Professional Documents
Culture Documents
Neuro Imagenes
Neuro Imagenes
Uploaded by
Andres Alberto Nuñez BellocchioCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuro Imagenes
Neuro Imagenes
Uploaded by
Andres Alberto Nuñez BellocchioCopyright:
Available Formats
KEY POINTS
NEUROIMAGING IN A The AAN
recommends at
DEMENTIA least one
structural scan
in the routine
Maria Carmela Tartaglia, Paolo Vitali, Raffaella Migliaccio, evaluation of
Federica Agosta, Howard Rosen dementia.
A Specific patterns
of atrophy are
ABSTRACT useful in the
As treatment of neurodegenerative disease moves toward therapies aimed at specific differential
molecular abnormalities, the importance of early and accurate diagnosis will increase, diagnosis of
as will the need for sensitive measures for tracking disease progression. Brain imaging, dementia.
using MRI and PET scanning, offers a variety of highly reliable techniques that examine
the structure, chemical content, metabolic state, and functional capacity of the brain.
For all the major neurodegenerative disorders, relatively specific findings can be
identified with some or all of these techniques. New approaches for imaging specific
molecular pathology likely will revolutionize brain imaging and be combined with
established imaging approaches to obtain a complete molecular, structural, and meta-
bolic characterization, which could be used to improve diagnosis, and to stage each
patient and follow disease progression and response to treatment.
Continuum Lifelong Learning Neurol 2010;16(2):153–175.
INTRODUCTION portance of making accurate etiologic
Brain imaging is routinely performed in diagnoses to avoid inappropriately ex-
evaluation of dementias, but it has tra- posing patients to potentially dangerous
ditionally been viewed as making a small medications. Parameters obtained from
contribution to clinical care.1 In most neuroimaging, such as metabolism or ce-
cases, clinicians use brain imaging to rebral volume, can be measured much
rule out obvious explanatory pathology, more accurately than changes in memory
such as tumors, hemorrhages, or other abilities or other clinical factors, making
subacute or chronic pathology. As the imaging an attractive technique for mea- 153
clinical approach to dementia changes suring the response to treatment, both
in the future, however, several factors will in research and in clinical practice. In ad-
require clinicians to rely more heavily on dition, as reviewed in this chapter, neuro-
brain imaging for diagnosis and patient degenerative diseases are associated with
management. The most important an- the development of pathologic changes
ticipated development will be the use of long before the development of functional
treatments targeted at specific molec- impairment (dementia). Thus, neuroim-
ular pathologies, eg, eradication of toxic aging has a potential role in diagnosing
-amyloid in patients with Alzheimer dementing disorders in very early clini-
disease (AD). This will increase the im- cal or even presymptomatic stages.
Relationship Disclosure: Drs Tartaglia, Vitali, Migliaccio, Agosta, and Rosen have nothing to disclose.
Unlabeled Use of Products/Investigational Use Disclosure: Drs Tartaglia, Vitali, Migliaccio, Agosta, and Rosen
have nothing to disclose.
Copyright # 2010, American Academy of Neurology. All rights reserved.
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
KEY POINT
For all these reasons, researchers are sulcal size. These changes probably de-
A Alzheimer
increasingly turning to neuroimaging to velop secondary to decreases in synap-
disease (AD)
shows a establish its role in early and accurate tic density, in addition to neuronal loss
particular diagnosis as well as to investigate how and cell shrinkage. Because every neu-
atrophy pattern changes in brain structure and function rodegenerative disease has a predilection
that includes can be measured over time. A variety of for specific brain systems, particularly
hippocampus imaging techniques are available. The early in the course of disease, each is
and entorhinal goal of this review is to provide a broad associated with tissue loss in particular
cortex as well overview of the various methods used brain regions. In AD, the medial tempo-
as the amygdala, to image neurodegenerative disease. ral lobes, especially the hippocampus
anterior and entorhinal cortex (ERC), are among
parahippocampal COMPUTED TOMOGRAPHY the earliest sites of pathologic involve-
gyrus, corpus AND MAGNETIC RESONANCE ment.2 Accordingly, studies of hippocam-
callosum and its IMAGING pal and ERC volumes have repeatedly
subregions, and
the frontal, Computed Tomography shown decreased hippocampal and ERC
temporal and CT imaging was the first technique to volumes in AD compared with age-
occipital lobes. provide a detailed image of the brain and matched controls (Figure 8-1).3
so has the longest history of use in de- Volume loss in AD is extensive and is
mentia. CT scanning adequately ad- not limited to the hippocampus and ERC
dresses the most basic goal for imaging but includes the frontal, temporal and
in neurodegenerative disease, which is occipital lobes,4 indicating that much of
to rule out alternate pathologies; how- the brain shrinks in AD. Among the re-
ever, such findings are rare. Although gions outside the medial temporal lobes,
CT scanning is still regularly used for the parietal and posterior superior tem-
diagnostic assessments and for studies poral regions on the lateral cerebral
of brain-behavior correlation, research surfaces, and posterior portion of the
on most aspects of degenerative demen- cingulate gyrus on the medial surface
tias has moved away from CT scanning are among the most severely affected
because this technique typically has
lower resolution than MRI scanning and
is not as sensitive to many types of ab-
normalities seen in neurodegenerative
syndromes.
Magnetic Resonance Imaging
154 MRI offers an increasingly diverse ar-
ray of approaches for imaging neurode-
generative diseases, including T1- and
T2-weighted imaging, fluid-attenuated in-
version recovery (FLAIR) (a variation of
T2-weighted imaging), diffusion-weighted
imaging (DWI), diffusion-tensor imaging
(DTI), magnetic resonance spectroscopy,
and functional MRI (fMRI).
Structural MRI/T1-weighted im-
aging. The most common abnormality Coronal MRI through
FIGURE 8-1
detectable using structural imaging in the brain of patient with
Alzheimer disease. Notice
neurodegenerative disease is loss of the enlarged temporal horns due to
brain volume, which is manifested by hippocampal (arrow) atrophy.
decreases in gyral size and increases in
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
(Figure 8-2).5 The utility of regional Longitudinal studies have demonstrated
A Behavioral
volume loss in the diagnosis of AD, how- greater atrophy rates in ERC,7 and the
variant
ever, is still unclear because in most vol- temporal lobe as a whole8 in both AD frontotemporal
umetric studies, at least some overlap and MCI compared with controls. degeneration is
exists between patients and controls, so Structural imaging has also been stud- associated with
that imaging measures correctly identify ied as a means of differentiating various volume loss in
between 80% and 100% of patients, de- causes of dementia from each other. This the ventromedial
pending on the study and the region has been examined extensively in fronto- frontal cortex,
being measured. Given that most of temporal degeneration (FTD), in which the posterior
these patients are clearly demented at MRI has revealed unique patterns of brain orbital frontal
the time of study, the added value of atrophy. (See the chapter ‘‘Frontotem- regions, the
insula, and the
imaging in this setting is unclear. poral Degeneration, page 191, for ex-
anterior cingulate
MRI has also been used to study pa- planation and discussion of terminology
cortex.
tients with mild cognitive impairment for FTD). In patients with the behavioral
(MCI), who have memory concerns and variant of FTD, frontal lobe volumes are
impairments on cognitive testing that are reduced compared with those of both
not impeding daily function. Patients AD patients and age-matched controls,
with MCI are at high risk for progression but most striking is the pattern of fron-
to AD, converting to dementia at a rate tal lobe changes. While some lateral
of about 12% to 15% per year. MRI stud- frontal lobe atrophy occurs with AD,
ies in MCI have shown that hippocam- FTD is uniquely associated with volume
pal volumes and cortical volumes in the loss in the ventromedial frontal cortex,
parietal and lateral temporal regions the posterior orbital frontal regions, the
could predict the likelihood of progres- insula, and the anterior cingulate cortex
sion,6 although precise prognostication (Figure 8-2).9 These regions are frontal
in an individual is still not achievable. components of the brain’s emotional
155
FIGURE 8-2 Voxel-based morphometry analysis. A, Volume loss in Alzheimer disease (AD)
compared with controls is not limited to the hippocampus and entorhinal cortex.
Other regions showing reduced volume in AD include the parietal and posterior
superior temporal regions on the lateral cerebral surfaces, and posterior portions of the cingulate
gyrus on the medial surface are among the most severely affected. B, In the behavioral
variant frontotemporal degeneration (FTD), frontal lobe volumes are reduced compared with
age-matched controls. Volume loss occurs in the ventromedial frontal cortex, the posterior orbital
frontal regions, the insula, and the anterior cingulate cortex.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
KEY POINTS
processing systems so that their involve- sonian dementias. In progressive supra-
A Patients with
ment in FTD explains the unique behav- nuclear palsy, third ventricle dilatation
semantic variant
show marked ioral symptoms seen in that disorder. In and midbrain atrophy with shortening of
loss of volume in contrast, patients with the semantic var- the anteroposterior length of the midbrain
the temporal iant of FTD have relative preservation are reportedly characteristic (Figure 8-4).
lobes, in of frontal lobe volumes but marked loss Direct measurement of midbrain size has
particular the of volumes in the temporal lobes, in yielded mixed results, with some studies
neocortex in the particular the neocortex in the tempo- showing good differentiation of progres-
temporal pole. ral pole (Figure 8-3).9 Patients with the sive supranuclear palsy from other de-
A Specific patterns semantic variant of FTD also have atro- mentias, and others showing overlap
of regional phy in the amygdala, which is a critical between syndromes. In corticobasal degen-
volume loss structure for emotional processing.9 eration, classical descriptions have stressed
have been Several studies have highlighted the asymmetric parietal lobe atrophy. How-
described in clinical utility of these patterns of re- ever, more recent analyses have indicated
parkinsonian gional atrophy. For example, frontal lobe that corticobasal degeneration is asso-
dementias. In volumes correctly classify 93% of patients ciated with as much frontal as parietal
progressive with FTD compared with controls.10 Many atrophy, and the diagnostic value of
supranuclear
studies have also demonstrated relation- asymmetric volume loss has been called
palsy, third
ships between local changes in brain vol- into question by recent studies indicat-
ventricle
ume and cognitive or behavioral changes ing that this pattern can be associated
dilatation and
midbrain in dementia. In AD, for example, several with several types of pathology.15 De-
atrophy with studies have found correlations between mentia with Lewy bodies is associated
shortening hippocampal volumes and episodic mem- with diffuse atrophy, and no established
of the ory performance, consistent with the long- pattern is characteristic on structural MRI.
anteroposterior established role for this structure in Some forms of spinocerebellar atro-
length of the memory consolidation.11 Many studies phy are associated with cognitive impair-
midbrain are of non-AD dementias, particularly FTD, ment and are typically associated with
reportedly have yielded findings that shed light on both cerebellar and cerebral atrophy
characteristic. poorly understood brain functions, in- along with caudate and putamen atro-
A In corticobasal cluding language and word access,12 phy in some variants.15
degeneration understanding of facial expressions of T2-weighted imaging, FLAIR, and
(CBD), classical emotion,13 and empathy.14 vascular changes. T2-weighted and
descriptions Specific patterns of regional volume FLAIR images are typically more sensitive
have stressed loss have also been described in parkin- than T1-weighted structural imaging
asymmetric
156 parietal lobe
atrophy, but
more recent
analyses have
indicated that
CBD is associated
with as much
frontal as
parietal atrophy,
and the
diagnostic
value of
asymmetry has
been questioned. MRI coronal (A) and axial (B) view of patient with semantic
FIGURE 8-3
variant. Significant left temporal atrophy with relative sparing
of medial temporal region is present.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
A T2-weighted
and FLAIR
images are
typically more
sensitive than
T1-weighted
structural
imaging to
edema and
gliosis, which
show up as
increased
(bright) signal.
Common
neurodegenerative
FIGURE 8-4 Sagittal and axial MRI sections of a patient with progressive
supranuclear palsy. A, Arrow on sagittal view points to flattening disorders such
of midbrain superior colliculi. The atrophy of the midbrain results as AD and
in a convex upper border of the midbrain with the typical humming bird sign. frontotemporal
B, Arrows on axial view indicate flattened superior colliculi.
degeneration
tend to show
no major
changes on
to cerebral pathology characterized by executive impairment.17 In subcortical vas- T2/FLAIR.
edema and gliosis, which appear as cular dementia, the pattern of white mat- A FLAIR imaging is
increased (bright) signal on T2 weight- ter abnormality can help to identify the very sensitive to
ing. Common neurodegenerative dis- underlying cause. Lesions in periventric- injury caused by
orders such as AD and FTD tend to ular and deep white matter are usually ischemia from
show no major changes on T2/FLAIR, al- associated with small vessel cerebrovas- both small
though these can be seen in some cases, cular disease (eg, systemic hypertension, vessel and large
particularly when severe atrophy is present. vessel disease.
Small vessel
T2/FLAIR imaging is, however, very sen-
disease causes
sitive to injury due to ischemia from both
incomplete or
small vessel and large vessel disease. Small complete
vessel disease causes incomplete or com- infarcts in the
plete infarcts in the white matter or in white matter or
subcortical gray matter nuclei.16 On FLAIR in subcortical
images, incomplete infarcts appear as hy- gray matter
157
perintensities, whereas complete infarcts nuclei. On
present as lacunes, which are hypoin- FLAIR images,
tense to the brain and isointense to the incomplete
CSF (Figure 8-5). Lacunar strokes are infarcts appear
small complete infarcts (2 mm to 15 mm). as hyperintensities,
whereas
Small vessel disease identified on MRI in
complete
the white matter has been called leuko-
infarcts present
araiosis and appears as multiple punc- as lacunes,
tuate or confluent T2 bright lesions. A which are
FIGURE 8-5 Axial fluid-attenuated
mild amount of leukoaraiosis is commonly inversion recovery image hypointense
seen in healthy older adults. Quantitative from a patient with to the brain
MRI studies in nondemented elderly sub- vascular dementia showing multiple patchy
areas of high signal in periventricular and isointense
jects demonstrate that the total volume of white matter. to the CSF.
subcortical lesions correlates with frontal
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
KEY POINT
diabetes, hyperhomocysteinemia) or T2/FLAIR imaging also reveals some
A Small vessel
acute hypotensive states (eg, orthostatic important findings in non–vascular
disease
identified on hypotension, congestive heart failure, degenerative diseases. For example, in
MRI in the arrhythmias).16 The involvement of sub- multiple system atrophy (MSA), T2/FLAIR
white matter is cortical white matter, often with small imaging often shows a posterolateral
called cortical infarcts, can be caused by cardiac, putaminal hypointensity, mainly due to
leukoaraiosis, aortic, or carotid microemboli, vasculitis, iron deposition, with a hyperintense rim,
which appears and cerebral autosomal dominant arterio- mainly due to gliosis. A combination of
as multiple pathy with subcortical infarct and leu- T2* gradient-echo sequences and FLAIR
punctuate or koencephalopathy.18,19 In vasculitis, MR shows fair accuracy in differentiating
confluent angiography shows some abnormalities in MSA from Parkinson disease.15 MSA also
lesions, but the minority of cases in which large vessels shows degeneration of transverse pon-
more often as
are involved, and paramagnetic contrast tine fibers as the characteristic ‘‘cross’’
incomplete
infarcts. It
injection may show brain or vessel wall sign (also called the hot cross bun sign),
is commonly enhancement, but the diagnosis usually which is also associated with middle ce-
seen in healthy requires angiography or brain biopsy.20 rebellar peduncle hyperintensity and with
older adults. T2/FLAIR imaging is also sensitive to pontine atrophy (Figure 8-7).
microhemorrhages. These are charac- Limbic encephalopathies often have
teristically hypointense lesions because T2-weighted medial temporal lobe and/or
cerebral iron deposition leads to local patchy white matter hyperintensity
inhomogeneities in the magnetic field. (Figure 8-8).23 Many rapidly progressive
These may be seen in up to 65% of cases dementias can cause leukoencephalop-
diagnosed with vascular dementia.21 T2* athy, including progressive multifocal leu-
gradient-echo images are most sensitive koencephalopathy and leukodystrophies,
to these findings (Figure 8-6). In amyloid or mixed gray and white matter involve-
angiopathy, unlike hypertension-related ment, such as mitochondrial diseases and
lesions, microhemorrhages are more fre- intravascular lymphoma.24 Infections and
quently located at the cortico-subcortical toxic condtions can also be a cause of
junctions in frontomesial, frontoorbital, dementia and are discussed in other sec-
and parietal regions.22 tions of this issue. MRI with contrast
158
FIGURE 8-6 A, Coronal and (B) axial gradient-echo MR images showing
multiple microhemorrhages.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
A DWI is useful
for diagnosing
Creutzfeldt-
Jakob disease
(CJD).
Decreased
diffusion in
cerebral cortex
(called cortical
ribboning) is
associated with
decreases in the
basal ganglia
FIGURE 8-7 A, Sagittal T1- and (B) axial T2-weighted images of a patient
with multiple system atrophy. Notice the pronounced cerebellar, and is highly
cerebellar peduncles, and pontine atrophy. On sagittal view, sensitive and
notable flattening of the pons is present. On axial view, note the hyperintense specific for the
brachium pontis and cruciform pattern (hot cross bun sign) in the pons as a result
of sparing of the pyramidal tracts. diagnosis of
CJD. Variant
CJD is often
associated
with high
should be used in the evaluation of most diffusion in cerebral cortex (called cortical signals in the
rapidly progressing dementias. ribboning) with associated decreases in pulvinar region
Diffusion-weighted imaging and the basal ganglia is highly sensitive and giving the
diffusion-tensor imaging. DWI is based specific for the diagnosis of CJD (sensitivity pulvinar sign.
on the analysis of the random motion of 91%, specificity of 95%) (Figure 8-9).25
of water molecules in the brain. DWI Variant CJD is often associated with high
images are grossly normal in most neu- signals in the pulvinar region.26
rodegenerative diseases; however, in Abnormal DWI can also be seen in other
Creutzfeldt-Jakob disease (CJD), decreased rapidly progressive dementias, including
Bartonella encephalopathy, Wernicke en-
cephalopathy and Wilson disease,27–29
while antibody-mediated encephalopa-
thies and neurofilament inclusion body
dementia can have FLAIR hyperinten-
sity in the cortex and/or deep nuclei. In
these condtions, unlike prion disease, 159
the underlying white matter is also of-
ten involved.30 Seizures, including non-
convulsive status epilepticus, can result
in cortical ribboning on DWI, but this
should resolve a few days after cessation
of seizures.31
DWI images represent an average of
diffusion in the three main directions
(right/left, front/back, up/down), and thus
FLAIR coronal view
the signal in each voxel of a DWI image
FIGURE 8-8 does not tell about the direction of
showing hyperintense
hippocampi in a patient movement of the water molecules. An
with autoimmune voltage-gated potassium
channel limbic encephalitis. important variation of DWI is DTI, which
represents the directional diffusion of
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
KEY POINT
A DTI represents
the diffusion
of water
in three
dimensions. In
axonal fibers,
an ordered
arrangement
of cells causes
the diffusion
of water to be
significantly
greater along
the axis of
those fibers
(anisotropic
FIGURE 8-9 Axial diffusion-weighted imaging showing cortical ribboning left
diffusion). greater than right in a patient with Creutzfeldt-Jakob disease.
water by tracking movement in three callosum.32 Recently, Zhang and col-
dimensions and providing information leagues identified reduced FA in the
on the predominant direction of diffu- portion of the cingulum bundle con-
sion within each voxel. This is done by necting the hippocampus to the poste-
measuring the movement of water out rior cingulate region in patients with
of each voxel in many different direc- MCI and AD compared with controls. The
tions, currently as many as 50 or 60. In use of this measure provided improved
certain biological structures, such as ax- classification of patients from controls
onal fibers, an ordered arrangement of compared with hippocampal volumes
cells causes the diffusion of water to alone.33 White matter tract integrity has
be significantly greater along the axis also been correlated with measures of
of those fibers (anisotropic diffusion, episodic memory in AD and MCI.34
meaning that diffusion is not the same DTI is also being used more to ex-
in all directions). Fractional anisotropy amine differences across dementia sub-
(FA) is a measure of the degree of an- types. A recent study found decreased
160 isotropy of a diffusion process. A value FA in the parietal lobes in dementia with
of zero means that diffusion is isotro- Lewy bodies compared with AD, con-
pic, ie, unrestricted in all directions, sistent with metabolic studies and the
whereas a value of one means that dif- prominent visuospatial difficulties often
fusion occurs only along one axis and seen in these patients.35 In a recent study
is fully restricted in other directions. comparing AD and FTD, it was shown
Therefore, FA can provide information that patients with FTD had reduced FA in
on the orientation and integrity of frontal and temporal regions, including
fibers. Although most of the pathology the anterior corpus callosum, bilateral
in neurodegenerative diseases, particu- anterior and descending cingulum tracts,
larly in AD, occurs in gray matter, several and uncinate fasciculus, compared to
recent studies have documented abnor- controls (Figure 8-10A), while patients
malities in white matter in AD, specifically with AD had reduced FA in parietal, tem-
in temporal lobe white matter, poste- poral and frontal regions, including the
rior cerebral white matter, and corpus left anterior and posterior cingulum tracts,
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
FIGURE 8-10 A and B represent anterior to posterior coronal slices of regional
fractional anisotropy (FA) between groups (voxel-wise analysis).
A, FTD<CN shows FA reductions in frontotemporal degeneration (FTD)
relative to normal controls involving the anterior frontal and temporal brain. B, FTD<AD
shows FA reductions in FTD relative to Alzheimer disease (AD) indicating FTD had
significantly lower FA in vast regions of bilateral frontal lobes, including anterior corpus
callosum, bilateral anterior cingulate gyrus, uncinate fibers, and anterior limb of internal
capsule. The areas with significantly decreased FA values are marked in warm colors
with threshold PFDR = 0.05.
CN = cranial nerve.
Figure courtesy of Yu Zhang, University of California, San Francisco.
bilateral descending cingulum tracts, and cused on NAA content in patients with
left uncinate fasciculus.36 This work dem- dementia. In patients with AD compared
onstrated not only that the location of with cognitively normal elderly subjects,
white matter abnormalities was specific NAA is consistently reported as lower in 161
for the frontal lobes in FTD (as would be various portions of the brain, particularly
expected) but also that the magnitude in the parietal gray matter and hippocam-
of white matter changes is larger in FTD pus.37 In vascular dementia the greatest
than in AD (Figure 8-10B). losses occur in the frontal and parietal
Magnetic resonance spectroscopy cortex.38 Myo-inositol, a marker associ-
with MRI. In vivo proton magnetic res- ated with gliosis, has also been reported
onance spectroscopy (1H MRS) with MRI as high in patients with AD.39 Decreased
allows noninvasive sampling of brain NAA and increased myo-inositol have
chemistry by measuring the levels of also been reported in MCI.40
1
relatively few specific metabolites, in- H MRS has been used in a few stud-
cluding N-acetylaspartate (NAA), choline, ies of non-AD dementias, including FTD,41
creatine, lactate, and glutamate. Because prion diseases,42 Huntington disease,43
NAA is thought to be a marker of neu- and AIDS dementia complex.44 In one
ronal integrity, many studies have fo- study comparing AD and FTD patients,
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
the NAA/creatine ratio was reduced in studies have shown increased activation
the posterior cingulate cortex in the pa- in AD or MCI, others have shown a
tients with AD and FTD/Pick disease, but combination of increased activation in
the patients with AD showed a greater some regions and decreases in others,
decrease posteriorly while the patients while others have seen only decreases.47
with FTD/Pick complex displayed greater Increases in activation are often inter-
frontal decrease.41 1H MRS has been used preted as evidence of compensatory pro-
relatively infrequently for brain-behavior cessing, but whether this is true and the
correlations. nature of this compensation are unknown.
Iron-dependent T2 contrast with fMRI has had limited use in non-AD
MRI. Iron-dependent T2 contrast has dementias. Rombouts and colleagues
been reported as increased in a number studied verbal working memory in early
of regions in AD, including the hippo- FTD and AD and found decreased acti-
campus, ERC, globus pallidus, putamen, vation in frontal and parietal regions in
and caudate.45 Although the significance FTD.48 The FTD group displayed a stronger
of the increased iron is still being in- response in the cerebellum, which was
vestigated, a growing body of literature interpreted as a possible compensatory
suggests that altered iron metabolism or mechanism. A recent study also showed
its accumulation is associated with toxic- increased temporal lobe activation in
ity or cell injury. Susceptibility-weighted dementia with Lewy bodies compared
imaging is an emerging technique that with AD on a visual motion processing
uses the information not only from the task.49 It is not yet clear what parame-
magnitude of a gradient-echo MRI se- ters predict increased versus decreased
quence signal, but also from the phase of activation for a given cognitive task.
the signal. The phase shift is strongly Until this is better understood, the role of
dependent on the susceptibility of the fMRI in diagnosis or monitoring of pa-
tissues to the local inhomogeneities in tients with dementia will remain unclear.
the magnetic field. Resting state functional MRI. The
Functional activation using MRI. variability in metabolic activity during
fMRI permits the measurement of brain periods when subjects are not actively
activity related to cognitive processing engaged in cognitive processing, either
because increased synaptic activity leads between blocks of trials of a cognitive
to local increases in blood flow. The task or during passive resting in the MRI
resulting changes in oxyhemoglobin/ scanner, has also proven relevant to de-
deoxyhemoglobin ratio alter the local mentia. Several regions across the brain,
162 magnetic properties in the brain,46 re- often with related functions, covary in
sulting in blood oxygen level-dependent terms of the rise and fall of their blood
signal. The ability provided by MRI to oxygen level-dependent signal during
indirectly measure synaptic activity in these periods. The resulting networks
response to cognitive demands provides of regions seen with this kind of analysis
a measure that may be the best correlate have been referred to as resting state net-
of cognitive performance and a promis- works, and several networks have been
ing technique for following disease pro- identified.50 The default mode network,
gression and treatment response. The which includes the posterior cingulate,
tasks can be tailored to examine specific inferior parietal, inferolateral temporal,
domains of function pertinent to whatever ventral anterior cingulate, and hippo-
subtype of dementia is being studied. campal regions, has received the most
A number of investigators have exam- attention in AD (Figure 8-11), and has
ined brain activation patterns in demen- been shown to have decreased activity
tia, with complex results. While several in AD and MCI. This is consistent with
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
A PET is most often
used with [18F]-
fluorodeoxyglucose
(FDG) to measure
brain energy
metabolism.
SPECT is most
commonly used
to study cerebral
perfusion with
compounds such
as HMPAO.
These techniques
FIGURE 8-11 Resting state data of default mode network and some key nodes from a group
analysis of 15 healthy young subjects’ resting-state data. The z-score can theoretically
distribution is shown on the color bar to the right. Key nodes in the network reveal metabolic
are indicated by green arrows. abnormalities in
MPFC = medial prefrontal cortex; PCC = posterior cingulate cortex; RSC = retrosplenial cortex; structurally
IPC = inferior parietal cortex; HC = hippocampus. normal brain.
Figure courtesy of Michael Greicius, MD, Stanford University.
A FDG-PET
demonstrates
reduced
glucose
the structural data reviewed in this potential in dementia were conducted metabolism in
chapter highlighting these regions as be- with metabolic imaging using radioactive the parietal and
ing affected particularly severely in AD. materials. The most commonly used tech- superior/
Other networks may have relevance to niques are SPECT and PET. Both tech- posterior
other dementias. For instance, a ‘‘salience’’ niques can be used to measure a variety of temporal
network that includes the dorsal ante- physiologic parameters in the brain using regions of
rior cingulate and orbital/frontoinsular various chemical compounds. PET is most patients
regions and tracks with emotional mea- often used with [18F]fluorodeoxyglucose with AD.
sures may be more relevant to FTD.51 (FDG) to measure brain energy metab-
The precise functions of these networks olism. SPECT is most commonly used to
and the physiologic basis of alterations study cerebral perfusion with compounds
in their functions have yet to be deter- such as 99mTc-hexamethylpropyleneamine
mined. However, their use in dementia oxime. These techniques theoretically
is attractive because they can be studied provide unique information about brain
in nearly any patient who can have an states relative to structural imaging be- 163
MRI scan, in contrast to the sometimes cause they can show metabolic abnor-
complex paradigms used for fMRI acti- malities in structurally normal brain.
vation studies. FDG-PET demonstrates reduced glu-
cose metabolism in the parietal and
POSITRON EMISSION superior/posterior temporal regions of
TOMOGRAPHY: GLUCOSE patients with AD. (Figure 8-12, top;
METABOLISM AND BRAIN arrows point to regions of hypometabo-
PERFUSION lism). Very early metabolic deficits occur
in AD and in MCI in the medial portion
Positron Emission Tomography of the parietal cortex, the posterior cin-
and Single-Photon Emission gulate, or retrosplenial region.52 Frontal
Computed Tomography lobe hypoperfusion is often also reported
The earliest studies documenting re- in AD but usually in conjunction with
gional abnormalities with real diagnostic temporoparietal abnormalities.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
KEY POINT
Patterns of metabolic abnormality may that temporoparietal metabolism mea-
A In contrast
differ according to dementia subtype. In sured using FDG-PET can distinguish pa-
to AD,
frontotemporal contrast to AD, FTD is associated with tients with MCI with a progressive course
degeneration is hypometabolism in the frontal and ante- from those with a nonprogressive course.55
associated with rior temporal regions, with relative sparing Posterior cingulate hypometabolism on
hypometabolism of posterior brain regions (Figure 8-12, SPECT has also been used to predict
in the frontal bottom). Dementia with Lewy bodies progression in this setting.56
and anterior is associated with decreased occipito- Altered regional brain metabolism has
temporal regions, temporal metabolism compared with been linked to specific cognitive and be-
with relative AD, consistent with the increased dif- havioral changes in dementia. Haxby and
sparing of ficulty such patients have with visual colleagues used PET to demonstrate that
posterior brain
processing.53 right-left hemisphere metabolic asym-
regions.
Studies investigating the diagnostic metry in AD was correlated with the
utility of these findings suggest that they degree of language versus visuospatial
are helpful in discriminating patients with impairment.57 Memory impairment has
clinically diagnosed AD from age-matched been linked to hippocampal hypometabo-
controls as well as from patients with lism,58 and behavioral/emotional varia-
vascular dementia and FTD.52 A recent bles, such as apathy, have been linked to
study of AD and FTD patients whose hypometabolism in the anterior cingu-
diagnoses were ultimately confirmed at late region.59
autopsy showed that FDG-PET increases Imaging of neurotransmitter sys-
diagnostic accuracy beyond clinical fea- tems with PET. PET and SPECT are
tures alone.54 capable of visualizing many physiologic
Metabolic imaging can also be useful parameters beyond perfusion and glu-
for prognosis. Some studies have found cose metabolism. One approach that
takes unique advantage of these capa-
bilities is the study of neurotransmitter
systems using molecules that bind to
neurotransmitter receptors or interact
with neurotransmitter systems in other
ways. For example, imaging of the cho-
linergic system in AD is possible using a
variety of agents that interact with ace-
tylcholine receptors and acetylcholines-
terase, a key enzyme whose function
164 decreases in AD.60 This type of imaging
could be helpful in guiding therapy by
establishing parameters to predict who
would respond best to neurotransmit-
ter manipulation and by following the
effects of treatment. In fact, PET imaging
FIGURE 8-12 FDG-PET in AD and FTD. In AD, notice has shown significant increases in 11C-
reduced glucose metabolism in superior/
posterior temporal and parietal regions nicotine binding sites after 3 months of
(arrows). In FTD hypometabolism is present in the frontal treatment with rivastigmine, and this
and anterior temporal regions, with relative sparing of
posterior brain regions (arrows).
correlates with improvements on atten-
tional tasks at 12 months.61
FDG-PET = [18F]Fluorodeoxyglucose–positron emission
tomography; AD = Alzheimer disease; FTD = frontotemporal Measurement of cholinergic function
degeneration. also has applications outside the context
Figure courtesy of Gil Rabinovici, MD, University of California, San Francisco. of typical AD. For instance, cognitive
deterioration in patients with Parkinson
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
disease may be caused by spread of Lewy included seven patients with a clinical
A PET ligands can
body pathology outside the substantia diagnosis of AD and 12 with FTD. All
be used to image
nigra or the development of superim- patients with AD (7/7) had increased disease-specific
posed AD. In either case, effects on cho- 11C-PiB retention by visual inspection, molecular pathology.
linergic function are likely. A recent PET while most (8/12) patients with FTD and Agents that bind
study with N-[11C]-methyl-4-piperidyl five (5/5) controls had no increase in to plaques
acetate (MP4A), which labels acetylcho- 11C-PiB retention, consistent with the containing -amyloid
line systems, and 18F-fluorodopa (FDOPA) proposal that non-AD dementia will not can be seen
evaluated cholinergic and dopaminergic usually show increased 11C-PiB reten- with radiolabeled
function in Parkinson disease patients tion (Figure 8-13).64 The increased Pittsburgh
with dementia and without dementia.62 11C-PiB retention in the four patients compound B
While FDOPA uptake in the striatum was with FTD may represent AD pathology (11C-PiB) and help
to establish a
decreased in both groups, cortical MP4A
diagnosis of AD.
binding was severely decreased in patients
with Parkinson disease with dementia
compared with controls, but only mod-
erately decreased in patients with Parkin-
son disease alone. The ability to measure
each of these neurotransmitters systems
could help to guide treatments specific
to each system.
Amyloid imaging with PET. The
recent development of new PET ligands
for imaging disease-specific pathology may
revolutionize brain imaging in neurode-
generative disease. Specifically, studies
with agents that bind in vivo to plaques
containing -amyloid, such as radio-
labeled Pittsburgh compound B (11C-PiB)
have demonstrated marked retention of
11C-PiB in the frontal, parietal, tempo-
ral, and occipital cortices as well as the
striatum in patients with AD compared
with controls.52 Because 11C-PiB labels
amyloid plaques that are not normally
present in healthy brains, 11C-PiB im- 165
ages in patients with AD usually appear
dramatically different than images from
healthy controls, allowing easy visual
interpretation of PiB images. The short FIGURE 8-13 Axial slices of mean 11-C Pittsburgh
compound B images (normalized to
half-life of 11C-PiB requires that the PET cerebellum) in patients clinically diagnosed
center have a cyclotron, which may ulti- with AD (top row, N = 27, mean age 67.1+/-9.9), FTD (middle
mately limit the utility of 11C-PiB and row, N = 31, mean age 64.5+/-7.5), and cognitively normal
controls (bottom row, N = 12, mean age 73.9+/-6.1).
favor other agents. Patients with AD show tracer uptake throughout frontal,
Since the first reports on 11C-PiB, sub- parietal, lateral temporal cortex, and striatum, while most
patients with FTD and controls show only mild nonspecific
sequent studies have shown increased tracer binding in white matter.
PiB retention in patients with MCI,63 AD = Alzheimer disease; FTD = frontotemporal degeneration.
and several reports have examined PiB
Figure courtesy of William Jagust, MD, University of California, Berkeley, and Gil
retention in non-AD dementias. A re- Rabinovici, MD, University of California, San Francisco.
cent study by Rabinovici and colleagues
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
mimicking the clinical presentation of FTD, CONCLUSION
or it may represent coexisting pathol- Brain imaging offers an increasingly wide
ogy. In addition to PiB, other approaches array of techniques for studying the
for imaging specific molecular pathology changes associated with neurodegener-
in neurodegenerative disease are under ative disease (summarized in Table 8-1).
development, thus far only in AD.52 In addition to the approaches highlighted
While molecular imaging is a very prom- in this chapter, which primarily utilize
ising approach for diagnosis of neu- MRI, PET, and SPECT, other approaches
rodegenerative disease, results of this for quantifying changes in the brain, in-
technique should be interpreted cau- cluding EEG and magnetoencephalog-
tiously as it gains wider use. The pres- raphy, could be considered ‘‘imaging’’
ence of increased PiB retention should approaches, because they depict regional
not be considered tantamount to a diag- changes across the brain; they are, how-
nosis of AD. The few studies in non-AD ever, beyond the scope of this chapter.67
dementias have highlighted the fact that Despite the availability of methods for
complex results may emerge, and the in- imaging many aspects of structure and
terpretation of these findings will require function, including white matter tract in-
much more study. In addition, 11C-PiB tegrity, neurotransmitter function, task-
studies have demonstrated increased related synaptic activity, and chemical
retention in up to approximately 20% to content, the bulk of imaging research in
30% of healthy older individuals who dementia is still focused on regional ab-
are cognitively normal.65 Whether such normalities in glucose metabolism, per-
patients are destined to develop demen- fusion, and tissue content. The simple
tia is still an open question. The fact that goal of making early and accurate diag-
increased 11C-PiB retention can occur nosis solely with imaging has not been
in cognitively normal individuals is con- achieved for the common degenerative
sistent with pathologic studies indicat- diseases, although DWI has emerged as
ing that up to approximately 37% of au- a critically important diagnostic tool in
topsies in patients who were cognitively CJD. In certain contexts, such as differ-
normal prior to death show pathology entiation of FTD from AD, imaging can
meeting National Institute on Aging– be a valuable addition to the clinical as-
Reagan criteria for a high or intermediate sessment. The arrival of amyloid imag-
likelihood of AD.66 As the review above ing may herald the emergence of a new
clearly demonstrates, however, many era in which imaging of the specific mo-
166 other techniques capable of tracking lecular abnormality associated with each
function over varying time intervals are degenerative syndrome will be possible.
available to image changes in brain oc- However, we must be cautious as we
curring secondary to neurodegenera- embrace this technology to avoid over-
tive disease. Techniques for imaging diagnosis and to recognize the possibil-
specific molecular pathology such as ity of multiple metabolic abnormalities
11C-PiB will likely be combined with accounting for a patient’s clinical pre-
one or more of these other imaging sentation. The future of brain imaging
techniques to identify molecular abnor- will likely involve combinations of imag-
malities and to quantify their effects ing techniques to identify the presence of
in the brain. Case 8-1 demonstrates a molecular abnormality, to gauge its
the utility of combining several imag- impact on the brain structure and func-
ing techniques to make a more accurate tion, and to predict and follow the effects
diagnosis. of treatment.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Case 8-1
A 55-year-old left-handed man had a 9-year
history of profound behavioral changes,
including compulsive sorting of recyclable
items, disinhibition, and socially inappropriate
behavior (eg, stripping naked at a family
beach outing, pretending to be blind so
that his dog would be allowed on a train,
hanging a dead bird on a clothesline).
He was insatiable and would eat as long
as food was present, and he would take food
from other peoples’ plates. He occasionally
ate food that was spoiled. His wife FIGURE 8-14 Coronal (left) and axial (right) sections
from T1-weighted MRI.
reported that he had become much
more self-centered and flat in emotional
expression. When his mother, with whom
he was very close, died, he showed no
emotion. He was irritable and occasionally
he became so angry that his wife was fearful
for her safety. She was not able to reason
with him, as he had no insight. He was
distractible and often failed to complete
tasks. He developed several repetitive
motor behaviors, including frequent
yawning, rubbing the edges of his mouth
with his finger, and throat clearing. Past
medical history and family history were
noncontributory.
His neurologic examination was
unremarkable. On neuropsychological
examination, he scored 20/30 on the
Mini-Mental State Examination and showed
deficits in episodic memory, visuospatial
tasks, and executive function. Language
was relatively spared.
MRI demonstrated predominantly
biparietal atrophy (Figure 8-14), and FIGURE 8-15 Results of (A) a Pittsburgh compound B (PiB)
FDG-PET showed a corresponding biparietal
PET scan and (B) 2-[18F]fluoro-2-deoxy-D- 167
glucose–PET scan obtained 27 months after
reduction in glucose metabolism initial presentation. A, PiB scan reveals amyloid in the brain;
(Figure 8-15). PiB PET showed increased warmer colors (eg, red) indicate greater concentrations of
amyloid deposition, and blue indicates the absence of
PiB retention. amyloid. B, The FDG-PET scan shows biparietal
Comment. This patient presented with the hypometabolism. On an FDG-PET scan, warmer colors
indicate greater metabolism, a sign of healthy brain.
classical symptoms of the behavioral variant
of FTD, but the pattern of brain atrophy Figure courtesy of Gil Rabinovici, MD, University of California, San Francisco.
and hypometabolism both suggested a
significant parietal disease, as seen in AD. PiB PET confirmed the presence of -amyloid,
strongly suggesting AD pathology in this case. In retrospect, the poor performance on visuospatial
testing was a clue to the parietal disease. The significance of the -amyloid remains to be clarified.
This case may represent a patient with AD presenting with the symptoms of FTD, or it may
reflect a more complex process, such as the coexistence of two pathologies: those of AD and FTD.
In either case, the identification of specific molecular pathology as seen in this patient will be
critically important as more specific therapies emerge.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
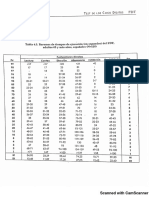
TABLE 8-1 Summary of Imaging Findings in Various Dementias
Mild Cognitive Impairment
(Amnestic–High Frontotemporal
Method Conversion Risk) Alzheimer Disease Degeneration
Standard Atrophy of parietal lobes
structural CT and hippocampus
Standard More overall atrophy and Atrophy of parietal lobes Behavioral variant FTD; focal
structural MRI focal atrophy involving and hippocampus and pathology in frontal (dorsolateral,
hippocampus, inferior and entorhinal cortex +/- orbital, and medial frontal cortices)
middle temporal gyrus, thinning of posterior and anterior temporal regions;
posterior cingulate, and body of corpus callosum; anterior temporal lobe greater
precuneus compared to widespread atrophy on the left than on the right
nonconverters side in semantic variant;
left-sided inferior frontal and
insular atrophy in PNFA
Diffusion-weighted
imaging
Diffusion-tensor Reduced FA in portion Alteration in temporal Decreased FA in superior
imaging of cingulum connecting white matter, posterior longitudinal fasciculus
hippocampus to posterior cerebral white matter, and connecting frontal and parietal
cingulate corpus callosum; reduced regions in behavioral variant FTD;
FA in portion of cingulum decreased FA in inferior
connecting hippocampus longitudinal fasciculus in
to posterior cingulate semantic variant
Perfusion MRI Reduced cerebral Arterial spin labeling
perfusion in medial and combination of decreased frontal
lateral parietal, superior perfusion + preserved parietal
temporal, and lateral perfusion in frontotemporal
frontal lobes lobar degeneration
Magnetic resonance Decreased NAA and Diffuse decreased NAA/Cr
spectroscopy increased myo-inositol ratio; focal decrease
NAA/Cr in parietal gray
matter and hippocampus;
high myo-inositol
168 Functional MRI Decreased hippocampal Increased activation in Decreased activation in
(active and activation during memory similar regions used by frontal and parietal
resting states) tasks; increased activation controls as well as activation regions; increased cerebellar
in similar regions used by of areas not used by activation
controls as well as activation controls; decreased activation
of areas not used by controls in medial temporal areas
during memory tasks
Resting state: decreased
activity in default mode
network of the posterior
cingulate cortex, inferior
parietal, inferolateral
temporal, ventral anterior
cingulate cortex and
hippocampus
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Vascular Lewy Body Corticobasal Creutzfeldt-Jakob Progressive
Dementia Dementia Syndrome Disease Supranuclear Palsy
Diffuse atrophy Asymmetric frontal Third ventricle
and/or parietal dilatation and
atrophy significant midbrain
atrophy, especially of
the anteroposterior
diameter
Hyperintensity of
cortical gyri (cortical
ribboning), the striatum
(caudate and putamen),
and/or thalamus in sCJD;
hyperintensity in pulvinar
(pulvinar sign) in vCJD
Decreased FA in
parietal lobes
Decreased NAA/Cr
ratio in frontal
and parietal cortex
but no significant
losses in medial
temporal lobes
Increased temporal
169
lobe activation on a
visual-processing
task
continued on next page
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
TABLE 8-1 Continued
Mild Cognitive Impairment
(Amnestic–High Frontotemporal
Method Conversion Risk) Alzheimer Disease Degeneration
[18F]Fluorodeoxyglucose Hypometabolism in the Reduced glucose metabolism Frontal hypometabolism
PET inferior parietal, posterior in parietal and superior/posterior in behavioral variant FTD,
cingulate, and medial temporal regions; early anterior temporal with
temporal region; changes in posterior cingulate semantic variant, and left
temporoparietal alterations cortex and precuneus; in perisylvian with PNFA
for distinguishing mild advanced stages of AD,
cognitive impairment frontal lobe hypoperfusion
with progressive course
Neurotransmitter Changes in neurotransmitter
systems imaging function
using PET ligands
Amyloid imaging Increased PiB signal Retention of 11C-PiB in Most do not show uptake
using PET the frontal, parietal,
temporal, and occipital
cortices and striatum
Perfusion with SPECT Hypoperfusion in inferior Temporoparietal Anterior temporal and
(eg, with HMPAO) parietal lobule, angular hypoperfusion frontal hypoperfusion
gyrus, and precuneus;
temporoparietal
hypoperfusion more
likely to progress to AD
T2-Weighted/proton Posterior portion of Increase of signal intensity
density/FLAIR corpus callosum may be seen in the
hyperintense subcortical white matter
of atrophied gyri,
extending into deep white
matter; corpus callosum
can appear atrophic either
anteriorly or diffusely
170
CT = computed tomography; MRI = magnetic resonance imaging; FTD = frontotemporal degeneration; PNFA = progressive
nonfluent aphasia; sCJD = sporadic Creutzfeldt-Jakob disease; vCJD = variant Creutzfeldt-Jakob disease; FA = fractional
anisotropy; NAA = N-acetylaspartate; Cr = creatine; AD = Alzheimer disease; PET = positron emission tomography;
PiB = Pittsburgh compound B; SPECT = single-photon emission computed tomography; HMPAO = hexamethylpropyleneamine
oxime; FLAIR = fluid-attenuated inversion recovery; CSF = cerebrospinal fluid.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Vascular Lewy Body Corticobasal Creutzfeldt-Jakob Progressive
Dementia Dementia Syndrome Disease Supranuclear Palsy
Decreased
occipitotemporal
metabolism
Hypoperfusion: left SPECT with presynaptic
anterior thalamic dopamine transporter
lesions; patchy (123I-FP-CIT): reduced
regions of striatal uptake of
hypometabolism dopamine or its
presymptomatic
transporters
FLAIR: hyperintensities Pulvinar sign (greater
(if incomplete) and hyperintensity of
hypointense to the posterior thalamus
brain and isointense relative to anterior
to the CSF if lacunes; putamen); CJD
small vessel disease
in white matter is
called leukoaraiosis
(multiple punctuate or
confluent lesions);
CADASIL: confluent
lesions in periventricular
white matter, characteristic
white matter lesions in 171
temporal poles and in the
external capsule and
striatocapsular lacunae and
microhemorrhages
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
REFERENCES
1. Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of
dementia (an evidence-based review). Report of the Quality Standards Subcommittee
of the American Academy of Neurology. Neurology 2001;56(9):1143–1153.
2. Braak H, Braak E. Neuropathological staging of Alzheimer-related changes. Acta
Neuropathol 1991;82(4):239–259.
3. Appel J, Potter E, Shen Q, et al. A comparative analysis of structural brain MRI in the
diagnosis of Alzheimer’s disease. Behav Neurol 2009;21(1):13–19.
4. Rusinek H, de Leon MJ, George AE, et al. Alzheimer disease: measuring loss of cerebral
gray matter with MR imaging. Radiology 1991;178(1):109–114.
5. Jones BF, Barnes J, Uylings HB, et al. Differential regional atrophy of the cingulate
gyrus in Alzheimer disease: a volumetric MRI study. Cereb Cortex 2006;16(12):1701–1708.
6. Risacher SL, Saykin AJ, West JD, et al. Baseline MRI predictors of conversion from MCI
to probable AD in the ADNI cohort. Curr Alzheimer Res 2009;6(4):347–361.
7. Du AT, Schuff N, Zhu XP, et al. Atrophy rates of entorhinal cortex in AD and normal
aging. Neurology 2003;60(3):481–486.
8. Schott JM, Fox NC, Frost C, et al. Assessing the onset of structural change in familial
Alzheimer’s disease. Ann Neurol 2003;53(2):181–188.
9. Rosen HJ, Gorno-Tempini ML, Goldman WP, et al. Patterns of brain atrophy in
frontotemporal dementia and semantic dementia. Neurology 2002;58(2):198–208.
10. Fukui T, Kertesz A. Volumetric study of lobar atrophy in Pick complex and Alzheimer’s
disease. J Neurol Sci 2000;174(2):111–121.
11. Cahn DA, Sullivan EV, Shear PK, et al. Structural MRI correlates of recognition memory
in Alzheimer’s disease. J Int Neuropsychol Soc 1998;4(2):106–114.
12. Brambati SM, Myers D, Wilson A, et al. The anatomy of category-specific object
naming in neurodegenerative diseases. J Cogn Neurosci 2006;18(10):1644–1653.
172 13. Rosen HJ, Wilson MR, Schauer GF, et al. Neuroanatomical correlates of impaired
recognition of emotion in dementia. Neuropsychologia 2006;44(3):365–373.
14. Rankin KP, Gorno-Tempini ML, Allison SC, et al. Structural anatomy of empathy in
neurodegenerative disease. Brain 2006;129(pt 11):2945–2956.
15. Seppi K, Schocke MF. An update on conventional and advanced magnetic resonance
imaging techniques in the differential diagnosis of neurodegenerative parkinsonism.
Curr Opin Neurol 2005;18(4):370–375.
16. Roman GC, Erkinjuntti T, Wallin A, et al. Subcortical ischaemic vascular dementia.
Lancet Neurol 2002;1(7):426–436.
17. Mungas D, Reed BR, Jagust WJ, et al. Volumetric MRI predicts rate of cognitive decline
related to AD and cerebrovascular disease. Neurology 2002;59(6):867–873.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
18. Kuker W. Imaging of cerebral vasculitis. Int J Stroke 2007;2(3):184–190.
19. Herve D, Godin O, Dufouil C, et al. Three-dimensional MRI analysis of individual
volume of lacunes in CADASIL. Stroke 2009;40(1):124–128.
20. Josephson SA, Papanastassiou AM, Berger MS, et al. The diagnostic utility of brain
biopsy procedures in patients with rapidly deteriorating neurological conditions or
dementia. J Neurosurg 2007;106(1):72–75.
21. Cordonnier C, van der Flier WM, Sluimer JD, et al. Prevalence and severity of
microbleeds in a memory clinic setting. Neurology 2006;66(9):1356–1360.
22. Lee SH, Kim SM, Kim N, et al. Cortico-subcortical distribution of microbleeds is
different between hypertension and cerebral amyloid angiopathy. J Neurol Sci
2007;258(1–2):111–144.
23. Vernino S, Geschwind M, Boeve B. Autoimmune encephalopathies. Neurologist
2007;13(3):140–147.
24. Geschwind MD, Haman A, Miller BL. Rapidly progressive dementia. Neurol Clin
2007;25(3):783–807.
25. Young GS, Geschwind MD, Fischbein NJ, et al. Diffusion-weighted and
fluid-attenuated inversion recovery imaging in Creutzfeldt-Jakob disease:
high sensitivity and specificity for diagnosis. Am J Neuroradiol 2005;26(6):1551–1562.
26. Zeidler M, Sellar RJ, Collie DA, et al. The pulvinar sign on magnetic resonance imaging
in variant Creutzfeldt-Jakob disease. Lancet 2000;355(9213):1412–1418.
27. Singhal AB, Newstein MC, Budzik R, et al. Diffusion-weighted magnetic resonance
imaging abnormalities in Bartonella encephalopathy. J Neuroimaging 2003;13(1):79–82.
28. Doherty MJ, Watson NF, Uchino K, et al. Diffusion abnormalities in patients with
Wernicke encephalopathy. Neurology 2002;58(4):655–657.
29. Favrole P, Chabriat H, Guichard JP, Woimant F. Clinical correlates of cerebral water
diffusion in Wilson disease. Neurology 2006;66(3):384–389.
30. Josephs KA, Holton JL, Rossor MN, et al. Neurofilament inclusion body disease: a new
proteinopathy? Brain 2003;126(pt 10):2291–2303.
31. Hufnagel A, Weber J, Marks S, et al. Brain diffusion after single seizures. Epilepsia 173
2003;44(1):54–63.
32. Bozzao A, Floris R, Baviera ME, et al. Diffusion and perfusion MR imaging in cases of
Alzheimer’s disease: correlations with cortical atrophy and lesion load. Am J
Neuroradiol 2001;22(6):1030–1036.
33. Zhang Y, Schuff N, Jahng GH, et al. Diffusion tensor imaging of cingulum fibers in
mild cognitive impairment and Alzheimer disease. Neurology 2007;68(1):13–19.
34. Huang J, Auchus AP. Diffusion tensor imaging of normal appearing white matter and
its correlation with cognitive functioning in mild cognitive impairment and
Alzheimer’s disease. Ann N Y Acad Sci 2007;1097:259–264.
35. Firbank MJ, Blamire AM, Krishnan MS, et al. Diffusion tensor imaging in dementia
with Lewy bodies and Alzheimer’s disease. Psychiatry Res 2007;155(2):135–145.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
" NEUROIMAGING
36. Zhang Y, Schuff N, Du AT, et al. White matter damage in frontotemporal dementia
and Alzheimer’s disease measured by diffusion MRI. Brain 2009;132(9):2579–2592.
37. Schuff N, Capizzano AA, Du AT, et al. Selective reduction of N-acetylaspartate in
medial temporal and parietal lobes in AD. Neurology 2002;58(6):928–935.
38. Schuff N, Capizzano AA, Du AT, et al. Different patterns of N-acetylaspartate loss in
subcortical ischemic vascular dementia and AD. Neurology 2003;61(3):358–364.
39. Miller BL, Moats RA, Shonk T, et al. Alzheimer disease: depiction of increased cerebral
myo-inositol with proton MR spectroscopy. Radiology 1993;187(2):433–437.
40. Franczak M, Prost RW, Antuono PG, et al. Proton magnetic resonance spectroscopy of
the hippocampus in patients with mild cognitive impairment: a pilot study. J Comput
Assist Tomogr 2007;31(5):666–670.
41. Mihara M, Hattori N, Abe K, et al. Magnetic resonance spectroscopic study of
Alzheimer’s disease and frontotemporal dementia/Pick complex. Neuroreport
2006;17(4):413–416.
42. Macfarlane RG, Wroe SJ, Collinge J, et al. Neuroimaging findings in human prion
disease. J Neurol Neurosurg Psychiatry 2007;78(7):664–670.
43. Gomez-Anson B, Alegret M, Munoz E, et al. Decreased frontal choline and
neuropsychological performance in preclinical Huntington disease. Neurology
2007;68(12):906–910.
44. Schifitto G, Navia BA, Yiannoutsos CT, et al. Memantine and HIV-associated cognitive
impairment: a neuropsychological and proton magnetic resonance spectroscopy
study. Aids 2007;21(14):1877–1886.
45. Schenck JF, Zimmerman EA, Li Z, et al. High-field magnetic resonance imaging of brain
iron in Alzheimer disease. Top Magn Reson Imaging 2006;17(1):41–50.
46. Logothetis NK. MR imaging in the non-human primate: studies of function and of
dynamic connectivity. Curr Opin Neurobiol 2003;13(5):630–642.
47. Pihlajamaki M, Jauhiainen AM, Soininen H. Structural and functional MRI in mild
cognitive impairment. Curr Alzheimer Res 2009;6(2):179–185.
48. Rombouts SA, van Swieten JC, Pijnenburg YA, et al. Loss of frontal fMRI activation in early
174 frontotemporal dementia compared to early AD. Neurology 2003;60(12):1904–1908.
49. Sauer J, ffytche DH, Ballard C, et al. Differences between Alzheimer’s disease and
dementia with Lewy bodies: an fMRI study of task-related brain activity. Brain
2006;129(pt 7):1780–1788.
50. Beckmann CF, DeLuca M, Devlin JT, Smith SM. Investigations into resting-state
connectivity using independent component analysis. Philos Trans R Soc Lond B Biol Sci
2005;360(1457):1001–1013.
51. Seeley WW, Menon V, Schatzberg AF, et al. Dissociable intrinsic connectivity networks
for salience processing and executive control. J Neurosci 2007;27(9):2349–2356.
52. Small GW, Bookheimer SY, Thompson PM, et al. Current and future uses of
neuroimaging for cognitively impaired patients. Lancet Neurol 2008;7(2):161–172.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
53. Gilman S, Koeppe RA, Little R, et al. Differentiation of Alzheimer’s disease
from dementia with Lewy bodies utilizing positron emission tomography with
[18F]fluorodeoxyglucose and neuropsychological testing. Exp Neurol 2005;
191(suppl 1):S95–S103.
54. Foster NL, Heidebrink JL, Clark CM, et al. FDG-PET improves accuracy in distinguishing
frontotemporal dementia and Alzheimer’s disease. Brain 2007;130(pt 10):2616–2635.
55. Chetelat G, Eustache F, Viader F, et al. FDG-PET measurement is more accurate than
neuropsychological assessments to predict global cognitive deterioration in patients
with mild cognitive impairment. Neurocase 2005;11(1):14–25.
56. Johnson KA, Moran EK, Becker JA, et al. Single photon emission computed
tomography perfusion differences in mild cognitive impairment. J Neurol Neurosurg
Psychiatry 2007;78(3):240–247.
57. Haxby JV, Duara R, Grady CL, et al. Relations between neuropsychological and
cerebral metabolic asymmetries in early Alzheimer’s disease. J Cereb Blood Flow
Metab 1985;5:193–200.
58. Mosconi L, De Santi S, Li J, et al. Hippocampal hypometabolism predicts cognitive
decline from normal aging. Neurobiol Aging 2007;29(5):676–692.
59. Benoit M, Koulibaly PM, Migneco O, et al. Brain perfusion in Alzheimer’s disease with
and without apathy: a SPECT study with statistical parametric mapping analysis.
Psychiatry Res 2002;114(2):103–111.
60. Kikuchi T, Okamura T, Fukushi K, et al. Cerebral acetylcholinesterase imaging:
development of the radioprobes. Curr Top Med Chem 2007;7(18):1790–1799.
61. Kadir A, Darreh-Shori T, Almkvist O, et al. Changes in brain 11C-nicotine binding sites
in patients with mild Alzheimer’s disease following rivastigmine treatment as assessed
by PET. Psychopharmacology (Berl) 2007;191(4):1005–1014.
62. Hilker R, Thomas AV, Klein JC, et al. Dementia in Parkinson disease: functional imaging
of cholinergic and dopaminergic pathways. Neurology 2005;65(11):1716–1722.
63. Kemppainen NM, Aalto S, Wilson IA, et al. PET amyloid ligand [11C]PIB uptake is
increased in mild cognitive impairment. Neurology 2007;68(19):1603–1606.
64. Rabinovici GD, Furst AJ, O’Neil JP, et al. 11C-PIB PET imaging in Alzheimer disease and
frontotemporal lobar degeneration. Neurology 2007;68(15):1205–1212. 175
65. Pike KE, Savage G, Villemagne VL, et al. Beta-amyloid imaging and memory
in non-demented individuals: evidence for preclinical Alzheimer’s disease. Brain
2007;130(pt 11):2837–2844.
66. Bennett DA, Schneider JA, Arvanitakis Z, et al. Neuropathology of older persons
without cognitive impairment from two community-based studies. Neurology
2006;66(12):1837–1844.
67. Rossini PM, Rossi S, Babiloni C, Polich J. Clinical neurophysiology of aging brain: from
normal aging to neurodegeneration. Prog Neurobiol 2007;83(6):375–400.
Continuum Lifelong Learning Neurol 2010;16(2)
Copyright @ American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Ospdrm 6Document10 pagesOspdrm 6mohamed ghazyNo ratings yet
- Budson - Memory Loss, Alzheimer's Disease, and Dementia - 2 Ed - 2015Document283 pagesBudson - Memory Loss, Alzheimer's Disease, and Dementia - 2 Ed - 2015Nathaly Cantor100% (3)
- Van Campen - The Proust Effect - 2014Document196 pagesVan Campen - The Proust Effect - 2014Nathaly CantorNo ratings yet
- Neuroimaging in DementiaDocument11 pagesNeuroimaging in DementiaAndika ResaNo ratings yet
- Imaging Alzheimer PDFDocument22 pagesImaging Alzheimer PDFSuman SharmaNo ratings yet
- MusicoterapiaDocument6 pagesMusicoterapiaCamila PinedaNo ratings yet
- Clinical Applications of Neuroimaging in PsychiatryDocument10 pagesClinical Applications of Neuroimaging in PsychiatryJujuNo ratings yet
- Classification of Alzheimers Disease Subjects From Mri Using Fuzzy Neural Network With Feature Extraction Using Discrete Wavelet TDocument8 pagesClassification of Alzheimers Disease Subjects From Mri Using Fuzzy Neural Network With Feature Extraction Using Discrete Wavelet TElenaNo ratings yet
- Neuroimaging in Investigation of Patients With.11Document20 pagesNeuroimaging in Investigation of Patients With.11mhd.mamdohNo ratings yet
- Uso de Neuroimagen en Diagnostico de DemenciaDocument14 pagesUso de Neuroimagen en Diagnostico de Demenciafrancisco NENTENo ratings yet
- MRI and CT Appearances in Metabolic Encephalopathies Due To Systemic Diseases in AdultsDocument10 pagesMRI and CT Appearances in Metabolic Encephalopathies Due To Systemic Diseases in Adultscatoelrey343No ratings yet
- Neuroimaging in DementiaDocument13 pagesNeuroimaging in DementiaLuciano AlvesNo ratings yet
- Spect PDFDocument14 pagesSpect PDFhalamadrid77No ratings yet
- Contents NCLDocument3 pagesContents NCLdewi najiraNo ratings yet
- Autoimmune Axonal Neuropathies. 2023Document15 pagesAutoimmune Axonal Neuropathies. 2023Arbey Aponte PuertoNo ratings yet
- Optical Coherence Tomography A Window Into The Mechanisms of Multiple SclerosisDocument12 pagesOptical Coherence Tomography A Window Into The Mechanisms of Multiple SclerosisSara BkrNo ratings yet
- Neurodegenerative Diseases in Geriatric Patients: Camilla Russo, Rossana Senese, and Mario MutoDocument25 pagesNeurodegenerative Diseases in Geriatric Patients: Camilla Russo, Rossana Senese, and Mario MutoolgaguerreroNo ratings yet
- Epi Zone Articles 1Document8 pagesEpi Zone Articles 1kai xinNo ratings yet
- El Valor Diagnostico de La Neuroimagen en DemenciaDocument22 pagesEl Valor Diagnostico de La Neuroimagen en Demenciajhoel cruzNo ratings yet
- Developmental Anomalies of The Brain in Mental RetardationDocument10 pagesDevelopmental Anomalies of The Brain in Mental RetardationKaterina ChatzNo ratings yet
- 05 Alzheimer'sDiseaseandFrontotemporalDementia SVM NaïveBayes, andkNN Algorithms GoodDocument12 pages05 Alzheimer'sDiseaseandFrontotemporalDementia SVM NaïveBayes, andkNN Algorithms Goodheineken2012No ratings yet
- Chapter 2Document11 pagesChapter 2fiskiyeyikimkirdi06No ratings yet
- Association Neurofilament and Alzheimer Progression Mattsson2019Document9 pagesAssociation Neurofilament and Alzheimer Progression Mattsson2019eastareaNo ratings yet
- Imagen Mas Epilepsia en NiñosDocument14 pagesImagen Mas Epilepsia en NiñosPosadasLoezaJosueKarlaNo ratings yet
- Imaging of Central Nervous System Demyelinating.14Document32 pagesImaging of Central Nervous System Demyelinating.14Adis GudukasaNo ratings yet
- Imaging in EncephalitisDocument10 pagesImaging in Encephalitisrafael rocha novaesNo ratings yet
- Antoine 2017Document8 pagesAntoine 2017Eliana NataliaNo ratings yet
- Magnetic Resonance Imaging in Alzheimers Disease and Mild Cognitive ImpairmentJournal of NeurologyDocument10 pagesMagnetic Resonance Imaging in Alzheimers Disease and Mild Cognitive ImpairmentJournal of NeurologyLOIDA CAMARGO CAMARGONo ratings yet
- Epileptic Seizures in Neurodegenerative Dementia SyndromesDocument6 pagesEpileptic Seizures in Neurodegenerative Dementia SyndromesInternational Medical PublisherNo ratings yet
- Neuroimagen en La Esclerosis Lateral Amiotrófica Usos Actuales y EmergentesDocument34 pagesNeuroimagen en La Esclerosis Lateral Amiotrófica Usos Actuales y EmergentesNatalia VelezNo ratings yet
- Epilepsy and Brain LesionDocument9 pagesEpilepsy and Brain LesionPosadasLoezaJosueKarlaNo ratings yet
- Brain Structure Alterations in Depression Psychoradiological EvidenceDocument10 pagesBrain Structure Alterations in Depression Psychoradiological EvidenceMoo GeeNo ratings yet
- Demented by AgeingDocument6 pagesDemented by AgeingSujoy DuttaNo ratings yet
- Art. Demencia EegDocument15 pagesArt. Demencia EegMaría BarrettNo ratings yet
- Marino S Et Al, Longitudinal Analysis of Brain Atrophy in Alzheimer's Disease and Frontotemporal Dementia, 2019Document9 pagesMarino S Et Al, Longitudinal Analysis of Brain Atrophy in Alzheimer's Disease and Frontotemporal Dementia, 2019henryfv2010No ratings yet
- Masdeu 2011Document10 pagesMasdeu 2011JujuNo ratings yet
- Mcfaline Figueroa2018Document9 pagesMcfaline Figueroa2018Kang LimbaNo ratings yet
- 7b9e60 Analysis of Meg Background Activity in AlzheimersDocument9 pages7b9e60 Analysis of Meg Background Activity in AlzheimerstourfrikiNo ratings yet
- Chronic Immune-Mediated Demyelinating NeuropathiesDocument21 pagesChronic Immune-Mediated Demyelinating NeuropathiesArbey Aponte PuertoNo ratings yet
- Brain SPECT Imaging in Complex Psychiatric Cases: An Evidence-Based, Underutilized ToolDocument9 pagesBrain SPECT Imaging in Complex Psychiatric Cases: An Evidence-Based, Underutilized ToolMariaNo ratings yet
- Introduction To NeuroimagingDocument11 pagesIntroduction To NeuroimagingJojo LastNo ratings yet
- Basal Ganglia Circuits As Targets For Neuromodulation in Parkinson DiseaseDocument7 pagesBasal Ganglia Circuits As Targets For Neuromodulation in Parkinson DiseaseSebastián GallegosNo ratings yet
- Chronic Traumatic Encephalopathy The Cellular Sequ - 2017 - Journal of ClinicalDocument6 pagesChronic Traumatic Encephalopathy The Cellular Sequ - 2017 - Journal of ClinicalBruno MañonNo ratings yet
- 4a007e Spectral and Non-Linear Analyses of Meg BackgrounDocument8 pages4a007e Spectral and Non-Linear Analyses of Meg BackgrountourfrikiNo ratings yet
- Jinyoung Park2021Document8 pagesJinyoung Park2021PPDS Rehab Medik UnhasNo ratings yet
- Past, Present and Future Alzheimer and OCTDocument38 pagesPast, Present and Future Alzheimer and OCTFernando lazzarettiNo ratings yet
- Mcanism B NeurodegenerativeDocument13 pagesMcanism B NeurodegenerativeAlin CiubotaruNo ratings yet
- Admin,+11 JT+13+-+HashimahDocument13 pagesAdmin,+11 JT+13+-+HashimahMomna AslamNo ratings yet
- 1891 FullDocument5 pages1891 FullArgtim RexhepiNo ratings yet
- Memory Loss in Alzheimer's DiseaseDocument10 pagesMemory Loss in Alzheimer's DiseaseDimitris VaziourakisNo ratings yet
- Park Inso N'S Dise ASEDocument132 pagesPark Inso N'S Dise ASEGrace Dela Rosa MelecioNo ratings yet
- Paraneoplastic SyndromesDocument8 pagesParaneoplastic SyndromesAndres F AristizabalNo ratings yet
- Meg Connectivity Analysis in Patients With AlzheiDocument13 pagesMeg Connectivity Analysis in Patients With AlzheitourfrikiNo ratings yet
- Neuro-Regeneration Therapeutic For Alzheimer's Dementia: Perspectives On Neurotrophic ActivityDocument14 pagesNeuro-Regeneration Therapeutic For Alzheimer's Dementia: Perspectives On Neurotrophic ActivityAnonymous kF9DLk3No ratings yet
- Neuroimaging and Psychiatric Disorders: A Literature ReviewDocument6 pagesNeuroimaging and Psychiatric Disorders: A Literature ReviewJAVED ATHER SIDDIQUINo ratings yet
- 06 - A Dataset of Scalp EEG Recordings of Alzheimer's Disease - GoodDocument10 pages06 - A Dataset of Scalp EEG Recordings of Alzheimer's Disease - Goodheineken2012No ratings yet
- Multimodal Neuroimaging BasicDocument14 pagesMultimodal Neuroimaging BasicJujuNo ratings yet
- Neuromodulation PDFDocument18 pagesNeuromodulation PDFSureshNo ratings yet
- Brain and Spinal MR Imaging FindingsDocument9 pagesBrain and Spinal MR Imaging FindingsAlaNo ratings yet
- A Clinician's Approach To Peripheral NeuropathyDocument12 pagesA Clinician's Approach To Peripheral Neuropathytsyrahmani100% (1)
- Echography and Doppler of the BrainFrom EverandEchography and Doppler of the BrainChiara RobbaNo ratings yet
- Scanned With CamscannerDocument2 pagesScanned With CamscannerNathaly CantorNo ratings yet
- I9 PDFDocument7 pagesI9 PDFNathaly CantorNo ratings yet
- What Should You Know About Limbic Encephalitis?: O Que Deve Saber Sobre Encefalites Auto-Imunes?Document6 pagesWhat Should You Know About Limbic Encephalitis?: O Que Deve Saber Sobre Encefalites Auto-Imunes?Nathaly CantorNo ratings yet
- Normal Brain Anatomy On Magnetic Resonance ImagingDocument9 pagesNormal Brain Anatomy On Magnetic Resonance ImagingNathaly CantorNo ratings yet
- Pituitaria SEMINARSDocument12 pagesPituitaria SEMINARSNathaly CantorNo ratings yet
- Estado Epiléptico Parcial No Convulsivo Como Síntoma de Presentación de Encefalitis LímbicaDocument4 pagesEstado Epiléptico Parcial No Convulsivo Como Síntoma de Presentación de Encefalitis LímbicaNathaly CantorNo ratings yet
- Use of Remote Sensing Data in A GIS Environment For Water Resources ManagementDocument13 pagesUse of Remote Sensing Data in A GIS Environment For Water Resources ManagementchuniNo ratings yet
- Changing An Occupied Bed Procedure ChecklistDocument4 pagesChanging An Occupied Bed Procedure ChecklistMarku LeeNo ratings yet
- FS5005 DSDocument2 pagesFS5005 DSMc CarmoNo ratings yet
- Road SafetyDocument48 pagesRoad SafetyAlie Bhin Abhu DhabiNo ratings yet
- E14F05P09Document6 pagesE14F05P09Víctor RomeuNo ratings yet
- Scam0114 PDFDocument76 pagesScam0114 PDFManuel Guardia AraujoNo ratings yet
- Efikasi Insektisida Gokilath-S50EC (D, D-Trans-Dengan Metode Pengabutan (Thermal Fogging)Document10 pagesEfikasi Insektisida Gokilath-S50EC (D, D-Trans-Dengan Metode Pengabutan (Thermal Fogging)rismaNo ratings yet
- Traffic Engineering MicroprojectDocument13 pagesTraffic Engineering MicroprojectSohel Torane100% (1)
- Effects of Soil Pollution On Geotechnical Behaviour of SoilsDocument8 pagesEffects of Soil Pollution On Geotechnical Behaviour of SoilsSupritha K100% (1)
- Ong Tze Ning Y2T3 Collection WorkDocument28 pagesOng Tze Ning Y2T3 Collection WorkTZE NING ONGNo ratings yet
- Trelleborg - Foam Testing ProtocolDocument2 pagesTrelleborg - Foam Testing ProtocolAhmad BalahNo ratings yet
- Glaucoma NCPDocument4 pagesGlaucoma NCPChantal CaraganNo ratings yet
- Giving Advice Tests Warmers Coolers - 17176Document1 pageGiving Advice Tests Warmers Coolers - 17176Angelia Vika SeptianaNo ratings yet
- The Evolving Story of Rice Evolution: Duncan A. Vaughan, Bao-Rong Lu, Norihiko TomookaDocument15 pagesThe Evolving Story of Rice Evolution: Duncan A. Vaughan, Bao-Rong Lu, Norihiko TomookaChetanNo ratings yet
- Chapter 3 - Understanding Research EthicsDocument16 pagesChapter 3 - Understanding Research EthicsArly TolentinoNo ratings yet
- Catalyst Deactivation1Document8 pagesCatalyst Deactivation1Hussain AliNo ratings yet
- Web. DistilationDocument277 pagesWeb. DistilationchetanjhaNo ratings yet
- PDS Benefit Overview - Dentist 2019Document4 pagesPDS Benefit Overview - Dentist 2019jentotheskyNo ratings yet
- Concept of Prana Vayu & Shat Chakras in Marma Chikitsa (मममम मममममममम)Document4 pagesConcept of Prana Vayu & Shat Chakras in Marma Chikitsa (मममम मममममममम)VestigeKamleshNo ratings yet
- Dr. Uttam Kumar Kanp Dr. Uttam Kumar Kanp: AuxinDocument24 pagesDr. Uttam Kumar Kanp Dr. Uttam Kumar Kanp: AuxinSasmitaNo ratings yet
- Fire Safety Signs Notices and Graphic SymbolsDocument28 pagesFire Safety Signs Notices and Graphic SymbolsEbenezer Blay100% (1)
- Nanoshi Samajik SabhagrahDocument4 pagesNanoshi Samajik SabhagrahAkshay NaikNo ratings yet
- Contoh Soal Bahasa InggrisDocument7 pagesContoh Soal Bahasa InggrisMaria Vinsensia AnuNo ratings yet
- Freight Transport Management Article 6 - Networked Rfid For Use in The Food ChainDocument6 pagesFreight Transport Management Article 6 - Networked Rfid For Use in The Food ChainfahmiamroziNo ratings yet
- Terrain Below Ground Drainage Dimensional DataDocument16 pagesTerrain Below Ground Drainage Dimensional DatamealysrNo ratings yet
- Unit 2Document74 pagesUnit 2Ahamed RaseethNo ratings yet
- Effect of Organic Manure On Degradation Assessment in Minna NJTA2021Document14 pagesEffect of Organic Manure On Degradation Assessment in Minna NJTA2021Awwal YasinNo ratings yet
- Detector arc-LAD - HS 2019Document11 pagesDetector arc-LAD - HS 2019kryo195No ratings yet
- BBCCT-101 - English July2021-Dec2022Document3 pagesBBCCT-101 - English July2021-Dec2022Cricket ClutchNo ratings yet