Professional Documents
Culture Documents
Aromaterapia Alzheimer PDF
Uploaded by
Anonymous aBzTQbeiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aromaterapia Alzheimer PDF
Uploaded by
Anonymous aBzTQbeiCopyright:
Available Formats
doi:10.1111/j.1479-8301.2009.00299.
x PSYCHOGERIATRICS 2009; 9: 173–179
ORIGINAL ARTICLE
Effect of aromatherapy on patients with Alzheimer’s disease psyg_299 173..179
Daiki JIMBO,1 Yuki KIMURA,1 Miyako TANIGUCHI,1 Masashi INOUE2 and Katsuya URAKAMI1
1
Section of Environment and Health Science, Abstract
Department of Biological Regulation, School of
Health Science, Faculty of Medicine and 2Informa- Objective: Recently, the importance of non-pharmacological therapies for
tion Media Center, Tottori University, Yonago, Japan dementia has come to the fore. In the present study, we examined the
Correspondence: Dr Katsuya Urakami PhD MD, curative effects of aromatherpay in dementia in 28 elderly people, 17 of
Section of Environment and Health Science, whom had Alzheimer’s disease (AD).
Department of Biological Regulation, School of
Methods: After a control period of 28 days, aromatherapy was performed
Health Science, Faculty of Medicine, Tottori Uni-
versity, Nishimachi 86, Yonago 683-8503, Japan. over the following 28 days, with a wash out period of another 28 days.
Email: kurakami@med.tottori-u.ac.jp Aromatherapy consisted of the use of rosemary and lemon essential oils in
Received 9 March 2009; accepted 31 August 2009. the morning, and lavender and orange in the evening. To determine the
effects of aromatherpay, patients were evaluated using the Japanese version
of the Gottfries, Brane, Steen scale (GBSS-J), Functional Assessment
Staging of Alzheimer’s disease (FAST), a revised version of Hasegawa’s
Dementia Scale (HDS-R), and the Touch Panel-type Dementia Assessment
Scale (TDAS) four times: before the control period, after the control period,
after aromatherpay, and after the washout period.
Results: All patients showed significant improvement in personal orienta-
tion related to cognitive function on both the GBSS-J and TDAS after
therapy. In particular, patients with AD showed significant improvement in
total TDAS scores. Result of routine laboratory tests showed no significant
changes, suggesting that there were no side-effects associated with the use
of aromatherapy. Results from Zarit’s score showed no significant changes,
suggesting that caregivers had no effect on the improved patient scores
seen in the other tests.
Key words: Alzheimer’s disease, aromatherapy, Conclusions: In conclusion, we found aromatherapy an efficacious non-
cognitive function, dementia, elderly people, pharmacological therapy for dementia. Aromatherapy may have some
non-pharmacological therapy. potential for improving cognitive function, especially in AD patients.
INTRODUCTION formed to complement the effects of pharmacothera-
Japan, having the highest life expectancy in the world, peutics and health care services, such as nursing
has seen a remarkable increase in senile dementia in home, day care etc., for elderly paitents. Aroma-
recent years. This has become a big social problem, therapy is one of the therapies used in comple-
with Alzheimer’s disease (AD) accounting for approxi- mentally alternative medicine.4,5 In recent years,
mately half the number of cases of dementia.1,2 Thus, non-pharmacological intervention has been based on
preventive medicine for dementia has become more the viewpoint of brain rehabilitation and the possible
important.3 Recently, complementary alternative prevention of senile dementia has also been reported
medicine, which, in addition to using medications, and non-pharmacological treatments other than aro-
also makes use of various ‘non-pharmacological’ matherapy, such as memory training, music therapy,
approaches, has become an attractive alternative in the recollection method, animal-assisted therapy,
the treatment of senile dementia after the introduction and optical treatment, have been studied.6–8 Aroma-
of elderly care insurance. These treatments are per- therapy experientially classifies the effect of the scent
© 2010 The Authors 173
Journal compilation © 2010 Japanese Psychogeriatric Society
D. Jinbo et al.
through the essential oil extracted from the plant, a pected that patients’ cognitive function could be
traditional treatment used according to its effect, improved by stimulation through the sense of smell.
and is used in many fields. In the present study, the The aromatherapy treatment used in the present
aromatherapy applied did not include mainstream study is is physically safer and easier to apply than
aroma massage, aroma baths etc. (including touch mainstream treatments, such as massage and baths,
therapy) because physical problems, such as low- so the operator feels no limitation because he or she
temperature burns, may occur in some cases.4,5,9–11 can work through purely aromatic means.
The mechanism(s) of action of underlying the effects Initially, the level of congnitive function was
of aromatherapy are not known for certain. In healthy assessed using the Gottfries, Brane, Steen (GBSS-J)
people, essential oils of rosemary and lavender are and Touch-panel type Dementia Assessment Scale
commonly used and there is at least one report (TDAS). Aromatherapy was applied to AD patients
showing that these oils influence feelings about a using a combination of a lavender oil–orange oil solu-
person’s surroundings.12 Moreover, lavender oil has tion, which activates the parasympathetic nervous
been reported to improve sleep disorders.13,14 It has system, with a rosemary oil–lemon oil solution used to
also been reported that the essential oil of lemon relieve depression and heighten concentration. In this
affects the anti-oxidant action of vitamin E and preliminary phase of the investigation, the possibility
improves the state of blood vessels near the skin.15 that the cognitive function could improve in AD
Although there are few reports on aromatherapy in patients following aromatherapy was discovered and
senile dementia, it has been suggested that aroma- the validity of using aromatherapy in AD patients was
therapy may bring about some feeling of relief and examine further.
the ability to act on outside influences such that the
obstacle to action in senile dementia can be coped
METHODS
with.10 However, there are no reports of the effects of
Patients
aromatherapy on cognitive functional disorder, often
In total, 28 elderly people (mean age 86.1 1 6.9 years)
seem in cases of dementia and the central feature of
were involved in the study. Seventeen patients had AD
senile dementia. Disorders of cognitive function pose
(two men, 15 women; mean age 86.3 1 6.4 years),
considerable problems for both AD patients and care
three had vascular dementia (VaD; all women; mean
workers.
age 89.7 1 5.5 years), and eight had other diagnoses,
The action of aromatherapy begins from a smell
including, among others, a mixed case of AD and
molecule combined with an acceptor peculiar to each
cerebrovascular lesions (CVL; all women; mean age
specific odor. The smell molecule passes along the
84.5 1 8.3 years). We provided patients and their fami-
nasal cavity and adheres to the olfactory epithelium.
lies with detailed information regarding the methods
The stimulus is transmitted to the hippocampus or
and purpose of the study (Table 1) and informed
cerebral limbic system and amygdaloid body through
consent was obtained. Patients with AD were diag-
the olfactory nerve system currently concentrated on
nosed by the DSM-IV18 and NINCDS-ADRDA,19
the olfactory epithelium. Although this process is
whereas patients with CVL were diagnosed using
deeply related to cognitive function, the odor is rec-
DSM-IV and NINCDS-AIREN.20
ognized and the stimulus sends information to the
hypothalamus on which it was projected by the cere-
bral limbic system, which then adjusts the autonomic Methodology
nervous system and the internal secretory system, The examine the effect of mixed aromas, a crossover
guiding a series of vital reactions in the hippocampus method was used in the present study. To evaluate
or amygdaloid body, such as the discharge of neu- the persistence of any effect of the aromatherapy, a
rotransmitters. In brief, aromatherapy is the result washout period of 28 days was included after the 28
of the vital reaction that occurs through the smell days of aromatherapy. Furthermore, to examine in
molecule. detail how the aromatherapy influenced cognitive
Although some reports have proposed that the function in dementia patients, the TDAS was applied
sense of smell is decreased in AD patients, nerve as a highly sensitive test with little influence from the
rebirth through smell is possible.16,17 We also sus- investigator.
174 © 2010 The Authors
Journal compilation © 2010 Japanese Psychogeriatric Society
Aromatherapy for Alzheimer’s disease
Table 1 Distribution of subjects according to Functional Assessment Staging of Alzheimer’s disease (FAST) assessment
Mean (1SD)
FAST3-5 FAST6-7 Total age (years)
AD 5 (0/5) 12 (2/10) 17 (2/15) 86.3 1 6.4
VaD 1 (0/1) 2 (0/2) 3 (0/3) 89.7 1 5.5
Others 3 (0/3) 5 (0/5) 8 (0/8) 84.5 1 8.3
Total 9 (0/9) 19 (2/17) 28 (2/26) 86.1 1 6.9
Mean (1SD) age (years) 83 1 6.9 87 1 6.2 86.1 1 6.9
Data show the number of patients in each group, with the number of men/women given in parentheses.
FAST3-5, mild to moderate Alzheimer’s disease (AD); FAST6-7, severe AD; AD, Alzheimer’s disease; VaD, cerebrovascular dementia; Others, mixed dementia
and other dementia.
After a control period of 28 days, aromatherapy Table 2 Study schedule
was performed over the following 28 days, followed Before 1 1 week
by a 28-day wash out period. During the control and Control period 4 weeks
wash out periods, patients did not receive any treat- Before 2 1 week
Aromatherapy period 4 weeks
ment. During the 28 days of aromatherapy, patients After 1 1 week
were exposed to the aroma of 0.04 mL lemon and Wash out period 4 weeks
0.08 mL rosemary essential oil in the morning from After 2 1 week
0900 to 1100 hours and to 0.08 mL lavender and To evaluate the effects of aromatherapy, tests were performed up to four
times throughout the schedule.
0.04 mL orange essential oils in the evening from
1930 to 2100 hours. The oils were placed on a piece
of gauze in diffusers with an electric fan. (All essential
Table 3 Tests used in the present study
oils and diffusers used in the present study were pro-
Before 1 Before 2 After 1 After 2
duced by the Peace of Mind Company (Tokyo,
Japan).) Two diffusers were set up in each room where HDS-R ✓ ✓ ✓ ✓
GBS ✓ ✓ ✓ ✓
patients had been moved. The essential oils (rose- FAST ✓ ✓ ✓ ✓
mary and lemon; lavender and orange) were then CT ✓ ✕ ✕ ✕
mixed as described above. The lemon and rosemary Blood Examination ✓ ✕ ✓ ✕
Biochemical Examination ✓ ✕ ✓ ✕
mix activates the sympathetic nervous system to TDAS ✓ ✓ ✓ ✓
strengthen concentration and memory, whereas the Zarit ✓ ✓ ✓ ✓
lavender and orange fragrance activates the parasym- ✓, test performed; ✕, test not performed; FAST, Functional Assessment
pathetic nervous system to calm patients’ nerves. The Staging of Alzheimer’s disease; HDS-R, revised version of Hasegawa’s
Dementia Scale; GBSS-J, Japanese version of the Gottfries, Brane, Steen
mixtures used in the mornings and evenings were scale; CT, computed tomography; TDAS, Touch Panel-type Dementia
changed because this method is known, through Assessment Scale.
experience, to synchronize the autonomic nervous
system to the circadian rhythm: the sympathetic nerve
system works predominantly after stimulation by Japanese version of the Gottfries, Brane, Steen (GBS)
rosemary–lemon oil in the morning, whereas the para- Scale)21 was used to determine the effect of medical
sympathetic nerve system works predominantly after treatment because this test is currently used in the
activation by the lavender–orange oil at night. Patients evaluation of pateints with AD. The GBSS-J consists
were evaluated at four time points throughout the of five items: GBSS-J-A (cognitive function), GBSS-
study: ‘Before 1’, consisting of 7 days of tests, fol- J-B (spontaneity), GBSS-J-C (feeling function),
lowed by the 28-day control period; ‘Before 2’, tests GBSS-J-D (other moral condition), and GBSS-J-E
for 7 days, followed by aromatherapy for the next 28 (movement function).
days; ‘After 1’, tests for the 7 days, followed by 28 The degree of AD was determined in patients using
days wash out; and ‘After 2’, tests for 7 days after the the Functional Assessment Staging of Alzheimer’s
28-day wash out period (Table 2). disease (FAST).22 This test is based on observation of
Tests were administered to patients according to patients with AD and classifies the level of dementia
the schedule given in Table 3. The GBSS-J scale (the into seven stages. To apply the FAST, the evaluator
© 2010 The Authors 175
Journal compilation © 2010 Japanese Psychogeriatric Society
D. Jinbo et al.
Table 4 Test results in dementia patients that did not exhibit significant changes after aromatherapy
Befere 1 Before 2 After 1 After 2 P value
FAST 5.64 1 1.32 5.58 1 1.37 5.53 1 1.07 5.76 1 0.97 0.573
HDS-R 11.06 1 7.72 10.61 1 7.49 10.27 1 7.72 10.56 1 7.83 0.833
GBSS-J-B 10.65 1 7.24 9.88 1 7.05 11.06 1 8.3 11.35 1 7.31 0.174
GBSS-J-C 10.29 1 7.54 9.76 1 7.05 11.2 1 7.09 11.65 1 7.48 0.463
GBSS-J-D 7.24 1 7.44 8.71 1 5.97 7.18 1 4.64 8.47 1 6.74 0.499
GBSS-J-E 15.65 1 8.98 15.18 1 8.91 15.88 1 9.55 17.59 1 8.74 0.071
FAST, Functional Assessment Staging of Alzheimer’s disease; HDS-R, revised version of Hasegawa’s Dementia Scale; GBSS-J, Japanese version of the
Gottfries, Brane, Steen scale.
needs to observe the patient objectively and obtain priately. In total, this questionnaire consists of 24
information from the nurse or care giver. As a screen- items about a care worker’s mental and economic
ing tool, the revised version of Hasegawa’s dementia burden.
scale (HDS-R) was used.23 Finally, a simple touch All results were compared by repeated-measures
panel was used to identify possible dementia (the ANOVA and Scheffé’s post hoc test using the Statview
Touch Panel-type Dementia Assessment Scale; software for analysis.
TDAS). One part of the TDAS is a modification of
the Alzheimer disease Assessment Scale (ADAS),24 a RESULTS
method used to evaluate cognitive function. The There were no significant differences between
TDAS clarifies the level of cognitive dysfunction by patients with dementia for most items, except for
using problems involving word recognition, vocal those evaluating actual function, such as GBSS-J-B
orders, figure recognition, understanding the concept (spontaneity), GBSS-J-C (feeling function), and
of mail, understanding knowledge items, money cal- GBSS-J-D (other psychotic manifestations), before
culation, recall of names and dates, the use of tools and after aromatherapy (Table 4). However, a signifi-
and being able to tell the time on a clock. An experi- cant improvement was seen in GBSS-J-A-13
enced TDAS investigator can easily inspect these (abstract function) in the FAST3-5 AD (mild–moderate
data in approximately 20 min per subject, but even AD) group (P < 0.05; Fig. 1).
in the absence of an experienced investigator, the There were no significant difference in HDS-R, in
test only takes approximately 40 min. In the TDAS, the transition of the FAST score or in the results of
decreasing scores indicate cognitive improvement. routine laboratory tests.
The four dementia assessment scales (i.e. TDAS, Although there were no significant changes on the
GBSS-J, FAST, and HDS-R) were applied by nurses TDAS for each of the individual items described above
and/or care workers. (i.e. word recognition, vocal orders etc.), some
In addition, head computed tomography (CT) improvement was seen in the overall score for the
scans were performed for all patients. A patient with a TDAS in all patient groups (P < 0.05; Fig. 2). Some
low-density area on the CT scan without history of significant improvement was noted in concept under-
stroke was considered as having CVL. Routine labo- standing (P < 0.05; Fig. 3). The overall total points for
ratory tests, such as blood analysis and biochemi- TDAS in the AD patient group were improved after
cal examination, were performed before and after aromatherpay (P < 0.01; Fig. 2).
aromatherapy. Finally, there were no significant differences differ-
Finally, two questions were added to the care ences in any items on the Zarit scale before and after
burden evaluation scale (Zarit)25 for 21 care workers. aromatherapy (Fig. 4).
Originally, the Zarit scale was designed to evaluate a
family’s care load so, in the present study, the ques- DISCUSSION
tions ‘Do you think the patient’s excreta is unpleas- In the present study, aromatherapy was performed
ant?’ and ‘Do you think that you unknowingly present on dementia patients and was found to improve
an unpleasant face to the patient?’ were added to the ability to form abstract ideas. In addition, some
help judge the nursing staff’s care load more appro- improvement in movement was noted. Furthermore,
176 © 2010 The Authors
Journal compilation © 2010 Japanese Psychogeriatric Society
Aromatherapy for Alzheimer’s disease
4.0 5.2
3.5 4.7
understanding score
GBSSJ-A-13 score
4.2
TDAS concept
3.0 *
3.7 *
2.5
3.2
2.0 2.7
1.5 2.2
1.7
1.0 1 2 1 2
1 2 1 2
Before After Before After
Figure 1 Changes in scores for item A-13 (abstract function) of the Figure 3 Change in Touch Panel-type Dementia Assessment Scale
the Japanese version of the Gottfries, Brane, Steen scale (GBSS-J) (TDAS; concept understanding) scores before the control period
in patients identifed as 3-5 on the Functional Assessment Staging (Before 1), after the control period (Before 2), after aromatherpay
of Alzheimer’s disease (FAST), before the control period (Before 1), (After 1), and after the washout period (After 2). Significant improve-
after the control period (Before 2), after aromatherpay (After 1), and ment in ideational praxis function after aromatherapy was
after the washout period (After 2). Significant improvement in cog- observed. Data are the mena 1 SEM. *P < 0.05 (repeated-measures
nitive function was observed after aromatherapy. Data are the ANOVA).
mena 1 SEM. *P < 0.05 (repeated-measures ANOVA).
20
35
15
30
Zarit score
TDAS score
10
25
* NS
20 5
†
15 0
1 2 1 2
1 2 1 2 Before After
Before After
Figure 4 Change in Zarit’s score before the control period (Before
Figure 2 Change in Touch Panel-type Dementia Assessment Scale 1), after the control period (Before 2), after aromatherpay (After 1),
(TDAS) scores in all subjects (䉬) and in patients with Alzheimer’s and after the washout period (After 2). There was no significant
disease (AD; 䊏), before the control period (Before 1), after the change in Zarit’s score after aromatherapy.
control period (Before 2), after aromatherpay (After 1), and after the
washout period (After 2). All subjects showed significant improve-
ment in cognitive function after aromatherapy, as did patients with
AD. Data are the mena 1 SEM. *P < 0.05, †P < 0.01 (repeated- significant changes on the HDS-R after aromatherapy.
measures ANOVA). Some studies of the effects of aromatherapy have
used scales evaluating behavioral and psychological
symptoms of dementia (BPSD).6-8 However, on the
using the TDAS, improvements in cognitive function basis of the results of the present study, our view is
were noted for the entire group, with some improve- that the most important effect of aromatherapy in
ment in conceptual understanding. Although no sig- dementia is on cognitive function. Thus, the main aim
nificant differences were seen in other disease of the present study was to determine whether aro-
groups, slight improvement in cognitive function was matherapy can improve cognitive disorders.
found in patients with moderate AD. Consequently, The TDAS results suggest an improvement in
we believe that aromatherapy effectively improves recognition after aromatherapy. Nevertheless, total
cognitive function and may be particularly effective for scores for abstract thinking and motor function on
patients with moderate AD. We did not observe any the GBSS-J remained the same. During preliminary
© 2010 The Authors 177
Journal compilation © 2010 Japanese Psychogeriatric Society
D. Jinbo et al.
investigations, we noted some improvement in the thus, the nursing load did not change and could
total score for GBSS-J-A (cognitive function) and not have impacted on the improvements in cogni-
GBSS-J-B (spontaneity) with less aromatherapy oil tive function seen or on general results of patient
than that used in the present study. Moreover, based evaluation.
on results of our preliminary investigations, the Complementary alternative medicines need to be
effects observed depend on the amount of aroma- safe. To confirm the safety of the aromatherapy used
therapy oil used. Thus, a stronger effect may be in the present study, we performed routine labora-
obtained by increasing the amount of the oil used. tory tests, such as blood analysis and biochemical
Conversely, although we did not see any significant examinations, before and after the treatment. There
effect on HDS-R, this doesn’t mean that aroma- were no significant differences in any of the param-
therapy is not effective. The HDS-R is simply a scale eters evaluated, indicating no deleterious side-
used for screening test for patients with dementia effects from the aromatherapy. Based on these
and, perhaps, we were not able to demonstrate any results, we believe that cognitive dysfunction, the
any cognitive improvement on screening because cental symptom of AD, improves after aromatherapy.
the HDS-R is a screening test with low sensitivity. As far as we know, the present study is the first
One of the limitations of the present study is the low to investigate the possibility of improved cognitive
patient numbers. In future studies, a greater number function with simulatneous improvemenmts in other
of patients may need to be evaluated to clearly dem- symptoms of AD using aromatherapy. We confirmed
onstrate the effect of aromatherapy in cognitive dis- that aromatherapy using pure aromas is safe.
orders. Stimulation of the sense of smell is projected Anyone can understand how easy it is to perform
to the cerebral limbic system. Very important areas, this type of treatment, which appears to be an effec-
such as the hippocampus and the amygdaloid body, tive complement to conventional therapy. Moreover,
are part of the cerebral limbic system. These are aromatherapy can be used not only a treatment, but
strongly related to the cognitive impairment that is the also as a preventive measure because it influences
central symptom of dementia. Moreover, neurofibril- neuropoiesis.
lary tangles (NFT) are observed in the early stages of Now that adult day care, brain rehabilitation, and
AD in the entorhinal cortex, hippocampus, amygdal- dementia syndrome prevention classrooms are
oid body, and thalamus, which receive stimulation becoming more and more necessary, it is thought that
from the cerebral limbic system.26,27 On the basis of aromatherapy may be very profitable as one type of
these observations, it has been suggested that the program in the near future. It will be necessary to
olfactory area is closely related to AD and the devel- verify the effect of this treatment, as well as the under-
opment of dysosmia in early AD may support this lying mechanism of action, from both a clinical and
hypothesis. Neuropoiesis in the human hippocampal biological perspective in order to establish a clear
dentate gyrus and subventricular zone is controlled by methodology for the use of aromatherapy in the
various environmental agents, but continues through- future. We are currently examining these issues by
out life.28 One hypothesis states that stimulation by investigating the effects of aromatherapy on cell
smell promotes neuropoiesis in the human hippocam- differentiation.
pal dentate.17 There is also a report that indicates a
positive effect of pleasant surroundings of levels of
senile plaques.29 ACKNOWLEDGMENTS
In brief, it is thought that neuropoesis, reinforced by The authors thank Professor Hiroyuki Arai, Dr Takae
stimulation from smell projected to the cerebral limbic Ebihara, and Dr Satoru Ebihara ( Department of Geri-
system, plays an important role in improving cognitive atrcs and Gerontology, Center for Asian Traditional
function. However, aromatherapy has positive effects Medicine) for their advice in the writing of this article.
on care givers in addition to the possibility of improv- In addition, the authors thank Rieko Hosoda, Aki
ing a patient’s actual function. To investigate these Yonehara, Junko Hasegawa, Norie Kojima, Yuriko
factors, we evaluated Zarit’s score to determine the Shimizu, Yasuko Morimoto, Takao Yorita, and Ryouhei
care load level. However, there appeared to be no Ojima (Yonago Chukai Hospital and Nursing Home,
significant change in Zarit’s score after aromatherapy; Awashima) for their cooperation with this study.
178 © 2010 The Authors
Journal compilation © 2010 Japanese Psychogeriatric Society
Aromatherapy for Alzheimer’s disease
REFERENCES oxidation of low density lipoprotein. Arzneimittelforschung
2001; 51: 799–805.
1 Urakami K, Adachi Y, Wakutani Y et al. Epidemiologic and
16 Peters JM, Hummel T, Kratzsch T, Lotsch J, Skarke C, Frolich L.
genetic studies of dementia of the alzheimer type in japan.
Olfactory function in mild cognitive impairment and Alzheimer’s
Dement Geriatr Cogn Disord 1998; 9: 294–298.
disease: An investigation using psychophysical and electro-
2 Yamada T, Hattori H, Miura A, Tanabe M, Yamori Y. Prevalence
physiological techniques. Am J Psychiatry 2003; 160: 1995–
of Alzheimer’s disease, vascular dementia and dementia with
2002.
Lewy bodies in a Japanese population. Psychiatry Clin Neurosci
17 Eriksson PS, Perfilieva E, Bjork-Eriksson T et al. Neurogenesis in
2001; 55: 21–25.
the adult human hippocampus. Nat Med 1998; 4: 1313–1317.
3 Urakami K. Prevention of dementia. Psychogeriatrics 2007; 7:
18 American Psychiatric Association. Diagnostic and Statistical
93–97.
Manual of Mental Disorders (DMS-IV). Washington, DC: America
4 Ballard CG, O’Brien JT, Reichelt K, Perry EK. Aromatherapy as
Psychiatric Association, 1987.
a safe and effective treatment for the management of agitation
19 McKhann G, Drachman D, Folstein M, Katzman R, Price D,
in severe dementia: The results of a double-blind, placebo-
Stadlan EM. Clinical diagnosis of Alzheimer’s disease: Report of
controlled trial with melissa. J Clin Psychiatry 2002; 63: 553–
the NINCDS-ADRDA Work Group under the auspices of Depart-
558.
ment of Health and Human Services Task Force on Alzheimer’s
5 Smallwood J, Brown R, Coulter F, Irvine E, Copland C. Aroma-
Disease. Neurology 1984; 34: 939–944.
therapy and behaviour disturbances in dementia: A randomized
20 Roman GC, Tatemichi TK, Erkinjuntti T et al. Vascular dementia:
controlled trial. Int J Geriatr Psychiatry 2001; 16: 1010–1013.
Diagnostic criteria for research studies. Report of the NINDS-
6 Kawamura N, Niiyama M, Niiyama H. Long-term evaluation of
AIREN International Workshop. Neurology 1993; 43: 250–260.
animal-assisted therapy for institutionalized elderly people: A
21 Homma A, Niina R, Ishii T, Hasegawa K. Behavioral evaluation
preliminary result. Psychogeriatrics 2007; 7: 8–13.
of Alzheimer disease in clinical trials: Development of the Japa-
7 Yamamoto-Mitani N, Matsuoka K, Fujii M. Home-based reha-
nese version of the GBS Scale. Alzheimer Dis Assoc Disord
bilitation program for older adults with cognitive impairment:
1991; 5: 40–48.
Preliminary results. Psychogeriatrics 2007; 7: 14–20.
22 Sclan SG, Reisberg B. Functional assessment staging (FAST) in
8 Yamagami T, Oosawa M, Ito S, Yamaguchi H. Effect of activity
Alzheimer’s disease: Reliability, validity, ordinality. Int Psycho-
reminiscence therapy as brain-activating rehabilitation for
geriatr 1992; 4: 55–69.
elderly people with and without dementia. Psychogeriatrics
23 Igarashi T, Konishi A, Sonehara D, Asahara H. Changes in
2007; 7: 69–75.
intellectual function during perioperative period evaluated by
9 Maddocks-Jennings W, Wilkinson JM. Aromatherapy practice
Hasegawa’s Dementia Scale. Masui 1995; 44: 60–65 (in Japa-
in nursing: Literature review. J Adv Nurs 2004; 48: 93–103.
nese with an English abstract).
10 Lee SY. The effect of lavender aromatherapy on cognitive func-
24 Rosen WG, Mohs RC, Davis KL. A new rating scale for Alzhe-
tion, emotion, and aggressive behavior of elderly with demenita.
imer’s disease. Am J Psychiatry 1984; 141: 1356–1364.
Taehan Kanho Hakhoe 2005; 35: 303–312 (in Korean with an
25 Arai Y, Kudo K, Hosokawa T, Washio M, Miura H, Hisamichi S.
English abstract).
Reliability and validity of the Japanese version of the Zarit Car-
11 Hur MH, Han SH. Clinical trial of aromatherapy on postpartum
egiver Burden Interview. Psychiatry Clin Neurosci 1997; 51:
mother’s perineal healing. Taehan Kanho Hakhoe 2004; 34:
281–287.
53–62 (in Korean with an English abstract).
26 Braak H, Braak E. Neuropathological stageing of Alzheimer-
12 Wheatley D. Medicinal plants for insomnia: A review of their
related changes. Acta Neuropathol 1991; 82: 239–259.
pharmacology, efficacy and tolerability. J Psychopharmacol
27 Gold G, Bouras C, Kovari E et al. Clinical validity of Braak
2005; 19: 414–421.
neuropathological staging in the oldest-old. Acta Neuropathol
13 Lewith GT, Godfrey AD, Prescott P. A single-blinded, random-
2000; 99: 579–584.
ized pilot study evaluating the aroma of Lavandula augustifolia
28 Bruel-Jungerman E, Laroche S, Rampon C. New neurons in the
as a treatment for mild insomnia. J Altern Complement 2005;
dentate gyrus are involved in the expression of enhanced long-
11: 631–637.
term memory following environmental enrichment. Eur J Neu-
14 Moss M, Cook J, Wesnes K, Duckett P. Aromas of rosemary and
rosci 2005; 21: 513–521.
lavender essential oils differentially affect cognition and mood in
29 Lazarov O, Robinson J, Tang Y et al. Environmental enrichment
healthy adults. Int J Neurosci 2003; 113: 15–38.
reduces Ab levels and amyloid deposition in transgenic mice.
15 Grassmann J, Schneider D, Weiser D, Elstner EF. Antioxidative
Cell 2005; 120: 701–713.
effects of lemon oil and its components on copper induced
© 2010 The Authors 179
Journal compilation © 2010 Japanese Psychogeriatric Society
You might also like
- Natural Perfume MakingDocument6 pagesNatural Perfume MakingAnonymous aBzTQbeiNo ratings yet
- DIY Perfume LocketDocument6 pagesDIY Perfume LocketAnonymous aBzTQbei100% (1)
- Essential Oils Perfume PDFDocument2 pagesEssential Oils Perfume PDFAnonymous aBzTQbeiNo ratings yet
- PerfumDocument4 pagesPerfumAnonymous aBzTQbeiNo ratings yet
- CHART - Essential Oil Complimentary Blending Chart - LEGAL PDFDocument3 pagesCHART - Essential Oil Complimentary Blending Chart - LEGAL PDFAnonymous aBzTQbeiNo ratings yet
- 15 DIY Essential Oil Recipes For Gifts HolidaysDocument6 pages15 DIY Essential Oil Recipes For Gifts HolidaysAnonymous aBzTQbeiNo ratings yet
- Twelve Tissue Remedies of Schussler Contents and Reading ExcerptDocument13 pagesTwelve Tissue Remedies of Schussler Contents and Reading ExcerptAnonymous aBzTQbeiNo ratings yet
- CHART - Essential Oil Complimentary Blending Chart - LEGAL PDFDocument3 pagesCHART - Essential Oil Complimentary Blending Chart - LEGAL PDFAnonymous aBzTQbeiNo ratings yet
- Perfum RECIPES LEGALDocument10 pagesPerfum RECIPES LEGALAnonymous aBzTQbeiNo ratings yet
- Deluxe HH Digital Microscope Manual 5lang WebDocument55 pagesDeluxe HH Digital Microscope Manual 5lang WebAnonymous aBzTQbeiNo ratings yet
- Essential Oil Recipes - Com Confidence Perfume RecipesDocument1 pageEssential Oil Recipes - Com Confidence Perfume RecipesAnonymous aBzTQbei100% (1)
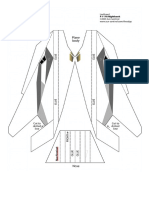
- Paper PlaneDocument1 pagePaper PlaneAnonymous aBzTQbeiNo ratings yet
- Aromatherapy Perfume RecipiesDocument19 pagesAromatherapy Perfume RecipiesAnonymous aBzTQbeiNo ratings yet
- Iridologia Psicoterapeutica VetorialDocument136 pagesIridologia Psicoterapeutica VetorialAnonymous aBzTQbei100% (1)
- Gráficos PDFDocument2 pagesGráficos PDFAnonymous aBzTQbeiNo ratings yet
- Airborne Glider 42in Oz10853Document1 pageAirborne Glider 42in Oz10853Anonymous aBzTQbeiNo ratings yet
- The Central RaceDocument22 pagesThe Central RaceJedidah100% (13)
- Aromatherapy and EpilepsyDocument4 pagesAromatherapy and EpilepsyAnonymous aBzTQbeiNo ratings yet
- Therapy For A New GenerationDocument3 pagesTherapy For A New GenerationAnonymous aBzTQbeiNo ratings yet
- Aromatherapy-Therapeutic Uses PDFDocument46 pagesAromatherapy-Therapeutic Uses PDFsachin.daga881No ratings yet
- ESense Skin Response Manual enDocument53 pagesESense Skin Response Manual enAnonymous aBzTQbeiNo ratings yet
- Therapy For A New GenerationDocument3 pagesTherapy For A New GenerationAnonymous aBzTQbeiNo ratings yet
- Aromatherapy Hand Massage Aromatherapy - GradworksDocument171 pagesAromatherapy Hand Massage Aromatherapy - GradworksAnonymous aBzTQbeiNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Goals of Prenatal CareDocument16 pagesGoals of Prenatal CareLhea Marie Trinidad100% (1)
- Peri ImplantitisDocument11 pagesPeri ImplantitisMuhammad GhifariNo ratings yet
- Research Interest Potential Advisors International StudentsDocument12 pagesResearch Interest Potential Advisors International StudentsAKREDITASI RS KOTA SERANGNo ratings yet
- Deciding When To Submit A 510 (K) For A Change To An Existing Device - Guidance For Industry and Food and Drug Administration StaffDocument77 pagesDeciding When To Submit A 510 (K) For A Change To An Existing Device - Guidance For Industry and Food and Drug Administration StaffsomzNo ratings yet
- The Impact of Nutrition Education On Knowledge, Attitude, and Practiceregarding Iron Deficiency Anemia Among Female Adolescent Studentsin JordanDocument7 pagesThe Impact of Nutrition Education On Knowledge, Attitude, and Practiceregarding Iron Deficiency Anemia Among Female Adolescent Studentsin JordanAppierien 4No ratings yet
- Antenatal CareDocument11 pagesAntenatal CareManasi ChaskarNo ratings yet
- What Is Medical DeontologyDocument11 pagesWhat Is Medical DeontologyExorticNo ratings yet
- Telemetry Recognition WorkbookDocument29 pagesTelemetry Recognition WorkbookQueenNo ratings yet
- Current Status of Child Health in IndiaDocument26 pagesCurrent Status of Child Health in IndiaAmy Lalringhluani100% (3)
- Air Quality Guidelines For EuropeDocument288 pagesAir Quality Guidelines For EuropeAlex OliveiraNo ratings yet
- Banking - Diksha Book On Effective Study Techniques PDFDocument66 pagesBanking - Diksha Book On Effective Study Techniques PDFHemrajSainiNo ratings yet
- Household 1Document2 pagesHousehold 1ainun rapikaNo ratings yet
- Pediatrics Wards History Taking TemplateDocument2 pagesPediatrics Wards History Taking TemplateBobet Reña80% (5)
- Nursing Care Plan Output (NCP) 50 Points: Activity 14Document2 pagesNursing Care Plan Output (NCP) 50 Points: Activity 14Nathaniel Pulido50% (2)
- f3 November Monthly TestDocument16 pagesf3 November Monthly TestNaqi SDARNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanAde HerlambangNo ratings yet
- Ab'Asanas (Expanded & Updated)Document56 pagesAb'Asanas (Expanded & Updated)Nicola AvonNo ratings yet
- Emergency ManagementDocument78 pagesEmergency ManagementHuey Calabines50% (2)
- AnemiaDocument33 pagesAnemiaDiwiasti Firdausi YasminNo ratings yet
- PE UNIT 1 Active Recreation (Lifestyle and Weight Management)Document26 pagesPE UNIT 1 Active Recreation (Lifestyle and Weight Management)Charmaine RamosNo ratings yet
- Black Book Project 3Document69 pagesBlack Book Project 3Pragya SinghNo ratings yet
- FOOTBALL (SOCCER) INJURY REPORTING FORM English WordsDocument3 pagesFOOTBALL (SOCCER) INJURY REPORTING FORM English WordsNinNo ratings yet
- 457 CBT UpdatedDocument82 pages457 CBT UpdatedDass DavidNo ratings yet
- Aat Dementia PDFDocument3 pagesAat Dementia PDFMinodora MilenaNo ratings yet
- Capillary Blood Glucose Performance Checklist: Numerical Rating Adjectival Description DescriptionDocument2 pagesCapillary Blood Glucose Performance Checklist: Numerical Rating Adjectival Description DescriptionAngeline NavarroNo ratings yet
- Textbook of Paediatric Emergency Medicine, 2ndDocument628 pagesTextbook of Paediatric Emergency Medicine, 2ndPhruek Hinhumpetch100% (1)
- EXSA - Gold Award Recipients 2006Document15 pagesEXSA - Gold Award Recipients 2006applebarrel100% (1)
- Ojs FianaDocument13 pagesOjs FianadespalitaNo ratings yet
- Approved Harmonized National RD Agenda 2017-2022 PDFDocument90 pagesApproved Harmonized National RD Agenda 2017-2022 PDFJoemel Bautista100% (1)