Professional Documents
Culture Documents
Jco 2007 14 5029
Uploaded by
Agung Budi PamungkasOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jco 2007 14 5029
Uploaded by
Agung Budi PamungkasCopyright:
Available Formats
VOLUME 26 䡠 NUMBER 14 䡠 MAY 10 2008
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Lapatinib Versus Hormone Therapy in Patients With
Advanced Renal Cell Carcinoma: A Randomized Phase III
Clinical Trial
Alain Ravaud, Robert Hawkins, Jason P. Gardner, Hans von der Maase, Niko Zantl, Peter Harper,
Frédéric Rolland, Bruno Audhuy, Jean-Pascal Machiels, Frank Pétavy, Martin Gore, Patrick Schöffski, and
Iman El-Hariry
From the Department of Medical
Oncology, Hôpital Saint André, A B S T R A C T
Bordeaux; Department of Medical
Oncology, Centre René Gauducheau, St Purpose
Herblain; Department of Medical Oncol- Lapatinib is an orally reversible inhibitor of epidermal growth factor receptor (EGFR)/human
ogy, Hôpital Pasteur, Colmar, France; epidermal growth factor receptor 2 (HER-2) tyrosine kinases with demonstrated activity in patients
Department of Medical Oncology, with HER-2–positive breast cancer. In the current phase III open-label trial, lapatinib was compared
Christie Hospital, Manchester; with hormone therapy (HT) in patients with advanced renal cell carcinoma (RCC) that express
GlaxoSmithKline, Greenford; Depart-
EGFR and/or HER-2.
ment of Medical Oncology, Guys and
St Thomas’s Hospitals; Department of Patients and Methods
Medical Oncology, Royal Marsden Patients with advanced RCC who had experienced disease progression through first-line cytokine
Hospital, London, United Kingdom; therapy—stratified by Karnofsky performance status and number of metastatic sites—were randomly
Department of Medical Oncology,
assigned to lapatinib 1,250 mg daily or HT. The primary end point was time to progression (TTP);
Rigshospital, Copenhagen, Denmark;
Department of Medical Oncology, Tech-
secondary end points included overall survival (OS), safety, and biomarker analyses.
nische Universität München, München, Results
Germany; Department of Medical Four hundred sixteen patients were enrolled onto the study. Median TTP was 15.3 weeks for lapatinib
Oncology, Université Catholique de
versus 15.4 weeks for HT (hazard ratio [HR] ⫽ 0.94; P ⫽ .60), and median OS was 46.9 weeks for
Louvain, Brussels; and Department of
Medical Oncology, Universitair Zeiken-
lapatinib versus 43.1 weeks for HT (HR ⫽ 0.88; P ⫽ .29). In a biomarker analysis of patients with
huis Gasthuisberg, Leuven, Belgium. EGFR-overexpressed tumors (3⫹ by immunohistochemistry [IHC]; n ⫽ 241) median TTP was 15.1
Submitted September 18, 2007;
weeks for lapatinib versus 10.9 weeks for HT (HR ⫽ 0.76; P ⫽ .06), and median OS was 46.0 weeks
accepted January 25, 2008. for lapatinib versus 37.9 weeks for HT (HR ⫽ 0.69; P ⫽ .02). These results were confirmed by Cox
regression analysis. No unexpected toxicities were observed; the most commonly reported drug-
Both A.R. and R.H. contributed equally
to this work.
related adverse events (all grades) for lapatinib were rash (44%) and diarrhea (40%).
Presented at the 42nd Annual Meeting Conclusion
of the American Society of Clinical Lapatinib was well tolerated with equivalent overall efficacy to HT in advanced RCC patients who
Oncology, June 2-6, 2006, Atlanta, GA. had experienced disease progression while receiving cytokines, and the study supports that
Authors’ disclosures of potential con- lapatinib prolonged OS relative to HT in patients with 3⫹ EGFR status determined by IHC.
flicts of interest and author contribu-
tions are found at the end of this J Clin Oncol 26:2285-2291. © 2008 by American Society of Clinical Oncology
article.
Corresponding author: Alain Ravaud,
tumor growth in vitro and in vivo.5,6 In addition,
MD, PhD, Department of Medical INTRODUCTION
Oncology, Hôpital Saint André, CHU EGFR signaling is involved in the tumorigenesis as-
Bordeaux, 1 rue Jean Burguet, 33075 The incidence of renal cell carcinoma (RCC) is in- sociated with mutations of the von Hippel-Lindau
Bordeaux cedex, France; e-mail:
alain.ravaud@chu-bordeaux.fr.
creasing in Europe and the United States.1 Meta- (VHL) tumor suppressor gene, which are found in
static RCC is insensitive to chemotherapy and shows the majority of cases of clear cell RCC.7,8 The role of
© 2008 by American Society of Clinical
Oncology low rates of response to immunotherapy.2 However, the related receptor, human epidermal growth fac-
0732-183X/08/2614-2285/$20.00 antiangiogenic-targeted therapies such as sunitinib tor receptor 2 (HER-2, or ErbB2), in RCC pathogen-
DOI: 10.1200/JCO.2007.14.5029
and sorafenib have emerged as important new stan- esis is less clear; however, co-overexpression of
dard treatments in first-line treatment or after fail- EGFR and HER-2 is associated with metastatic dis-
ure of immunotherapy.3,4 ease.9 Lapatinib (Tykerb/Tyverb; GlaxoSmithKline,
Epidermal growth factor receptor (EGFR) and Research Triangle Park, NC) is a dual inhibitor of the
its ligands, EGF and transforming growth factor ␣ intracellular tyrosine kinase domains of EGFR and
(TGF-␣), are overexpressed in RCC.5,6 Both ligands HER-2, and has recently demonstrated efficacy in a
stimulate the proliferation of human RCC cell lines, randomized phase III study in combination with
while inhibitors of EGFR inhibit proliferation and chemotherapy in HER-2– overexpressing breast
© 2008 by American Society of Clinical Oncology 2285
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Ravaud et al
cancer patients.10 Lapatinib is a particularly attractive agent to study in The primary end point was TTP, defined as the interval between date of
advanced RCC. randomization and the earliest date of radiologically confirmed progression by
independent review or death due to RCC, in the intent-to-treat population.
Therefore, we conducted a prospective, open-label, randomized
Secondary end points included tumor response rate; time to response; clinical
phase III trial of lapatinib in patients with advanced RCC that ex- benefit; overall survival (OS); and correlative analysis of tumor biomarkers,
pressed EGFR or HER-2, and had experienced disease progression including analysis of TTP and OS, depending on level of expression of EGFR
while receiving first-line cytokine therapy. At the time this trial was and/or HER-2.
designed, there were limited treatment options for RCC patients who Further determination of efficacy was based on objective measurements
of disease using Response Evaluation Criteria in Solid Tumors.14 Disease
had experienced disease progression while receiving cytokine therapy.
assessment was done at baseline, then every 8 weeks after initiating treatment.
Hormone therapy (HT) was selected for the control arm in the trial Patients experiencing a partial response (PR) or complete response had to have
because it is well tolerated and was used as a standard comparison a confirmatory assessment at least 4 weeks later. Disease assessments were
treatment in a seminal randomized trial.11 continued until progressive disease was documented, even if treatment was
discontinued. All scans were reviewed by a blinded, independent radiologic
review board (Synarc, San Francisco, CA).
Safety was assessed by analyzing the physical examination findings,
PATIENTS AND METHODS CBCs, coagulation parameters, clinical chemistry, urinalysis, and KPS (as-
sessed every 4 weeks); 12-lead ECG, conducted at baseline and follow-up;
multigated acquisition scan or echocardiography (conducted every 8 weeks);
Patients
and adverse events. All randomly assigned patients who received at least one
Eligible patients had histologically or cytologically confirmed, locally
dose of the study drug were included in the safety population. Adverse events
advanced or metastatic RCC of any histologic subtype that was not amenable
were rated by the investigators using the National Cancer Institute Common
to curative surgery or radiotherapy. Other inclusion criteria included disease
Toxicity Criteria v2.0.15
progression after or intolerance to first-line cytokine-based therapy; expres-
IHC for EGFR (PharmDx; Dako, Glostrup, Denmark) and HER-2 (Her-
sion of EGFR and/or HER-2 in tumor tissue with immunohistochemistry
cepTest, Dako) expression was performed centrally in a blinded, independent
(IHC) 1⫹, 2⫹, or 3⫹; measurable disease according to the Response Evalua-
manner by Quest Diagnostics (Madison, NJ) using fresh or paraffin-
tion Criteria in Solid Tumors; cardiac ejection fraction within institutional
embedded biopsy tissue taken from primary and/or metastatic tumor sites
normal limits as measured by multigated acquisition scan or echocardiogra-
before the patient was enrolled onto the study. Moderate to strong complete
phy; age ⱖ 18 years; Karnofsky performance status (KPS) ⱖ 70%; and life
membrane staining in more than 10% of the tumor cells was classified as 3⫹
expectancy ⱖ 12 weeks. Prior systemic neoadjuvant or adjuvant therapy was
strongly positive.
allowed. Patients had to have adequate hematologic, renal, and hepatic func-
tion, defined as granulocyte count ⱖ 1,500/L; platelet count ⱖ75,000/L; Statistical Analysis
hemoglobin ⱖ 9 g/dL; serum creatinine ⱕ 180 mol/L and estimated creati- It was determined that a total of 257 TTP events would be required to
nine clearance ⱖ 30 mL/min; total bilirubin less than 1.5⫻ the upper limit of detect a 50% increase in the median TTP (from 4 to 6 months) between groups
normal (ULN); ALT less than 3⫻ ULN unless due to disease, in which case up using a log-rank test at the two-sided 5% significance level with 90% power. To
to 5⫻ ULN was allowed. Exclusion criteria included prior or concurrent allow for losses to follow-up of up to 10% of patients, it was determined that
treatment with an EGFR or HER-2 inhibitor; concurrent systemic corticoste- 400 patients would need to be enrolled. Interim analyses for safety and futility
roid therapy; recently completed or concurrent treatment with another inves- were dictated by the protocol after 100 and an additional 100 patients (total of
tigational therapy; active CNS metastases; malabsorption syndrome or other 200 patients) were enrolled and observed for at least 16 weeks. An independent
GI disease or resection that could affect absorption; and severe cardiovascular data-monitoring committee evaluated the interim data to provide an opportunity
disease or cardiac disease requiring a device. The study was approved by the to terminate the study if concerns about safety arose or if there was adequate
institutional review board or independent ethics committee at each clinical evidence to reject the alternative hypothesis that lapatinib improves TTP by 50%
site. All patients gave written informed consent before participating in the trial. compared with hormonal treatment in favor of the null hypothesis.
TTP was summarized using inverse cumulative incidence curves, from
Study Design which median TTP was calculated. Treatment arms were compared using the
Patients were randomly assigned to receive lapatinib 1,250 mg daily or stratified log-rank test, and an estimate of the hazard ratio (HR) and corre-
HT. Randomization was done centrally via an interactive voice response sys- sponding 95% CI were calculated. Tumor response rates and clinical benefit
tem, and stratified according to KPS (70% to 80%, or 90% to 100%) and the (overall response rate [complete response ⫹ PR] ⫹ stable disease at 6 months)
number of metastatic sites (ⱕ two or ⬎ two). rates in each group were compared using stratified Fisher’s exact tests, with
Lapatinib was administered the same time each day immediately after the 95% CI calculated for differences in rates between groups.
morning meal; HT was also administered daily, and consisted of megestrol A Cox regression analysis for OS was performed on the following sub-
acetate or tamoxifen selected and provided by the investigator. All patients groups: treatment with lapatinib versus HT and EGFR (0, 1⫹, or 2⫹ v 3⫹).
were treated until disease progression or withdrawal from the study, and were The regression model was adjusted for KPS and number of metastatic sites. A
evaluated for toxicity every 4 weeks. Those patients who had derived clinical risk factor analysis was also conducted according to key categoric variables
benefit as determined by the investigator were allowed to continue receiving relevant in this patient population: KPS (⬍ 80% or ⱖ 80%), hemoglobin (less
treatment even after evidence of radiologic disease progression. than normal or more than normal), corrected serum calcium (ⱕ 10 or ⬎ 10
The study was designed in 2001, initially as a phase II randomized trial mg/dL) to define risk groups.16
using objective response rate as the primary end point. In 2002, emerging
evidence demonstrated that time to disease progression was a more suitable
end point for targeted therapies than response rate, and the design was modi- RESULTS
fied to incorporate time to progression (TTP) as a new primary end point.12,13
A total of 110 patients were recruited after completing the phase II part of the Patients
study. The study accrual was stopped for 3 months in the interim until the
protocol was amended and local ethics committee approvals were obtained.
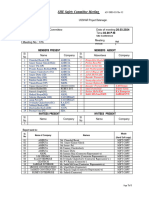
Between December 2002 and February 2005, a total of 416 pa-
The study was also expanded to a phase III design based on results from a tients from 116 centers in 11 countries were randomly assigned to
preplanned interim analysis of safety data alone. Throughout the amendment, receive lapatinib (n ⫽ 209) or HT (n ⫽ 207). Figure 1 shows the
the investigators and the sponsor were blinded to the results. patients’ progression through the trial, and Table 1 lists the baseline
2286 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Phase III Trial of Lapatinib Versus HT in RCC
416 Randomized
209 allocated to lapatinib 207 allocated to HT
205 received allocated intervention 199 received allocated intervention
4 did not receive allocated 8 did not receive allocated
intervention intervention
(1 died, 1 progressed, 1 withdrew (1 progressed, 2 withdrew
consent, 1 unspecified) consent, 1 protocol violation,
4 unspecified)
Fig 1. Trial profile. HT, hormone therapy;
ITT, intent to treat.
2 Lost to follow-up 3 Lost to follow-up
186 Discontinued intervention 187 Discontinued intervention
146 progressive disease 160 progressive disease
20 adverse event, 11 adverse events
8 died 7 died
5 withdrew consent 4 withdrew consent
1 protocol violation 1 protocol violation
6 not specified 3 not specified
209 included in efficacy analysis (ITT) 207 included in efficacy analysis (ITT)
205 included in safety analysis 199 included in safety analysis
characteristics of the enrolled patients. The two treatment arms were months) were similar between arms: 8.1% with lapatinib and 9.7%
well balanced for all baseline factors, including EGFR expression levels with HT.
and the relevant prognostic risk factors in this patient population.16 Exploratory analyses of TTP and OS were conducted based on
The majority of patients had clear cell histology (87%) and high (IHC EGFR tumor expression levels as part of the secondary biomarker end
3⫹) tumor expression of EGFR (58%). point. Significant differences were not observed between groups for
TTP or OS for patients with EGFR 0, 1⫹, or 2⫹ staining intensity (Figs
Efficacy 2C and 2D). In the group of patients with EGFR 3⫹ tumors, median
The planned analysis of efficacy end points, including EGFR TTP was prolonged over 4 weeks in the lapatinib arm (HR, 0.76; 95%
expression, was performed when 257 progression events by indepen- CI, 0.6 to 1.0; P ⫽ .06) from 10.9 to 15.1 weeks, and median OS was
dent assessment were achieved in September 2005, and the results are significantly increased by more than 8 weeks (HR, 0.69; 95% CI, 0.5 to
presented here. For time-to-event end points, the last date of known 1.0; P ⫽ .019) from 37.9 to 46.0 weeks (Figs 2E and 2F). These results
contact was used for those patients that had not reached the event at
were confirmed by multivariate Cox regression modeling, which
the time of analysis, and such patients were considered as censored in
demonstrated no treatment difference in the patients with low expres-
the analysis.
sion of EGFR (HR, 1.18; 95% CI, 0.80 to 1.73; P ⫽ .40), and a
Median TTP, the primary end point, was similar between treat-
significant effect on OS between the two treatment groups for patients
ment arms in the intent-to-treat analysis (Fig 2A). The median TTP
was 15.3 weeks in the lapatinib arm versus 15.4 weeks in the HT arm with EGFR 3⫹ expression (HR, 0.66; 95% CI, 0.48 to 0.91; P ⫽ .012).
(HR, 0.94; P ⫽ .595; 95% CI, 0.75 to 1.18). Median OS (Fig 2B), was After progression, approximately half of the patients in each arm
46.9 weeks in the lapatinib arm and 43.1 weeks in the HT arm (HR, (92 receiving lapatinib and 105 receiving HT) received subsequent
0.88; P ⫽ .290; 95% CI, 0.69 to 1.12). therapy. Those patients who had derived clinical benefit continued to
Tumor response rate (PR only) was 1.4% and 0.5% in the lapa- receive treatment as determined by the investigator after disease pro-
tinib and HT groups, respectively. Approximately one third of pa- gression. These included 49 patients in the lapatinib arm (average
tients in each arm experienced stable disease at 2 months as the best duration 25 days), and 45 patients in the HT arm (average duration 28
response to treatment (66 [32%] in the lapatinib arm, and 65 [31%] in days). Other therapies included antiangiogenesis agents, and were
the HT arm). Rates of clinical benefit (PR or stable disease ⱖ 6 evenly distributed between the arms (13 after lapatinib v 15 after HT).
www.jco.org © 2008 by American Society of Clinical Oncology 2287
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Ravaud et al
[n ⫽ 15] and 2.0% with HT [n ⫽ 3]). No grade 4 events were reported
Table 1. Baseline Patient Characteristics of the 416 Patients
Included in the Analysis
in the lapatinib arm. Adverse events led to treatment discontinuation
in 13% (n ⫽ 26) and 9% (n ⫽ 18) of patients in the lapatinib and HT
Lapatinib HT
(n ⫽ 209) (n ⫽ 207) arms, respectively. Two patients in the lapatinib group died as a result
No. of No. of
of a serious, drug-related adverse event. One of these patients devel-
Characteristic Patients % Patients % oped a fatal cerebral hemorrhage 265 days after starting lapatinib. The
Age, years other patient developed interstitial pulmonary fibrosis after complet-
Median 61 62 ing lapatinib treatment 201 days earlier, and this event was categorized
Range 31-83 19-81 by the investigator as drug related.
Sex
Male 149 71 156 75
Female 60 29 51 25 DISCUSSION
KPS
90%-100% 117 56 128 62
70%-80% 92 44 79 38 This large, phase III trial of lapatinib versus HT did not meet the
Stage primary end point in the overall population of advanced RCC patients
III 7 3 4 2 whose disease had previously progressed after cytokine-based therapy.
IV 201 96 202 98 However, based on an exploratory analysis of EGFR level expression in
Histology
tumors, treatment with lapatinib seemed to prolong survival relative
Clear cell 175 84 187 90
Papillary 16 8 8 4
to HT in patients with high levels of tumor EGFR.
Chromophobe 6 3 3 1 EGFR is a well-described potential therapeutic target in RCC.
Collecting duct 0 1 ⬍1 Both EGFR and its ligand TGF-␣ are overexpressed in RCC, and
Unclassified 12 6 8 4 TGF-␣ is a critical mitogen for the autonomous growth of VHL-
Prior nephrectomy 196 94 194 94 inactivated (VHL⫺/⫺) RCC cells.8 Indeed, the TGF-␣/EGFR path-
No. of metastatic sites way seems to be an important pathway for carcinogenesis in VHL⫺/⫺
ⱕ2 106 51 105 51
RCC. When EGFR is inhibited, the autonomous growth of VHL⫺/⫺
⬎2 103 49 102 49
Common sites of metastasis
RCC cells is abolished in vitro.8 As such, several EGFR inhibitors have
Lung 167 43 169 46 been evaluated in phase II trials in RCC. The anti-EGFR monoclonal
Bone 70 18 58 16 antibody (mAb), cetuximab, produced no responses among 55 pa-
Liver 44 11 52 14 tients with metastatic RCC treated in a single-arm phase II trial,17
Lymph node 109 28 90 24 whereas a similar anti-EGFR mAb, panitumumab, produced three
Risk factor levelⴱ major responses, two minor responses, and disease stabilization in 44
Favorable 86 41 77 37
patients with metastatic RCC treated in a dose-ranging trial (N ⫽
Intermediate 65 31 76 37
Poor 58 28 54 26
88).18 The small-molecule tyrosine kinase inhibitors, gefitinib and
EGFR expression IHC scoring erlotinib, have not demonstrated significant activity with respect to
0 3 1 1 ⬍1 response rates in phase II trials, although disease stabilization was
1⫹ 25 12 21 10 reported in approximately 25% to 50% of patients.19-22 Dual targeted
2⫹ 65 31 60 29 therapy with a combination of erlotinib and bevacizumab, a mAb
3⫹ 116 56 125 60
directed against vascular endothelial growth factor, seemed to have
HER-2 expression IHC scoring
0 196 94 193 93
promising activity in metastatic RCC in a single-arm, open-label tri-
1⫹ 10 5 8 4 al.23 However, the combination was not found to be superior to
2⫹ 2 ⬍1 1 ⬍1 bevacizumab alone in this setting.24 None of these studies with EGFR
3⫹ 0 0 inhibitors selected patients for target expression or analyzed the results
Abbreviations: HT, hormone therapy; KPS, Karnofsky performance status; based on EGFR levels.
HER-2, human epidermal growth factor receptor 2; EGFR, epidermal growth To our knowledge, this was the first randomized phase III trial of
factor receptor; IHC, immunohistochemistry.
ⴱ
The variables considered in the risk factor assessment included hemoglobin
an EGFR/HER-2 inhibitor in RCC patients who were selected for
(⬍ normal or ⬎ normal), corrected serum calcium (ⱕ 10 or ⬎ 10 mg/dL), and expression of either target receptor. EGFR was overexpressed (IHC
KPS (⬍ 80% or ⱖ 80%) The favorable category was defined by the presence 3⫹) by the majority (58%) of patients; conversely, HER-2 was de-
of 0 factors, intermediate by one factor and poor by two or three factors.16
Forty-one patients had missing values for one factor, and five patients had tected in only 5% of patients. The exploratory subset analysis in the
missing values for two factors. EGFR-overexpressing patients (n ⫽ 241) was conducted as part of the
biomarker secondary end point of this study to generate hypotheses
and showed that OS was more prolonged in the lapatinib arm than in
the HT arm (HR ⫽ 0.69). Two nonexclusive hypotheses could explain
Safety the results observed in the current study. First, EGFR is a poor prog-
Table 2 summarizes the most commonly reported drug-related nostic factor in several malignancies, and is associated with reduction
adverse events in the safety population. In the lapatinib arm, these in survival. Previous smaller studies in RCC have suggested that the
events were rash (44%), diarrhea (40%), and nausea (18%). The presence and/or expression level of EGFR could have a deleterious
majority of drug-related adverse events were grade 1 and 2, and the impact on survival.5,25 Therefore, patients in the control arm with high
overall incidence of grade 3 and 4 events was low (7.3% with lapatinib EGFR-expressing tumors may have significantly worse prognosis than
2288 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Phase III Trial of Lapatinib Versus HT in RCC
A B
100 100
No Disease Progression
Cumulative Survival (%)
90 90
P = 0.595 P = 0.29
80 HR = 0.94 80 HR = 0.88
70 70
60 60 Lapatinib 1250 mg (N = 209; median OS, 46.9 wks)
50 50
40 40
Lapatinib 1250 mg (N = 209; median TTP, 15.3 wks)
30 30
20 20 Hormonal Therapy
Hormonal Therapy
10 (N = 207; median TTP, 15.4 wks) 10 (N = 207; median OS, 43.1 wks)
0 6 16 24 32 40 48 56 64 72 0 8 16 24 32 40 48 56 64 72 80 88 96 104 112 120 128 136 144
No. at risk Time (weeks) No. at risk Time (weeks)
Lapatinib 209 141 79 46 29 17 10 3 1 1 Lapatinib 209 192 168 140 113 89 75 50 34 24 16 12 9 7 5 3 1 1
HT 207 137 71 40 22 12 6 3 2 1 HT 207 186 163 136 100 71 52 36 26 23 14 6 3 3 2 1
C D
100 100
No Disease Progression
Cumulative Survival (%)
90 90
P = 0.182 P = 0.56
80 HR = 1.25 80 HR = 1.11
70 70
60 60 Hormonal Therapy (N =82; median OS, 54.1 wks )
Hormonal Therapy (N = 82; median TTP, 19 wks)
50 50
40 40
Lapatinib 1250 mg
30 30 (N = 93; median OS, 46.9 wks)
20 Lapatinib 1250 mg 20
10 (N = 93; median TTP, 25.7 wks) 10
0 6 16 24 32 40 48 56 64 72 0 8 16 24 32 40 48 56 64 72 80 88 96 104 112 120 128 136 144
No. at risk Time (weeks) No. at risk Time (weeks)
Lapatinib 93 64 36 18 10 7 4 2 1 1 Lapatinib 93 85 74 62 52 42 32 25 17 14 9 7 4 3 2 2 1 1
HT 82 60 37 26 16 8 5 3 2 1 HT 82 74 66 58 46 35 28 23 22 19 13 5 2 2 1 1
E F
100 100
No Disease Progression
Cumulative Survival (%)
90 90
P = 0.063 P = 0.019
80 HR = 0.76 80 HR = 0.69
70 70
60 60 Lapatinib 1250 mg (N = 116; median OS, 46.0 wks)
50 50
40 Lapatinib 1250 mg (N = 116; median TTP, 15.1 wks) 40
30 30
20 20
Hormonal Therapy Hormonal Therapy
10 (N = 125; median TTP, 10.9 wks)
10 (N =125; median OS, 37.9 wks)
0 6 16 24 32 40 48 56 64 72 0 8 16 24 32 40 48 56 64 72 80 88 96 104 112 120 128 136 144
No. at risk Time (weeks) No. at risk Time (weeks)
Lapatinib 116 77 43 28 19 10 6 1 Lapatinib 116 107 94 78 61 47 43 25 17 10 7 5 5 4 3 1
HT 125 77 34 14 6 4 1 HT 125 112 97 78 54 36 24 13 4 4 1 1 1 1 1
Fig. 2. Kaplan-Meier estimates of cumulative incidence of time to progression (TTP) according to the assessment of the independent review committee (A, C, E) and
overall survival (OS; B, D, F). (A) TTP in the intent-to-treat (ITT) population for lapatinib versus hormone therapy (HT). (B) OS in the ITT population for lapatinib versus
HT. (C) TTP for lapatinib versus HT in patients with tumor epidermal growth factor receptor (EGFR) 0, 1, 2⫹ intensity staining. (D) OS for lapatinib versus HT in patients
with tumor EGFR 0, 1, 2⫹ intensity staining. (E) TTP for lapatinib versus HT in patients with tumor EGFR 3⫹ intensity staining. (F) OS for lapatinib versus HT in patients
with tumor EGFR 3⫹ intensity staining. HR, hazard ratio.
patients with tumors expressing reduced EGFR. These observations levels of tumor EGFR expression (37.9 v 54.1 weeks; P ⬍ .01). Second,
were confirmed in the current study, where patients overexpressing lapatinib is an active inhibitor of tumor EGFR in vivo and is most
EGFR in the control arm had a poorer outcome than those with low efficacious in patients who express higher levels of EGFR (IHC 3⫹)
www.jco.org © 2008 by American Society of Clinical Oncology 2289
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Ravaud et al
Table 2. Drug-Related Adverse Events in the Patients Included in the Safety Population
Lapatinib (n ⫽ 205) HT (n ⫽ 199)
Any Grade Grade 3 Grade 4 Any Grade Grade 3 Grade 4
No. of No. of No. of No. of No. of No. of
Adverse Event Patients % Patients % Patients % Patients % Patients % Patients %
Any drug-related event 161 79 58 29
Rash 90 44 4 2 0 6 3 0 0
Diarrhea 83 40 3 1 0 5 3 0 0
Nausea 36 18 2 ⬍1 0 7 4 0 0
Vomiting 15 7 2 ⬍1 0 4 2 0 0
Fatigue 13 6 1 ⬍1 0 1 ⬍1 0 0
Asthenia 9 4 1 ⬍1 0 1 ⬍1 0 0
LVEF decline 10 5 1 ⬍1 0 0 0 0
Vascular disorders 4 2 0 0 11 6 2 1 1 ⬍1
Stomatitis 4 2 1 ⬍1 0 0 0 0
Hand-foot skin reaction 1 ⬍1 0 0 0 0 0
Hands and feet skin erythrosis 1 ⬍1 0 0 0 0 0
Abbreviations: HT, hormone therapy; LVEF, left ventricular ejection fraction.
than lower levels (IHC 0, 1⫹, or 2⫹) when compared with the control In conclusion, although this large randomized trial was negative
arm. This rationale is consistent with previous studies of targeted for the primary end point in the overall patient population, explor-
agents, including lapatinib, which have demonstrated efficacy in pa- atory biomarker analysis has shown that second-line treatment with
tients who overexpressed HER-2.10 lapatinib seems to prolong overall survival relative to HT in patients
Lapatinib is a dual-targeted inhibitor of EGFR and HER-2, and with advanced RCC whose tumors overexpress EGFR.
potently blocks the intense signaling via the EGFR/HER-2 het-
erodimer pathway that has been shown to induce tumor cell prolifer-
ation. Therefore, a complementary hypothesis is that more complete AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS
OF INTEREST
inhibition that translates to clinical benefit may be possible in RCC
when EGFR expression is upregulated, even though HER-2 expres-
Although all authors completed the disclosure declaration, the following
sion is low. Additional biomarker studies are underway to investigate author(s) indicated a financial or other interest that is relevant to the subject
these hypotheses and other potential pathways. matter under consideration in this article. Certain relationships marked
HT offers only symptomatic benefit to RCC patients with a with a “U” are those for which no compensation was received; those
well-tolerated safety profile, and is widely administered to patients relationships marked with a “C” were compensated. For a detailed
who have experienced disease progression while receiving standard description of the disclosure categories, or for more information about
first-line therapy.11 Furthermore, expression of hormone receptors ASCO’s conflict of interest policy, please refer to the Author Disclosure
Declaration and the Disclosures of Potential Conflicts of Interest section in
was detected in only 1% of RCC patients26; therefore, the use of HT in
Information for Contributors.
the current trial would not be expected to influence the efficacy results Employment or Leadership Position: Jason P. Gardner,
in the EGFR subpopulations. GlaxoSmithKline (C); Frank Pétavy, GlaxoSmithKline (C); Iman
Although patients were not stratified for the established risk El-Hariry, GlaxoSmithKline (C) Consultant or Advisory Role: Alain
factors in the second-line RCC setting,16 a retrospective analysis dem- Ravaud, GlaxoSmithKline, Pfizer Inc, Bayer, Novartis, Wyeth (C);
onstrated that the distributions of KPS, corrected serum calcium, and Robert Hawkins, GlaxoSmithKline (C); Peter Harper, GlaxoSmithKline
hemoglobin were well balanced between the two treatment arms and (C); Martin Gore, GlaxoSmithKline (C) Stock Ownership: Jason P.
Gardner, GlaxoSmithKline; Frank Pétavy, GlaxoSmithKline; Iman
in each of the EGFR subgroups. Moreover, the use of subsequent
El-Hariry, GlaxoSmithKline Honoraria: Alain Ravaud, Pfizer Inc, Bayer;
therapies after progression, including antiangiogenesis agents and the Hans von der Maase, Novo Nordisk, Pierre Fabre, Eli Lilly & Co, Roche,
continuation of lapatinib or HT, was also equivalent and would not be Bayer, Pfizer Inc; Peter Harper, GlaxoSmithKline; Bruno Audhuy,
expected to bias the results. GlaxoSmithKline Research Funding: Alain Ravaud, GlaxoSmithKline,
Taken together, these results are consistent enough to hypothe- Roche; Martin Gore, GlaxoSmithKline Expert Testimony: None Other
size that an overall survival benefit could be obtained by targeting Remuneration: Alain Ravaud, Pfizer Inc, Bayer, Roche, Novartis; Hans
EGFR/HER-2 inhibition in RCC. However, the significant difference von der Maase, Novo Nordisk, Pierre Fabre, Eli Lilly & Co, Roche, Bayer,
Pfizer Inc
in the EGFR-overexpressing population was not observed with a sim-
ilar magnitude using the TTP end point. This may be due to the rapid
progression of approximately 50% of patients at the first disease as- AUTHOR CONTRIBUTIONS
sessment (8 weeks), which could have contributed to an underpow-
ered primary end point despite the divergence of the Kaplan and Meier Conception and design: Alain Ravaud, Robert Hawkins, Jason P.
curves at this time point. This may have masked the longer-term effect Gardner, Niko Zantl, Peter Harper, Frank Pétavy, Martin Gore, Patrick
of lapatinib on the EGFR pathway observed in the survival end point. Schöffski, Iman El-Hariry
2290 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
Phase III Trial of Lapatinib Versus HT in RCC
Administrative support: Jason P. Gardner, Iman El-Hariry Rolland, Bruno Audhuy, Jean-Pascal Machiels, Frank Pétavy, Martin
Provision of study materials or patients: Alain Ravaud, Robert Gore, Patrick Schöffski, Iman El-Hariry
Hawkins, Jason P. Gardner, Hans von der Maase, Niko Zantl, Peter Manuscript writing: Alain Ravaud, Robert Hawkins, Jason P. Gardner,
Harper, Frédéric Rolland, Bruno Audhuy, Jean-Pascal Machiels, Frank Iman El-Hariry
Pétavy, Martin Gore, Patrick Schöffski Final approval of manuscript: Alain Ravaud, Robert Hawkins,
Collection and assembly of data: Jason P. Gardner, Hans von der Maase, Jason P. Gardner, Hans von der Maase, Niko Zantl, Peter
Frank Pétavy, Iman El-Hariry Harper, Frédéric Rolland, Bruno Audhuy, Jean-Pascal
Data analysis and interpretation: Alain Ravaud, Robert Hawkins, Jason Machiels, Frank Pétavy, Martin Gore, Patrick Schöffski,
P. Gardner, Hans von der Maase, Niko Zantl, Peter Harper, Frédéric Iman El-Hariry
10. Geyer CE, Forster J, Lindquist D, et al: Lapa- 19. Drucker B, Bacik J, Ginsberg M, et al: Phase II
REFERENCES tinib plus capecitabine for HER2-positive advanced trial of ZD1839 (IRESSA) in patients with advanced
breast cancer. N Engl J Med 355:2733-2743, 2006 renal cell carcinoma. Invest New Drugs 21:341-345,
1. Lipworth T, Tarone RE, McLaughin JK: The 11. Medical Research Council Renal Cancer Col- 2003
epidemiology of renal cell carcinoma. J Urol 176: laborators: Interferon-alpha and survival in meta- 20. Dawson NA, Guo C, Zak R, et al: A phase II
2353-2358, 2006 static renal carcinoma: Early results of a randomised trial of ZD1839 in stage IV and recurrent renal cell
2. Rohrmann K, Staehler M, Haseke N, et al: controlled trial. Lancet 353:14-17, 1999 carcinoma. Clin Cancer Res 10:7812-7819, 2004
Immunotherapy in metastatic renal cell carcinoma. 12. Atzpodien J, Hoffmann R, Franzke M, et al: 21. Jermann M, Stahel RA, Salzberg M, et al: A
World J Urol 23:196-201, 2005 Thirteen-year, long-term efficacy of interferon 2al- phase II, open-label study of gefitinib (IRESSA) in
3. Motzer RJ, Hutson TE, Tomczak P, et al: pha and interleukin 2-based home therapy in pa- patients with locally advanced, metastatic, or re-
Sunitinib versus interferon alfa in metastatic renal- tients with advanced renal cell carcinoma. Cancer lapsed renal-cell carcinoma. Cancer Chemother
cell carcinoma. N Engl J Med 356:115-124, 2007 95:1045-1050, 2002 Pharmacol 57:533-539, 2006
4. Escudier B, Eisen T, Stadler WM, et al: Sor- 13. Stebbing J, Benson C, Eisen T, et al: The 22. Beeram M, Rowinsky EK, Weiss GR, et al:
afenib in advanced clear-cell renal-cell carcinoma. treatment of advanced renal cell cancer with high- Durable disease stabilization and antitumor activity
N Engl J Med 356:125-134, 2007 dose oral thalidomide. Br J Cancer 85:953-958, 2001
with OSI-774 in renal cell carcinoma: A phase II,
14. Therasse P, Arbuck SG, Eisenhauer EA, et al:
5. Moch H, Sauter G, Buchholz N, et al: Epider- pharmacokinetic (PK) and biological correlative study
New guidelines to evaluate the response to treat-
mal growth factor receptor expression is associated with FDG-PET imaging. J Clin Oncol 22:207s, 2004
ment in solid tumors: European Organization for
with rapid tumor cell proliferation in renal cell carci- (suppl; abstr 3050)
Research and Treatment of Cancer, National Cancer
noma. Hum Pathol 28:1255-1259, 1997 23. Hainsworth JD, Sosman JA, Spigel DR, et al:
Institute of the United States, National Cancer Insti-
6. Prewett M, Rothman M, Waksal H, et al: Treatment of metastatic renal cell carcinoma with a
tute of Canada. J Natl Cancer Inst 92:205-216, 2000
Mouse-human chimeric anti-epidermal growth fac- combination of bevacizumab and erlotinib. J Clin
15. National Cancer Institute: National Cancer In-
tor receptor antibody C225 inhibits the growth of Oncol 23:7889-7896, 2005
stitute Common Toxicity Criteria version 2.0. http://
human renal cell carcinoma xenografts in nude 24. Bukowski RM, Kabbinavar F, Figlin RA, et al:
ctep.cancer.gov/forms/CTCv20_4-30-992.pdf
mice. Clin Cancer Res 4:2957-2966, 1998 16. Motzer RJ, Bacik J, Schwartz LH, et al: Prog- Randomized phase II or erlotinib combined with
7. Merseburger AS, Hennenlotter J, Simon P, et nostic factors for survival in previously treated pa- bevacizumab compared with bevacizumab alone in
al: Membranous expression and prognostic implica- tients with metastatic renal cell carcinoma. J Clin metastatic renal cell carcinoma. J Clin Oncol 25:
tions of epidermal growth factor receptor protein in Oncol 22:454-463, 2004 4536-4541, 2007
human renal cell cancer. Anticancer Res 25:1901- 17. Motzer RJ, Amato R, Todd M, et al: Phase II 25. Stumm G, Eberwein S, Rostock-Wolf S, et al:
1907, 2005 trial of antiepidermal growth factor receptor anti- Concomitant overexpression of the EGFR and
8. Smith K, Gunaratnam L, Morley M, et al: body C225 in patients with advanced renal cell erbB-2 genes in renal cell carcinoma (RCC) is corre-
Silencing of epidermal growth factor receptor sup- carcinoma. Invest New Drugs 21:99-101, 2003 lated with dedifferentiation and metastasis. Int J
presses hypoxia-inducible factor-2-driven VHL-/- re- 18. Rowinsky EK, Schwartz GH, Gollob JA, et al: Cancer 69:17-22, 1996
nal cancer. Cancer Res 65:5221-5230, 2005 Safety, pharmacokinetics, and activity of ABX-EGF, 26. Langner C, Ratschek M, Rehak P, et al: Ste-
9. Latif Z, Watters AD, Bartlett JM, et al: Gene a fully human anti-epidermal growth factor receptor roid hormone receptor expression in renal cell car-
amplification and overexpression of HER2 in renal monoclonal antibody in patients with metastatic cinoma: An immunohistochemical analysis of 182
cell carcinoma. BJU Int 89:5-9, 2002 renal cell cancer. J Clin Oncol 22:3003-3015, 2004 tumors. J Urol 171:611-614, 2004
■ ■ ■
Acknowledgment
We thank the patients who participated in this study and their families; the medical, nursing, and research staff; the independent monitoring
committee; the monitors, staff, data managers, and statisticians (N. Compton, H. Hassani) at GlaxoSmithKline; and the editorial assistance of
L. Pender from The Phillips Group Oncology Communications.
Appendix
The Appendix is included in the full-text version of this article, available online at www.jco.org. It is not included in the PDF version
(via Adobe® Reader®).
www.jco.org © 2008 by American Society of Clinical Oncology 2291
Downloaded from ascopubs.org by 114.125.228.88 on September 9, 2019 from 114.125.228.088
Copyright © 2019 American Society of Clinical Oncology. All rights reserved.
You might also like
- Idr 12 745 PDFDocument13 pagesIdr 12 745 PDFAgung Budi PamungkasNo ratings yet
- Pi Is 0749806319304943Document7 pagesPi Is 0749806319304943Agung Budi PamungkasNo ratings yet
- Pi Is 0969212619303090Document11 pagesPi Is 0969212619303090Agung Budi PamungkasNo ratings yet
- s41586 019 1545 0 PDFDocument22 pagess41586 019 1545 0 PDFAgung Budi PamungkasNo ratings yet
- Idr 12 745 PDFDocument13 pagesIdr 12 745 PDFAgung Budi PamungkasNo ratings yet
- Profile of HBV Integration in The Plasma DNA of Hepatocellular Carci-Noma PatientsDocument8 pagesProfile of HBV Integration in The Plasma DNA of Hepatocellular Carci-Noma PatientsAgung Budi PamungkasNo ratings yet
- Nutrients: Vitamin C Status and Cognitive Function: A Systematic ReviewDocument21 pagesNutrients: Vitamin C Status and Cognitive Function: A Systematic ReviewAgung Budi PamungkasNo ratings yet
- Pi Is 0969212619303090Document11 pagesPi Is 0969212619303090Agung Budi PamungkasNo ratings yet
- Hybt VTVRDocument12 pagesHybt VTVRAgung Budi PamungkasNo ratings yet
- Hargreave2018 Jurnal PDFDocument8 pagesHargreave2018 Jurnal PDFAgung Budi PamungkasNo ratings yet
- Pi Is 1470204519304565Document13 pagesPi Is 1470204519304565Agung Budi PamungkasNo ratings yet
- Clinical Practice GuidelinesDocument3 pagesClinical Practice GuidelinessigitNo ratings yet
- Jamaoncology Sledge 2019 Oi 190093Document9 pagesJamaoncology Sledge 2019 Oi 190093Agung Budi PamungkasNo ratings yet
- Main PDFDocument12 pagesMain PDFAgung Budi PamungkasNo ratings yet
- AnnOncol 2012 Chan Vii83 5 PDFDocument3 pagesAnnOncol 2012 Chan Vii83 5 PDFAgung Budi PamungkasNo ratings yet
- Pi Is 1470204519304565Document13 pagesPi Is 1470204519304565Agung Budi PamungkasNo ratings yet
- 2.7 Yuseva Pengaruh MgSO4 MaDocument8 pages2.7 Yuseva Pengaruh MgSO4 MaUPI RSBRNo ratings yet
- Hargreave2018 JurnalDocument8 pagesHargreave2018 JurnalAgung Budi PamungkasNo ratings yet
- 2.7 Yuseva Pengaruh MgSO4 MaDocument8 pages2.7 Yuseva Pengaruh MgSO4 MaUPI RSBRNo ratings yet
- Obstetrical Complications in Women With Endometriosis: A Cohort Study in JapanDocument12 pagesObstetrical Complications in Women With Endometriosis: A Cohort Study in JapanAgung Budi PamungkasNo ratings yet
- Landscape of Enhancer-Enhancer Cooperative Regulation During Human Cardiac CommitmentDocument12 pagesLandscape of Enhancer-Enhancer Cooperative Regulation During Human Cardiac CommitmentAgung Budi PamungkasNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Approved Harmonized National RD Agenda 2017-2022 PDFDocument90 pagesApproved Harmonized National RD Agenda 2017-2022 PDFJoemel Bautista100% (1)
- Organisational Change and Stress ManagementDocument18 pagesOrganisational Change and Stress ManagementDisha GanatraNo ratings yet
- Anosognosia FSDocument2 pagesAnosognosia FSraquel perezNo ratings yet
- Management of Normal Labor and PartographDocument89 pagesManagement of Normal Labor and PartographKIPA SHRESTHANo ratings yet
- FAMILY NURSING CARE PLAN - AsthmaDocument1 pageFAMILY NURSING CARE PLAN - AsthmaJULIANNE BAYHON80% (5)
- Cerebral Palsy Care Giving GuideDocument511 pagesCerebral Palsy Care Giving GuideJoel OntiverosNo ratings yet
- Meinhardt WaterborneDiseaseDocument3 pagesMeinhardt WaterborneDiseaseਮਕੁਮਾਰNo ratings yet
- Research Interest Potential Advisors International StudentsDocument12 pagesResearch Interest Potential Advisors International StudentsAKREDITASI RS KOTA SERANGNo ratings yet
- Doloplus 2 ToolDocument3 pagesDoloplus 2 ToolHaMy NguyenNo ratings yet
- Fast Food Addiction: A Major Public Health ConcernDocument12 pagesFast Food Addiction: A Major Public Health ConcernA. K. Mohiuddin100% (1)
- The Health Insurance WorkbookDocument12 pagesThe Health Insurance WorkbookLarry ThomasNo ratings yet
- Mission HR Handbook Ocb Template Revision May 2018Document12 pagesMission HR Handbook Ocb Template Revision May 2018Mohammed HammadiNo ratings yet
- Operator Edge 6 Wkphase 1 V2Document23 pagesOperator Edge 6 Wkphase 1 V2Luis Santamaría Álvarez-Gómez0% (1)
- Shaping A Humane World Edward J. Valeau, Rosalind L. RabyDocument17 pagesShaping A Humane World Edward J. Valeau, Rosalind L. RabySTAR ScholarsNo ratings yet
- Megan Haky: M.M.Haky@eagle - Clarion.eduDocument2 pagesMegan Haky: M.M.Haky@eagle - Clarion.eduapi-285540869No ratings yet
- Ab'Asanas (Expanded & Updated)Document56 pagesAb'Asanas (Expanded & Updated)Nicola AvonNo ratings yet
- Attachment Styles View of Self and Negative AffectDocument16 pagesAttachment Styles View of Self and Negative AffectStephanie MokashiNo ratings yet
- Pediatrics Wards History Taking TemplateDocument2 pagesPediatrics Wards History Taking TemplateBobet Reña80% (5)
- 7-A CengcengDocument11 pages7-A CengcengBela RonaldoeNo ratings yet
- G8 Health Q4 LM CigarettesDocument39 pagesG8 Health Q4 LM CigarettesJoseph R. GallenoNo ratings yet
- Medical-Cert BlsDocument1 pageMedical-Cert BlsYram Yoj ZeraujNo ratings yet
- Lecture 3Document6 pagesLecture 3api-707529158No ratings yet
- Admission and DischargeDocument14 pagesAdmission and DischargeDaryl Adrian Recaido100% (1)
- Unit Time (HRS) Learning Objective Teaching Learning Activities EvaluationDocument12 pagesUnit Time (HRS) Learning Objective Teaching Learning Activities EvaluationSAYMABANUNo ratings yet
- Mom-20 03 2024Document7 pagesMom-20 03 2024smn.ussharNo ratings yet
- Report Risk Management For HospitalsDocument10 pagesReport Risk Management For Hospitalsresh0401404100% (1)
- Stages of Oil Spill ResponseDocument1 pageStages of Oil Spill Responseapi-575247814No ratings yet
- Argumentative Essay REGDocument18 pagesArgumentative Essay REGMaeva AlexandreNo ratings yet
- Hospital 1Document45 pagesHospital 1shaista siddiqueNo ratings yet
- Household 1Document2 pagesHousehold 1ainun rapikaNo ratings yet