications for urgent
ing enzyme inhibitors, termine the cause of AKI and de- kidney replacement therapy
and angiotensin receptor (volume overload, uremic
blockers with non- tect its complications. After de-
steroidal anti-
complications, electrolyte
inflammatory drugs and
tection, whether rapid evaluation disorders, drug toxicity)
risk of acute kidney in- is necessary depends on the clin- Conduct urine studies
jury: nested case-control
study. BMJ. 2013;346: ical setting and severity of AKI. Consider additional laboratory
e8525. [PMID: We recommend a combined di- tests and imaging
23299844]
17. Dreischulte T, Morales agnostic and therapeutic ap- In all cases, thoroughly review the
DR, Bell S, Guthrie B. history of present illness,
Combined use of non-
proach (see the Box). If AKI is
medical history, medications
steroidal anti- severe, treatment must begin and exposure to radiocontrast
inflammatory drugs with
diuretics and/or renin- concurrently with evaluation. media, recent surgery and
angiotensin system in- other procedures, recent travel
hibitors in the commu- Evaluating Causes
nity increases the risk of or exposure to infectious
acute kidney injury. Decreased kidney perfusion is diseases, fluid intake and
Kidney Int. 2015;88: output, and laboratory tests and
396-403. [PMID:
the most common cause of
imaging and conduct a careful
25874600] community-acquired AKI, whereas
18. Trivedi HS, Moore H, physical examination. In
Nasr S, et al. A random- ATN is the most common cause of particular, assessment for
ized prospective trial to hospital-acquired AKI.
assess the role of saline
complications should be done
hydration on the devel- promptly to determine the
opment of contrast neph- Causes of community-acquired AKI were de- need for urgent therapy.
rotoxicity. Nephron Clin
Pract. 2003;93:C29-34.
scribed in a large survey of hospital discharges AKI = acute kidney injury.
[PMID: 12411756] in China. Of 4136 patients, 49% of AKI cases
姝 2017 American College of Physicians ITC70 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
salt restriction or diuretic therapy. gests lesions in the urinary tract.
Increased GFR within hours of Complete obstruction causes Drugs That Contribute to
volume repletion with oral or IV anuria, but partial obstruction may Acute Kidney Injury and the
fluids confirms the diagnosis. De- cause polyuria due to impairment Pathophysiologic Mechanism
creased kidney perfusion due to of tubular function. Immediate im- of Injury*
exacerbations of chronic heart, provement in GFR is expected af- Iodinated radiocontrast media
(acute tubular necrosis)
lung, or liver disease manifests as ter relief of acute obstruction, but
Nonsteroidal anti-inflammatory
weight gain and edema (car- improvement after relief of chronic
drugs (decreased kidney
diorenal and hepatorenal syn- obstruction may be slow or perfusion and tubular
dromes), often with low blood incomplete. toxicity)
pressure. Sepsis may also be as- Aminoglycosides (acute tubular
Parenchymal kidney diseases necrosis)
sociated with low blood pressure
other than ATN are frequent Amphotericin B (acute tubular
and other features of the sys-
causes of AKI. Many of these necrosis)
temic inflammatory response
diseases occur in the setting of -Lactam antibiotics (interstitial
syndrome. Intra-abdominal pres-
systemic disorders (infections; nephritis)
sure may increase in critically ill
vasculitis; inflammatory, my- Sulfonamides (interstitial
patients with abdominal or pelvic nephrtitis)
eloproliferative, or lymphoprolif-
disorders (trauma, hemoperito- Vancomycin (acute tubular
erative diseases; or drug toxicity)
neum, pancreatitis, surgery, ra- necrosis)
and may be associated with fe-
diologic procedures) or in condi- Acyclovir (crystal nephropathy)
ver, night sweats, arthralgias,
tions that do not originate in that Tenofovir (tubular toxicity)
mononeuropathy, or skin rash.
region (fluid resuscitation, sepsis, Glomerulonephritis may cause Methotrexate (crystal
burns). Bilateral renal artery ste- nephropathy)
gross hematuria (without clots).
nosis may occur in patients with Cisplatinum and carboplatin
Acute interstitial nephritis is gen- (acute tubular necrosis)
aortic aneurysm or diffuse ath- erally due to an allergic or toxic Ifosphamide (acute tubular
erosclerotic cardiovascular dis- drug reaction (see the Box). Bac- necrosis)
ease and causes severe hyper- terial pyelonephritis must be se- Vascular endothelial growth factor
tension. Use of NSAIDs can vere and bilateral to cause AKI inhibitors (thrombotic
decrease kidney perfusion, even and often causes flank pain with microangiopathy)
without volume or blood pres- high fever. Urinary symptoms are Calcineurin inhibitors (e.g.,
sure abnormalities. ACEIs and cyclosporine, tacrolimus)
prominent when pyelonephritis is (decreased kidney perfusion
ARBs reduce GFR in patients with caused by ascending infection and tubular toxicity)
acute and chronic kidney disease from the lower urinary tract but Herbal and dietary supplements
and may cause severe AKI in the may be absent in the presence of (e.g., aristolochic acid;
setting of decreased kidney hematogeneous dissemination of creatine; vitamins A, C, and
perfusion. bacteremia. Thrombotic microan- D; germanium; star fruit)
(interstitial nephritis)
giopathy is accompanied by mir-
Obstruction of both kidneys or Proton-pump inhibitors (interstitial
coangiopathic hemolysis and
obstruction of a solitary kidney nephritis)
thrombocytopenia with schisto-
may cause AKI. Obstruction may Angiotensin-converting enzyme
cytes. Cast nephropathy in my- inhibitors, angiotensin-receptor
be acute or chronic, complete or
eloma is typically associated with blockers, direct renin inhibitors
partial, due to upper or lower (decreased kidney perfusion)
a high tumor burden and large
urinary tract disease, and due to * Many drugs have several
amounts of paraprotein in the
lesions within or outside the uri- pathyphysiologic
urine and frequently with hyper-
nary tract. Flank pain or a history mechanisms.
calcemia. Renal infarction is asso-
of urolithiasis, genitourinary tract
ciated with flank pain and abrupt
neoplasia, or retroperitoneal dis-
onset of severe hypertension.
ease should raise suspicion for
Atheroembolism may occur af- 19. Taylor AJ, Hotchkiss D,
obstruction (28). Symptoms of
ter percutaneous intra-arterial Morse RW, McCabe J.
lower urinary tract disease in- procedures or surgery involving
PREPARED: Preparation
for Angiography in Renal
clude dysuria, suprapubic pain, the aorta or initiation of Dysfunction: a random-
ized trial of inpatient vs
slow urine stream, and increased anticoagulation. outpatient hydration
frequency of urination. Bladder protocols for cardiac
catheterization in mild-
distention may be detectable by The pathology of ATN is charac- to-moderate renal dys-
physical examination. Gross he- terized by necrosis of tubular function. Chest. 1998;
114:1570-4. [PMID:
maturia (with blood clots) sug- epithelial cells diffusely or local- 9872190]
7 November 2017 Annals of Internal Medicine In the Clinic ITC71 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
ized to nephron segments, with- of intermittently administered
out involvement of the glomeruli, medication.
20. Mueller C, Buerkle G,
Buettner HJ, et al. Pre-
accompanied by variable intersti-
Evaluating Complications
vention of contrast tial inflammation. However, clini-
media-associated ne- Irrespective of cause, the stage
phropathy: randomized cal pathologic correlations are
(severity) of AKI is related to the
comparison of 2 hydra- imprecise, and renal biopsy is
tion regimens in 1620 risk for complications.
patients undergoing rarely done in AKI. As a result,
coronary angioplasty.
Arch Intern Med. 2002; the diagnosis of ATN in AKI is The frequency of AKI-related complications was
162:329-36. [PMID: generally presumed in patients studied in 18 410 patients in ICUs in 4 hospitals
11822926]
21. Krasuski RA, Beard BM, with a typical clinical history and (29). The risk for volume overload increased
Geoghagan JD, Thomp-
urinary tract findings (as de- from 41% in patients without AKI to 58% for
son CM, Guidera SA.
Optimal timing of hydra- scribed below) after exclusion of stage 1, 77% for stage 2, and 83% for stage
tion to erase contrast-
other causes of AKI. Despite this 3 AKI. Other comparisons found respective
associated nephropathy:
increases in hyperkalemia from 3% to 9%,
the OTHER CAN study. J uncertainty, we will retain use of
Invasive Cardiol. 2003; 17%, and 32%; in metabolic acidosis from
15:699-702. [PMID: the term ATN as a cause of AKI 59% to 74%, 86%, and 91%; in hyponatre-
14660821]
22. Bader BD, Berger ED, because it remains a useful clini- mia from 19% to 30%, 46%, and 60%; and
Heede MB, et al. What is cal concept in diagnosis and azotemia (blood urea nitrogen >60 mg/dL)
the best hydration regi-
men to prevent contrast treatment. Circulatory shock and from 1% to 10%, 20%, and 49%.
media-induced nephro-
toxicity? Clin Nephrol.
sepsis are the most common
2004;62:1-7. [PMID: causes of ATN. Other common Physical examination can detect
15267006]
causes include recent exposure to volume overload (dyspnea, jugu-
23. Brar SS, Aharonian V,
Mansukhani P, et al. nephrotoxic drugs (see the Box) or lar venous distention, rales, as-
Haemodynamic-guided cites, lower extremity edema),
fluid administration for radiocontrast media, transient hy-
the prevention of
potension after surgery or a proce- uremic encephalopathy (leth-
contrast-induced acute
kidney injury: the POSEI- dure, and rapid cell necrosis (he- argy, asterixis, hyperreflexia, and
DON randomised con-
molysis, rhabdomyolysis, and myoclonus), and pericarditis
trolled trial. Lancet.
2014;383:1814-23.
tumor lysis). Pigment-associated (pericardial friction rub), which
[PMID: 24856027]
24. Qian G, Fu Z, Guo J, Cao ATN may cause urine discolor- require urgent therapy. Detec-
F, Chen Y. Prevention of
ation. Tumor lysis can occur before tion of other complications re-
contrast-induced ne-
quires laboratory testing.
phropathy by central or after chemotherapy.
venous pressure-guided
fluid administration in What laboratory tests and
chronic kidney disease It is essential to review the history
and congestive heart imaging should clinicians use?
failure patients. JACC and medical record to determine
The need for laboratory tests and
Cardiovasc Interv. 2016; whether the patient has had CKD
9:89-96. [PMID: imaging depends on the clinical
26685074] or past episodes of AKD. Com-
25. Subramaniam RM, setting. No further evaluation
Suarez-Cuervo C, Wilson
parison of current values of SCC
may be necessary for outpatients
RF, et al. Effectiveness of and eGFR to previous levels is
prevention strategies for with AKI and decreased kidney
contrast-induced ne- helpful for early detection of AKI.
phropathy: a systematic perfusion due to volume deple-
Past urinalyses, measures of albu-
review and meta- tion and rapid resolution of AKI
analysis. Ann Intern minuria (albumin-to-creatinine
Med. 2016;164:406-16. after oral or IV volume repletion.
[PMID: 26830221] ratio, protein-to-creatinine ratio),
If volume status is not clear, we rec-
26. Eng J, Wilson RF, Subra- and imaging studies of the kid-
maniam RM, et al. Com- ommend an early therapeutic trial of
parative effect of contrast neys (abdominal ultrasonogra-
media type on the inci- withholding diuretics and adminis-
phy, computed tomography,
dence of contrast- tering an IV fluid bolus of 500 mL
induced nephropathy: a magnetic resonance imaging,
systematic review and isotonic saline over 4–6 hours with
meta-analysis. Ann Intern and angiography) may also be
Med. 2016;164:417-24.
assessment of volume status, urine
used. AKI superimposed on CKD
[PMID: 26830055] output, and SCC and eGFR within
27. Nash K, Hafeez A, Hou S. may be due to an exacerbation
Hospital-acquired renal 8–12 hours. Improved urine output,
insufficiency. Am J Kid- of the underlying disease, which SCC, and eGFR suggests AKI due to
ney Dis. 2002;39:930-6. is common in chronic diseases volume depletion, whereas no im-
[PMID: 11979336]
28. Licurse A, Kim MC, Dz- causing decreased kidney perfu- provement suggests some other
iura J, et al. Renal ultra-
sonography in the evalu-
sion, or onset of a new condition. cause.
ation of acute kidney A history of AKD may provide a
injury: developing a risk
stratification framework. clue to the cause of a current epi- In patients with AKI from some
Arch Intern Med. 2010; sode, such as a flare of autoim- other cause, urine appearance,
170:1900-7. [PMID:
21098348] mune disease or nephrotoxicity dipstick, sediment, and chemis-
姝 2017 American College of Physicians ITC72 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
tries (osmolality, sodium, urea ated with preserved urine concen-
nitrogen, creatinine, albumin, tration, despite the presence of
and total protein) must be as- urine sediment findings suggestive
sessed to ascertain concentra- of ATN.
29. Libório AB, Leite TT,
tion; albuminuria and total pro- Neves FM, Teles F, Be-
teinuria; and the presence or Tests for albumin rather than to- zerra CT. AKI complica-
absence of hematuria, pyuria, tal protein are preferred for eval- tions in critically ill pa-
tients: association with
uation of kidney disease in adults mortality rates and RRT.
renal tubular epithelial cells, and Clin J Am Soc Nephrol.
(12), but both may be helpful in
granular and cellular casts (Ap- 2015;10:21-8. [PMID:
the evaluation of AKI. Loss of al- 25376761]
pendix Table 1, available at 30. Miller TR, Anderson RJ,
bumin in the urine is a marker of Linas SL, et al. Urinary
Annals.org). If obstruction is sus-
glomerular damage and occurs diagnostic indices in
pected, ultrasonography of the acute renal failure: a
in most parenchymal kidney dis- prospective study. Ann
kidneys is warranted, with a Intern Med. 1978;89:47-
eases other than ATN. Total pro-
postvoiding image of the blad- 50. [PMID: 666184]
teinuria in the absence of albu- 31. Muriithi AK, Nasr SH,
der if symptoms occur during Leung N. Utility of urine
minuria is a marker of increased eosinophils in the diag-
urination (Appendix Table 1) nosis of acute interstitial
production or impaired tubular
(28). We generally obtain a urine nephritis. Clin J Am Soc
reabsorption of low-molecular- Nephrol. 2013;8:1857-
culture, since urinary tract infec- 62. [PMID: 24052222]
weight serum proteins (light- 32. Wald R, Bell CM, Nisen-
tion can be a cause of AKI (pye-
chain proteinuria or tubular pro- baum R, et al. Interob-
lonephritis or ATN associated server reliability of urine
teinuria, respectively). The urine sediment interpretation.
with sepsis) or may complicate Clin J Am Soc Nephrol.
dipstick is more sensitive to albu-
other causes. Additional tests min than other serum proteins;
2009;4:567-71. [PMID:
19261816]
are required to assess complica- the albumin-to-creatinine ratio 33. Perazella MA, Coca SG,
Kanbay M, Brewster UC,
tions, systemic diseases or dis- and protein-to-creatinine ratio Parikh CR. Diagnostic
eases in other organ systems, provide a quantitative assess-
value of urine micros-
copy for differential diag-
and hemodynamic status in criti- ment, but urine creatinine excre- nosis of acute kidney
injury in hospitalized
cally ill patients. tion decreases when SCC in- patients. Clin J Am Soc
Nephrol. 2008;3:1615-9.
Tests of urine concentration were creases, which may cause a [PMID: 18784207]
initially proposed for the evalua- falsely elevated albumin-to- 34. Chawla LS, Bellomo R,
Bihorac A, et al; Acute
tion of oliguric AKI to distinguish creatinine or protein-to- Disease Quality Initiative
creatinine ratio. Workgroup 16. Acute
decreased kidney perfusion from kidney disease and renal
recovery: consensus
ATN (14, 30). They are also useful Red blood cells and white blood report of the Acute Dis-
in nonoliguric AKI due to these cells may be detected in unspun
ease Quality Initiative
(ADQI) 16 Workgroup.
and other causes. The glomerular urine with a dipstick (heme or Nat Rev Nephrol. 2017;
13:241-257. [PMID:
filtrate is isotonic with plasma; con- leukocyte esterase reagent pads, 28239173]
centration of the urine requires in- respectively) and quantified with 35. Bellomo R, Vaara ST,
Kellum JA. How to im-
tact tubular function. Concentration a manual or automated cell coun- prove the care of patients
of the urine in the setting of AKI indi- with acute kidney injury
ter. We do not recommend rou- [Editorial]. Intensive Care
cates decreased kidney perfusion tine testing for urine eosinophils Med. 2017;43:727-729.
[PMID: 28600756]
and preserved tubular function. Ab- (31). Detection of renal tubular 36. Davenport A, Anker SD,
sence of urine concentration indi- epithelial cells and granular and Mebazaa A, et al; Acute
Dialysis Quality Initiative
cates impaired tubular function. The cellular casts requires micro- (ADQI) consensus group.
ADQI 7: the clinical man-
fractional excretion of sodium and scopic examination of urine sedi- agement of the Cardio-
urea (FENa and FEurea) can be ment. Increased red or white Renal syndromes: work
group statements from
computed easily from simultaneous blood cells in the urine indicates the 7th ADQI consensus
serum and spot urine samples (Ap- conference. Nephrol Dial
a urinary tract lesion, but the Transplant. 2010;25:
pendix Table 1). Diuretic therapy presence of renal tubular epithe- 2077-89. [PMID:
20494894]
impairs sodium reabsorption more lial cells or granular or cellular 37. Facciorusso A, Chandar
than urea reabsorption, so a low casts in the sediment localizes AK, Murad MH, et al.
Comparative efficacy of
FEurea may be a more reliable test the lesion to the kidney. The di- pharmacological strate-
gies for management of
for distinguishing decreased kidney agnostic accuracy of these find- type 1 hepatorenal syn-
perfusion from ATN than a low ings has not been well-studied drome: a systematic
review and network
FENa in patients with recent diuretic (32, 33). Our interpretation is that meta-analysis. Lancet
therapy. Exacerbations of heart, the presence of renal tubular epi- Gastroenterol Hepatol.
2017;2:94-102. [PMID:
lung, or liver disease may be associ- thelial cells and granular and cel- 28403995]
7 November 2017 Annals of Internal Medicine In the Clinic ITC73 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
lular casts for the conditions in bodies, complement compo-
Appendix Table 2 (available at nents, and inflammatory markers
38. Dellinger RP, Levy MM, Annals.org) is more specific than may be indicated.
Rhodes A, et al; Surviv-
ing Sepsis Campaign sensitive—in other words, paren-
Guidelines Committee
chymal kidney disease is more Hemodynamic monitoring (jugular
including the Pediatric
Subgroup. Surviving likely when these findings are venous pressure or pulmonary capil-
sepsis campaign: inter-
present but is not ruled out lary wedge pressure) may be re-
national guidelines for
management of severe
when they are absent. Kidney quired to assess cardiac filling and
sepsis and septic shock:
2012. Crit Care Med. biopsy may be performed when guide volume management in pa-
2013;41:580-637.
suspicion for a parenchymal dis- tients with hypotension. Dynamic
[PMID: 23353941]
39. Cattran DC, Feehally J, ease other than ATN is high. variables, such as pulse–pressure
Cook TH, et al. Kidney variation, inferior vena cava filling on
disease: Improving
global outcomes (KDIGO) Imaging studies are usually done ultrasonography, and echocardiog-
glomerulonephritis work
group. KDIGO clinical
to assess hydronephrosis, de- raphy may be useful. Intra-
practice guideline for fined as dilatation of the renal abdominal pressure can be as-
glomerulonephritis.
Kidney International collecting system due to obstruc- sessed by measuring bladder
Supplement 1s. 2012;2): tion. However, they may also be pressure. Subclavian vein catheters
135.
40. González E, Gutiérrez E, performed to assess kidney should be avoided in patients with
Galeano C, et al; Grupo
Madrileño De Nefritis
shape and size in patients with CKD stages 4–5 (GFR <30 mL/min/
Intersticiales. Early ste- AKI superimposed on CKD or in 1.73 m2) to avoid venous stenosis
roid treatment improves
the recovery of renal patients who have not had previ- that may preclude later vascular ac-
function in patients with ous imaging studies. Renal ultra- cess for hemodialysis.
drug-induced acute inter-
stitial nephritis. Kidney sonography is preferred because
Int. 2008;73:940-6. What other diagnoses should
[PMID: 18185501] it has >90% sensitivity for detect-
clinicians consider in patients
41. Koyner JL, Davison DL, ing hydronephrosis and is not
Brasha-Mitchell E, et al.
associated with radiation expo- with possible AKI?
Furosemide Stress Test
and Biomarkers for the sure or contrast administration. Decreased GFR is classified as
Prediction of AKI Sever-
ity. J Am Soc Nephrol. Causes of obstruction of the urinary CKD, AKD, or AKI, depending on
2015;26:2023-31.
tract without hydronephrosis in- severity and duration; AKD and
[PMID: 25655065]
42. Chawla LS, Davison DL, clude massive bleeding into the AKI can be superimposed on
Brasha-Mitchell E, et al. CKD (Figure 1). Distinguishing
Development and stan- urinary tract or extensive retroperito-
dardization of a furo- neal fibrosis. Dilatation of the urinary among these conditions is impor-
semide stress test to
predict the severity of tract in the absence of obstruction tant for determining the cause of
acute kidney injury. Crit
may be observed after relief of ob- kidney disease and for determin-
Care. 2013;17:R207.
[PMID: 24053972] struction in vesicoureteral reflux, ing the urgency of evaluation and
43. Ho KM, Sheridan DJ. treatment. Many causes of kidney
Meta-analysis of during massive diuresis, and in
frusemide to prevent or
pregnancy. A combination of clinical disease may have an acute or
treat acute renal failure.
BMJ. 2006;333:420. characteristics can identify patients chronic presentation, although
[PMID: 16861256]
in which ultrasonography could be the most common causes of CKD
44. Cantarovich F, Rangoon-
wala B, Lorenz H, et al; omitted (28). (diabetic glomerulosclerosis and
High-Dose Flurosemide hypertension nephrosclerosis) do
in Acute Renal Failure
Study Group. High-dose Other tests are required to assess not have an acute presentation,
furosemide for estab-
lished ARF: a prospec-
causes and complications of AKI. and ATN does not have a chronic
tive, randomized, Serum urea nitrogen and electro- presentation. Due to the non-
double-blind, placebo-
controlled, multicenter lyte (sodium, potassium, chlo- steady state, changes in SCC and
trial. Am J Kidney Dis.
2004;44:402-9. [PMID:
ride, bicarbonate, calcium, phos- eGFR lag behind those in GFR,
15332212] phorus, magnesium) levels causing delayed recognition of
45. Finfer S, Bellomo R,
Boyce N, et al; SAFE
should be measured. Venous or AKI. The rise in SCC (and de-
Study Investigators. A arterial blood gasses may be re- crease in eGFR) may be slower in
comparison of albumin
and saline for fluid resus- quired for interpretation of acid– patients with low muscle mass or
citation in the intensive base disorders. Complete blood volume overload and faster in
care unit. N Engl J Med.
2004;350:2247-56. count; liver function tests; muscle patients with high muscle mass
[PMID: 15163774]
46. Perel P, Roberts I. Col- enzymes; and imaging for heart, or volume depletion. When base-
loids versus crystalloids lung, and liver diseases should line GFR is low, minor fluctua-
for fluid resuscitation in
critically ill patients. be obtained. Blood and body tions in GFR can cause a rise in
Cochrane Database Syst fluid cultures and serologic tests SCC by 0.3 mg/dL in the absence
Rev. 2007:CD000567.
[PMID: 17943746] for infectious diseases, autoanti- of acute kidney disease. Adher-
姝 2017 American College of Physicians ITC74 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
ence to the time requirement for less than 20 mL/min/1.73 m2, it can
diagnosis of AKI (48 hours) can be assessed as the mean of urine
minimize overdiagnosis. An in- clearance of urea and creatinine
crease in SCC (and decrease in during a timed urine collection.
eGFR) in the absence of decline 47. Young P, Bailey M, Beas-
in GFR may occur after a medica- When should clinicians consider ley R, et al; SPLIT Investi-
tion is started that inhibits creati- consulting a specialist? gators. Effect of a buff-
ered crystalloid solution
nine secretion (trimethoprim or Consultation with a nephrologist vs saline on acute kidney
injury among patients in
cimetidine) or interferes with the is often unnecessary for detect- the intensive care unit:
assay for creatinine (flucytosine ing AKI. However, it should usu- The SPLIT randomized
clinical trial. JAMA.
for the creatinine iminohydrolase ally be requested for identifying 2015;314:1701-10.
[PMID: 26444692]
assay). Serum ketones interfere with the cause of AKI resulting from 48. Hewitt J, Uniacke M,
the widely used colorimetric assay something other than volume Hansi NK, Venkat-Raman
G, McCarthy K. Sodium
for creatinine. GFR, measured using depletion that resolves promptly bicarbonate supplements
for treating acute kidney
clearance of an exogenous filtration with volume repletion (Figure 2). injury. Cochrane Data-
marker, or creatinine clearance, can Consultation may also be helpful base Syst Rev. 2012:
CD009204. [PMID:
be assessed to identify misleading for identifying the cause of 22696382]
alterations in SCC or eGFR. If GFR is CKD. 49. Bellomo R, Cass A, Cole
L, et al; RENAL Study
Investigators. Calorie
intake and patient out-
comes in severe acute
Diagnosis... Decreased GFR may be due to AKI, AKD, or CKD. KDIGO kidney injury: findings
guidelines define AKI as an increase in SCC by ≥50% within 7 days or from The Randomized
Evaluation of Normal vs.
≥0.3 mg/dL (26.5 μmol/L) within 2 days, or oliguria for ≥6 hours. The Augmented Level of
stage (severity) is defined by the peak increase in SCC compared with Replacement Therapy
(RENAL) study trial. Crit
previous values and the nadir in urine output, and is related to the risk Care. 2014;18:R45.
for complications and the prognosis. The causes of AKI— decreased kid- [PMID: 24629036]
ney perfusion, obstruction of the urinary tract, parenchymal kidney dis- 50. Bellomo R, Cass A, Cole
L, et al; RENAL Study
eases other than ATN, and ATN—are grouped according to underlying Investigators. Daily pro-
pathophysiology and are the basis for specific therapy. The clinical set- tein intake and patient
outcomes in severe acute
ting, including response to IV fluid, and urinary tract findings are helpful kidney injury: findings of
in determining the cause of AKI. the randomized evalua-
tion of normal versus
augmented level of
replacement therapy
CLINICAL BOTTOM LINE (RENAL) trial. Blood Purif.
2014;37:325-34. [PMID:
25171270]
51. Cox ZL, McCoy AB, Ma-
theny ME, et al. Adverse
drug events during AKI
Treatment and its recovery. Clin J
Am Soc Nephrol. 2013;
8:1070-8. [PMID:
The goals of management of AKI ther diagnostic evaluation is re- 23539228]
include use of specific treatments quired, if AKI is severe or not 52. Matzke GR, Aronoff GR,
Atkinson AJ Jr, et al.
according to the underlying rapidly reversible, or when Drug dosing consider-
ation in patients with
cause and providing supportive complications are present. Man- acute and chronic kidney
care to prevent and manage agement in the ICU should be disease-a clinical update
from Kidney Disease:
complications. KRT is used when considered for patients with AKI Improving Global Out-
comes (KDIGO). Kidney
complications develop that can- and serious illness (35). Int. 2011;80:1122-37.
not be managed with medical [PMID: 21918498]
What pharmacologic therapies 53. McCoy AB, Waitman LR,
therapy alone (Figure 2). Gadd CS, et al. A com-
should be used? puterized provider order
When should patients be The use of pharmacologic thera- entry intervention for
medication safety during
hospitalized? pies in the setting of AKI is spe- acute kidney injury: a
quality improvement
For outpatients with new-onset cific to the underlying cause report. Am J Kidney Dis.
or worsening GFR decline, early (Appendix Table 2). IV fluids are 2010;56:832-41. [PMID:
20709437]
follow-up is required to distin- recommended to correct volume 54. Bagshaw SM, Wald R.
Strategies for the optimal
guish AKI from AKD and CKD depletion. Afterload reducing timing to start renal
(1, 34). Although evidence to sup- agents are appropriate in cases replacement therapy in
critically ill patients with
port specific criteria for hospitaliza- of acute heart failure (36), acute kidney injury.
tion is not available, hospitalization whereas midodrine, octreotide, Kidney Int. 2017;91:
1022-1032. [PMID:
is generally recommended if fur- and albumin can be used in 28222898]
7 November 2017 Annals of Internal Medicine In the Clinic ITC75 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
cases of liver failure (37). IV fluid ceiving dialysis, or time to achieve a serum cre-
55. Gaudry S, Hajage D,
Schortgen F, et al; AKIKI and early antibiotic therapy is atinine level < 200 umol/L was noted (44).
Study Group. Initiation important for treating infections
strategies for renal- KDIGO guidelines recommend
replacement therapy in (38). Withdrawal of NSAIDs,
the intensive care unit. N using vasopressors (e.g., norepi-
Engl J Med. 2016;375: ACEIs, and ARBs is recom-
nephrine or vasopressin) in con-
122-33. [PMID: mended. Immunosuppressive
27181456] junction with fluids in patients
56. Zarbock A, Kellum JA, therapies are recommended for
Schmidt C, et al. Effect of with vasomotor shock accompa-
many causes of acute glomerulo-
early vs delayed initia- nying AKI (1). Low-quality evi-
tion of renal replacement nephritis (39). Although high-
therapy on mortality in dence suggests using a protocol-
critically ill patients with quality evidence is lacking, many
based approach to achieve
acute kidney injury: the experts recommend corticoste-
ELAIN randomized clini- specific mean arterial pressure and
cal trial. JAMA. 2016; roids to treat acute interstitial ne-
315:2190-9. [PMID: other physiologic targets (1). On
27209269]
phritis when AKI is severe or in
the basis of moderate-quality evi-
57. Bellomo R, Cass A, Cole cases of drug-induced interstitial
L, et al; RENAL Replace- dence, KDIGO guidelines recom-
ment Therapy Study nephritis if AKI does not resolve
Investigators. Intensity of mend against dopamine, fenoldo-
after the causative medication is
continuous renal- pam, atrial natriuretic peptides,
replacement therapy in discontinued (40). Plasma ex-
critically ill patients. N insulin-like growth factor, or
Engl J Med. 2009;361: change is recommended for some
N-acetylcysteine to treat AKI (1).
1627-38. [PMID: causes of thrombotic microangi-
19846848]
58. Palevsky PM, O’Connor opathy. High-dose chemotherapy How should clinicians manage
TZ, Chertow GM, et al;
US Department of Veter-
is used in multiple myeloma. There volume problems?
ans Affairs/National Insti- are currently no effective pharma- AKI may develop in the setting of
tutes of Health Acute
Renal Failure Trial Net- cotherapies for treating ATN. The volume depletion or overload,
work. Intensity of renal KIDGO guidelines recommend and either condition may occur
replacement therapy in
acute kidney injury: against diuretics to treat AKI ex- during the course of AKI. Volume
perspective from within
the Acute Renal Failure
cept for management of volume overload is more likely to occur
Trial Network Study. Crit overload. However, a furosemide in the setting of oliguria, is asso-
Care. 2009;13:310.
[PMID: 19678919] “stress test” (administration of 1 ciated with poor outcomes in
59. Pannu N, Klarenbach S, mg/kg of IV furosemide with 1:1
Wiebe N, Manns B, To- AKI, and should be avoided to
nelli M; Alberta Kidney replacement of urine output with prevent life-threatening pulmo-
Disease Network. Renal
replacement therapy in saline) can be used to assess prog- nary edema. Volume depletion
patients with acute renal nosis: Patients with <200 mL of should also be avoided because
failure: a systematic
review. JAMA. 2008; urine output over the subsequent it can delay recovery of AKI due
299:793-805. [PMID:
18285591]
2 hours are at greater risk for pro- to other conditions. Frequent
60. Vinsonneau C, Camus C, gression to a higher AKI stage or monitoring of fluid intake and
Combes A, et al; Hemo-
diafe Study Group. Con- to the need for KRT (41, 42). Al- output, body weight, and volume
tinuous venovenous though high-dose loop diuretics status and administering or re-
haemodiafiltration versus
intermittent haemodialy- can increase urine output in AKI, stricting fluid depending on the
sis for acute renal failure
in patients with multiple-
they do not seem to reduce mor- results are important.
organ dysfunction syn- tality or the need for dialysis.
drome: a multicentre
randomised trial. Lancet. IV fluids are recommended for
2006;368:379-85. A systematic review of 6 moderate- to low- correcting AKI with volume de-
[PMID: 16876666] quality randomized controlled trials of furo-
61. Coca SG, Yusuf B, Sh- pletion and for intravascular vol-
lipak MG, Garg AX, semide to treat AKI reported that it did not re-
Parikh CR. Long-term risk duce in-hospital mortality, requirement for ume expansion in AKI with sepsis
of mortality and other
dialysis, or the number of dialysis treatments (1). Isotonic crystalloids (e.g., nor-
adverse outcomes after
acute kidney injury: a required until recovery of kidney function. In mal saline, Ringer lactate, or
systematic review and other balanced crystalloid solu-
meta-analysis. Am J addition, higher doses were associated with in-
Kidney Dis. 2009;53: creased toxicity (43). tions) are recommended rather
961-73. [PMID:
19346042] than colloids (albumin or
In a moderate-quality randomized trial of 338
62. James MT, Samuel SM, starches) as initial management
Manning MA, et al. patients from ICUs and nephrology wards who
Contrast-induced acute on the basis of moderate-quality
kidney injury and risk of had AKI requiring KRT, patients who were ran-
adverse clinical out- domly assigned to daily furosemide 25 mg/kg evidence (45– 47). Colloids may
comes after coronary
IV or 35 mg/kg orally more rapidly achieved be used for patients with liver
angiography: a system-
atic review and meta- urine output >2 L per day (5.7 days with furo- failure or burns. Treatment of vol-
analysis. Circ Cardiovasc ume overload in patients with
Interv. 2013;6:37-43.
semide vs. 7.8 days with placebo). However,
[PMID: 23322741] no significant differences in mortality, time re- AKI can sometimes be accom-
姝 2017 American College of Physicians ITC76 In the Clinic Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
plished using high doses of IV erally appropriate. In the presence
loop diuretics, given as multiple of volume overload, water restric-
doses throughout the day or as tion and loop diuretics should be
an infusion and often in conjunc- used. Hypercalcemia may be en-
tion with IV thiazide diuretics. countered in AKI accompanying
multiple myeloma and can be cor-
How should clinicians manage rected by volume expansion and
electrolyte problems? loop diuretics in patients who are
Initial management of electrolyte not oliguric or by promoting bone
abnormalities should start with uptake with administration of an IV
medical management and pro- bisphosphate. Hyperphos-
ceed to KRT when medical man- phatemia can be managed by di-
agement is no longer satisfac- etary phosphate restriction and
tory. Dietary potassium should oral phosphate binders. Hyperma- 63. Coca SG, Singanamala S,
be restricted, and medications Parikh CR. Chronic kid-
gnesemia may occur after magne- ney disease after acute
that cause hyperkalemia should sium infusion and can be man- kidney injury: a system-
atic review and meta-
be used cautiously. Treatment of aged by discontinuing the infusion analysis. Kidney Int.
severe hyperkalemia (serum po- and administering loop diuretics. 2012;81:442-8. [PMID:
22113526]
tassium > 6.5 mmol/L or with 64. Hsu CY, Hsu RK, Yang J,
electrocardiographic changes)
How should clinicians manage et al. Elevated BP after
AKI. J Am Soc Nephrol.
includes administration of cal- nutrition, drug dosing, and 2016;27:914-23. [PMID:
cium gluconate to reduce the risk anticoagulation? 26134154]
65. Sawhney S, Marks A,
for arrhythmia, followed by insu- Nutrition should provide ade- Fluck N, et al. Post-
discharge kidney func-
lin plus dextrose, -agonists, or quate calories with restricted po- tion is associated with
sodium bicarbonate to shift po- tassium and phosphate. KDIGO subsequent ten-year
renal progression risk
tassium from the extracellular to guidelines for patients with AKI among survivors of acute
kidney injury. Kidney Int.
the intracellular compartment. recommend a total energy intake 2017;92:440-452.
These treatments are temporary of 20 –30 kcal/kg per day, prefer- [PMID: 28416224]
66. Schmitt R, Coca S, Kan-
and must be accompanied by ably provided via the enteral bay M, et al. Recovery of
measures to remove potassium route (49). Minimal nitrogenous kidney function after
acute kidney injury in
from the body. For patients with- waste production is desirable in the elderly: a systematic
review and meta-
out oliguria, high-dose loop di- AKI; however, protein restriction analysis. Am J Kidney
uretics can be used to increase is not suggested as a means to Dis. 2008;52:262-71.
[PMID: 18511164]
urine output and potassium ex- avoid KRT. On the basis of low- 67. Heung M, Steffick DE,
cretion. For patients with oliguria, quality evidence, KDIGO guide- Zivin K, et al; Centers for
Disease Control and
sorbitol with sodium polystyrene lines recommend protein goals Prevention CKD Surveil-
lance Team. Acute kidney
sulfonate or calcium polystyrene of 0.8 –1.0 g/kg per day in non- injury recovery pattern
sulfonate resins can be used to catabolic patients, 1.1–1.5 g/kg and subsequent risk of
CKD: an analysis of Vet-
per day in patients receiving re- erans Health Administra-
induce osmotic diarrhea and fe-
nal replacement therapy, and a tion data. Am J Kidney
cal potassium losses. Most ex- Dis. 2016;67:742-52.
maximum 1.7 g/kg per day in [PMID: 26690912]
perts suggest using supplemen- 68. Wu VC, Wu CH, Huang
hypercatabolic patients or those
tal sodium bicarbonate when TM, et al; NSARF Group.
requiring continuous KRT (1, 50). Long-term risk of coro-
metabolic acidosis is severe, al- nary events after AKI. J
In critically ill patients, KDIGO Am Soc Nephrol. 2014;
though there is no high-quality
guidelines suggest insulin ther- 25:595-605. [PMID:
evidence (48). Hypernatremia 24503241]
apy targeting plasma glucose 69. Ftouh S, Thomas M;
may be encountered in AKI with Acute Kidney Injury
110 –149 mg/dL. Guideline Development
dehydration, after normal saline Group. Acute kidney
resuscitation, or when access to Patients with AKI require special injury: summary of NICE
guidance. BMJ. 2013;
water is restricted. It can usually drug dosing due to buildup from 347:f4930. [PMID:
be corrected by providing water decreased excretion and metab- 23985310]
70. Soares DM, Pessanha JF,
via enteral routes or IV hypnatric olism by the kidney as well as the Sharma A, Brocca A,
Ronco C. Delayed ne-
solutions. The management of effects of kidney failure on other phrology consultation
hyponatremia in the setting of routes of drug excretion and me- and high mortality on
acute kidney injury: a
AKI depends on its cause. In tabolism (51, 52). Estimated GFR meta-analysis. Blood
states of volume depletion, admin- is less accurate to guide dosing Purif. 2017;43:57-67.
[PMID: 27915348] doi:
istration of isotonic IV fluids is gen- in the nonsteady state than in the 10.1159/000452316
7 November 2017 Annals of Internal Medicine ITC77 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
steady state. Expert consensus What is the role of KRT? Significant differences between
recommends closely monitoring KRT is used to manage the com- the 2 methods in terms of mor-
drug response in patients with plications of severe AKI. Com- tality, length of hospitalization,
known nephrotoxicity or other mon indications include life- and long-term requirements for
toxicities, using therapeutic drug threatening changes in fluid, dialysis have not been found
monitoring when clinically useful electrolyte, and acid– base bal- (59, 60).
assays are available, and being ance that require emergent cor- What is the prognosis?
cognizant of residual effects of rection (Figure 2). KRT may be
AKI is associated with high mor-
medicines that are excreted by started before these complications
tality rates that range from 16%–
the kidney even after they have develop, although evidence con-
50% according to stage (Appen-
been discontinued (e.g., oral flicts about whether preemptive
dix Figure, available at Annals.
hypoglycemic agents and opi- initiation at an earlier stage of AKI
org) and vary according to the
oids) (52, 53). The assistance of a is more beneficial than when com-
cause, coexisting conditions, and
pharmacist may be helpful, par- plications occur (54 –56). KRT
availability of KRT (3). Survivors
ticularly in determining dosing should be discontinued as soon as
of AKI are at increased risk for
and dosing intervals in patients it is no longer required, either be-
hypertension and progressive
receiving dialysis and those re- cause kidney function has recov-
CKD, including end-stage kidney
quiring antibiotics for AKI ac- ered enough to meet the patient's
disease (61– 65). KDIGO guide-
companying sepsis. needs or life-sustaining therapy is
lines thus recommend evaluat-
no longer the goal of the patient's
ing patients after AKI for recov-
Certain anticoagulants should be care.
ery of kidney function, new
used with caution in patients with
Several types of KRT can be onset, or worsening of preexist-
AKI due to the increased bleeding
used, and the type varies by loca- ing CKD. Older age, lower base-
risk attributed to uremic platelet
tion of care and available equip- line eGFR, higher baseline albu-
dysfunction and to decreased minuria, and AKI severity
excretion of low-molecular-weight ment and expertise (Appendix
Table 3, available at Annals.org). (KDIGO stage) are predictors of
heparins and direct oral anticoag- CKD after AKI and should
Peritoneal dialysis is rarely used
ulants. Although some manufac- prompt postdischarge follow-up
for KRT in adults with AKI in
turers provide altered dosing (6, 66, 67). Referral to commu-
North America, although it is
schedules based on creatinine nity nephrology services may be
more commonly used in areas
clearance for some low- appropriate for patients who do
with limited resources. Continu-
molecular-weight heparins (e.g., not recover kidney function
ous KRT is a slow, continuous
enoxaparin) and direct oral anti- given the associated long-term
form of therapy delivered 24
coagulants (e.g., dabigatran), de- risks of kidney failure, cardiovas-
hours a day in ICUs and is usu-
termining safe dosing schedules ally used to treat hemodynami- cular events, and mortality for
when GFR is changing, especially cally unstable patients (57). several years after hospital dis-
during dialysis, is difficult. Al- Conventional intermittent hemo- charge (62, 68).
though low-molecular-weight dialysis is used in AKI for hemo-
heparins are used intermittently in In a systematic review, the pooled mortality
dynamically stable patients; it is rate was 23.0% overall and 49.4% in patients
patients receiving long-term dialy- similar to the in-center long-term needing dialysis (Appendix Figure) (3). The
sis and some organizations have hemodialysis used for end-stage pooled unadjusted odds of death were 3.4-
suggested monitoring anti-factor kidney disease (58). More fre- fold higher for patients with KDIGO stage 1
X activity with continuous use, quent sessions may be required AKI, 7.5-fold higher for stage 2, 13.2-fold
many experts prefer to use unfrac- to manage fluid and electrolyte higher for stage 3, and 24-fold higher in pa-
tionated heparin in severe AKI. abnormalities for some patients tients needing dialysis compared with patients
For patients with active bleeding with AKI. Prolonged intermittent without AKI. The AKI-associated mortality rate
in the presence of uremia, desmo- KRT uses the same equipment declined over 8 years and was inversely related
pressin (0.3 mcg/kg IV, subcuta- to the percentage of a country's gross domes-
as conventional dialysis but pro-
tic product spent on total health
neous, or intranasal) and cryopre- vides dialysis using lower blood expenditure.
cipitate can be used to rapidly flow rates over longer sessions
diminish bleeding time, whereas (usually ≥6 hours/session). Sev- When should clinicians
conjugated estrogens and dialysis eral randomized trials have com- consider consulting a specialist?
(without systemic anticoagulation) pared outcomes with continuous Because AKI is a common com-
can be used for more prolonged KRT versus intermittent hemodi- plication of many medical and
bleeding control. alysis in critically ill patients (59). surgical illnesses, most patients
姝 2017 American College of Physicians ITC78 Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
with AKI are cared for by general tion have been excluded or cor-
internists, hospitalists, surgeons, rected. Clinicians should discuss
and critical care and primary care management with a nephrologist if
physicians. These clinicians a diagnosis that may need specific
should consult a nephrologist or treatments is suspected (e.g., paren-
critical care specialist for patients chymal kidney diseases other than
who have AKI with any indication ATN), response to treatment has
for KRT (69). Nephrology referral been inadequate, there are associ-
and comanagement is also appro- ated complications, AKI is severe
priate if the cause of AKI is uncertain, (KDIGO stage 3), or it is superim-
particularly when decreased kidney posed on CKD stages 4–5 (baseline
perfusion and urinary tract obstruc- GFR < 30 mL/min/1.73 m2) (70).
Treatment... The main goals of managing AKI are specific pharmaco-
logic therapy addressing underlying causes and providing supportive
care to prevent and manage complications. Supportive care includes
maintenance of hemodynamic stability and kidney perfusion using IV
crystalloids when volume expansion is needed and the use of diuretics
in states of volume overload, medical management of electrolyte disor-
ders, provision of adequate nutrition and glycemic control, and cau-
tious use of medications to avoid adverse drug events. When AKI is se-
vere, KRT may be required to manage complications. Survivors of AKI
should be assessed for recovery of kidney function and receive subse-
quent follow-up to identify and subsequently manage CKD.
CLINICAL BOTTOM LINE
In the Clinic Clinical Guidelines
IntheClinic
www.kdigo.org/clinical_practice_guidelines/pdf
Tool Kit
/KDIGO%20AKI%20Guideline.pdf
Guidelines published by the International Society of
Nephrology.
www.clinicalguidelines.gov.au/portal/2481/clinical
-practice-guideline-acute-kidney-injury
2014 guideline from the National Health and Medical
Research Council of Australia.
Acute Kidney www.nice.org.uk/guidance/cg169
Injury Guidance from the National Institute for Health and Care
Excellence.
Patient Information
www.kidney.org/atoz/content/AcuteKidneyInjury
Information presented by the National Kidney foundation
for both patients and caregivers.
www.thinkkidneys.nhs.uk/aki/wp-content/uploads
/sites/2/2015/11/BKPA-RCGP-A4-Printout-Leaflet_v4
.pdf
Printable leaflet of the British Kidney Patient Association.
www.ncbi.nlm.nih.gov/pubmedhealth/PMH0071507/
Information for patients and caregivers from PubMed
Health.
www.nhs.uk/conditions/acute-kidney-injury/Pages
/Introduction.aspx
Information from the National Health Service.
7 November 2017 Annals of Internal Medicine ITC79 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
WHAT YOU SHOULD KNOW In the Clinic
Annals of Internal Medicine
ABOUT ACUTE KIDNEY INJURY
What Is Acute Kidney Injury?
Doctors diagnose acute kidney injury (AKI) when
your kidneys stop working properly and the
change happens over a few hours or a few days.
It can cause a buildup of waste products in your
blood and make it hard for your kidneys to bal-
ance the fluids in your body. It can lead to seri-
ous health problems, such as permanent kidney
damage and even death.
AKI usually happens to people who are sick, espe-
cially when they are in the hospital. AKI can be a
complication of the following conditions:
• Sepsis (a type of infection)
• Shock
• Accidents
• Burns • Swelling or retaining fluid
• Heart attack or other heart disease • Shortness of breath
• Blockage of the urinary tract • Feeling dizzy or lightheaded
• Infection of the urinary tract
• Surgery How Is It Diagnosed?
• Dyes for x-rays • Your doctor will ask you questions about your
• Certain over-the-counter and prescription health history and take blood and urine
medicines samples.
• Contact with a poisonous plant or animal • If there is something wrong with your kidneys,
• Severe allergic reaction you may have an imaging test. This could
include an ultrasound.
What Are the Risk Factors?
You are more susceptible to AKI if you: How Is It Treated?
• Are an older adult • Patients with AKI are usually treated in a
• Are female hospital. Your health care provider will give
• Are African American you intravenous fluids to bring your levels
Patient Information
• Have chronic kidney disease back to normal. You may also take medicines
• Have chronic heart, lung, or liver disease to help balance your fluid levels.
• Have diabetes • In more serious cases, you may need dialysis
• Have cancer while your kidneys recover. Dialysis filters the
• Are anemic waste in your body, just as healthy kidneys do.
What Are the Symptoms? Questions for My Doctor
AKI usually has no symptoms until your kidneys • What caused my AKI?
start to fail. Kidney failure means that your kid- • Will I need dialysis?
neys can no longer properly remove waste from • Will I have permanent damage?
your body. These symptoms may occur if you • If I recover, what are the chances I'll get it
have kidney failure: again in the future?
• Feeling sleepy • Should I eat a special diet?
• Feeling sick to your stomach • Should I avoid any medications?
For More Information
National Kidney Foundation
www.kidney.org/atoz/content/AcuteKidneyInjury
Medline Plus
https://medlineplus.gov/ency/article/000501.htm
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Appendix Table 1. Findings of Urine Testing in Acute Kidney Injury
Variable Normal Decreased Obstruction of the Parenchymal Kidney ATN
Kidney Perfusion Urinary Tract Diseases Other Than ATN
Concentration* Varies, depending Concentrated, Concentrated, not if Not concentrated, may Not concentrated;
on water intake possibly not if chronic be concentrated in may be concen-
recent glomerulonephritis trated in heart
diuretic failure or liver
administration failure
Albumin/total Normal to mildly Normal to mildly Normal to mildly Increased albumin Normal to mildly
protein levels† increased increased increased (unless and total protein in increased
chronic) glomerular disease;
normal albumin and
increased total protein
in cast nephropathy
(immunoglobulin light
chains) and in tubular
diseases (2-micro-
globulin)
Hematuria (RBCs)‡ No No Yes, with instrinsic Yes, with dysmorphic No, heme-positive
disease RBCs and RBC casts in dipstick in
glomerulonephritis; yes, hemolysis and
without RBC casts in rhabdomyolysis
thrombotic
microangiopathy
Pyuria (WBCs)‡ No No Yes, if superimposed Yes, with WBC casts in No
urinary tract interstitial nephritis
infection
Renal tubular No No (may contain No (except if Yes Yes
epithelial cells hyaline casts) chronic)
and granular
casts
Hydronephrosis, No No Hydronephrosis, No hydronephrosis, No
kidney shape hydronephrosis, hydronephrosis, enlarged, may be normal size, may be hydronephrosis,
and size§ normal size, normal size, small if chronic, large in infiltrative normal size
symmetrical symmetrical, may be diseases, symmetrical,
may be asymmetrical if may be small if chronic
asymmetrical unilateral,
if renal artery nephrolithiasis
stenosis may be present
RBC = red blood cell; HPF = high-power field; WBC = white blood cell.
* Urine concentration assessed from urine specific gravity (concentrated > 1.020); osmolality (concentrated >500 mosm/kg);
fractional excretion of sodium (FENa) (concentrated <1%); fractional excretion of urea (FEurea) (concentrated <35%); ratio of SUN
to serum creatinine clearance (Scr) >20:1. FENa is calculated from UNa x Scr/SNa x Ucr. FEurea is calculated from UUN x Scr/SUN
x Ucr.
† Albumin and total protein assessed from dipstick (more sensitive to albumin than other proteins); albumin-to-creatinine ratio
(ACR), moderately increased 30 –300 mg/g, severely increased >300 mg/g (nephrotic range >2200 mg/g); and total protein-to-
creatinine ratio (PCR), moderately increased 150 –500 mg/g, severely increased >500 mg/g (nephrotic range >3500 mg/g).
Ranges for ACR and PCR are defined for steady-state conditions; values may be higher in acute kidney injury because urine
creatinine excretion decreases with increased Scr.
‡ Normal urine contains <5 RBC/HPF and <5 WBC/HPF.
§ Renal ultrasonography is the preferred method for evaluating hydronephrosis. Hydronephrosis may be absent in cases of
massive bleeding into the urinary tract or extensive retroperitoneal fibrosis.
姝 2017 American College of Physicians Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Appendix Table 2. Treatment According to Specific Causes of AKI Other Than Acute Tubular Necrosis
Cause of AKI Treatment/Intervention Comment
Decreased kidney perfusion
Volume depletion Intravenous fluid Isotonic crystalloids (normal saline, Ringer lactate, or
balanced crystalloid solutions) are recommended
rather than colloids as initial management for
intravascular volume expansion; improvement in Scr
and eGFR and urine output after intravenous fluid
administration confirms the diagnosis of decreased
kidney perfusion due to volume depletion
Heart failure, left- or right-sided Afterload reduction and Cardiac output may be improved with ACE/ARB,
(with lung disease) (cardiorenal diuretics if volume hydralazine or nitrates; diuresis can improve GFR when
syndrome) overloaded left ventricular filling pressure exceeds that for
optimum cardiac output or when systemic venous
pressure is elevated so as to reduce the afferent versus
efferent arteriolar pressure gradient across the
glomerulus
Liver failure (hepatorenal syndrome) Albumin, midodrine, and Volume may be expanded with albumin, especially in
octreotide setting of bacterial peritonitis or paracentesis;
midodrine and octreotide are used to raise blood
pressure and promote splanchnic vasoconstriction;
terlipressin may improve outcomes (but is not currently
available in the United States or Canada); kidney failure
can be an indication for liver transplant in eligible
patients
Sepsis Intravenous fluid and Intravenous volume expansion and early broad-spectrum
antibiotics antibiotics, subsequently tailored to culture and
sensitivity results
Increased intra-abdominal pressure Intra-abdominal Nasogastric and rectal drainage, and evacuation of
decompression intra-abdominal space-occupying lesions (e.g., ascites,
fluid collections, hematomas); may require surgical
decompression (open abdomen) when
intra-abdominal pressure is ≥20 mm Hg
Renovascular disease Antihypertensive therapy; Angioplasty with or without stenting or surgical bypass of
revascularization the renal artery can be considered in select situations
of AKI (e.g., bilateral renal artery stenosis or stenosis to
a solitary kidney)
Nonsteroidal anti-inflammatory Withdrawal of medications Isotonic crystalloid is a useful adjunct
drugs
ACE inhibitors and ARBs Temporary medication Consider educating patients about tablet holidays
withdrawal (withholding ACE inhibitors or ARBs, especially when
combined with diuretics); during periods of potential
volume depletion from acute illness, to avoid recurrent
AKI episodes
Urinary tract obstruction
Obstructive nephropathy Nephrostomy tube or Percutaneous nephrostomy tubes or ureteric stenting for
urinary catheter relief of upper tract obstruction or Foley catheter or
definitive surgical intervention for lower tract
obstruction
Parenchymal kidney disease
Acute glomerulonephritis Immunosuppressive therapy Dependent on histopathologic findings on kidney biopsy
and underlying cause; crescentic glomerulonephritis
(e.g., anti-neutrophil cytoplasmic antibody and
anti-GBM disease) is usually treated with induction
therapy using steroids and cyclophosphamide;
proliferative lupus nephritis is treated with steroids and
cyclophosphamide or mycophenolate mofetil for
induction therapy; corticosteroids or other
immunosuppressive regimens may be used to treat IgA
nephropathy; when glomerulonephritis is due to an
infection or cancer, these secondary causes should be
treated
Continued on following page
7 November 2017 Annals of Internal Medicine 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Appendix Table 2—Continued
Cause of AKI Treatment/Intervention Comment
Acute interstitial nephritis Withdrawal of culprit Stop culprit drug when medication-related; may consider
medication and corticosteroids if AKI is severe or patient is not
corticosteroids recovering
Acute pyelonephritis Antibiotics Intravenous antibiotics when accompanied by AKI;
consider investigations for anatomical urinary tract
abnormalities, obstruction or stones, or sources of
hematogenous dissemination
Thrombotic microangiopathy Plasma exchange Used for thrombotic thromobocytopenia purpura and
some secondary (immune-mediated) causes of
thrombotic microangiopathy.
Cast nephropathy (multiple Chemotherapy High-dose chemotherapy provided through consultation
myeloma) with a hematologist, which may include steroids,
cyclophosphamide, immunomodulatory drugs (e.g.,
lenolidamide, or proteasome inhibitors (e.g.,
bortezemab) for initial treatement, followed by
autologous hematopoietic cell transplantation for
eligible patients
Renal infarction Revascularization or Consider revascularization for arterial fibromuscular
anticoagulation dysplasia of the renal arteries or anticoagulation for
arterial embolism or venous thrombosis to prevent
recurrence; not indicated for treatment of acute events
Atheroembolism Avoidance of intra-arterial Avoidance of intra-arterial procedures to prevent
procedures recurrence; consider withdrawal of anticoagulation (if
recently initiated) and atheroembolism is spontaneous
(not following intra-arterial procedures)
ACE = angiotensin-converting enzyme; AKI = acute kidney injury; ARB = angiotensin-receptor blocker; eGFR = estimated glo-
merular filration rate; GBM = glomerular basement membrane; GFR = glomerular filration rate; Scr = serum creatinine.
Appendix Table 3. Kidney Replacement Therapies for Hemodialysis and Hemofiltration in Acute Kidney Injury
Example Solute Removal Blood Flow Rate Duration Recommended Dose
Continuous kidney
replacement
therapies
Continuous Convective 150–250 mL/min Daily for 24 h/d (minus To deliver an effluent volume
venovenous interruptions) (replacement for fluid
hemofiltration removed by ultrafiltration)
of 20–25 mL/kg per h
Continuous Diffusive
venovenous
hemodialysis
Continuous Diffusive and
venovenous convective
hemodiafiltration
Intermittent kidney
replacement
therapies
Intermittent Diffusive 200–350 mL/min Typically 3–4 times/wk, To deliver a weekly Kt/V (a
hemodialysis 4 h/session measure of urea clearance)
of 3.9
Prolonged intermittent
kidney replacement
therapies
Sustained low Diffusive 100–300 mL/min Typically daily for ≥6 h To deliver a weekly Kt/V (a
efficiency dialysis measure of urea clearance)
of 3.9
Sustained low Diffusive and
efficiency convective
diafiltration
Sustained continuous Convective
ultrafiltration
姝 2017 American College of Physicians Annals of Internal Medicine 7 November 2017
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
Appendix Figure. Pooled AKI-associated mortality rate from studies based on KDIGO creatinine-based staging.
70
60 49.4
47.8
Pooled AKI-Associated
50
Mortality Rate
40
28.5
30 23.0
15.9
20
10
Overall Stage 1 Stage 2 Stage 3 Dialysis
(KDIGO- (Risk) (Injury) (Failure) Requirement
Equivalent)
Studies, n 110 26 25 25 31
Patients With AKI, n 429 535 8226 42 354 42 354 6534
Error bars represent 95% CIs. AKI = acute kidney injury; KDIGO = Kidney Disease Improving Global Outcomes.
7 November 2017 Annals of Internal Medicine 姝 2017 American College of Physicians
Downloaded From: https://annals.org/ by a Scott Memorial Library User on 12/03/2017
You might also like
- ABGC Practice Exam - No AnswersDocument32 pagesABGC Practice Exam - No AnswersSara WoffordNo ratings yet
- Case Study Guide 2: Awful Pain PillsDocument11 pagesCase Study Guide 2: Awful Pain PillsAila Marie ArandillaNo ratings yet
- Acute Kidney Injury - Seminar Lancet 2019Document16 pagesAcute Kidney Injury - Seminar Lancet 2019Giliana P. García AcevedoNo ratings yet
- Malaria MEQDocument6 pagesMalaria MEQMuvenn KannanNo ratings yet
- NCM 106 - Case Analysis - Nursing Care Plan of Heart FailureDocument2 pagesNCM 106 - Case Analysis - Nursing Care Plan of Heart FailureMarisol Jane JomayaNo ratings yet
- Mbbs BooksDocument7 pagesMbbs Booksbakhem7hbk2002190% (1)
- Acute Kidney InjuryDocument9 pagesAcute Kidney InjuryRobertNo ratings yet
- Chronic Kidney DiseaseDocument11 pagesChronic Kidney Diseasenaly23No ratings yet
- Initial PE and Labs History Initial Impression: Location &Document1 pageInitial PE and Labs History Initial Impression: Location &kaydee.arNo ratings yet
- Drug Induced NephrotoxicityDocument13 pagesDrug Induced NephrotoxicityAgnes BastonNo ratings yet
- Acute Kidney InjuryDocument15 pagesAcute Kidney InjuryManish VijayNo ratings yet
- By B. Shalini Under The Guidance of Neelakant Reddy Patil M.PharmDocument25 pagesBy B. Shalini Under The Guidance of Neelakant Reddy Patil M.PharmShalini Reddy100% (1)
- Approach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDateDocument21 pagesApproach To Acute Lower Gastrointestinal Bleeding in Adults - UpToDateChrista OvalleNo ratings yet
- Clinical Scenario and Worksheet For Diagnostic Appraisal (Journal On Dengue)Document3 pagesClinical Scenario and Worksheet For Diagnostic Appraisal (Journal On Dengue)Stephie E.No ratings yet
- Chronic Glomerulonephritis in DetailDocument9 pagesChronic Glomerulonephritis in Detailfile fileNo ratings yet
- DIC Case StudyDocument7 pagesDIC Case StudyRobertNo ratings yet
- 03 GiDocument76 pages03 Giandirio7486No ratings yet
- Acute Kidney Injury-An UpdateDocument99 pagesAcute Kidney Injury-An UpdateProf Brigadier Mamun MostafiNo ratings yet
- GERDDocument2 pagesGERDRee AhmedNo ratings yet
- Case 7 ResultsDocument14 pagesCase 7 ResultsRegia putri ellandaNo ratings yet
- Clinical Pharmacy Lab - Quiz Part 2Document4 pagesClinical Pharmacy Lab - Quiz Part 2Aassh DcmbrNo ratings yet
- Chronic Renal FailureDocument37 pagesChronic Renal Failuredorkiebaby100% (10)
- Ulcerative ColitisDocument18 pagesUlcerative ColitisHoussein EL HajjNo ratings yet
- 620 General Internal MedicineDocument18 pages620 General Internal Medicinesteven rioNo ratings yet
- Case Study 4th Year 1st Sem 2 Final FixDocument30 pagesCase Study 4th Year 1st Sem 2 Final FixHerschel QuerimitNo ratings yet
- Case Scenario Dengue FeverDocument2 pagesCase Scenario Dengue FeverJaslir MendozaNo ratings yet
- Diagnosis of Gastrointestinal Bleeding in AdultsDocument8 pagesDiagnosis of Gastrointestinal Bleeding in AdultsSaeed Al-YafeiNo ratings yet
- Liver Pathophysiology and Schematic Diagram BGFJNDocument1 pageLiver Pathophysiology and Schematic Diagram BGFJNKate Mylhen Espenido EnerlanNo ratings yet
- Learning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14Document9 pagesLearning Objectives:: Pathophysiology & Therapeutics, I (MSPR 521) Lecture No. 14adzhangNo ratings yet
- SLE Case PresentationDocument29 pagesSLE Case PresentationBlesson JohnNo ratings yet
- Acute Lymphocytic LeukemiaDocument7 pagesAcute Lymphocytic Leukemiamildred alidon100% (1)
- SamplesDocument4 pagesSamplesRalph Lawrence Ruiz Tagorda0% (1)
- ACE InhibitorsDocument2 pagesACE InhibitorsJosephine Irena100% (1)
- Acute Kidney InjuryDocument8 pagesAcute Kidney InjuryRohitKumarNo ratings yet
- Lupus NephritisDocument29 pagesLupus NephritisMuhammad Julpian0% (1)
- A Case of A 61/M Client With Upper Gastrointestinal Bleeding Secondary To Peptic Ulcer DiseaseDocument3 pagesA Case of A 61/M Client With Upper Gastrointestinal Bleeding Secondary To Peptic Ulcer DiseasejohndavennarvaezNo ratings yet
- Anemia in CKD: Ppds Sp1 Divisi Ginjal Hipertensi Bagian Ilmu Penyakit Dalam Rsup Dr. Mohammad Hoesin Palembang 2021Document31 pagesAnemia in CKD: Ppds Sp1 Divisi Ginjal Hipertensi Bagian Ilmu Penyakit Dalam Rsup Dr. Mohammad Hoesin Palembang 2021Richard 151289No ratings yet
- Irritable Bowel SyndromeDocument22 pagesIrritable Bowel SyndromeMarium NabeelNo ratings yet
- Renal TransplantationDocument33 pagesRenal TransplantationRohini Rai100% (1)
- Poststreptococcal GlomerulonephritisDocument19 pagesPoststreptococcal GlomerulonephritisAlex Ismael Catalan CabreraNo ratings yet
- Diabetic Ketoacidosis Is An Extreme Metabolic Hyperosmotiic Hyperglycemic State Is A LifeDocument2 pagesDiabetic Ketoacidosis Is An Extreme Metabolic Hyperosmotiic Hyperglycemic State Is A LifeLyod BalagasayNo ratings yet
- GlomerulonephritisDocument58 pagesGlomerulonephritisJosa Anggi Pratama0% (1)
- Φ PathophysiologyDocument4 pagesΦ PathophysiologyMariah AshooriyanNo ratings yet
- Pa Tho Physiology of Diabetes MellitusDocument3 pagesPa Tho Physiology of Diabetes MellitusPong's Teodoro SalvadorNo ratings yet
- Appendicitis Case StudyDocument2 pagesAppendicitis Case StudyLeviThomasStafford100% (1)
- DiverticulitisDocument15 pagesDiverticulitisElisabeth MelisaNo ratings yet
- Aminogycoside AntibioticsDocument31 pagesAminogycoside AntibioticsNurul Febrina100% (2)
- Gi - PathophysiologyDocument96 pagesGi - Pathophysiologyjmosser100% (4)
- HyperlipidemiaDocument17 pagesHyperlipidemiabent alfay7a2No ratings yet
- Anemia of Chronic Disease - Inflammation - UpToDateDocument36 pagesAnemia of Chronic Disease - Inflammation - UpToDateDomenica MurilloNo ratings yet
- Nosocomial Bloodstream Infection and The Emerging Carbapenem Resistant Pathogen Ralstonia Mannitolilytica: A Case SeriesDocument7 pagesNosocomial Bloodstream Infection and The Emerging Carbapenem Resistant Pathogen Ralstonia Mannitolilytica: A Case SeriesOpenaccess Research paperNo ratings yet
- Gestational Diabetes Mellitus - NISALDocument7 pagesGestational Diabetes Mellitus - NISALKevin de SilvaNo ratings yet
- Acute Glomerulonephritis: Gordon Sara Sonnya Ayutthaya Novita Sari DewiDocument12 pagesAcute Glomerulonephritis: Gordon Sara Sonnya Ayutthaya Novita Sari DewiSara Sonnya Ayutthaya NapitupuluNo ratings yet
- Case Study On Alcoholic Liver DiseaseDocument20 pagesCase Study On Alcoholic Liver DiseaseHomework PingNo ratings yet
- Case Study 1 For Advanced PathophysiologyDocument7 pagesCase Study 1 For Advanced Pathophysiologyapi-270901138No ratings yet
- Hyponatremia and Hypernatremia in The ElderlyDocument15 pagesHyponatremia and Hypernatremia in The ElderlyStacey WoodsNo ratings yet
- Stroke and Cerebrovascular DiseaseDocument14 pagesStroke and Cerebrovascular DiseaseMarwan M.No ratings yet
- Portal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandPortal Hypertension, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- A Simple Guide to Hyperaldosteronism, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hyperaldosteronism, Diagnosis, Treatment and Related ConditionsNo ratings yet
- Necrotizing Fasciitis, (Flesh Eating Disease) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandNecrotizing Fasciitis, (Flesh Eating Disease) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Biomarkers of Kidney DiseaseFrom EverandBiomarkers of Kidney DiseaseCharles L. EdelsteinRating: 3 out of 5 stars3/5 (1)
- Fellowship in DiabetologyDocument2 pagesFellowship in DiabetologyGahsj usjskNo ratings yet
- Postpartum BluesDocument5 pagesPostpartum BluesaolbinarNo ratings yet
- CardioDocument6 pagesCardioGrace GurdielNo ratings yet
- DR Abha Mittal: CollegeDocument64 pagesDR Abha Mittal: CollegeTRH RECRUITMENTNo ratings yet
- Epididymo OrchitisDocument18 pagesEpididymo OrchitisRifqi AlridjalNo ratings yet
- Cultural Beliefs On Disease Causation in The PhilippinesDocument11 pagesCultural Beliefs On Disease Causation in The PhilippinesGizelle Ann Gonzales AlcarionNo ratings yet
- 14Document18 pages14JuliusNo ratings yet
- FICADocument3 pagesFICAIsmi Jihan MidianiNo ratings yet
- Introduction To English For Law (TLE 0813)Document11 pagesIntroduction To English For Law (TLE 0813)ilham naylaNo ratings yet
- Your COVID-19 ResultDocument1 pageYour COVID-19 Resultsebhat lab denekewNo ratings yet
- 10 1080@09273948 2018 1432764Document11 pages10 1080@09273948 2018 1432764Yaaei channelNo ratings yet
- Pathway Leukimia Limfosit AkutDocument99 pagesPathway Leukimia Limfosit AkutElla Meilani100% (1)
- Matter For PGDIPC Course PromotionDocument1 pageMatter For PGDIPC Course PromotionAnkur VasudevaNo ratings yet
- HypertensionDocument36 pagesHypertensionRECEPTION AND DIAGNOSTIC CENTER RDC MEDICAL SECTIONNo ratings yet
- Translate - Indo Eng FINALDocument6 pagesTranslate - Indo Eng FINALJidanNo ratings yet
- The Effect of Testosterone On Thyroid Autoimmunity in Euthyroid Men With Hashimoto's Thyroiditis and Low Testosterone LevelsDocument8 pagesThe Effect of Testosterone On Thyroid Autoimmunity in Euthyroid Men With Hashimoto's Thyroiditis and Low Testosterone LevelsdeboratomeNo ratings yet
- Handbook of OrthodonticsDocument1 pageHandbook of OrthodonticsCarlos Alberto CastañedaNo ratings yet
- Bacteria Causing Respiratory Tract Infections: Damanhour University Faculty of PharmacyDocument7 pagesBacteria Causing Respiratory Tract Infections: Damanhour University Faculty of Pharmacyزياد محمدNo ratings yet
- Capstone ResumeDocument2 pagesCapstone Resumeapi-357214812No ratings yet
- CV SecordDocument4 pagesCV Secordapi-287571981No ratings yet
- Early Detection and Intervention of Autism Spectrum DisorderDocument7 pagesEarly Detection and Intervention of Autism Spectrum DisorderIgnacio WettlingNo ratings yet
- Dental Local Anesthesia and PregnancyDocument4 pagesDental Local Anesthesia and Pregnancy4gen_9No ratings yet
- Standard Precautions: Dr. AntoDocument39 pagesStandard Precautions: Dr. AntoANTO MATHINo ratings yet
- Fluids and Electrolytes SamplexDocument3 pagesFluids and Electrolytes SamplexVincentNo ratings yet
- Letter To Registrar Paramedical Council Regarding Final Syllabus For BSC PA Course Run Under WBUHSDocument27 pagesLetter To Registrar Paramedical Council Regarding Final Syllabus For BSC PA Course Run Under WBUHSArup D. SparrowNo ratings yet
- Fas CaseDocument2 pagesFas Caseanon_378668477No ratings yet
- Slagle AnnotationDocument2 pagesSlagle Annotationapi-270744371No ratings yet
- Occupational Therapy For Inpatients With Chronic Schizophrenia: A Pilot Randomized Controlled TrialDocument6 pagesOccupational Therapy For Inpatients With Chronic Schizophrenia: A Pilot Randomized Controlled TrialAngela EnacheNo ratings yet